Percutaneous Left Ventricular Assist Device to Support PCI of Unprotected Left Main Coronary Artery Disease
Introduction
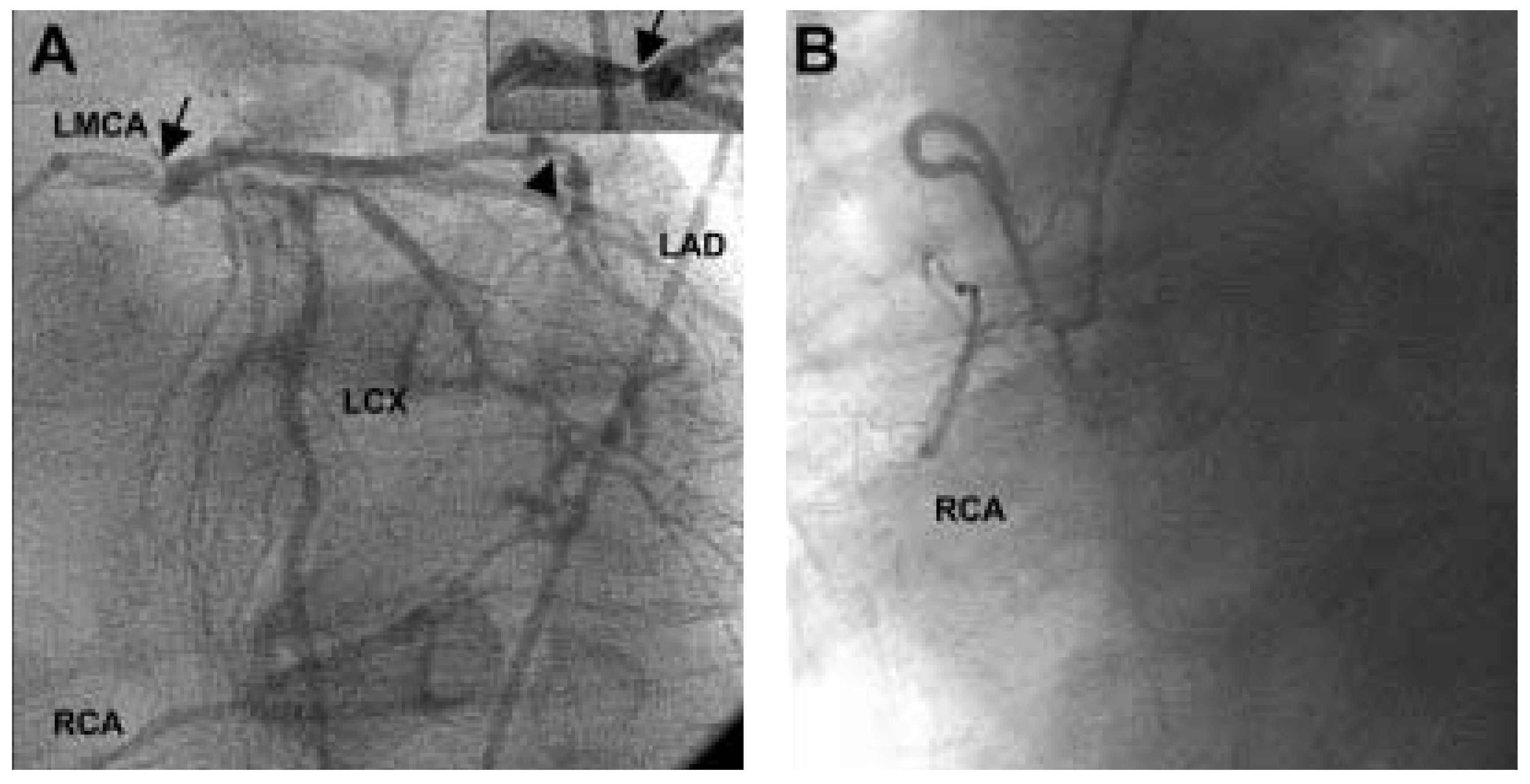
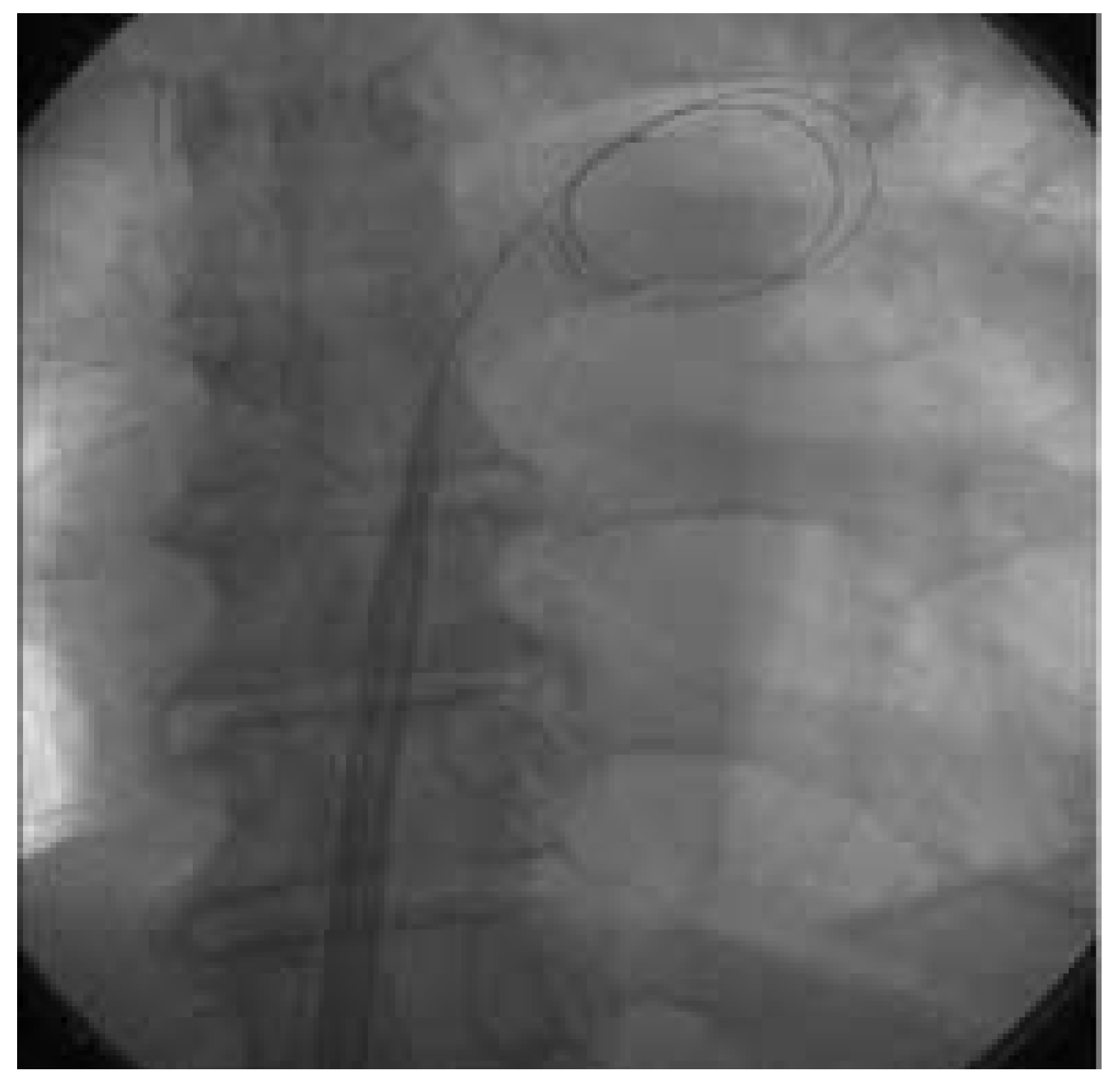
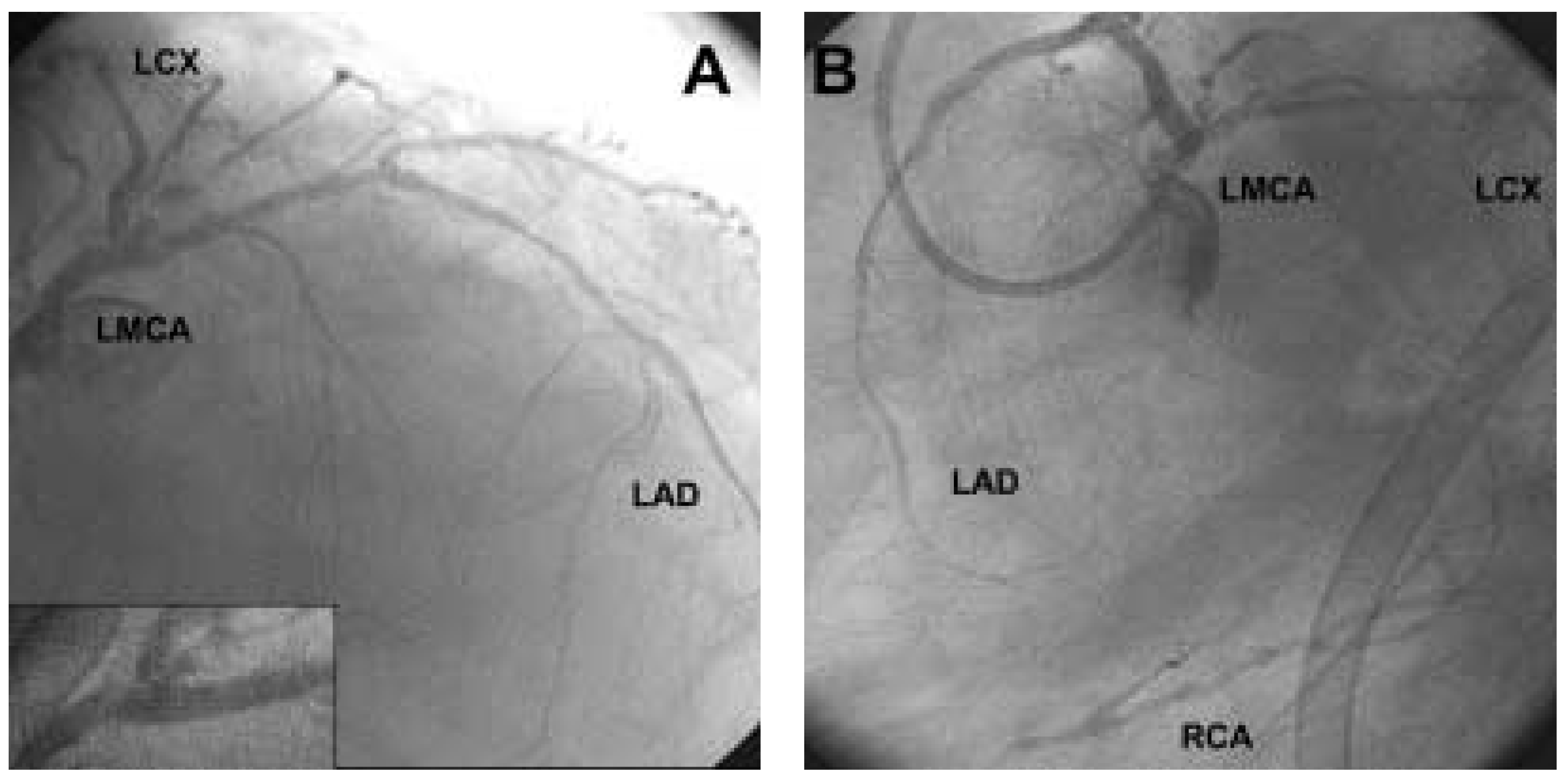
Case report
Discussion
References
- Windecker, S.; Roffi, M.; Meier, B. Sirolimus eluting stent: a new era in interventional cardiology? Curr. Pharm. Des. 2003, 9, 1077–1094. [Google Scholar] [CrossRef] [PubMed]
- Smith SCJr Dove, J.T.; Jacobs, A.K.; et al. ACC/AHA guidelines of percutaneous coronary interventions (revision of the 1993 PTCA guidelines) — executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty). J. Am. Coll. Cardiol. 2001, 37, 2215–2239. [Google Scholar]
- O’Keefe JHJr Hartzler, G.O.; Rutherford, B.D.; et al. Left main coronary angioplasty: early and late results of 127 acute and elective procedures. Am. J. Cardiol. 1989, 64, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Eagle, K.A.; Guyton, R.A.; Davidoff, R.; et al. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation 1999, 100, 1464–1480. [Google Scholar] [PubMed]
- Brueren, B.R.; Ernst, J.M.; Suttorp, M.J.; et al. Long-term followup after elective percutaneous coronary intervention for unprotected non-bifurcational left main stenosis: is it time to change the guidelines? Heart 2003, 89, 1336–1339. [Google Scholar] [CrossRef] [PubMed]
- Kelley, M.P.; Klugherz, B.D.; Hashemi, S.M.; et al. One-year clinical outcomes of protected and unprotected left main coronary artery stenting. Eur. Heart J. 2003, 24, 1554–1559. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, P.; Foley, D.P.; de Feijter, P.J.; Vos, J.; Smits, P.; Serruys, P.W. Clinical introduction of the Tandemheart, a percutaneous left ventricular assist device, for circulatory support during high-risk percutaneous coronary intervention. Int. J. Cardiovasc Intervent 2003, 5, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Arampatzis, C.A.; Lemos, P.A.; Tanabe, K.; et al. Effectiveness of sirolimus-eluting stent for treatment of left main coronary artery disease. Am. J. Cardiol. 2003, 92, 327–329. [Google Scholar] [CrossRef] [PubMed]
- Butman, S.M.; Jamison, K.; Slepian, M.; Edling, N.; Arabia, F.; Copeland, J.G. Percutaneous intervention for unprotected left main disease prior to explantation of a left ventricular assist device. Catheter. Cardiovasc. Interv. 2003, 59, 471–474. [Google Scholar] [CrossRef] [PubMed]
© 2004 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Cook, S.; Meier, B.; Windecker, S. Percutaneous Left Ventricular Assist Device to Support PCI of Unprotected Left Main Coronary Artery Disease. Cardiovasc. Med. 2004, 7, 258. https://doi.org/10.4414/cvm.2004.01030
Cook S, Meier B, Windecker S. Percutaneous Left Ventricular Assist Device to Support PCI of Unprotected Left Main Coronary Artery Disease. Cardiovascular Medicine. 2004; 7(6):258. https://doi.org/10.4414/cvm.2004.01030
Chicago/Turabian StyleCook, Stéphane, Bernhard Meier, and Stephan Windecker. 2004. "Percutaneous Left Ventricular Assist Device to Support PCI of Unprotected Left Main Coronary Artery Disease" Cardiovascular Medicine 7, no. 6: 258. https://doi.org/10.4414/cvm.2004.01030
APA StyleCook, S., Meier, B., & Windecker, S. (2004). Percutaneous Left Ventricular Assist Device to Support PCI of Unprotected Left Main Coronary Artery Disease. Cardiovascular Medicine, 7(6), 258. https://doi.org/10.4414/cvm.2004.01030



