Atrioventricular Nodal Reentrant Tachycardia After Heart Transplant
Abstract
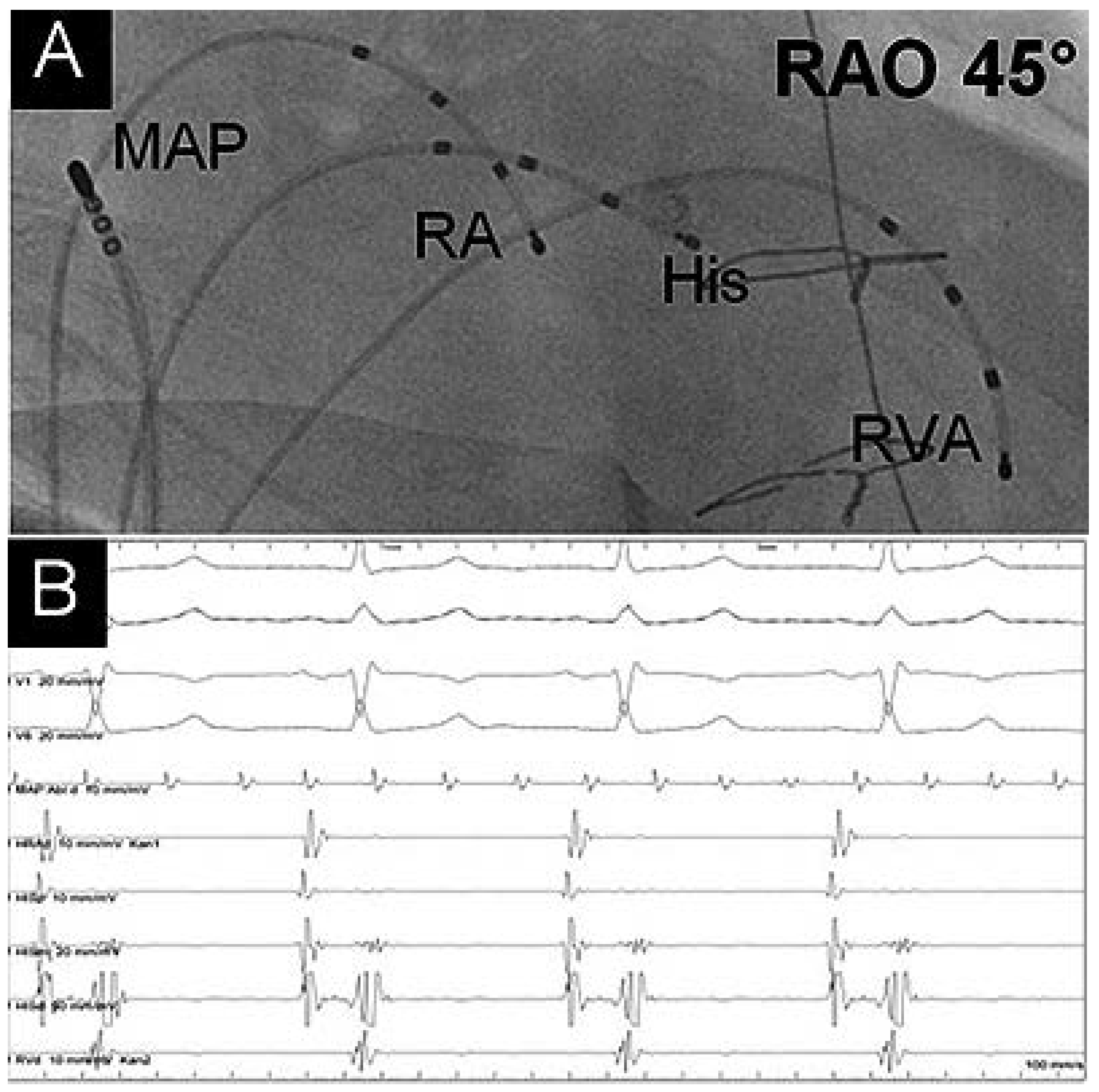
Case Report
Disclosure Statement
References
- Vaseghi, M.; Boyle, N.G.; Kedia, R.; Patel, J.K.; Cesario, D.A.; Wiener, I.; et al. Supraventricular Tachycardia Aher Orthotopic Cardiac Transplantation. J. Am. Coll. Cardiol. 2008, 51, 2241–2249. [Google Scholar] [CrossRef] [PubMed]
- Nof, E.; Stevenson, W.G.; Epstein, L.M.; Tedrow, U.B.; Koplan, B.A. Catheter ablation of atrial arrhythmias after cardiac transplantation: Findings at EP study utility of 3-D mapping and outcomes. J. Cardiovasc. Electrophysiol. 2013, 24, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Elsik, M.; Teh, A.; Ling, L.H.; Virdee, M.; Parameshwar, J.; Fynn, S.P.; Kistler, P.M. Supraventricular arrhythmias late after orthotopic cardiac transplantation: Electrocardiographic and electrophysiological characterization and radiofrequency ablation. Europace 2012, 14, 1498–1505. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.X.; Sun, H. Case Report: Radiofrequency Catheter Ablation of Atrioventricular Nodal Reentrant Tachycardia in a Patient with Heart Transplantation. J. Interv. Card. Electrophysiol. 1997, 2, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Ellenbogen, K.A.; Thames, M.D.; DiMarco, J.P.; Sheehan, H.; Lerman, B.B. Electrophysiological e ects of adenosine in the transplanted human heart. Evidence of supersensitivity. Circulation 1990, 81, 821–828. [Google Scholar] [CrossRef] [PubMed]

© 2016 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Sabti, Z.; Pfister, O.; Reichlin, T. Atrioventricular Nodal Reentrant Tachycardia After Heart Transplant. Cardiovasc. Med. 2016, 19, 332. https://doi.org/10.4414/cvm.2016.00440
Sabti Z, Pfister O, Reichlin T. Atrioventricular Nodal Reentrant Tachycardia After Heart Transplant. Cardiovascular Medicine. 2016; 19(12):332. https://doi.org/10.4414/cvm.2016.00440
Chicago/Turabian StyleSabti, Zaid, Otmar Pfister, and Tobias Reichlin. 2016. "Atrioventricular Nodal Reentrant Tachycardia After Heart Transplant" Cardiovascular Medicine 19, no. 12: 332. https://doi.org/10.4414/cvm.2016.00440
APA StyleSabti, Z., Pfister, O., & Reichlin, T. (2016). Atrioventricular Nodal Reentrant Tachycardia After Heart Transplant. Cardiovascular Medicine, 19(12), 332. https://doi.org/10.4414/cvm.2016.00440



