Eliminating the Trigger for Polymorphic Ventricular Tachycardia
Abstract
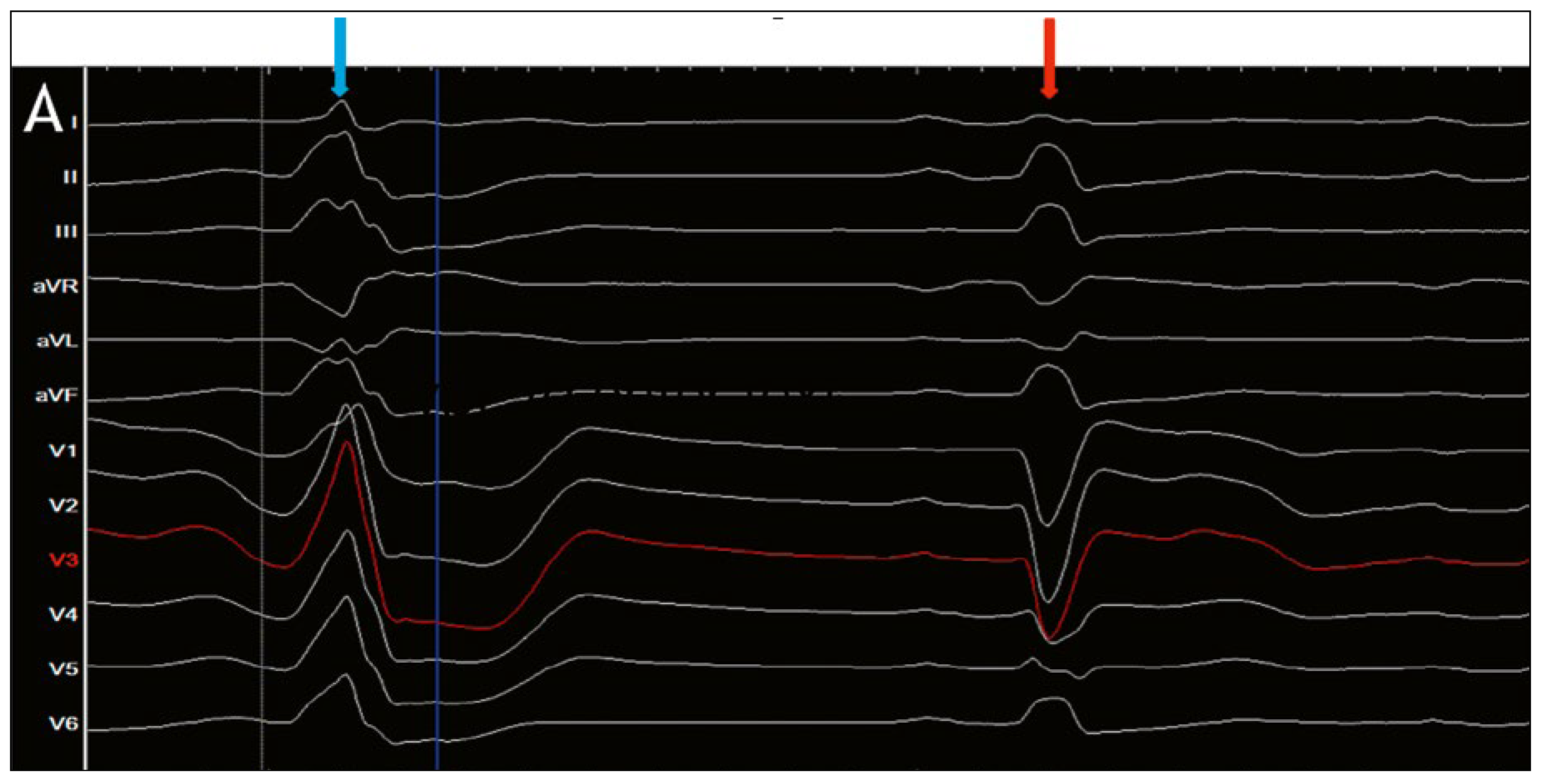
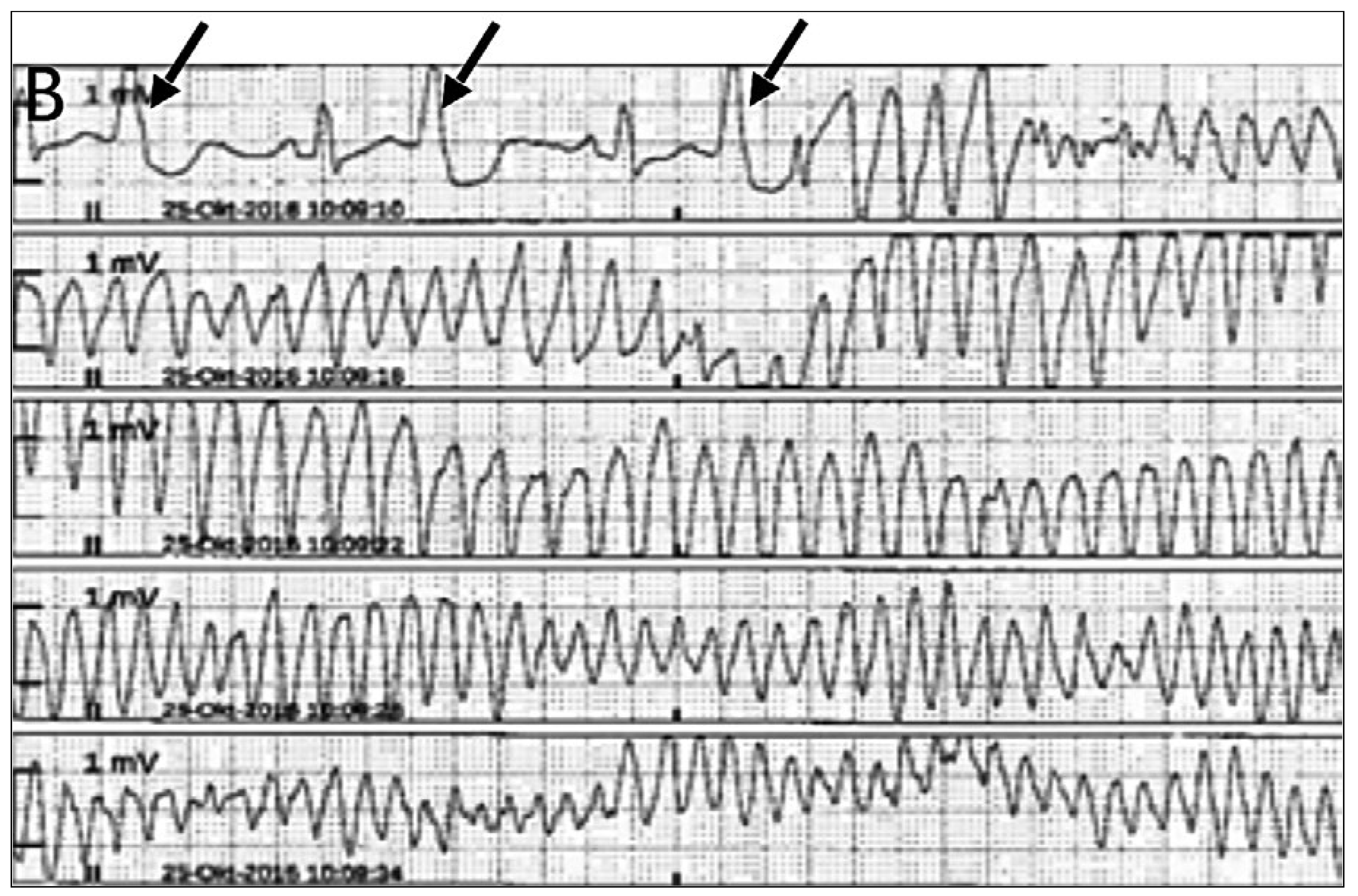
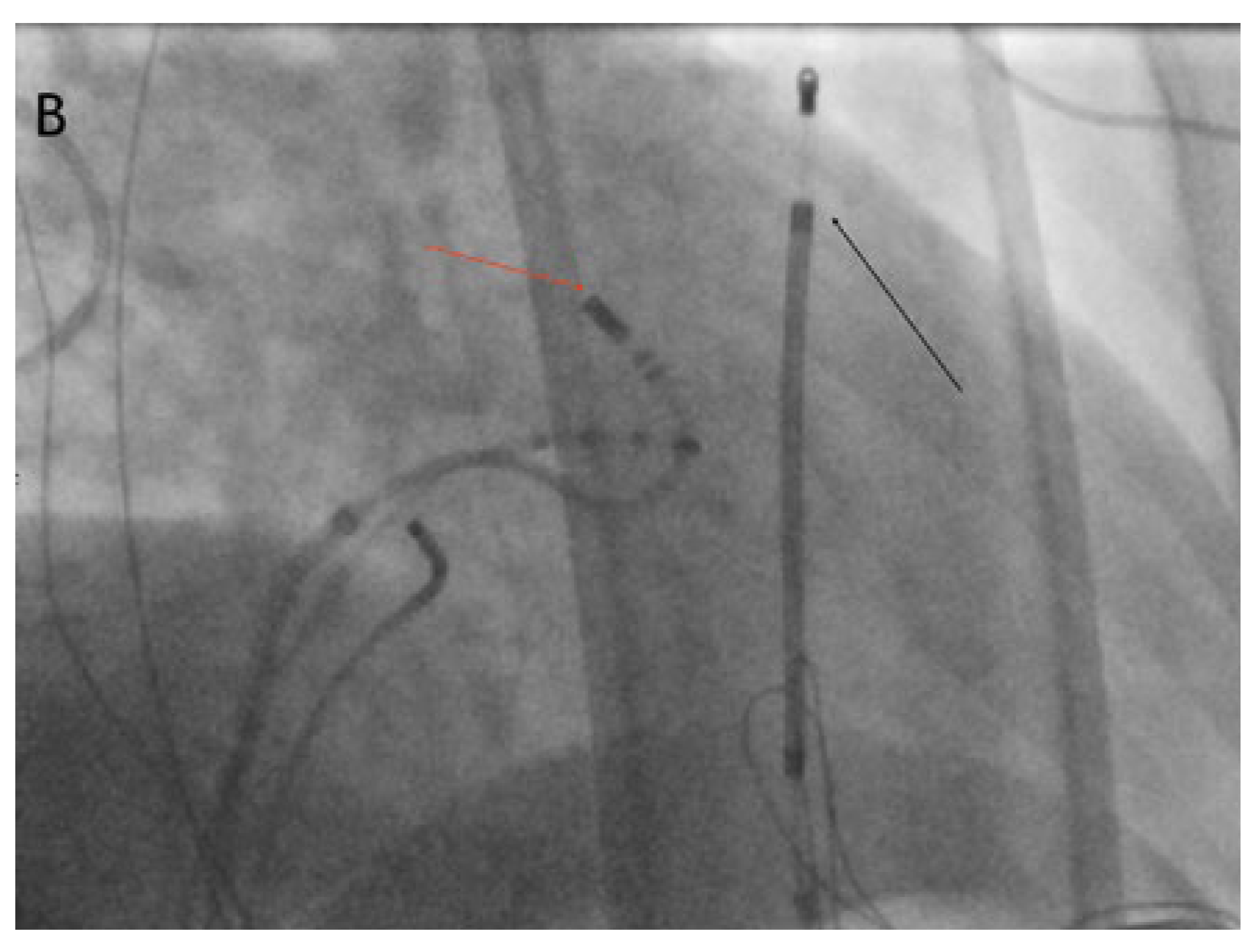
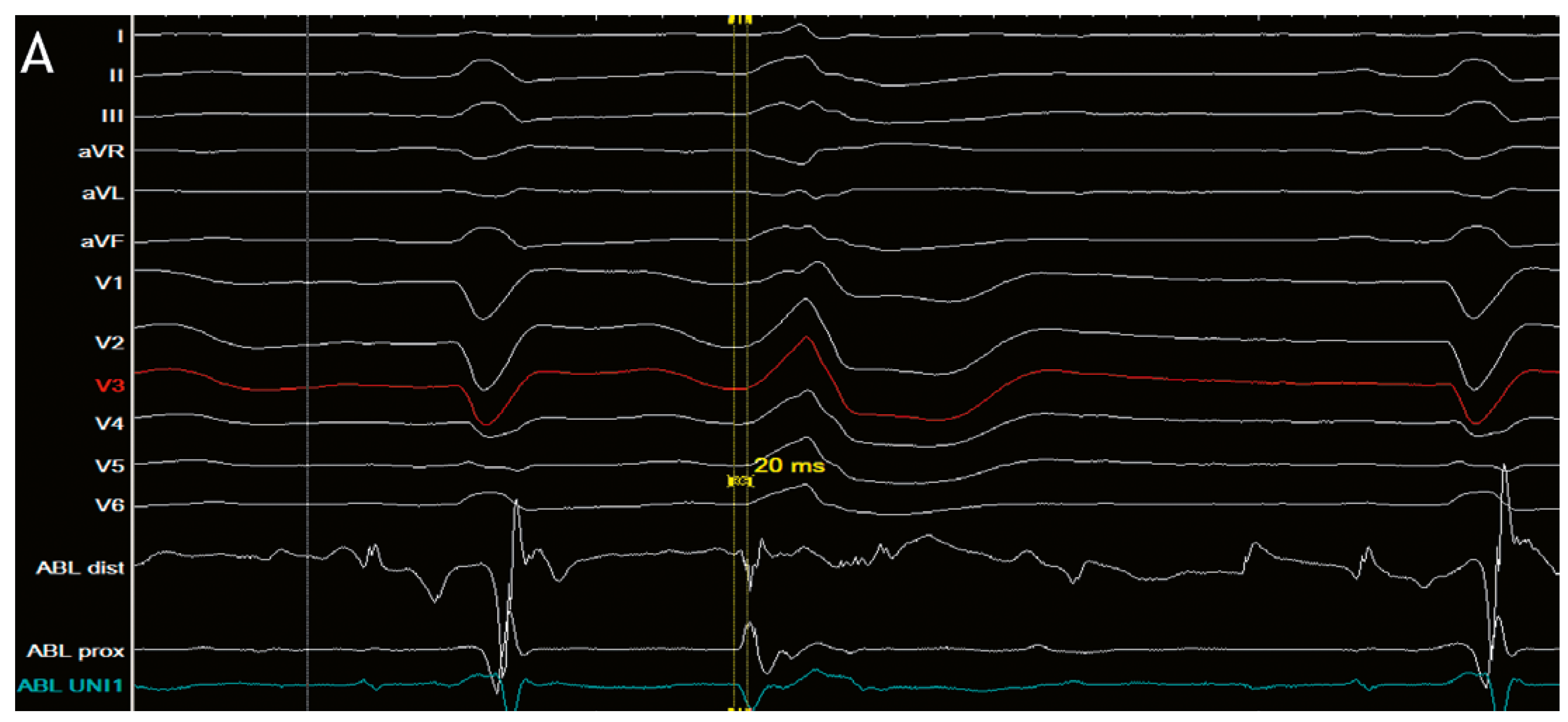
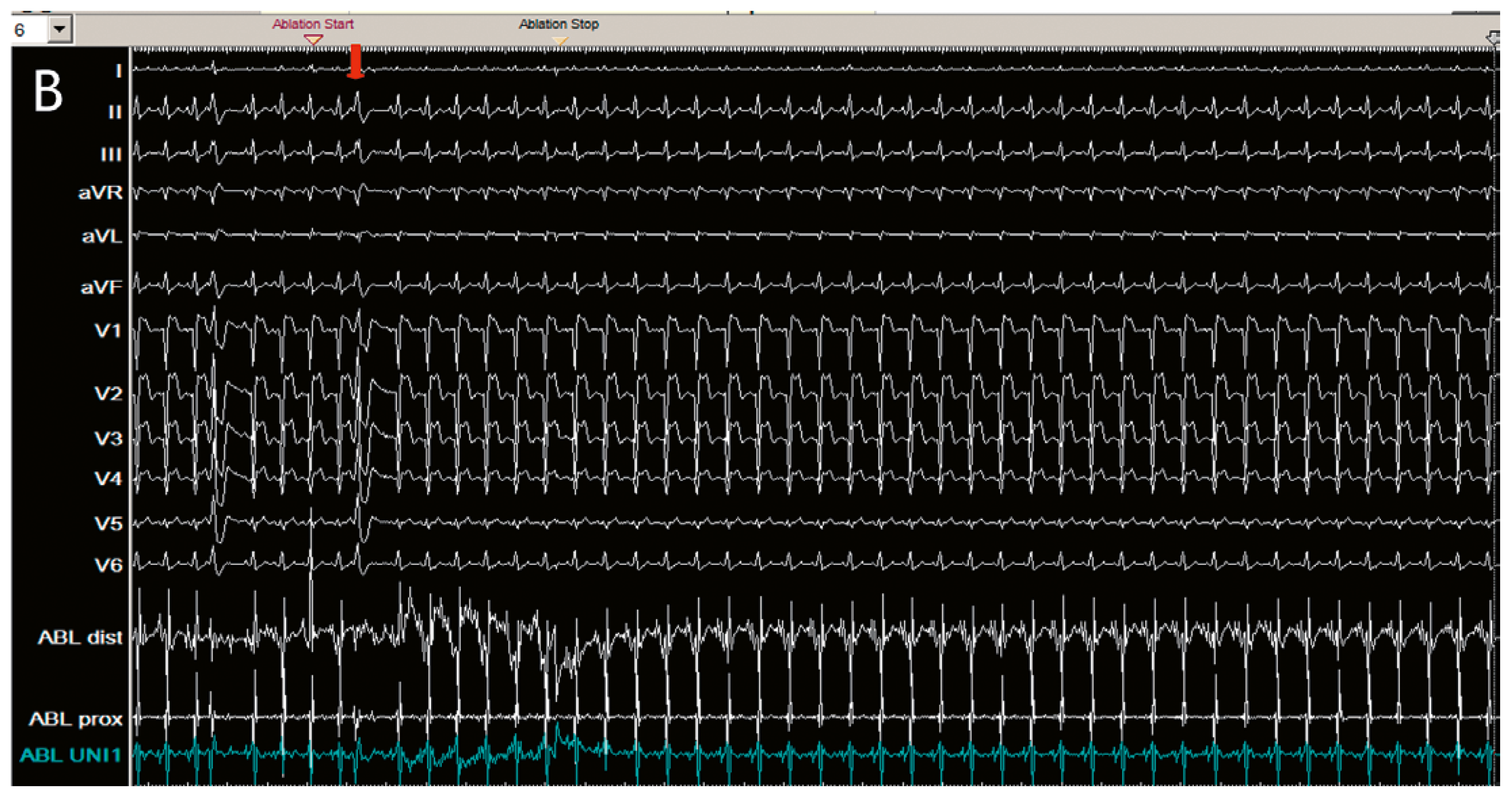
Clinical case
Conclusions
Disclosure statement
References
- Ouyang, F.; Mathew, S.; Wu, S.; Kamioka, M.; Metzner, A.; Xue, Y.; et al. Ventricular Arrhythmias Arising from the Leh Ventricular Outflow Tract Below the Aortic Sinus Cusps. Arrhythm Electrophysiol. 2014, 7, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Prystowsky, E.N.; Padanilam, B.J.; Joshi, S.; Fogel, R.I. Ventricular arrhythmias in the absence of structural heart disease J Am Coll Cardiol. 2012, 59, 1733–1744.
- Yokokawa, M.; Good, E.; Desjardins, B.; Crawford, T.; Jongnarangsin, K.; Chugh, A.; et al. Predictors of successful catheter ablation of ventricular arrhythmias arising from the papillary muscles Heart Rhythm. 2010, 7, 1654–1659.
- Crawford, T.; Mueller, G.; Good, E.; Jongnarangsin, K.; Chugh, A.; Pelosi, F.; et al. Ventricular arrhythmias originating from papillary muscles in the right ventricle. Heart Rhythm. 2010, 7, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Haissaguerre, M.; Shah, D.C.; Jaïs, P.; Shoda, M.; Kautzner, J.; Arentz, T.; et al. Role of Purkinje conducting system in triggering of idiopathic ventricular fibrillation. Lancet. 2002, 359, 677–678. [Google Scholar] [CrossRef] [PubMed]
- Haissaguerre, M.; Shoda, M.; Jaïs, P.; Haissaguerre, M.; Shoda, M.; Jaïs, P.; et al. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002, 106, 962–967. [Google Scholar] [CrossRef] [PubMed]
- Bänsch, D.; Oyang, F.; Antz, M.; Arentz, T.; Weber, R.; Val-Mejias, J.E.; et al. Successful catheter ablation of electrical storm aher myocardial infarction. Circulation. 2003, 108, 3011–3016. [Google Scholar] [CrossRef] [PubMed]
- Szumowski, L.; Sanders, P.; Walczak, F.; Hocini, M.; Jais, P.; Kepski, R.; et al. Mapping and ablation of polymorphic ventricular tachycardia ahermyocardial infarction. J Am Coll Cardiol 2004, 44, 1700–1706. [Google Scholar] [CrossRef] [PubMed]
- Haissaguerre, M.; Extramiana, F.; Hocini, M.; Cauchemez, B.; Jais, P.; Cabrera, J.A.; et al. : Mapping and ablation of ventricular fibrillation associated with long-QT and Brugada syndromes. Circulation 2003, 108, 925–928. [Google Scholar] [CrossRef] [PubMed]
- Knecht, S.; Sacher, F.; Wright, M.; Hocini, M.; Nogami, A.; Arentz, T.; et al. Long-term follow-up of idiopathic ventricular fibrillation ablation: a multicenter study. J Am Coll Cardiol. 2009, 54, 522–528. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Molitor, N.; Breitenstein, A.; Saguner, A.M. Eliminating the Trigger for Polymorphic Ventricular Tachycardia. Cardiovasc. Med. 2018, 21, 255. https://doi.org/10.4414/cvm.2018.00584
Molitor N, Breitenstein A, Saguner AM. Eliminating the Trigger for Polymorphic Ventricular Tachycardia. Cardiovascular Medicine. 2018; 21(10):255. https://doi.org/10.4414/cvm.2018.00584
Chicago/Turabian StyleMolitor, Nadina, Alexander Breitenstein, and Ardan M. Saguner. 2018. "Eliminating the Trigger for Polymorphic Ventricular Tachycardia" Cardiovascular Medicine 21, no. 10: 255. https://doi.org/10.4414/cvm.2018.00584
APA StyleMolitor, N., Breitenstein, A., & Saguner, A. M. (2018). Eliminating the Trigger for Polymorphic Ventricular Tachycardia. Cardiovascular Medicine, 21(10), 255. https://doi.org/10.4414/cvm.2018.00584



