An Unusual Case of Upper Rate Behaviour
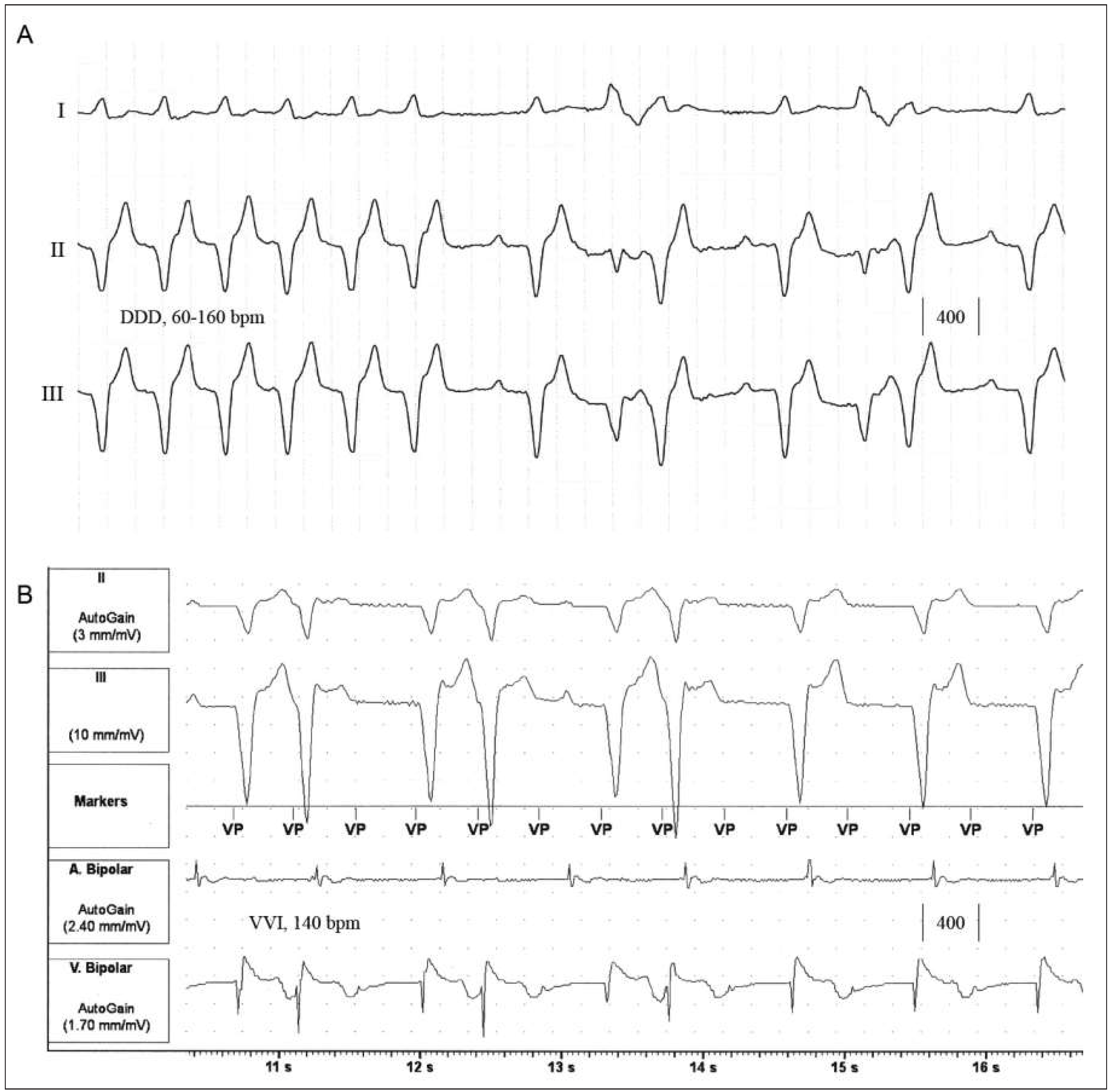
Case report
Discussion
Disclosure statement
Author Contribution
References
- Furman, S. Dual chamber pacemakers: upper rate behavior. Pacing Clin Electrophysiol. 1985, 8, 197–214. [Google Scholar] [CrossRef] [PubMed]
- Poon, K.; Young, C.; Vakulenko, M.; Gupta, N. Runaway pacemaker protection-or a problem? Heart Rhythm. 2013, 10, 1732–1734. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Müggler, S.A.; Mutter, M.; Müller-Burri, S.A. An Unusual Case of Upper Rate Behaviour. Cardiovasc. Med. 2016, 19, 134. https://doi.org/10.4414/cvm.2016.00414
Müggler SA, Mutter M, Müller-Burri SA. An Unusual Case of Upper Rate Behaviour. Cardiovascular Medicine. 2016; 19(4):134. https://doi.org/10.4414/cvm.2016.00414
Chicago/Turabian StyleMüggler, Simon Andreas, Michael Mutter, and Stephan Andreas Müller-Burri. 2016. "An Unusual Case of Upper Rate Behaviour" Cardiovascular Medicine 19, no. 4: 134. https://doi.org/10.4414/cvm.2016.00414
APA StyleMüggler, S. A., Mutter, M., & Müller-Burri, S. A. (2016). An Unusual Case of Upper Rate Behaviour. Cardiovascular Medicine, 19(4), 134. https://doi.org/10.4414/cvm.2016.00414



