Recurrent Unexplained Syncope in an Adolescent Girl
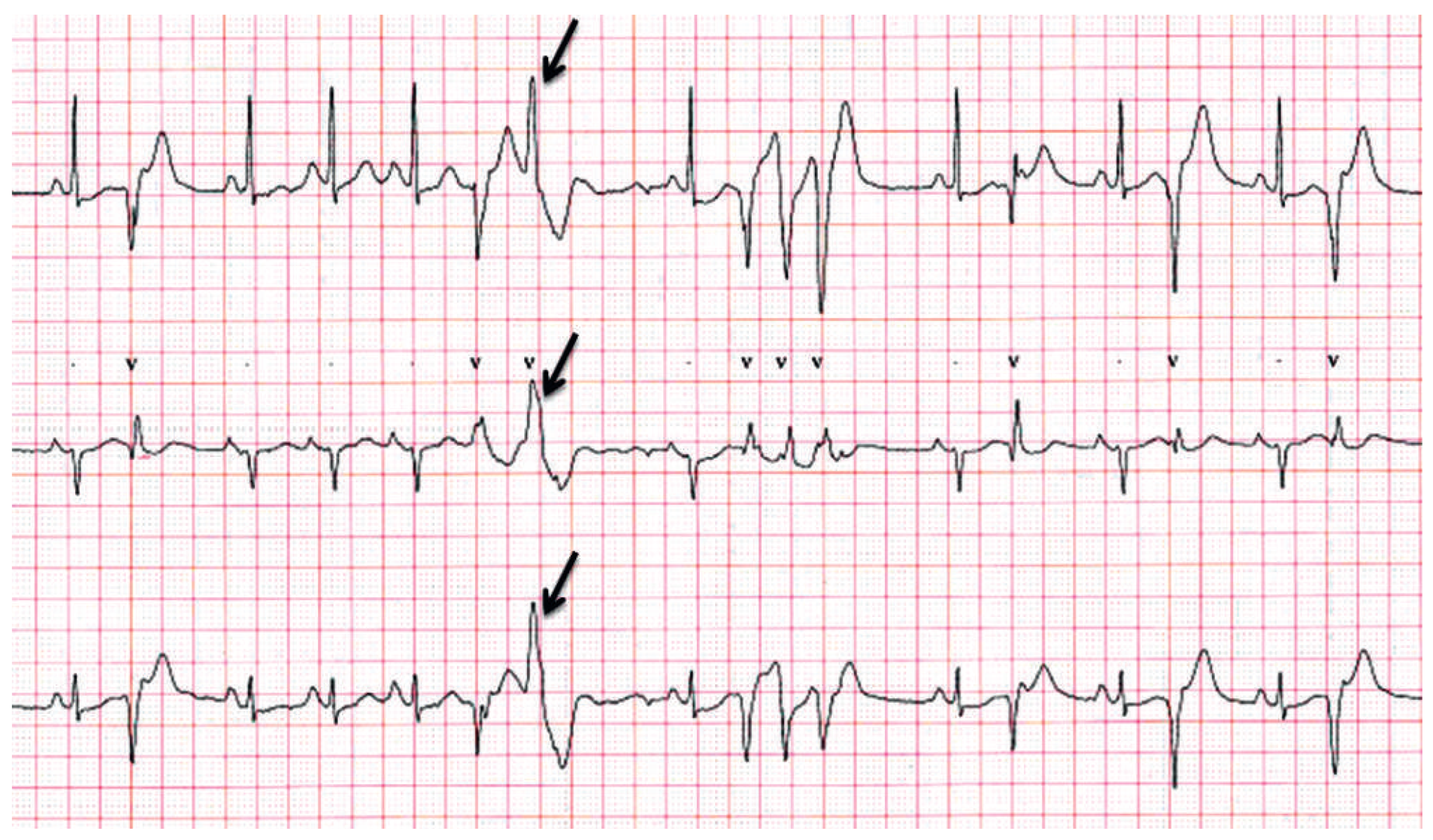
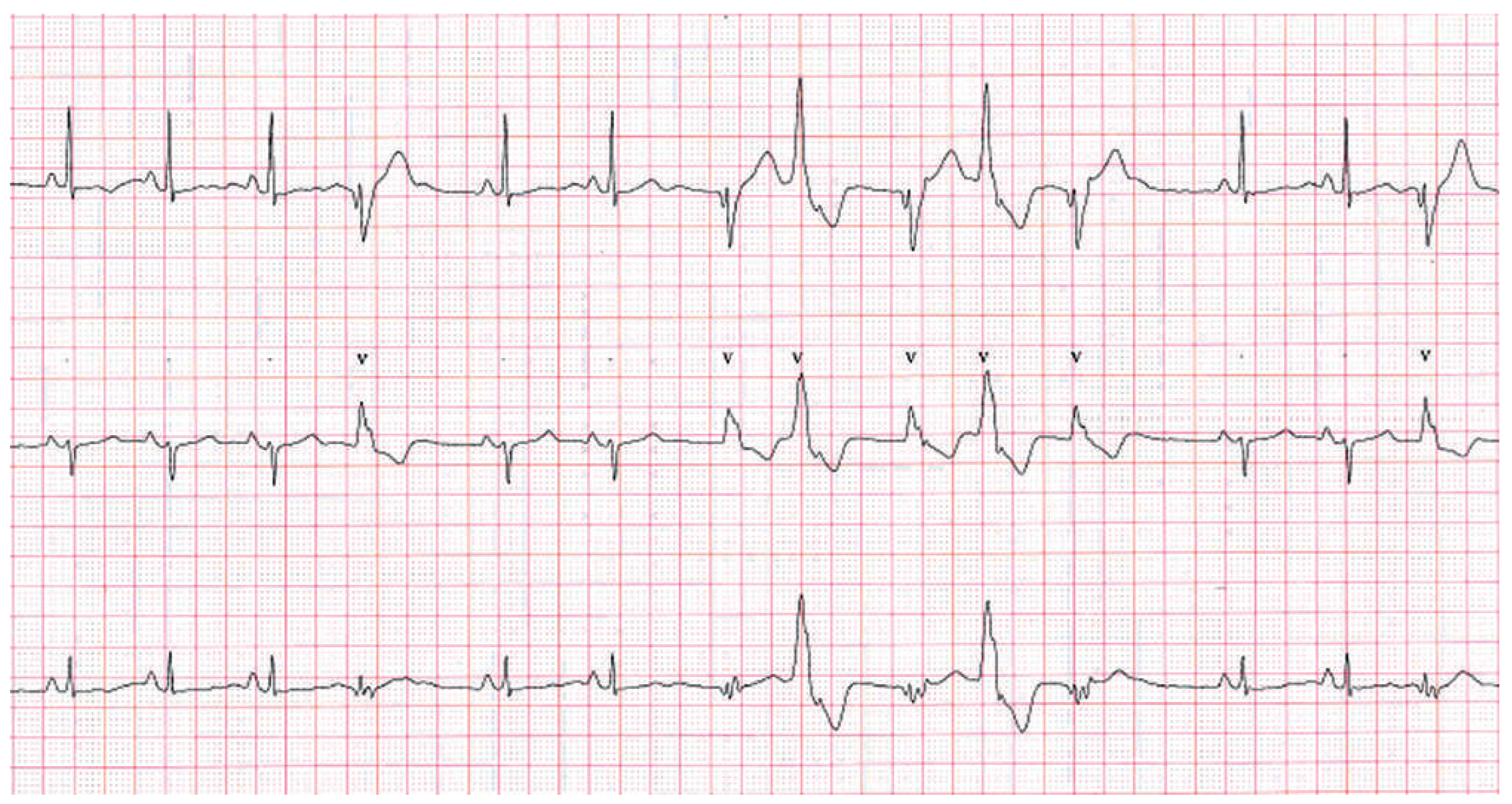
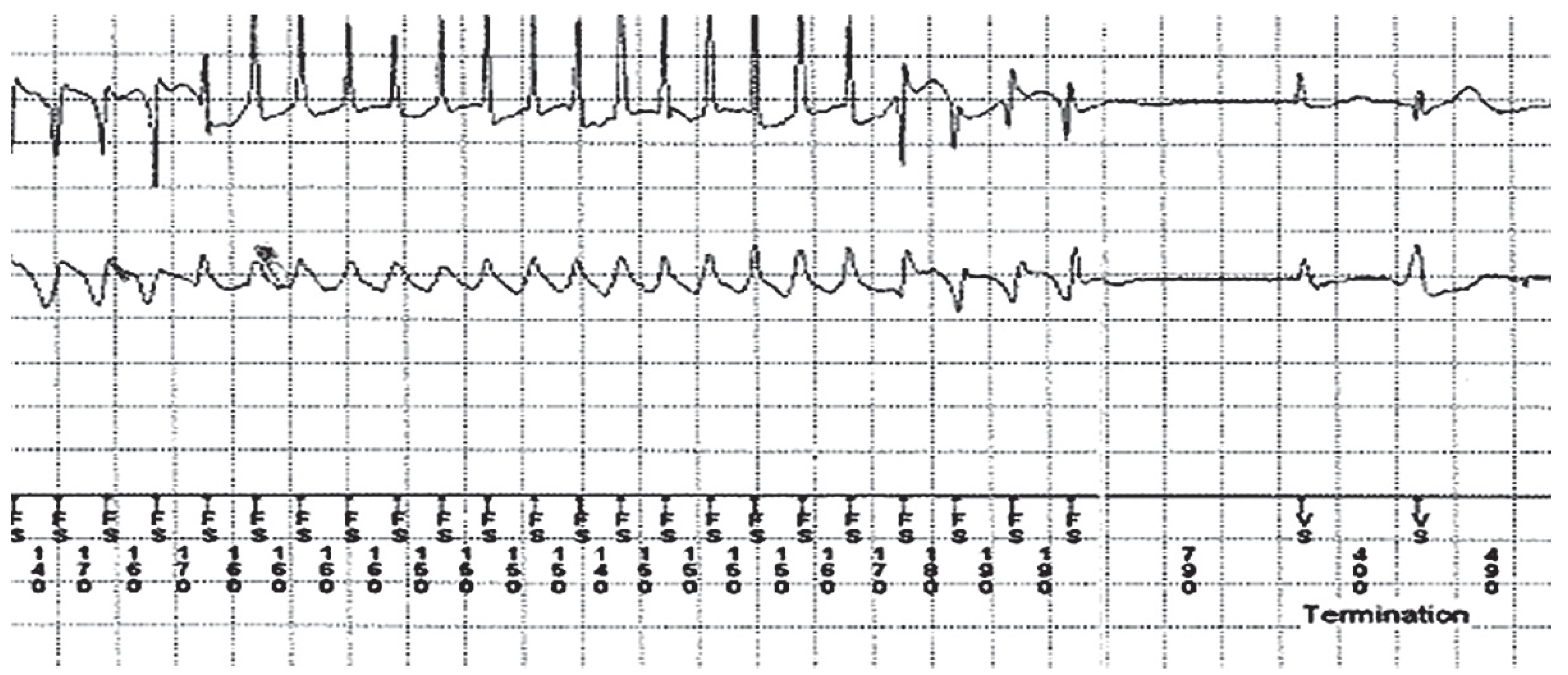
Case presentation
Question
Comments
Funding/potential competing interests:
References
- Hekkala, A.M.; Viitasalo, M.; Vaananen, H.; Swan, H.; Toivonen, L. Abnormal repolarization dynamics revealed in exercise test in long QT syndrome mutation carriers with normal resting QT interval. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2010, 12, 1296–1301. [Google Scholar] [CrossRef] [PubMed]
- Richter, S.; Gebauer, R.; Hindricks, G.; Brugada, P. A classic electrocardiographic manifestation of catecholaminergic polymorphic ventricular tachycardia. J Cardiovasc Electrophysiol. 2012, 23, 560. [Google Scholar] [CrossRef] [PubMed]
- Nam, G.B.; Burashnikov, A.; Antzelevitch, C. Cellular mechanisms underlying the development of catecholaminergic ventricular tachycardia. Circulation. 2005, 111, 2727–2733. [Google Scholar] [CrossRef] [PubMed]
- Van der Werf, C.; Zwinderman, A.H.; Wilde, A.A. Therapeutic approach for patients with catecholaminergic polymorphic ventricular tachycardia: state of the art and future developments. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2012, 14, 175–183. [Google Scholar] [CrossRef]
- Swan, H.; Laitinen, P.; Kontula, K.; Toivonen, L. Calcium channel antagonism reduces exercise-induced ventricular arrhythmias in catecholaminergic polymorphic ventricular tachycardia patients with RyR2 mutations. J Cardiovas Electrophysiol. 2005, 16, 162–166. [Google Scholar] [CrossRef] [PubMed]
- Massin, M.M.; Bourguignont, A.; Coremans, C.; Comte, L.; Lepage, P.; Gerard, P. Syncope in pediatric patients presenting to an emergency department. J Pediatr. 2004, 145, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D.A.; Dhala, A. Syncope in the pediatric patient. The cardiologist’s perspective. Pediatr Clin North Am. 1999, 46, 205–219. [Google Scholar] [CrossRef] [PubMed]


© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Di Bernado, S.; Boulos-Ksontini, T.; Mivelaz, Y.; Sekarski, N.; Pruvot, E. Recurrent Unexplained Syncope in an Adolescent Girl. Cardiovasc. Med. 2014, 17, 27. https://doi.org/10.4414/cvm.2014.00200
Di Bernado S, Boulos-Ksontini T, Mivelaz Y, Sekarski N, Pruvot E. Recurrent Unexplained Syncope in an Adolescent Girl. Cardiovascular Medicine. 2014; 17(1):27. https://doi.org/10.4414/cvm.2014.00200
Chicago/Turabian StyleDi Bernado, Stefano, Tatiana Boulos-Ksontini, Yvan Mivelaz, Niccole Sekarski, and Etienne Pruvot. 2014. "Recurrent Unexplained Syncope in an Adolescent Girl" Cardiovascular Medicine 17, no. 1: 27. https://doi.org/10.4414/cvm.2014.00200
APA StyleDi Bernado, S., Boulos-Ksontini, T., Mivelaz, Y., Sekarski, N., & Pruvot, E. (2014). Recurrent Unexplained Syncope in an Adolescent Girl. Cardiovascular Medicine, 17(1), 27. https://doi.org/10.4414/cvm.2014.00200



