Preparticipation Screening of Elite and Recreational Athletes
Abstract
Introduction
Incidence of sudden cardiac death
Aetiology of sudden cardiac death
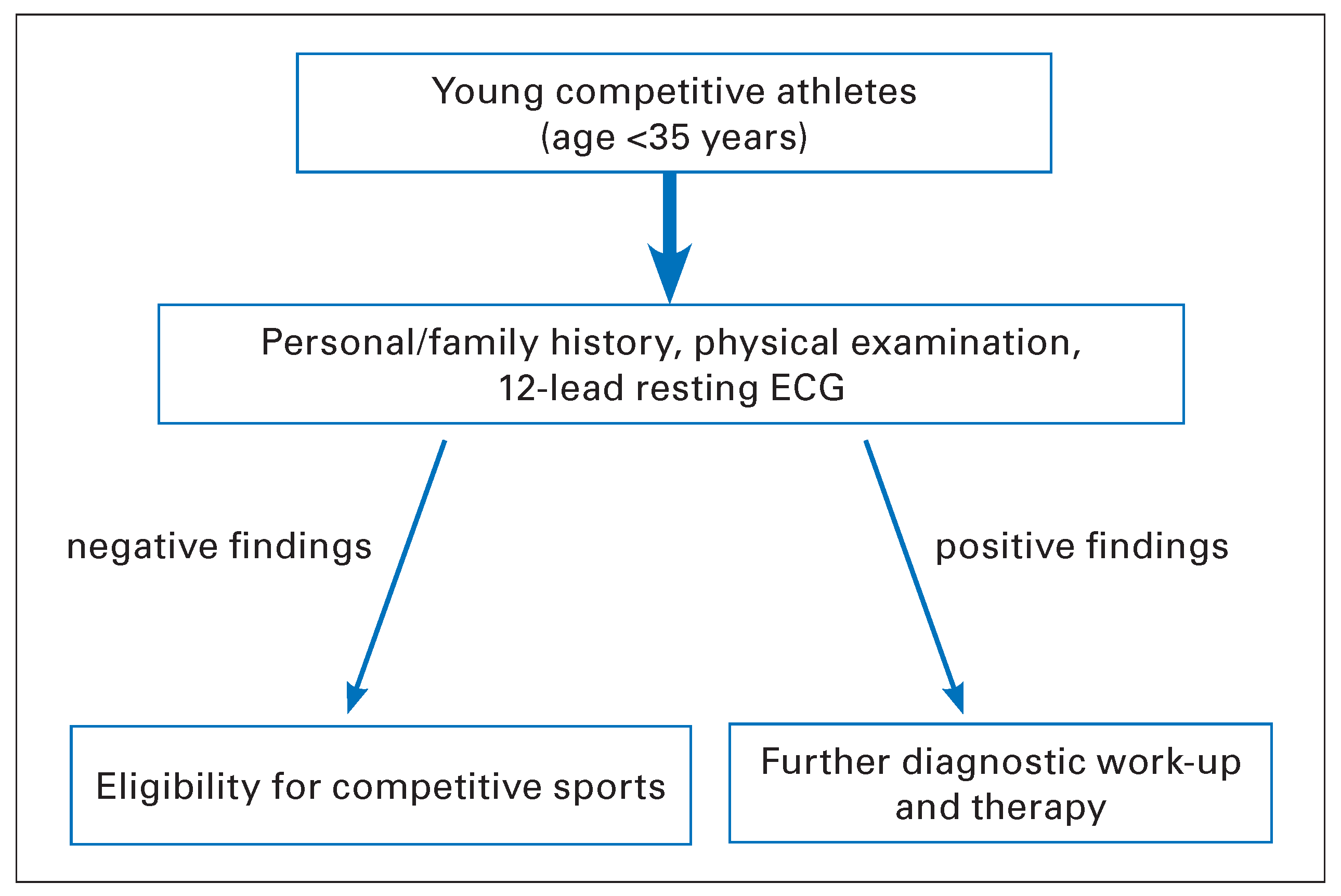
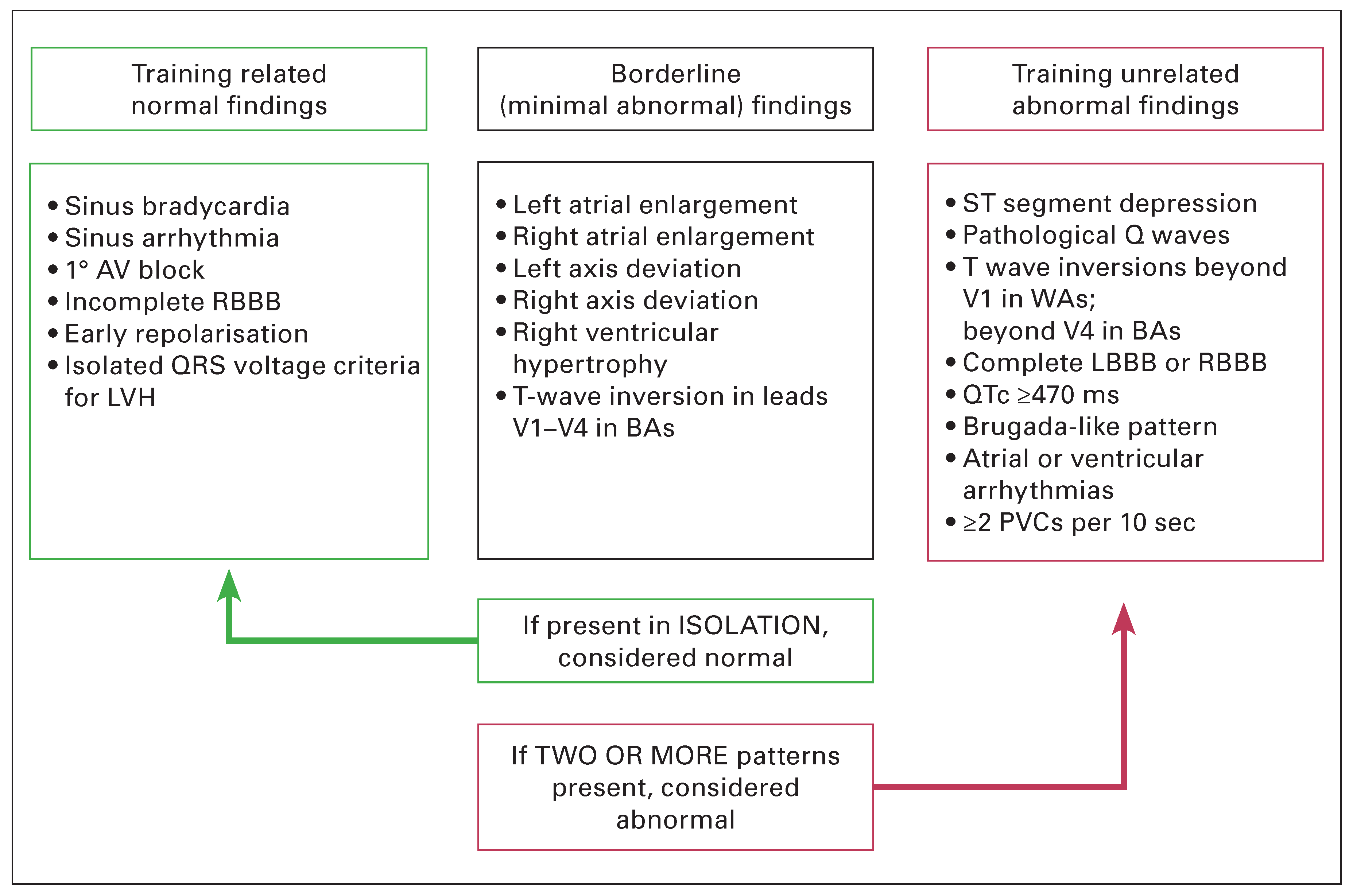
Cardiovascular screening
Conclusions
Conflicts of Interest
Abbreviations
| AED | automated external defibrillator |
| AHA | American Heart Association |
| ARVC | arrhythmogenic right ventricular cardiomyopathy |
| CAA | coronary artery anomaly |
| CAD | coronary artery disease |
| CPR | cardiopulmonary resuscitation |
| ECG | electrocardiogram |
| ESC | European Society of Cardiology |
| PPS | preparticipation screening |
| SCA | sudden cardiac arrest |
| SCD | sudden cardiac death |
| SrSCD | sports-related sudden cardiac death |
References
- Thompson, P.D.; Buchner, D.; Pina, I.L.; Balady, G.J.; Williams, M.A.; Marcus, B.H.; et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: A statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 2003, 107, 3109–3116. [Google Scholar][Green Version]
- De Backer, G.; Ambrosioni, E.; Borch-Johnsen, K.; Brotons, C.; Cifkova, R.; Dallongeville, J.; et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2003, 24, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Nocon, M.; Hiemann, T.; Muller-Riemenschneider, F.; Thalau, F.; Roll, S.; Willich, S.N. Association of physical activity with all-cause and cardiovascular mortality: A systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008, 15, 239–246. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081–1093. [Google Scholar] [CrossRef]
- Corrado, D.; Basso, C.; Rizzoli, G.; Schiavon, M.; Thiene, G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003, 42, 1959–1963. [Google Scholar] [CrossRef]
- Bille, K.; Figueiras, D.; Schamasch, P.; Kappenberger, L.; Brenner, J.I.; Meijboom, F.J.; et al. Sudden cardiac death in athletes: The Lausanne Recommendations. Eur J Cardiovasc Prev Rehabil. 2006, 13, 859–875. [Google Scholar] [CrossRef]
- Borjesson, M.; Pelliccia, A. Incidence and aetiology of sudden cardiac death in young athletes: An international perspective. Br J Sports Med. 2009, 43, 644–648. [Google Scholar] [CrossRef]
- Chugh, S.S.; Weiss, J.B. Sudden Cardiac Death in the Older Athlete. J Am Coll Cardiol. 2015, 65, 493–502. [Google Scholar] [CrossRef]
- Bohm, P.; Kastner, A.; Meyer, T. Sudden cardiac death in football. J Sports Sci. 2013, 31, 1451–1459. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; Blair, S.N.; Corrado, D.; Estes, N.A., 3rd; et al. Exercise and acute cardiovascular events placing the risks into perspective: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation 2007, 115, 2358–2368. [Google Scholar] [PubMed]
- Corrado, D.; Migliore, F.; Basso, C.; Thiene, G. Exercise and the risk of sudden cardiac death. Herz 2006, 31, 553–558. [Google Scholar] [CrossRef]
- Schmied, C.; Borjesson, M. Sudden cardiac death in athletes. J Intern Med. 2014, 275, 93–103. [Google Scholar] [CrossRef]
- Harmon, K.G.; Drezner, J.A.; Wilson, M.G.; Sharma, S. Incidence of sudden cardiac death in athletes: A state-of-the-art review. Heart. 2014, 100, 1227–1234. [Google Scholar] [CrossRef]
- Maron, B.J.; Doerer, J.J.; Haas, T.S.; Tierney, D.M.; Mueller, F.O. Sudden deaths in young competitive athletes: Analysis of 1866 deaths in the United States, 1980–2006. Circulation 2009, 119, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Malhotra, R.; Chiampas, G.; d’Hemecourt, P.; Troyanos, C.; Cianca, J.; et al. Cardiac arrest during long-distance running races. N Engl J Med. 2012, 366, 130–140. [Google Scholar] [CrossRef]
- Harmon, K.G.; Asif, I.M.; Klossner, D.; Drezner, J.A. Incidence of sudden cardiac death in national collegiate athletic association athletes. Circulation 2011, 123, 1594–1600. [Google Scholar] [CrossRef] [PubMed]
- Eckart, R.E.; Scoville, S.L.; Campbell, C.L.; Shry, E.A.; Stajduhar, K.C.; Potter, R.N.; et al. Sudden death in young adults: A 25-year review of autopsies in military recruits. Ann Intern Med. 2004, 141, 829–834. [Google Scholar] [CrossRef]
- Marijon, E.; Tafflet, M.; Celermajer, D.S.; Dumas, F.; Perier, M.C.; Mustafic, H.; et al. Sports-related sudden death in the general population. Circulation 2011, 124, 672–681. [Google Scholar] [CrossRef]
- Maron, B.J. Sudden death in young athletes. N Engl J Med. 2003, 349, 1064–1075. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Basso, C.; Schiavon, M.; Thiene, G. Screening for hypertrophic cardiomyopathy in young athletes. N Engl J Med. 1998, 339, 364–369. [Google Scholar] [CrossRef]
- Corrado, D.; Basso, C.; Thiene, G. Essay: Sudden death in young athletes. Lancet 2005, 366 (Suppl. 1), S47–S48. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Basso, C.; Pavei, A.; Michieli, P.; Schiavon, M.; Thiene, G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 2006, 296, 1593–1601. [Google Scholar] [CrossRef] [PubMed]
- Winkel, B.G.; Risgaard, B.; Sadjadieh, G.; Bundgaard, H.; Haunso, S.; Tfelt-Hansen, J. Sudden cardiac death in children (1–18 years): Symptoms and causes of death in a nationwide setting. Eur Heart J. 2014, 35, 868–875. [Google Scholar] [CrossRef]
- Corrado, D.; Schmied, C.; Basso, C.; Borjesson, M.; Schiavon, M.; Pelliccia, A.; et al. Risk of sports: Do we need a pre-participation screening for competitive and leisure athletes? Eur Heart J. 2011, 32, 934–944. [Google Scholar] [CrossRef]
- Waller, B.F.; Roberts, W.C. Sudden death while running in conditioned runners aged 40 years or over. Am J Cardiol. 1980, 45, 1292–1300. [Google Scholar] [CrossRef]
- Suarez-Mier, M.P.; Aguilera, B.; Mosquera, R.M.; Sanchez-de-Leon, M.S. Pathology of sudden death during recreational sports in Spain. Forensic Sci Int. 2013, 226, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Meyer, L.; Stubbs, B.; Fahrenbruch, C.; Maeda, C.; Harmon, K.; Eisenberg, M.; et al. Incidence, causes, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults 0 to 35 years of age: A 30-year review. Circulation 2012, 126, 1363–1372. [Google Scholar] [CrossRef]
- Solberg, E.E.; Gjertsen, F.; Haugstad, E.; Kolsrud, L. Sudden death in sports among young adults in Norway. Eur J Cardiovasc Prev Rehabil. 2010, 17, 337–341. [Google Scholar] [CrossRef]
- Corrado, D.; Pelliccia, A.; Bjornstad, H.H.; Vanhees, L.; Biffi, A.; Borjesson, M.; et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: Proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005, 26, 516–524. [Google Scholar]
- Ljungqvist, A.; Jenoure, P.; Engebretsen, L.; Alonso, J.M.; Bahr, R.; Clough, A.; et al. The International Olympic Committee (IOC) Consensus Statement on periodic health evaluation of elite athletes March 2009. Br J Sports Med. 2009, 43, 631–643. [Google Scholar] [CrossRef]
- Maron, B.J.; Thompson, P.D.; Ackerman, M.J.; Balady, G.; Berger, S.; Cohen, D.; et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: Endorsed by the American College of Cardiology Foundation. Circulation 2007, 115, 1643–1655. [Google Scholar]
- Marcus, F.I. Electrocardiographic features of inherited diseases that predispose to the development of cardiac arrhythmias, long QT syndrome, arrhythmogenic right ventricular cardiomyopathy/dysplasia, and Brugada syndrome. J Electrocardiol. 2000, 33 (Suppl. 1), 1–10. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J. Hypertrophic cardiomyopathy: A systematic review. JAMA 2002, 287, 1308–1320. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J.; Pelliccia, A.; Spirito, P. Cardiac disease in young trained athletes. Insights into methods for distinguishing athlete’s heart from structural heart disease, with particular emphasis on hypertrophic cardiomyopathy. Circulation 1995, 91, 1596–1601. [Google Scholar] [CrossRef]
- Papadakis, M.; Sharma, S. Electrocardiographic screening in athletes: The time is now for universal screening. Br J Sports Med. 2009, 43, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Pelliccia, A.; Heidbuchel, H.; Sharma, S.; Link, M.; Basso, C.; et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J. 2010, 31, 243–259. [Google Scholar] [CrossRef]
- Drezner, J.A.; Ackerman, M.J.; Anderson, J.; Ashley, E.; Asplund, C.A.; Baggish, A.L.; et al. Electrocardiographic interpretation in athletes: The ‘Seattle criteria’. Br J Sports Med. 2013, 47, 122–124. [Google Scholar] [CrossRef]
- Brosnan, M.; La Gerche, A.; Kalman, J.; Lo, W.; Fallon, K.; MacIsaac, A.; et al. The Seattle Criteria increase the specificity of preparticipation ECG screening among elite athletes. Br J Sports Med. 2014, 48, 1144–1150. [Google Scholar] [CrossRef]
- Sheikh, N.; Papadakis, M.; Ghani, S.; Zaidi, A.; Gati, S.; Adami, P.E.; et al. Comparison of electrocardiographic criteria for the detection of cardiac abnormalities in elite black and white athletes. Circulation 2014, 129, 1637–1649. [Google Scholar] [CrossRef]
- Chandra, N.; Bastiaenen, R.; Papadakis, M.; Panoulas, V.F.; Ghani, S.; Duschl, J.; et al. Prevalence of electrocardiographic anomalies in young individuals: Relevance to a nationwide cardiac screening program. J Am Coll Cardiol. 2014, 63, 2028–2034. [Google Scholar] [CrossRef]
- Riding, N.R.; Sheikh, N.; Adamuz, C.; Watt, V.; Farooq, A.; Whyte, G.P.; et al. Comparison of three current sets of electrocardiographic interpretation criteria for use in screening athletes. Heart 2015, 101, 384–390. [Google Scholar] [CrossRef]
- Borjesson, M.; Urhausen, A.; Kouidi, E.; Dugmore, D.; Sharma, S.; Halle, M.; et al. Cardiovascular evaluation of middle-aged/ senior individuals engaged in leisure-time sport activities: Position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011, 18, 446–458. [Google Scholar] [CrossRef] [PubMed]
- Conroy, R.M.; Pyorala, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Maron, B.J.; Araujo, C.G.; Thompson, P.D.; Fletcher, G.F.; de Luna, A.B.; Fleg, J.L.; et al. Recommendations for preparticipation screening and the assessment of cardiovascular disease in masters athletes: An advisory for healthcare professionals from the working groups of the World Heart Federation, the International Federation of Sports Medicine, and the American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation 2001, 103, 327–334. [Google Scholar]
- Braber, T.L.; Mosterd, A.; Prakken, N.H.; Doevendans, P.A.; Mali, W.P.; Backx, F.J.; et al. Rationale and design of the Measuring Athlete’s Risk of Cardiovascular events (MARC) study: The role of coronary CT in the cardiovascular evaluation of middle-aged sportsmen. Neth Heart J. 2014. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Soar, J.; Zideman, D.A.; Biarent, D.; Bossaert, L.L.; Deakin, C.; et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 2010, 81, 1219–1276. [Google Scholar] [CrossRef] [PubMed]
- Drezner, J.A. Preparing for sudden cardiac arrest--the essential role of automated external defibrillators in athletic medicine: A critical review. Br J Sports Med. 2009, 43, 702–707. [Google Scholar] [CrossRef]
- Dvorak, J.; Kramer, E.B.; Schmied, C.M.; Drezner, J.A.; Zideman, D.; Patricios, J.; et al. The FIFA medical emergency bag and FIFA 11 steps to prevent sudden cardiac death: Setting a global standard and promoting consistent football field emergency care. Br J Sports Med. 2013, 47, 1199–1202. [Google Scholar] [CrossRef]

| Author | Study design | Population | Incidence | Age range (years) | M/F ratio |
|---|---|---|---|---|---|
| Corrado et al. [5] | Prospective | Competitive Italian athletes | 1:43.478 (SCD) | 12–35 | 9.2 |
| Maron et al. [14] | Retrospective | US athletes | 1:163.934 (SCD) | 8–39 | 8.4 |
| Harmon et al. [16] | Retrospective | US college athletes | 1:43.770 (SCD) | 17–23 | 2.3 |
| Eckart et al. [17] | Retrospective | US military recruits | 1:9.000 (SCD) | 18–35 | 11.8 |
| Kim et al. [15] | Prospective | US marathon racers | 1:184.000 (SCA) | 29–55 | 5.6 |
| Marijon et al. [18] | Prospective | General population | 1:217.391 (SCA/D) | 12–75 | 18.1 |
© 2015 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bohm, P.; Meyer, T.; Scharhag, J. Preparticipation Screening of Elite and Recreational Athletes. Cardiovasc. Med. 2015, 18, 306. https://doi.org/10.4414/cvm.2015.00339
Bohm P, Meyer T, Scharhag J. Preparticipation Screening of Elite and Recreational Athletes. Cardiovascular Medicine. 2015; 18(11):306. https://doi.org/10.4414/cvm.2015.00339
Chicago/Turabian StyleBohm, Philipp, Tim Meyer, and Jürgen Scharhag. 2015. "Preparticipation Screening of Elite and Recreational Athletes" Cardiovascular Medicine 18, no. 11: 306. https://doi.org/10.4414/cvm.2015.00339
APA StyleBohm, P., Meyer, T., & Scharhag, J. (2015). Preparticipation Screening of Elite and Recreational Athletes. Cardiovascular Medicine, 18(11), 306. https://doi.org/10.4414/cvm.2015.00339




