Important changes in personnel and organisation
Ernst Lüthy, who had become assistant professor, pushed for a quick expansion of the cardiovascular division of the Policlinic and requested more personnel. Paul Rossier, chief of the Medical Clinic and near retirement, strongly opposed this request, which created tension between him and Hegglin. When Lüthy met more opposition and also fell out openly with Hegglin, he reoriented his career and took a post in the Basel pharmaceutical industry. Finally on November 22, 1969, in the morning of Rutishauser’s lecture for his habilitation as privat-docent, Hegglin died suddenly, and his presentation began with “Our highly admired chef is no more”. Rudolf Amman became interim head of the Medical Policlinic.
After Rossier’s retirement the government created a Medical Department with three directors: Paul Frick, Alexis Labhart and Walter Siegenthaler, all promoted to the rank of full professor. In April 1970 Rutishauser was promoted to be the first extraordinary professor of cardiology and head of the Cardiology Division of this Medical Department in Zurich.
Towards percutaneous vascular therapies
When Rutishauser studied medicine, there was a saying: “Small surgeons make small incisions; great surgeons make big incisions because with more visibility the operation is safer.” The patient was not asked at that time. This has radically changed.
Dilatation of peripheral arteries
The very industrious Andreas Grüntzig started as an assistant in 1969 in Zurich in Bollinger’s Angiology Unit after studies and postgraduate training mainly in Heidelberg. In 1964 Charles Dotter in Oregon had begun dilating stenosed arteries in the thigh, using progressively larger coaxial catheters. Grüntzig saw this procedure applied by Zeitler in a hospital near Cologne and tried it himself in Zurich, first together with Zeitler. Obviously this led to large holes in the access artery. The balloon catheter described in 1963 by Thomas Fogarty was unsuitable for dilating arterial stenoses because it took an hourglass shape when inflated in short stenoses and left them unchanged. Grüntzig tried, on his famous kitchen table, to fix balloons on catheters with side holes and tip occlusion. But only the use of polyvinylchloride–suggested by Prof. Hopff from the ETH–led to balloons which could effectively dilate vascular stenoses. This was an important step forward. Andreas Grüntzig developed good connections with Ms Heliane Canepa who headed a small team at the firm Schneider AG in Bülach. With her collaborators she improved the balloons, made them slimmer and less prone to break under higher pressure. Grüntzig realised that only as a member of the Radiology Department he could carry out his plans. In 1971–1972 he was able to dilate with balloons of Schneider AG more than 200 patients with stenoses of the iliac and femoral arteries in the angiography room of Radiology. Patients to whom an amputation had been proposed because of disturbing claudication were able to walk out of the hospital without pain.
Preparations for the angioplasty of coronary arteries
For Rutishauser, who was in good contact with Grüntzig and Bollinger [
20], the success of the peripheral artery dilatation was a clear signal that balloons could also be used in patients with angina pectoris due to coronary artery stenoses. It was obviously the same disease! Therefore he hired Grüntzig in October 1973 and promoted him in March 1974 to “Oberassistent”, and in August 1974 to “Oberarzt” of the Cardiology Division (
Figure 1). In spite of his pioneering achievements Grüntzig remained in this position nearly until his departure for Atlanta, Georgia when Krayenbühl had become chief of Cardiology in summer 1976.
Grüntzig was a gifted, hardworking colleague with an exceptional ability to grasp and solve problems quickly. It was a pleasure to introduce the angiologist to right, left and transseptal catheterisation of the heart and coronary angiography. With the ultimate goal of dilating coronary vessels in mind, and as former assistant of Radiology, Grüntzig had ready access to the angiography room.
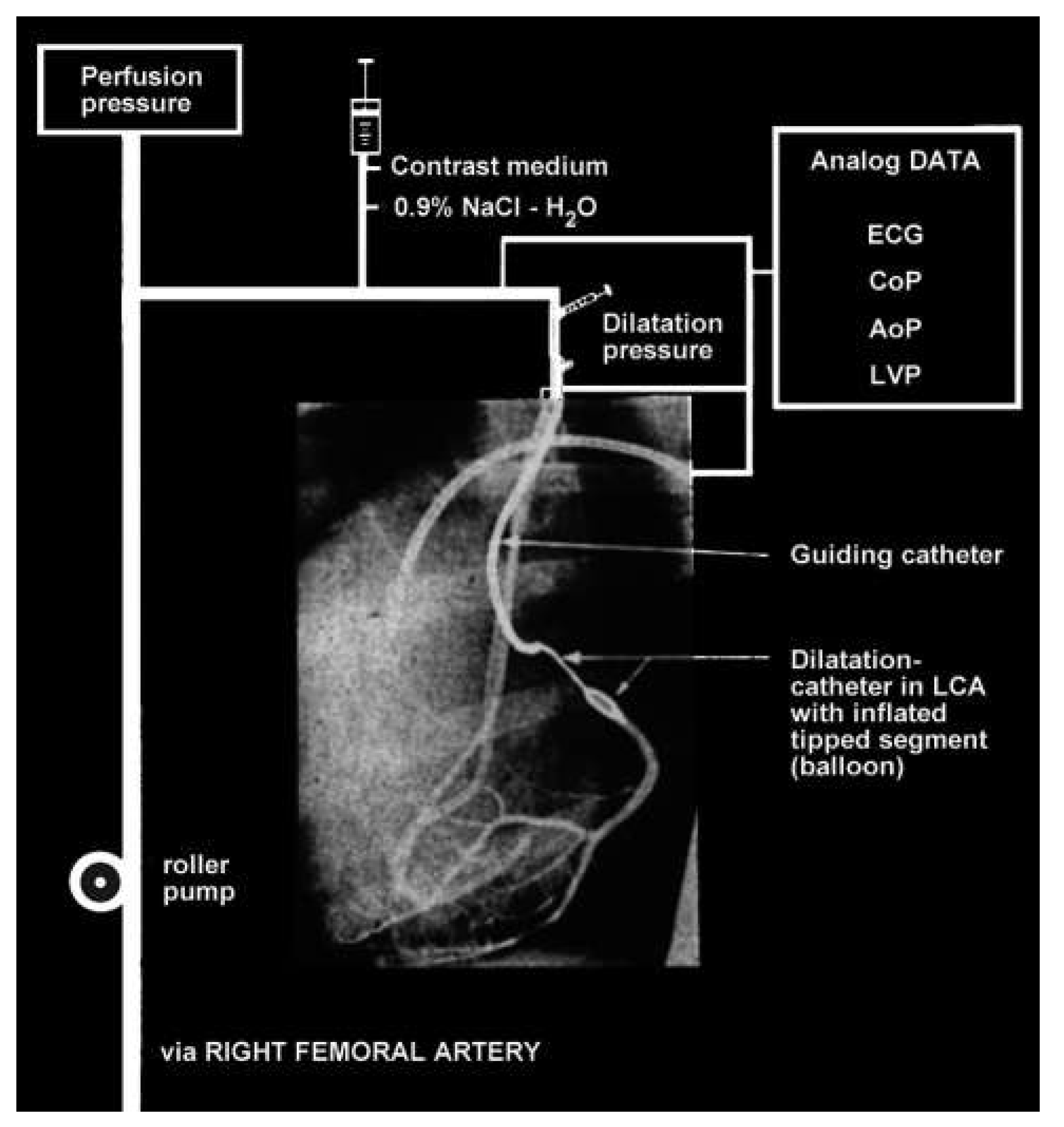
Before the dilatation of coronary arteries could be practised in humans, animal experiments were crucial. Our conscience acted as ethical committee since none existed at that time. Since the threshold for ventricular fibrillation in pigs as experienced by René Lerch was very low and unknown in humans, we did not want to take any risks. After all patients do not die from coronary stenoses, they die from arrhythmias caused by ischaemia. Therefore we asked Schneider AG to manufacture a double lumen balloon catheter permitting blood from the other femoral artery to be pumped through the central lumen into the periphery of the coronary artery during dilatation. We also used intermittently the central lumen for pressure measurements distal to the stenosis before and during dilatation (
Figure 2).
We did acute and chronic experiments in dogs in which Marko Turina had created stenoses with 6–0 silk thread around proximal coronary branches. We presented the results of these percutaneous dilatations of coronary stenoses in dogs at the spring meeting 1976 of the German Society of Kreislaufforschung in Bad Nauheim to an audience which concluded that the application of this technique in humans should be banned. This was more than one year before Andreas Grüntzig presented his often cited abstract at the American Heart Association in fall 1977. Our work was published in the Archives of the “Deutsche Gesellschaft für Kreislaufforschung” in German [
21] (
Figure 2) and, therefore, discovered only later by American cardiologists.
Even if in man with chronic stenoses and collaterals the peripheral perfusion of the coronary arteries during angioplasty proved to be unnecessary, the measurement of the poststenotic pressure is used today to assess the degree of stenoses and the importance of the collateral circulation by the Fractional Flow Reserve (FFR). The actual PCI procedure with stenting is performed today (with exception of John Simpson’s wire published in 1982) using an approach very similar to the one we used in 1975/76.
In Zurich it was impossible for the Cardiology Division to obtain beds (we had to beg for each patient individually), and the head of a subspeciality, as cardiology, could not become full professor. This was completely different at the University of Geneva where Rutishauser was called in April 1976 as ordinary professor, and where the chief of the first Cardiology Centre in Switzerland had 20 beds and was directly responding to the Hospital director.
Rutishauser would have liked to take Grüntzig with him to Geneva, but there was a convincing argument against it: the quality of the angiographic images to visualise fine dilatation catheters was insufficient and replacement needed too much time, while in Zurich we had just obtained new angiography laboratories with optimal Siemens image intensifiers. They were a prerequisite for coronary angioplasty in man, which we felt could soon be realised.
The first coronary angioplasty
Andreas Grüntzig, who “tried the impossible”, was unduly delayed and faced suspicion and many obstacles in Zurich after Rutishauser’s leave. In the USA Richard Myler performed with Grüntzig the first intraoperative dilatation of a coronary artery in a patient who had this vessel bypassed. The fact that Martin Kaltenbach was inclined to try in his laboratory in Frankfurt a coronary dilatation together with Grüntzig increased the pressure on Krayenbühl and Siegenthaler to give the placet for the first coronary angioplasty in Zurich. The only person who then supported Grüntzig was Senning. He said “If something happens, I will operate”.
On September 16, 1977 Grüntzig performed the first and from all points of view successful coronary angioplasty in the anterior descending branch of the left coronary artery in a business man 38 years old–the same age as Grüntzig. The perfusion of the peripheral coronary artery to be dilated was ready but not employed because the distal coronary pressure after the first dilatation was practically the same as the aortic pressure; the coronary stenosis was barely visible and no complication occurred. Grüntzig described the procedure in 1978 [
22]. Before that, the patient and Andreas had initiated the publication of the event, with pictures, in a Swiss tabloid (Schweizer Illustrierte). This incensed those cardiologists who were envious of Grüntzig. A spicy detail is recalled: The abstract that Grüntzig submitted for the spring meeting of the Swiss Society of Cardiology in 1978 was accepted only because Rutishauser, then chairman of the selection committee, had the casting vote against three opposing Swiss University Cardiology chiefs. They expressed doubts about his method of coronary dilatation and blamed Grüntzig for the publication in the Swiss tabloid [
2].
Bernhard Meier was an assistant in Internal Medicine on the ward of Walter Siegenthaler, successor of Hegglin at the Policlinic. In this ward the patient with the first successful angioplasty was hospitalised. Meier witnessed and described in detail the conversations Grüntzig had with the patient on the evening before and what happened during the intervention and the following days. After having completed his training in Internal Medicine Bernhard Meier followed Andreas Grüntzig, who had become professor at Emory University in Atlanta, Georgia in 1980 with Willis Hurst and Spencer King. Bernhard Meier has dedicated his professional life to interventional cardiology. In 1983 he became “Oberarzt”, later privat-docent and “Leitender Arzt” with Rutishauser in the Geneva Cardiology Center, where he organized nine courses in interventional cardiology. In 1992 he was appointed professor and head of Cardiology at the University of Berne and proudly named his clinic Swiss Cardiology Center.
Conclusion
During the years 1970–76, when Rutishauser was in charge of the Cardiology Division of the Medical Department in Zurich, he had many excellent coworkers. A total of 23 were eventually promoted later to the rank of professor.
Also in the future the recruitment of bright young people will be the key for academic medicine. An honest education towards self discipline forms a good foundation and is essential to look forward with confidence in science for innovation. The patient must always stay in the centre in order that these young people become successful clinical investigators and integral cardiologists.
The enormous expansion of the interventional therapy since then, including valves, shunt closure devices, stented grafts, ablations, tissue engineering and other therapies–thought even by internet–went beyond our wildest dreams in 1975 and continues to this day. The instruments became more sophisticated, smaller and with the aid of several imaging methods easier to manipulate from outside the body. The catheter interventions moved from the cardiovascular system to other tubular organs and even to tumour therapy. Today one could state that progress in instrumentation and engineering in certain fields is in competition with and for certain diseases equals or surpasses the progress made in pharmacologic and surgical therapies.