Summary
The aim of this prospective study was to evaluate the appropriateness of cholesterol management in Swiss clinical practice according to the recommendations of Swiss Society of Cardiology. 99 office-based physicians participated in this survey in order to provide questionnaire reporting demographic and clinical data for every adult consulting each physician during five consecutive days. Questionnaires were obtained for 8791 patients (55% of women) with mean age of 56 ± 18 years. Among them, 63% were screened for total cholesterol, 49% for triglycerides, 39% for HDL-cholesterol and only 21% for LDL-cholesterol. Cardiac (CHD) risk category and age over 50 years were good predictors of lipid screening. Among eligible patients, only 34% of women and 55% of men received lipid-lowering agents in the high risk group, whereas this proportion was much more lower in moderate and low risk groups. Furthermore, among treated patients, the mean level of cholesterol was higher than ideal (<5.0 mmol/L), even in the high risk group (7.2 ± 1.0 and 6.9 ± 1.4 mmol/L), respectively for women and men. According to Evidence-Based Medicine, these results clearly indicate a missed opportunity for detection and treatment of patients with increased cardiovascular risk. Such data require to promote the quality of cholesterol management in clinical practice.
Key words: preventive cardiology; cholesterol management; cholesterol screening; cholesterol therapy; primary care physicians; appropriateness
Résumé
Cette étude a eu pour but d'évaluer l'adéquation de la prise en charge du facteur cholestérol, d'après les recommandations de la Société suisse de Cardiologie, au cabinet médical en Suisse. 99 médecins installés en pratique privée participèrent à cette enquête, en remplissant un questionnaire médical se rapportant aux données démographiques et cliniques pour chaque patient qui s'était présenté au cabinet médical durant cinq jours consécutifs. 8791 patients, dont 55% de femmes (Fe) furent examinés. L'âge moyen était de 56 ± 18 ans. Le «screening» du cholestérol total fut établi pour 63% d'entre-deux, ce taux étant respectivement de 49% pour les triglycérides, 39% pour le HDL-cholestérol et de 21% pour le LDL-cholestérol. Dans la catégories des patients à haut risque qui étaient éligibles pour un traitement médicamenteux hypolipémiant, seuls 34% des femmes (Fe) et 55% des hommes (Ho) étaient traités. Cette proportion était encore plus faible dans les catégories à risque modéré et faible. De plus, chez les patients à risque, le taux de cholestérol mesuré se situait bien au-dessus des valeurs idéales (<5,0 mmol/l), y compris chez les patients à haut risque (Fe = 7,2 ± 1,0 et Ho = 6,9 ± 1,4 mmol/l). En regard des connaissances médicales actuelles, ces données montrent clairement un manquement d'opportunité pour le dépistage et le traitement de l'hypercholestérolémie chez les patients à risque cardiovasculaire accru. Cela démontre la nécessité de promouvoir la qualité de la prise en charge du facteur cholestérol au cabinet médical.
Key words: cardiologie préventive; cholestérol management; cholestérol screening; cholestérol thérapie; médedins généralistes; approprié
Introduction
Epidemiological and clinical studies clearly established the link between dyslipidaemia and coronary heart disease (CHD) [
1,
2,
3,
4,
5]. Effectiveness of lipid-lowering therapy became an evident knowledge when a significant reduction of CHD mortality and morbidity was demonstrated in primary and secondary prevention trials among patients using a statin treatment as compared to the placebo groups [
6,
7,
8,
9,
10].
Despite the evidence of preventable coronary events, particularly among high risk patients, many studies suggest that lipid-lowering drugs (LLDs) are underprescripted. Cholesterol values are often far from goal levels according to patient risk category. Surprisingly after an acute myocardial infarction (AMI) or with a severe cardiovascular disease most patients do not receive any treatment, despite
a pathological lipid status. Moreover, it was reported that 30–35% of patients discharged after an AMI took lipid-lowering drugs and only 10–15% of subjects reached LDL-cholesterol goal levels [
11,
12,
13,
14]
.In Switzerland two studies presented similar results in secondary prevention patients [15, 16]. Approximately one third of the patients with CHD received a cholesterol-lowering drug and 50% of these patients had a total cholesterol level above 7.8 mmol/L.
In light of the previous observational studies, the aim of our study was to evaluate the actual adherence to the guidelines published in 1999 by the Working group Lipid/Atherosclerosis of the Swiss Society of Cardiology (WGLA/SSC) among Swiss physicians in clinical practice [
17]. Moreover, we tried to identify factors that were associated with a better cholesterol management.
Patients and methods
For the present observational study a sample of 99 office-based physicians was chosen providing 8791 visits to adults during the first semester 2000. A standardized questionnaire was completed by each practitioner to report demographic data, cardiovascular risk profile, lipid status if a screening had been carried out and the eventual lipid current therapy for any patients. 55 general practitioners, 26 cardiologists and 18 internists participated. Territorial distribution of these physicians was homogenous in the four countries portions: West, Alps/Prealps, West Middle-Land and East Middle-Land. The questionnaire was completed for every adult patient (>20 years) consulting each physician during five consecutive days.
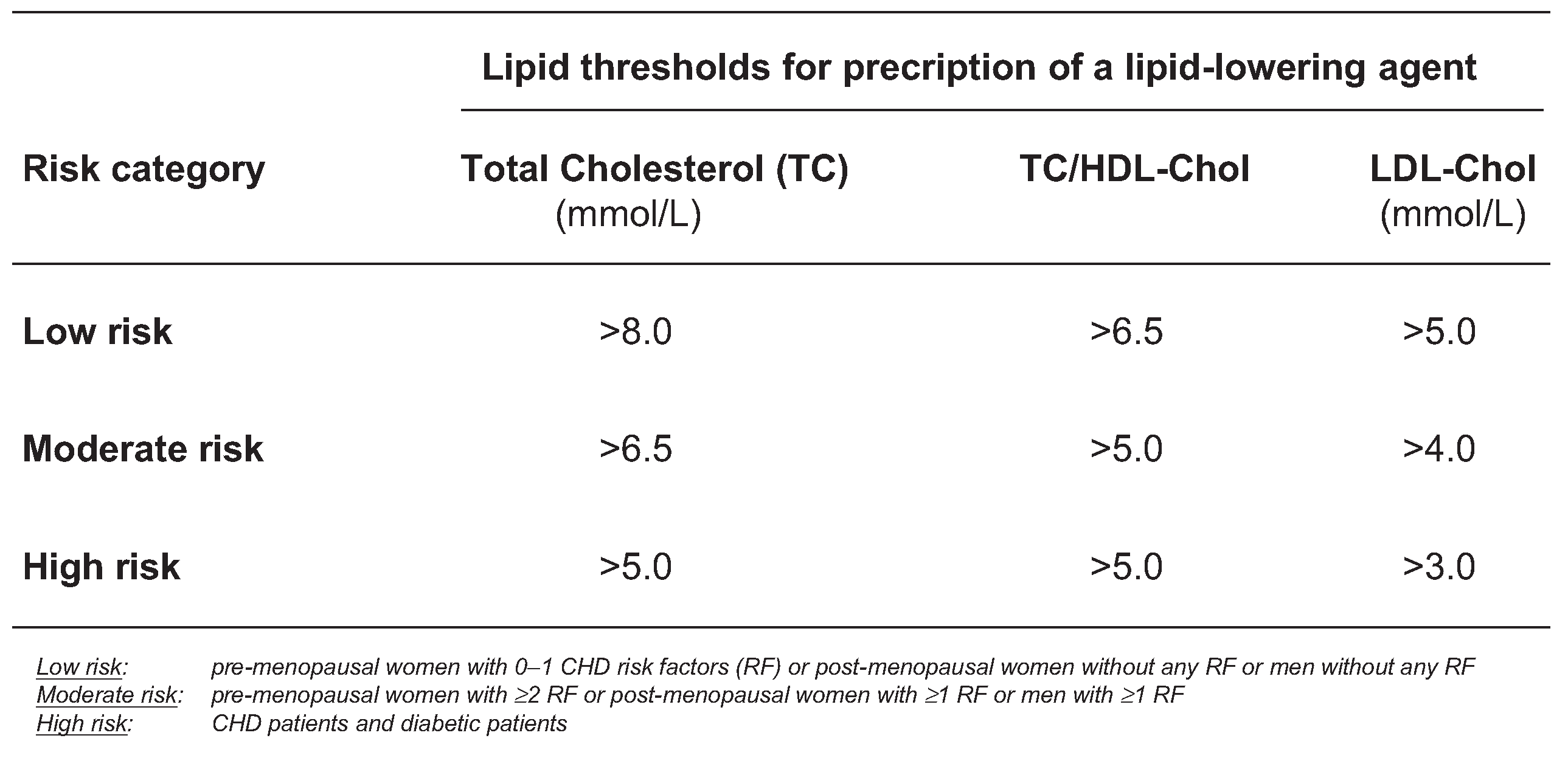
According to the 1999 Swiss guidelines (
Figure 1), the patients were stratified in three categories of CHDrisk based on the following criteria: the high risk group included CHD patients and diabetic patients. CHD patients had a established history of coronary heart disease: a past history of infarction, angina or revascularisation procedures. The moderate risk group included pre-menopausal women with at least two CHD risk factors or post-menopausal women and men with at least one risk factor. The low risk group included pre-menopausal women with none or one risk factor or post-menopausal women and men without any risk factor.
The following CHD risk factors were considered in our analysis: family history of CHD (cardiovascular disease among primary degree parents aged <65 years for women and <55 years for men); age (women >60 years, men >50 years); cigarette smoking; hypertension (blood pressure ≥140/90 mm Hg); obesity (BMI >30 kg/m2). Diabetes was regarded as a CHD risk equivalent.
Statistical analyses
The final results set included data from 8791 questionnaires. Categorizations of lipid levels were based on the WGLA guidelines. The chi squared tests were used in preliminary analyses for comparison of categorical variables. Logistic regression was used to determine the predictors of the lipid screening and of the prescription of LLDs. The following variables were considered potential predictors: age, gender, history of diabetes, hypertension, smoke, obesity, family history and previous CHD. For each CHD factor risk we fixed as reference [
1] the absence of risk. For sex factor, female was reference and age ≤50 years was age reference. A p <0.05 was considered statistically significant. All analyses were carried out in Stata software version 7.0 (Stata Corp., College Station, Texas, USA).
Results
Baseline characteristics
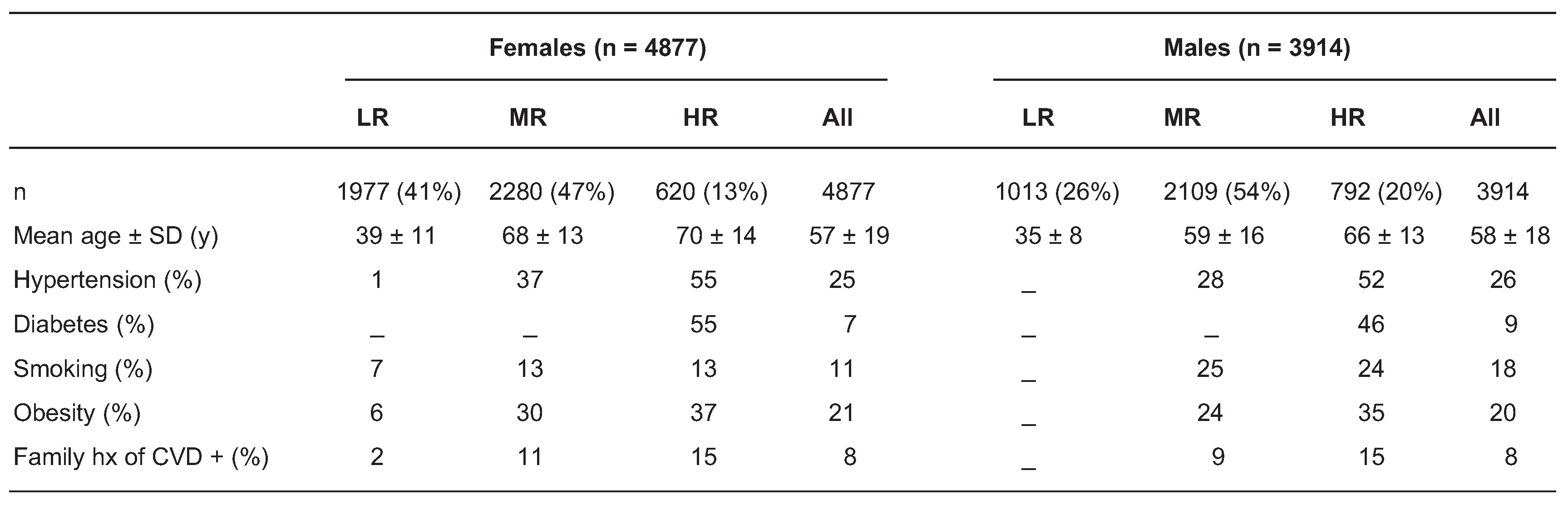
8791 questionnaires were analysed, comprising 4877 women (55%) and 3914 men (45%) with a mean age of 56 ± 18 years. According to the WGLA/SSC guidelines, 2990 patients were classified in the low risk group (34%), 4389 in the moderate risk one (50%) and 1412 in the high risk one (16%). In this latter group, 52% of patients had CHD and 50% of patients had diabetes. Clinical characteristics of participants were summarised in
Figure 2. Hypertension represented the most prevalent risk factor. A quarter of all patients and 50% of high risk patients had hypertension.
Lipid screening
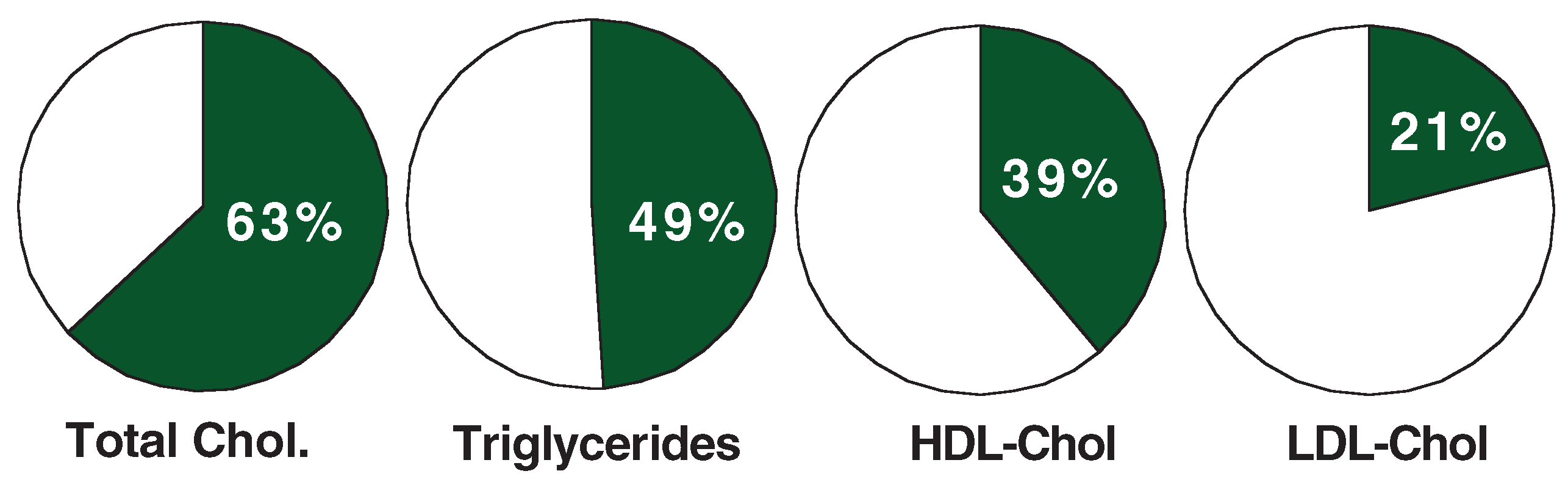
61% of females and 63% of males were screened for cholesterol, whereas this proportion was lower for triglycerides, HDL-cholesterol and particularly LDL-cholesterol.
Figure 3 shows the proportion of patients among the whole sample with known lipid parameters. Total cholesterol dosage was required by general practitioners in 57% of their patients, by internist in 68% and by cardiologist in 71% (p <0.001). In west and middle-west Switzer
land the screening rate was higher with 68% and 64% respectively, compared to 57% in the other area (p <0.001).
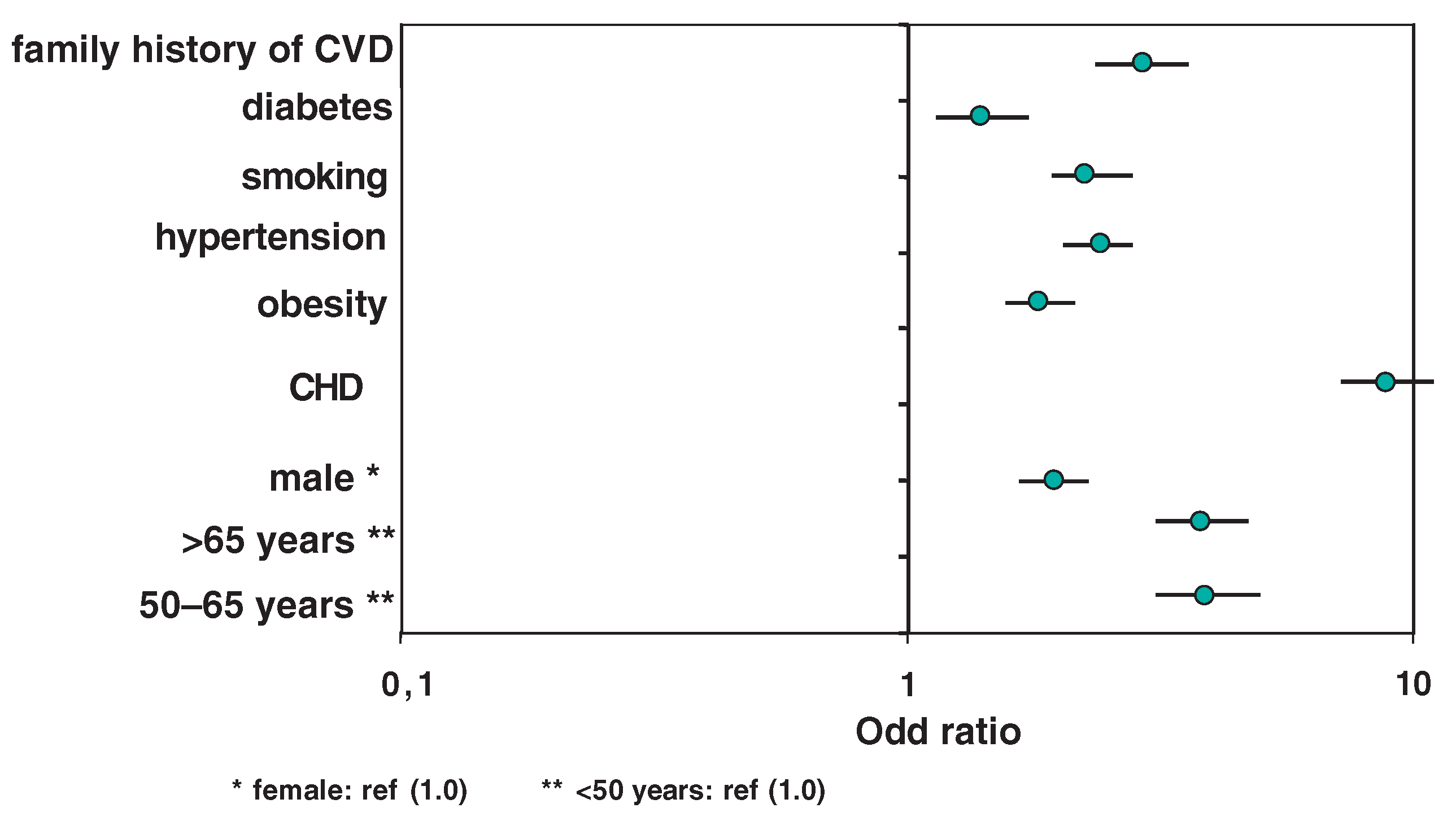
The multivariate analysis showed the characteristics which predicted lipid screening. Patients with one or more cardiovascular risk factors were more likely to be screened. Patients with diabetes, hypertension, obesity or family history had an odd ratio (OR) of being screened between 2.16 and 2.67 (p <0.001). Patients who smoked had an OR of 1.52 (95% CI 1.32–1.76; p <0.001). Age of patients was also significantly associated with cholesterol screening. Between 50 and 65 years the OR of being screened was 3.84 (95% CI 3.40–4.34; p <0.001), at over 65 years it was 3.64 (95% CI 3.23–4.10; p <0.001), compared to patients below 50 years. Furthermore, patients of the moderate risk and high risk groups were more likely screened than in the low risk one. OR was 4.57 (95% CI 4.14–5.04; p <0.001) and 11.02 (95% CI 9.34–13.00; p <0.001) respectively.
Eligibility to the lipid-lowering therapy
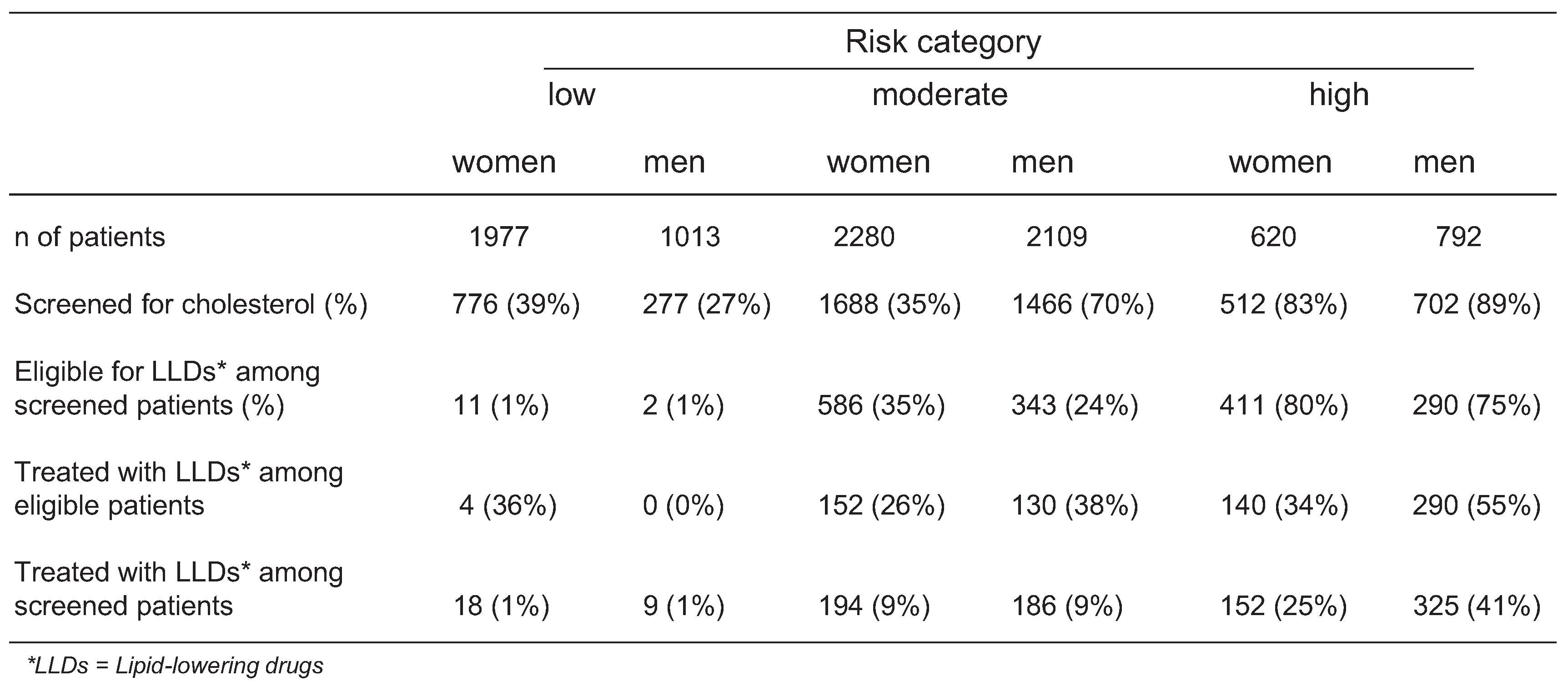
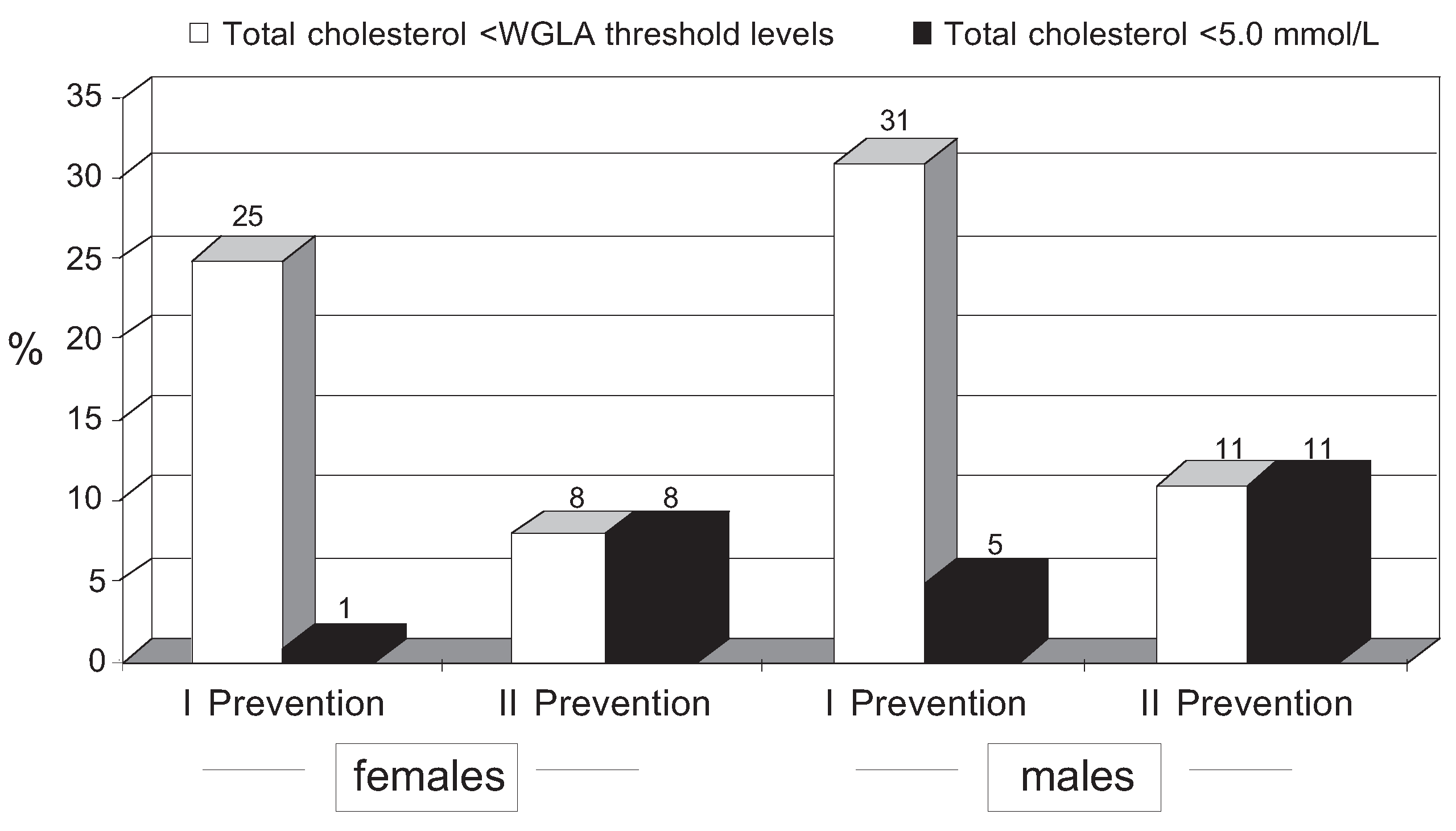
These data are summarised in
Figure 4. Among screened patients, in the low risk group 1% of women and 1% of men had a cholesterol value
above WGLA treatment threshold (8 mmol/L). In the moderate risk group, 35% of women and 24% of men had a value above this goal (6.5 mmol/L). Finally, in the high risk group 80% of women and 75% of men were above the treatment threshold level (5.0 mmol/L).
Lipid-lowering treatment
The proportion of patients receiving lipid lowering agents (LLDs) among eligible patients according to the risk category, respectively for women and men, is presented in the second part of
Figure 4. The rate of treatment was the highest in the high risk group, with 34% of females and 55% of males under LLDs. These rates reached only 26% and 38% respectively, in the moderate risk group. 39% of CHD patients managed by a general practitioner or an internist were treated by LLDs, whereas
this proportion was significantly higher (52%, p <0.001) when the patients were treated by a cardiologist. Treatment rate in secondary prevention was higher in the west region (56%) contrasting with the rest of the country (39%, p <0.001).
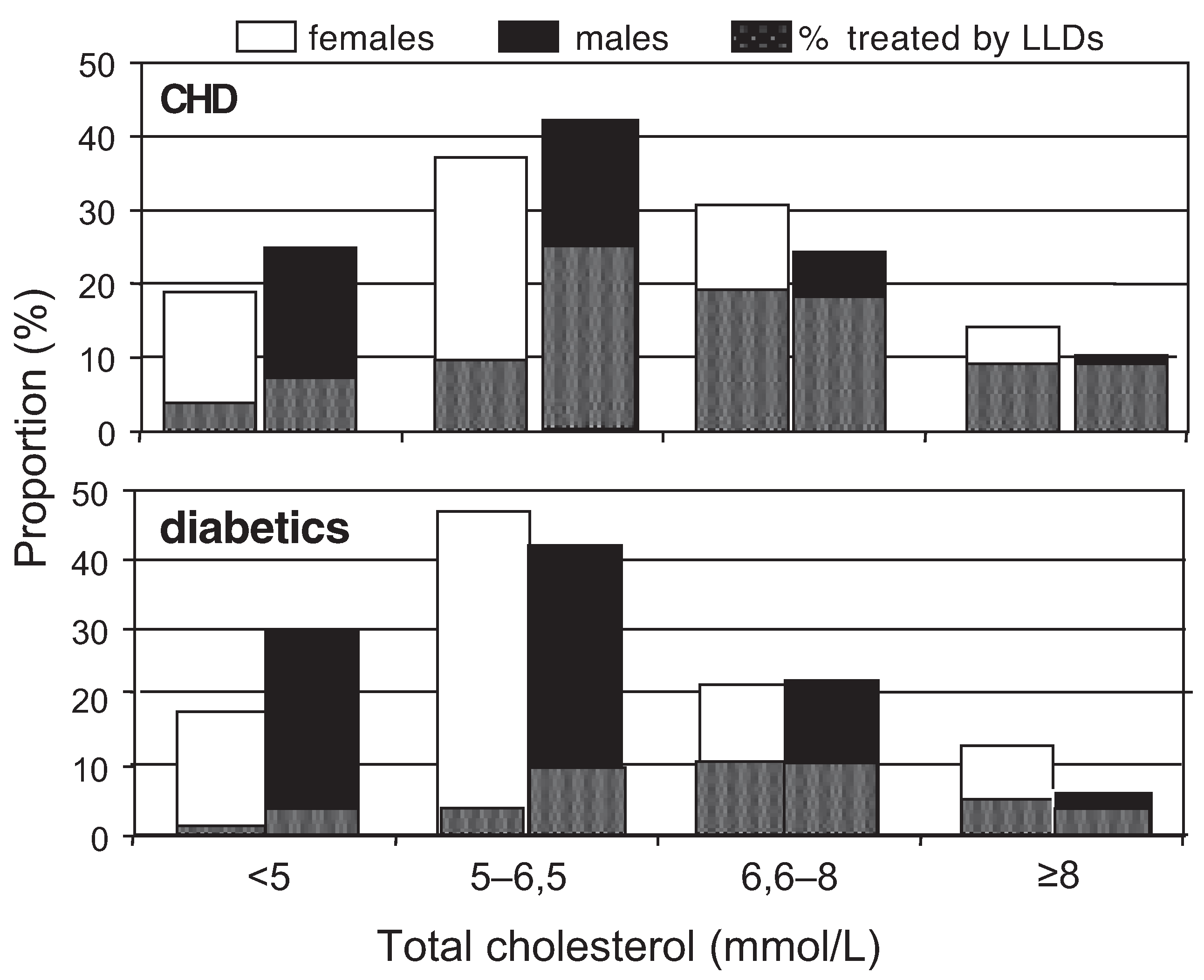
Figure 6 represents the proportion high risk patients, such as diabetic and CHD patients under LLDs, according to cholesterol values. Despite a similar distribution of total cholesterol values between the two groups, the proportion of treated patients was much lower in diabetic patients. With a cholesterol level at 5.0–6.5 mmol/L, only 16% of diabetics and 48% of CHD patients received LLDs (p <0.001). When cholesterol level was at 6.5–8.0 mmol/L, these rates reached 48% and 72% respectively in diabetic and CHD groups (p <0.001). A similar score was observed in patients with a cho
lesterol level above 8 mmol/L (48% and 79%,
p <0.001). The predictors of prescription of LLDs among eligible patients was established with a multivariate analysis. As presented in
Figure 5, the most important factors which predicted a lipid-lowering treatment were CHD (OR = 8.42, 95% CI 7.69–10.04; p <0.001) and age
between 50 and 65 years (OR = 3.90, 95% CI
3.10–4.90; p <0.001) or age >65 years as compared to age below 50 years (OR = 3.83, 95% CI 3.04–4.82; p <0.001). In contrast, diabetes was the weakest predictor factor: OR = 1.38 (95% CI 1.12–1.72; p <0.001).
Discussion
In our population lipid screening was clearly underused. In the whole sample cholesterol levels had been determined in 63% of patients. In the high risk group, physicians ignored cholesterol value of 15% of their patients. Among the screened patients, only in one third of cases the physician tested all three lipid values (total cholesterol, HDL-cholesterol and triglycerides) and calculated the LDL-cholesterol level. These results are comparable to those of
Ledergerber Swiss study, which showed a complete lipid screening in only 33% of patients [
16]
. No significant difference was observed in cholesterol screening according to physician specialty. Advanced age (>50 years) was a significant factor for lipid screening; on the other hand the gender of patients did not influence the physician attitude.
Although WGLA guidelines were widely distributed since 1989 and updated in 1999, these data demonstrate that only a minority of patients who could benefit from such treatment, including those with documented CHD, are treated appropriately. Euroaspire Study [
18] results clearly point out an underuse of LLAs in CHD patients in other European countries.
In our group of CHD and diabetic patients who were eligible for a lipid lowering agent, 66% of women and 45% of men did not take any hypolipidemic drugs.
The multivariate analysis showed that despite a clear eligibility, diabetic patients and women were less likely to receive lipid lowering medication. In the eligible patients group, 24% of diabetic females were treated versus 47% of CHD females and 35% of diabetic males versus 70% of CHD ones.
Under-treatment in female and diabetic patients had also been reported in our 2002 study examining cholesterol management in 4072 Swiss workers [
19].
Unlike other studies [13, 20] older age over 50 years was a predictor of a better cholesterol management. Furthermore, our data demonstrate a clear correlation between the baseline cholesterol level and the proportion of treated patients. 80% of CHD patients with a total cholesterol above 8 mmol/L were treated; on the other hand when total cholesterol ranged between 5 and 6.5 mmol/L only 43% of CHD patients were treated. This result is particularly significant if we consider that 45% of the whole sample had a total cholesterol level between 5 and 6.5 mmol/L.
Nevertheless, treated patients often had a total cholesterol above the optimal value of 5 mmol/L despite of a drug intake. In primary prevention only 1% of females and 5% of males had a total cholesterol level below 5 mmol/L despite a treatment. In secondary prevention 8% of treated females and 11% of treated males had an «optimal» cholesterol value. Mean cholesterol values in treated patients were far to reach the target level; we found in any group of patients a mean total cholesterol always above 6.9 mmol/L. The data suggest that the majority of treated patients are recruited with the highest values of total cholesterol and that these patients received inappropriate choice and/or dose of statins to achieve the therapeutic goal.
Our study had several methodological limitations. The sample of 99 physicians who participated to this study could not be representative of daily clinical practice performed by primary care physicians and specialists. However, these data confirm the evidence of inappropriateness of cholesterol management according to evidence based medicine observed in other reports.
Another limitation is linked to the type of data collection based on medical records reported by physicians. Patients demographic data, cardiovascular risk factors, lipid values and lipid lowering treatment data were not verified on patient chart. Moreover, we based our definition of hyperlipidaemia (and achievement of WGLA 99 goals) on single values of total cholesterol, rather than multiple determinations of lipoprotein subfractions (particularly LDL-cholesterol values as defined by ATP II guidelines) [
21]. For these reasons we might have misclassified a few patients with elevated LDL-cholesterol levels but a total cholesterol level below the target value or patients with a total cholesterol level above target values but reduced LDL-cholesterol level and elevated HDL-cholesterol levels.
A last limitation was the lack of previous cholesterol values, before lipid lowering treatment prescription; this further information could permit to estimate overuse of lipid lowering agents and to report a longitudinal observation on lipid management.
Finally, this study was not designed to identify the specific causes of non-prescription attributable either to the patients or to the physicians. In this regard, further studies are absolutely needed to optimize quality management of cholesterol in clinical practice.
Conclusion
Our results suggest that there was no evidence of overuse of lipid screening or therapy. Patients were globally undertreated despite a pathological lipid status, particularly in patients with a high CHD risk. Diabetes was often not considered as a CHD risk equivalent, a CHD patient was more likely to be treated than a diabetic one. Moreover, among the treated patients, the mean levels of total cholesterol were far from the target values according to risk category.
These results lead us to necessity to promote the quality management of cholesterol in clinical practice in order to improve the fight against cardiovascular diseases.