Of Nutty Professors and Pristine Coronary Arteries
“Professor Meier is nuts!”
Braunwald-Horton Trajectory
PCA65 Patients
The Power of a Zero Calcium Score
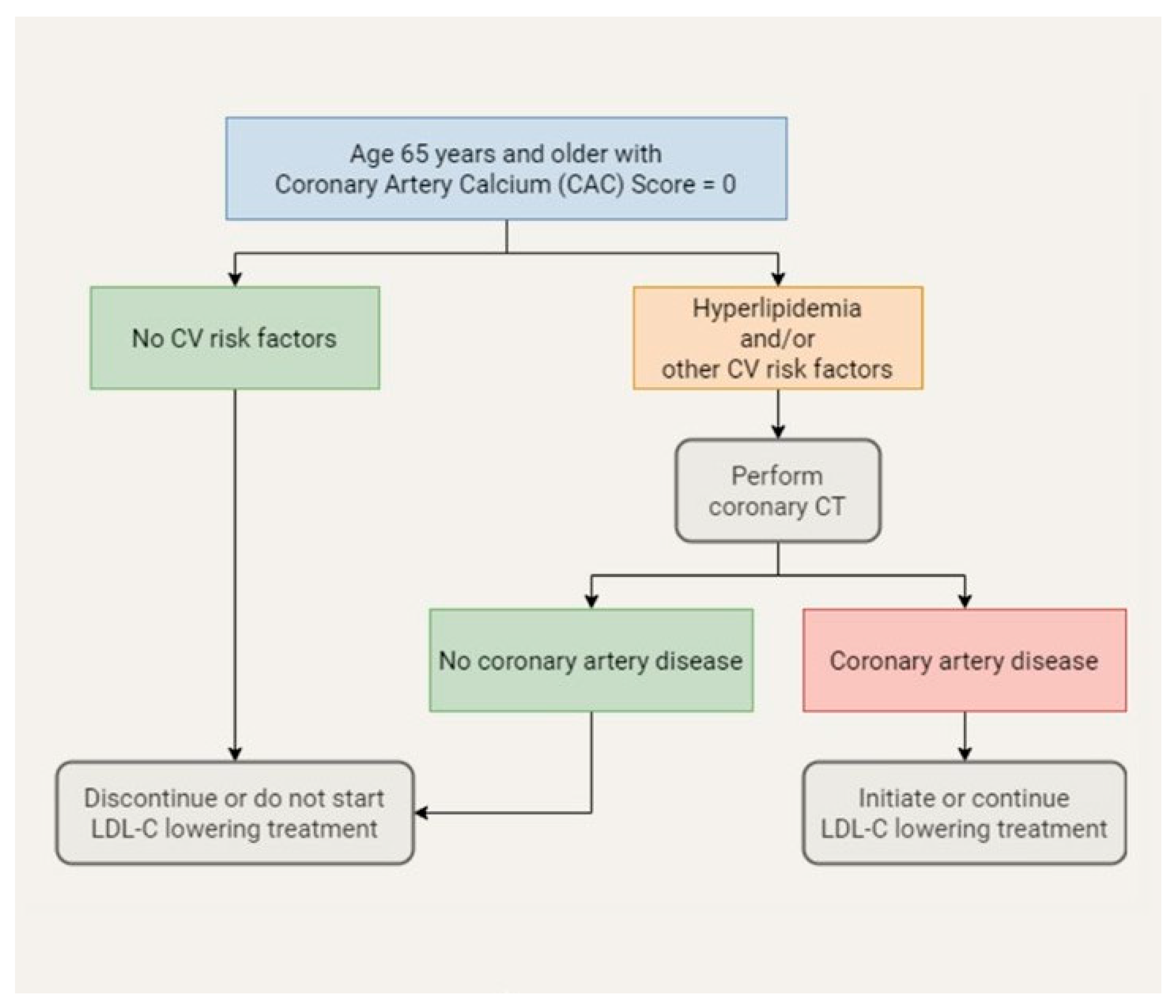
To Treat or Not to Treat
Outlook
Conflict of Interest
References
- Braunwald, E. How to live to 100 before developing clinical coronary artery disease: A suggestion. Eur Heart J. 2022, 43, 249–250. [Google Scholar] [CrossRef] [PubMed]
- Horton, J.D.; Cohen, J.C.; Hobbs, H.H. PCSK9: A conver- tase that coordinates LDL catabolism. J Lipid Res. 2009, 50, S172–S177. [Google Scholar] [CrossRef] [PubMed]
- Yano, Y.; O’Donnell, C.J.; Kuller, L.; Kavousi, M.; Erbel, R.; Ning, H.; et al. Association of Coronary Artery Calcium Score vs Age With Cardiovascular Risk in Older Adults: An Analysis of Pooled Population-Based Studies. JAMA Cardiol. 2017, 2, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Valenti, V.; Ó Hartaigh, B.; Heo, R.; Cho, I.; Schulman- Marcus, J.; Gransar, H.; et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: A prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 2015, 8, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Mittal, T.K.; Pottle, A.; Nicol, E.; Barbir, M.; Ariff, B.; Mirsad- raee, S.; et al. Prevalence of obstructive coronary artery disease and prognosis in patients with stable symp- toms and a zero-coronary calcium score. Eur Heart J Cardiovasc Imaging. 2017, 18, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, M.B.; Gaur, S.; Frimmer, A.; Bøtker, H.E.; Sørensen, H.T.; Kragholm, K.H.; et al. Association of Age With the Diagnostic Value of Coronary Artery Calcium Score for Ruling Out Coronary Stenosis in Symptomatic Patients. JAMA Cardiol. 2022, 7, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Bigler, M.R.; Gräni, C. The power of zero calcium score: Is there a need for improvement? J Nucl Cardiol. 2022, 29, 334–336. [Google Scholar] [CrossRef] [PubMed]
- Messerli, F.H. Ephemeral Coronary Heart Disease. Eur Heart J. 2019, 40, 1906–1908. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, M.B.; Dzaye, O.; Bøtker, H.E.; Jensen, J.M.; Maeng, M.; Bentzon, J.F.; et al. Low-Density Lipoprotein Cholesterol Is Predominantly Associated With Athero- sclerotic Cardiovascular Disease Events in Patients With Evidence of Coronary Atherosclerosis: The Western Denmark Heart Registry. Circulation. 2023, 147, 1053–1063. [Google Scholar] [CrossRef] [PubMed]
- Berner Institut für Hausarztmedizin (BIHAM), Inselspital Bern. (2023). STREAM Trial. Available online: https://www.statin-stream.ch.
- Walser, R. Der Räuber. Frankfurt: Suhrkamp; 1986.
© 2024 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Messerli, F.H.; Blum, M.R.; Meier, B. Of Nutty Professors and Pristine Coronary Arteries. Cardiovasc. Med. 2024, 27, 31. https://doi.org/10.4414/cvm.2024.1262905452
Messerli FH, Blum MR, Meier B. Of Nutty Professors and Pristine Coronary Arteries. Cardiovascular Medicine. 2024; 27(1):31. https://doi.org/10.4414/cvm.2024.1262905452
Chicago/Turabian StyleMesserli, Franz H., Manuel R. Blum, and Bernhard Meier. 2024. "Of Nutty Professors and Pristine Coronary Arteries" Cardiovascular Medicine 27, no. 1: 31. https://doi.org/10.4414/cvm.2024.1262905452
APA StyleMesserli, F. H., Blum, M. R., & Meier, B. (2024). Of Nutty Professors and Pristine Coronary Arteries. Cardiovascular Medicine, 27(1), 31. https://doi.org/10.4414/cvm.2024.1262905452



