The L Wave—A Reminder
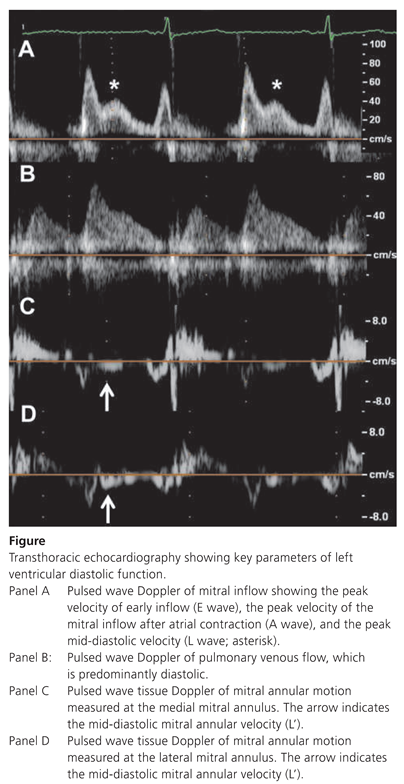
Case report
Comment
Funding/potential competing interests:
References
- Kerut, E.K. The mitral L-wave: a relatively common but ignored useful finding. Echocardiography 2008, 25, 548–550. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.W.; Oh, J.K.; Redfield, M.M.; Ujino, K.; Seward, J.B.; Tajik, A.J. Triphasic mitral inflow velocity with middiastolic filling: Clinical implications and associated echocardiographic findings. J Am Soc Echocardiogr. 2004, 17, 428–431. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.S.; Han, L.; Ha, J.W.; Oh, J.K.; Ling, L.H. The mitral L wave: a marker of pseudonormal filling and predictor of heart failure in patients with left ventricular hypertrophy. J Am Soc Echocardiogr. 2005, 18, 336–341. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Eppinger, N.; Maeder, M.T. The L Wave—A Reminder. Cardiovasc. Med. 2014, 17, 305. https://doi.org/10.4414/cvm.2014.00272
Eppinger N, Maeder MT. The L Wave—A Reminder. Cardiovascular Medicine. 2014; 17(10):305. https://doi.org/10.4414/cvm.2014.00272
Chicago/Turabian StyleEppinger, Nina, and Micha T. Maeder. 2014. "The L Wave—A Reminder" Cardiovascular Medicine 17, no. 10: 305. https://doi.org/10.4414/cvm.2014.00272
APA StyleEppinger, N., & Maeder, M. T. (2014). The L Wave—A Reminder. Cardiovascular Medicine, 17(10), 305. https://doi.org/10.4414/cvm.2014.00272



