Beating Heart Surgery
Abstract
Zusammenfassung
Introduction
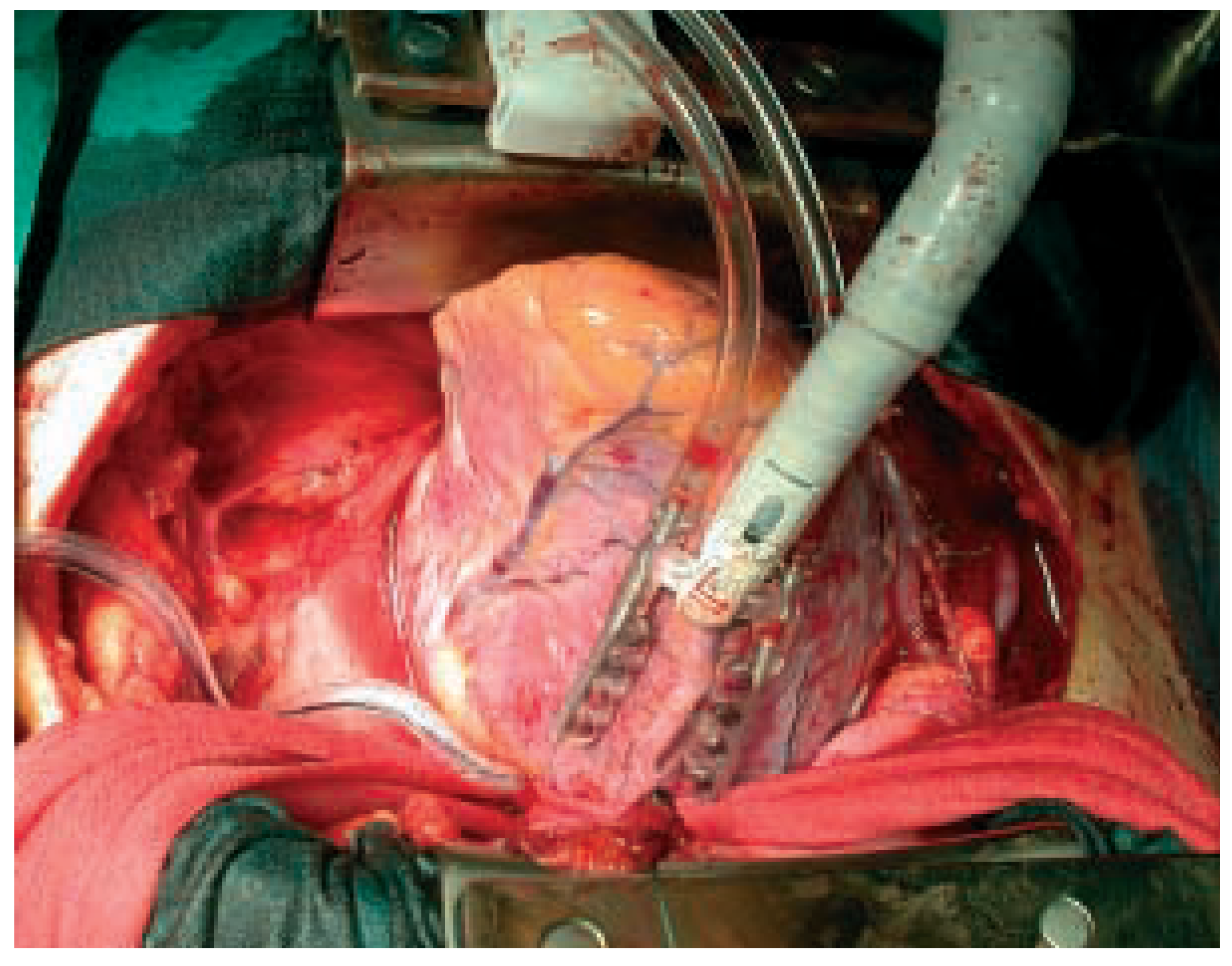
Surgical technique
First experience with this technique
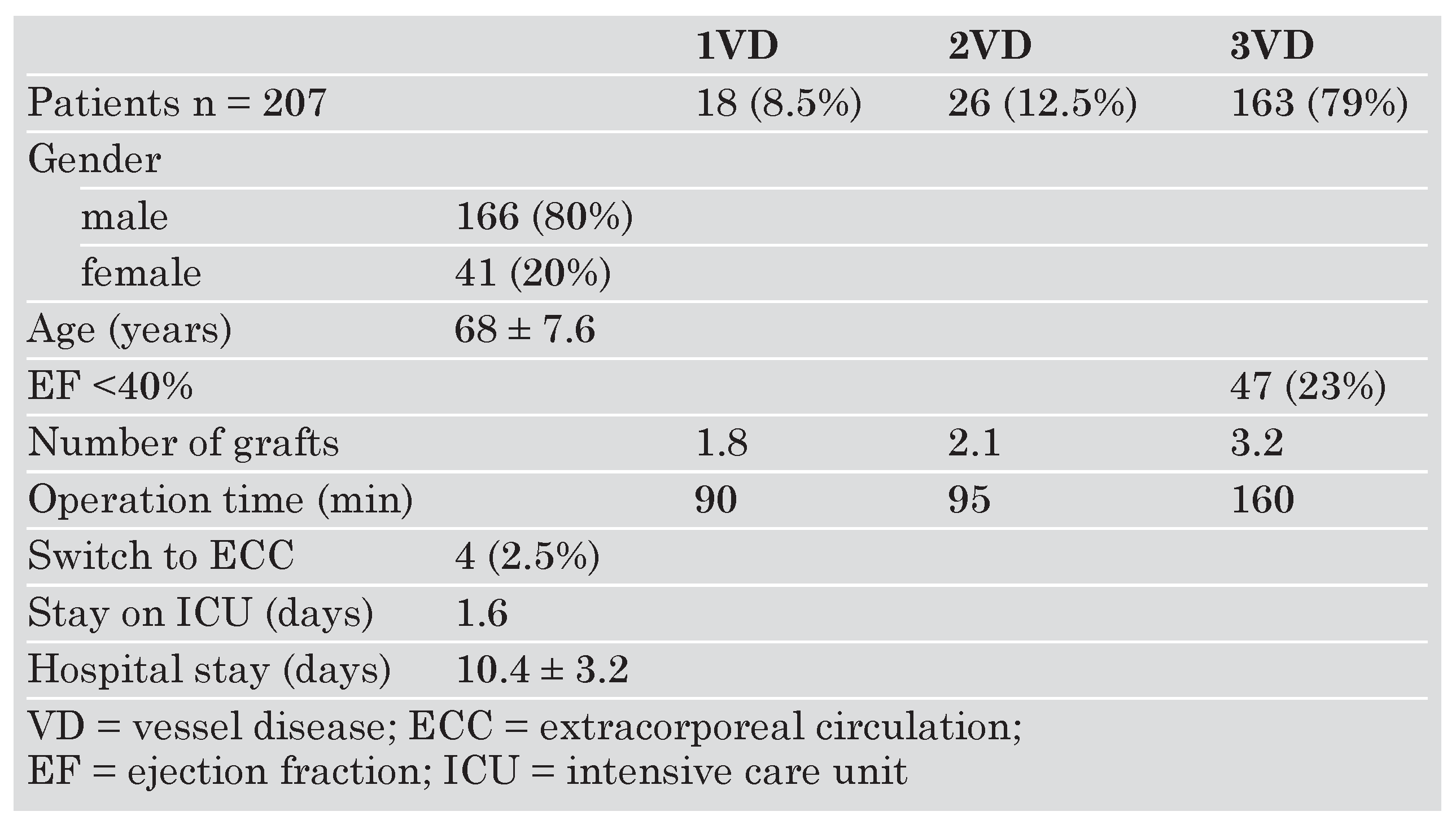
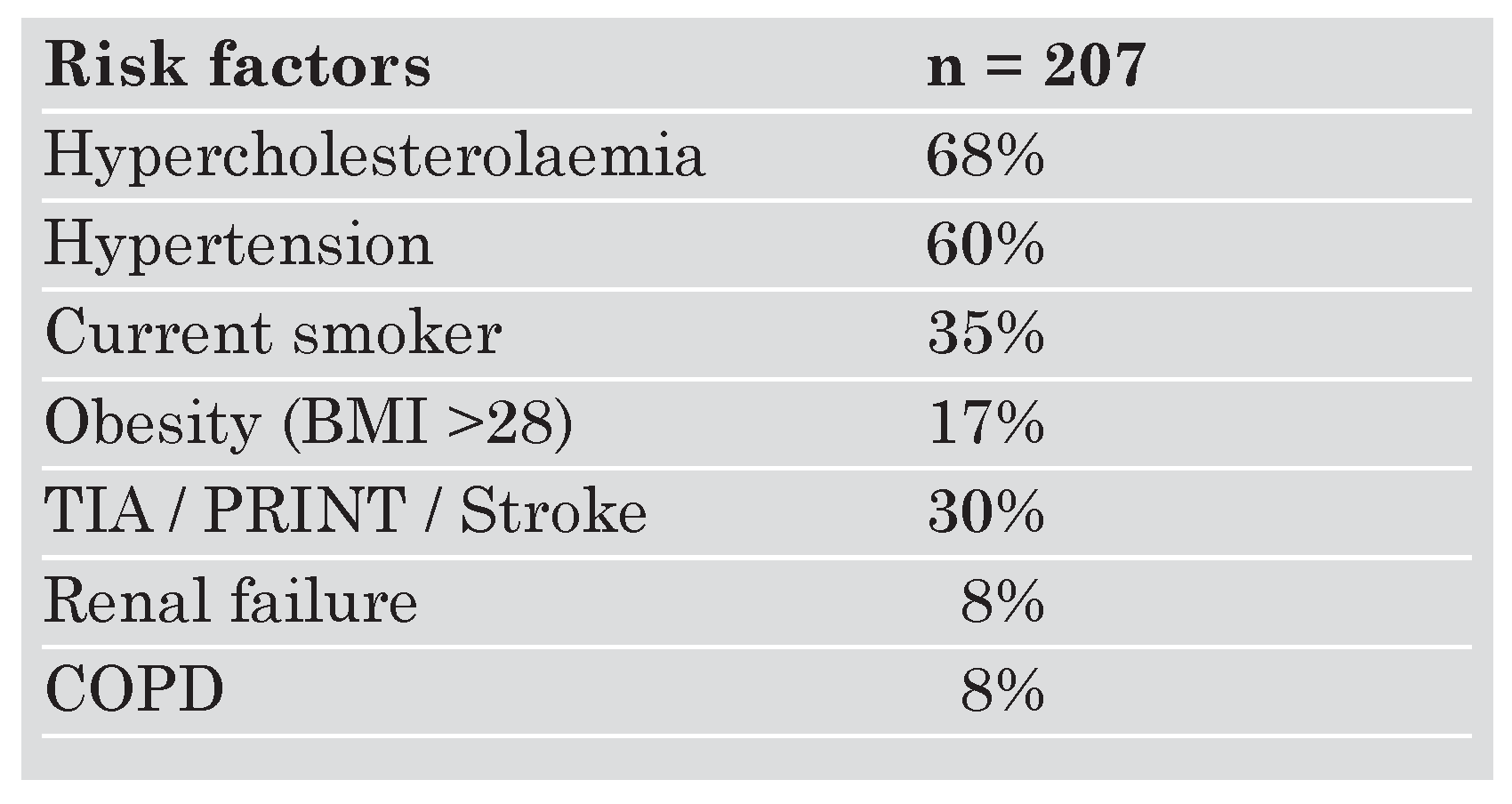
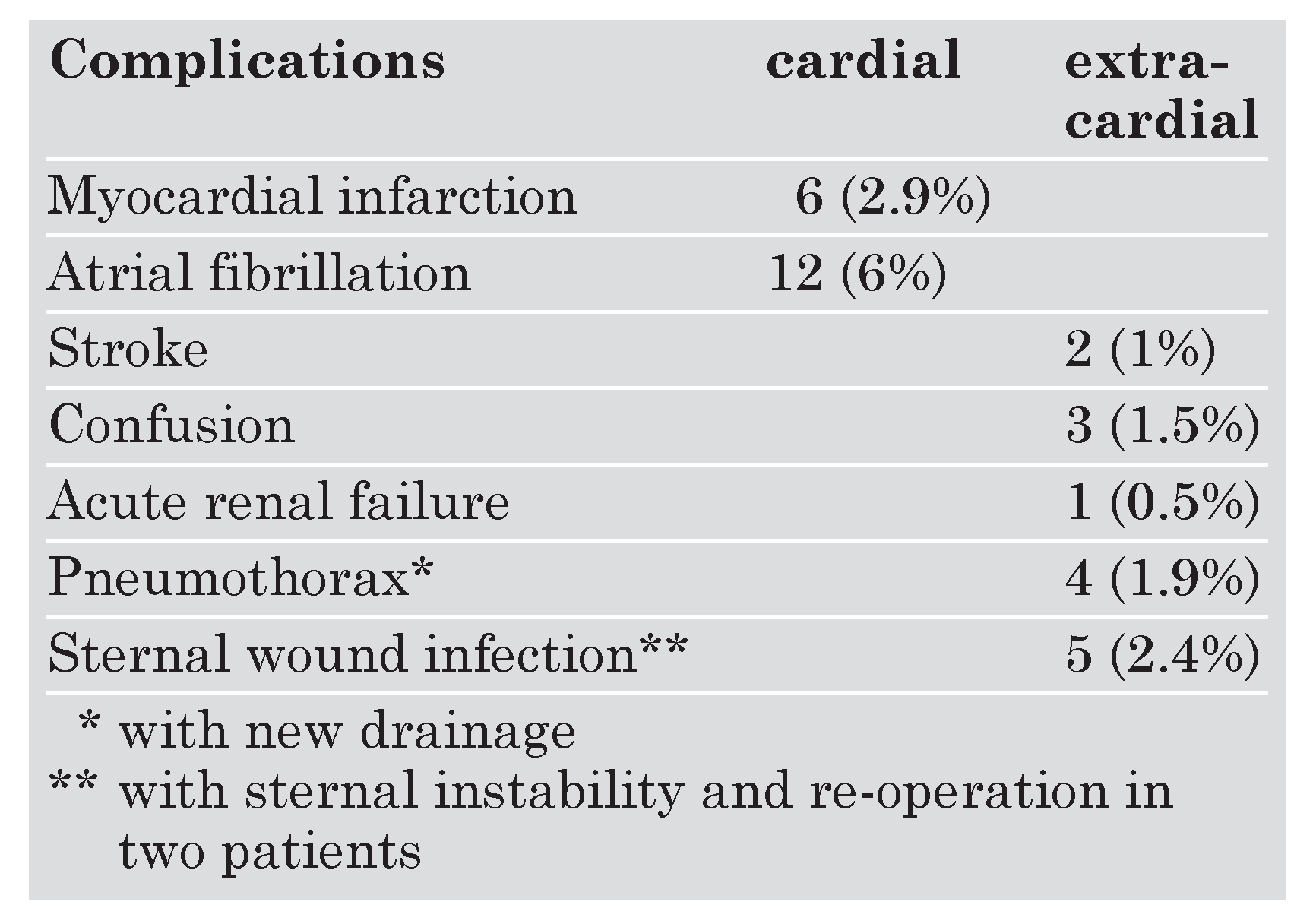
Discussion
Summary
References
- Yacoub, M. Off-pump coronary bypass surgery: in search of an identity. Circulation 2001, 104, 1743–1745. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, I.; Murkin, J.M. Beating heart surgery or conventional CABG: are neurological outcomes different? J Thoracic Cardiovasc Surg 2001, 13, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Kirklin, J.K.; Westaby, S.; Blackstone, E.F.; Kirklin, J.W.; Chenwerth, D.E.; Pacifico, A.D. Complement and the damaging effects of cardiopulmonary bypass. J. Thorac. Cardiovasc. Surg. 1983, 86, 845–857. [Google Scholar] [CrossRef] [PubMed]
- Kirklin, J.K. Prospects for understanding and eliminating the deleterious effects of cardiopulmonary bypass. Ann. Thorac. Surg. 1991, 51, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Rocker, G.M.; Westaby, S. Inflammatory response to cardiopulmonary bypass. Ann. Thorac. Surg. 1993, 55, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Stump, D.A.; Jones, T.J.J.; Rorie, K.D. Neuropsychological monitoring and outcomes in cardiovascular surgery. J. Cardiothorac. Vasc. Anesth. 1999, 13, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Pugsley, W.; Klingert, L.; Paschalis, C.; Treasure, T.; Harrison, M.; Newman, S. The impact of micro emboli during cardiopulmonary bypass on neuropsychological functioning. Stroke 1994, 25, 1393–1399. [Google Scholar] [CrossRef] [PubMed]
- Jansen, E.W.L.; Grünemann, P.F.; Borst, C. Less invasive off pump CABG using a suction device for immobilization: the Octopus method. Eur. J. Cardiovasc. Surg. 1997, 12, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Calafiore, A.M.; di Mauro, M.; Contini, M.; di Giammarco, G.; Pano, M.; Vitolla, G.; et al. Myocardial revascularization with and without cardiopulmonary bypass in multivessel disease: impact of the strategy on early outcome. Ann. Thorac. Surg. 2001, 72, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.C.; Spoomer, T.H.; Pym, J.; et al. A review of 1582 consecutive Octopus off pump coronary artery bypass patients. Ann. Thorac. Surg. 2000, 70, 1017–1020. [Google Scholar] [CrossRef] [PubMed]
- Shanewise JS, Cheung AT, Aronson S, Stuwart WJ, Weiss RL, Mark JB, et al. : ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transoesophageal echocardiography examination: recommendations. Anesth. Analg. 1999, 89, 870–887. [Google Scholar]
- Fransen, E.; Maessen, J.; Dentener, M.; Senden, N.; Gesekes, G.; Buurman, W. Systemic inflammation present in patients undergoing CABG without extracorporal circulation. Chest 1998, 113, 1290–1295. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.S.; Larsen, K.; Houx, P.; Skovgaard, L.T.; Hanning, C.D.; Moller, J.T. The assessment of postoperative cognitive function. Act. Anaesthesiol. Scand. 2001, 45, 275–289. [Google Scholar] [CrossRef] [PubMed]
- Diegeler, A.; Hirsch, R.; Schneider, F.; Schilling, L.O.; Falk, V.; Tauch, T.; et al. Neuromonitoring and neurocognitive outcome in off-pump versus conventional coronary bypass operation. Ann. Thorac. Surg. 2000, 69, 1162–1166. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk D, Jansen EWL, et al (Octopus Study Group). Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery. JAMA 2002, 287, 1405–1412. [Google Scholar] [CrossRef] [PubMed]
- Puskas, J.D.; Thourani, V.H.; Marshall, J.J.; Dempsey, S.J.; Steiner, M.A.; Sammons, B.H.; et al. Clinical outcomes, angiographic patency and resource utilization in 200 consecutive off-pump coronary bypass patients. Ann Thorac Surg 2001, 71, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk D, Nierich AP, Jansen EWL, et al (Octpus Study Group). Early outcome after off-pump versus on-pump coronary bypass surgery: results from a randomized study. Circulation 2001, 104, 1761–1766. [Google Scholar] [CrossRef] [PubMed]
- Angelini, G.D.; Taylor, F.C.; Reeves, B.C.; Ascione, R. Early and midterm outcome after off-pump and on-pump surgery in beating heart against cardioplegic arrest studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet 2002, 359, 1194–1199. [Google Scholar] [CrossRef] [PubMed]
- Ascione, R.; Caputo, M.; Calori, G.; Lloyd, C.T.; Underwood, M.J.; Angelini, G.D. Predictors of atrial fibrillation after conventional and beating heart coronary surgery: a prospective randomized study. Circulation 2000, 102, 1530–1535. [Google Scholar] [CrossRef] [PubMed]
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernet, F.; Grapow, M.; Zerkowski, H.-R. Beating Heart Surgery. Cardiovasc. Med. 2004, 7, 214. https://doi.org/10.4414/cvm.2004.01026
Bernet F, Grapow M, Zerkowski H-R. Beating Heart Surgery. Cardiovascular Medicine. 2004; 7(5):214. https://doi.org/10.4414/cvm.2004.01026
Chicago/Turabian StyleBernet, F., M. Grapow, and H.-R. Zerkowski. 2004. "Beating Heart Surgery" Cardiovascular Medicine 7, no. 5: 214. https://doi.org/10.4414/cvm.2004.01026
APA StyleBernet, F., Grapow, M., & Zerkowski, H.-R. (2004). Beating Heart Surgery. Cardiovascular Medicine, 7(5), 214. https://doi.org/10.4414/cvm.2004.01026




