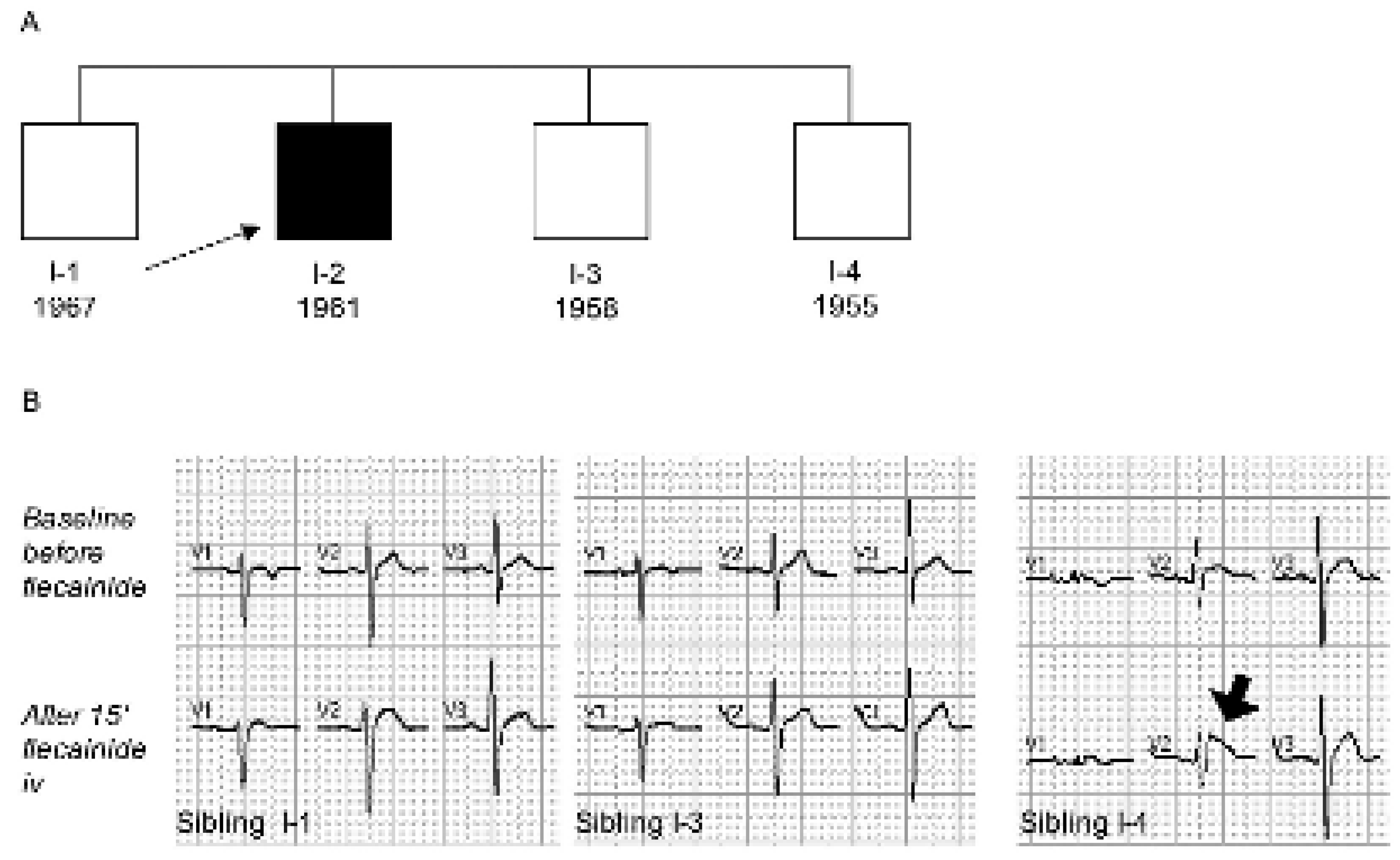
Right Bundle Branch Block or Brugada Syndrome?
Case Report
Explanatory Answers
References
- Brugada, P.; Brugada, J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome. J Am Coll Cardiol 1992, 20, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Wilde, A.A.M.; Antzelevitch, C.; Borggrefe, M.; Brugada, J.; Brugada, R.; Brugada, P.; et al. Proposed diagnostic criteria for the Brugada syndrome: Consensus report. Circulation 2002, 106, 2514–2519. [Google Scholar] [CrossRef] [PubMed]
- Keller, D.I.; Rougier, J.S.; Kucera, J.P.; Bennamar, N.; Fressart, V.; Guicheney, P.; et al. Brugada syndrome and fever: Genetic and molecular characterization of patients carrying SCN5A mutations. Cardiovasc Res 2005, 67, 510–519. [Google Scholar] [CrossRef] [PubMed]

© 2005 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Keller, D.I.; Osswald, S. Right Bundle Branch Block or Brugada Syndrome? Cardiovasc. Med. 2005, 8, 410. https://doi.org/10.4414/cvm.2005.01134
Keller DI, Osswald S. Right Bundle Branch Block or Brugada Syndrome? Cardiovascular Medicine. 2005; 8(11):410. https://doi.org/10.4414/cvm.2005.01134
Chicago/Turabian StyleKeller, Dagmar I., and Stefan Osswald. 2005. "Right Bundle Branch Block or Brugada Syndrome?" Cardiovascular Medicine 8, no. 11: 410. https://doi.org/10.4414/cvm.2005.01134
APA StyleKeller, D. I., & Osswald, S. (2005). Right Bundle Branch Block or Brugada Syndrome? Cardiovascular Medicine, 8(11), 410. https://doi.org/10.4414/cvm.2005.01134



