Waiting for Evidence Seems to Make Sense—Except for the One Providing the Evidence
Abstract
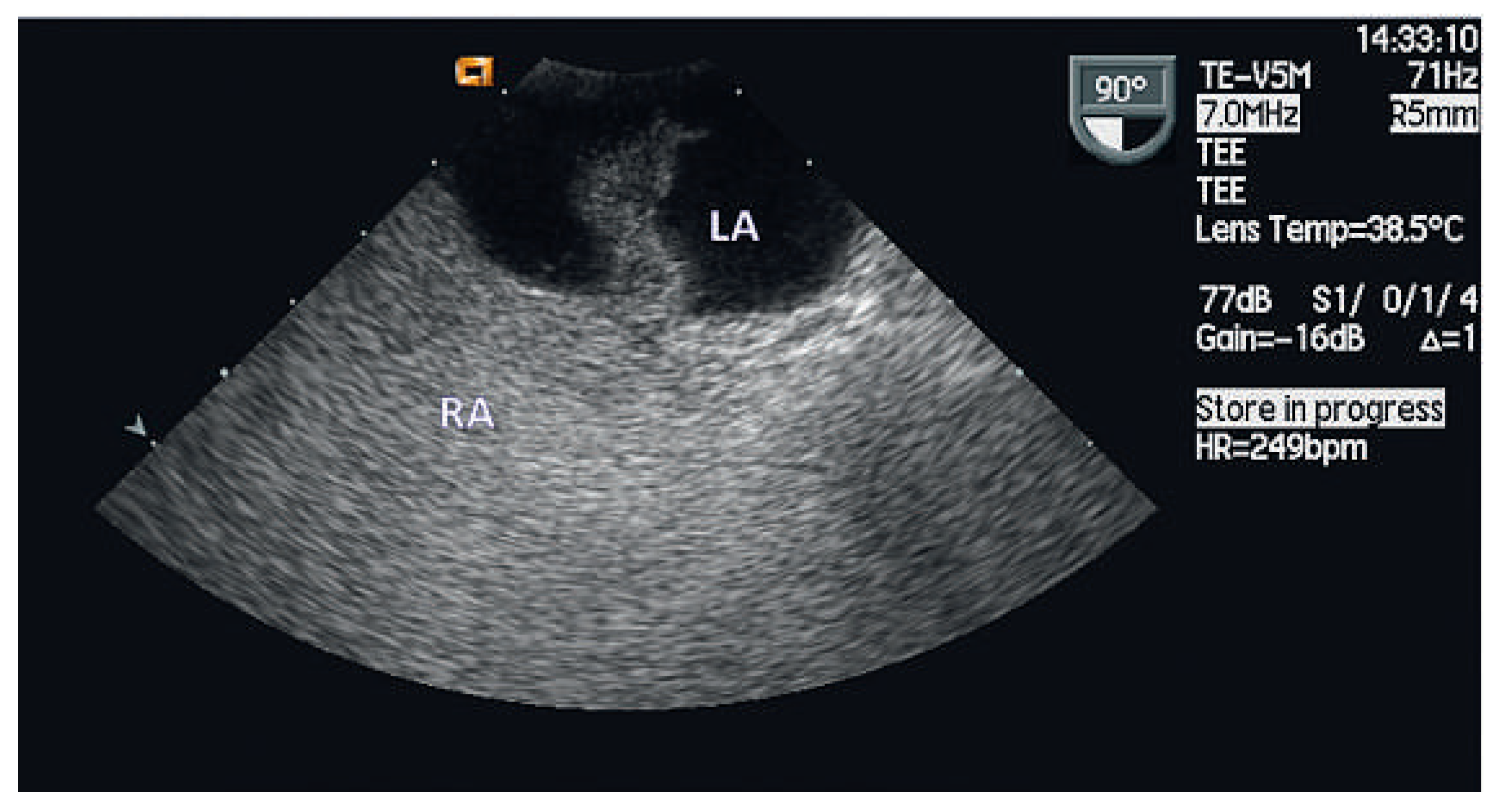
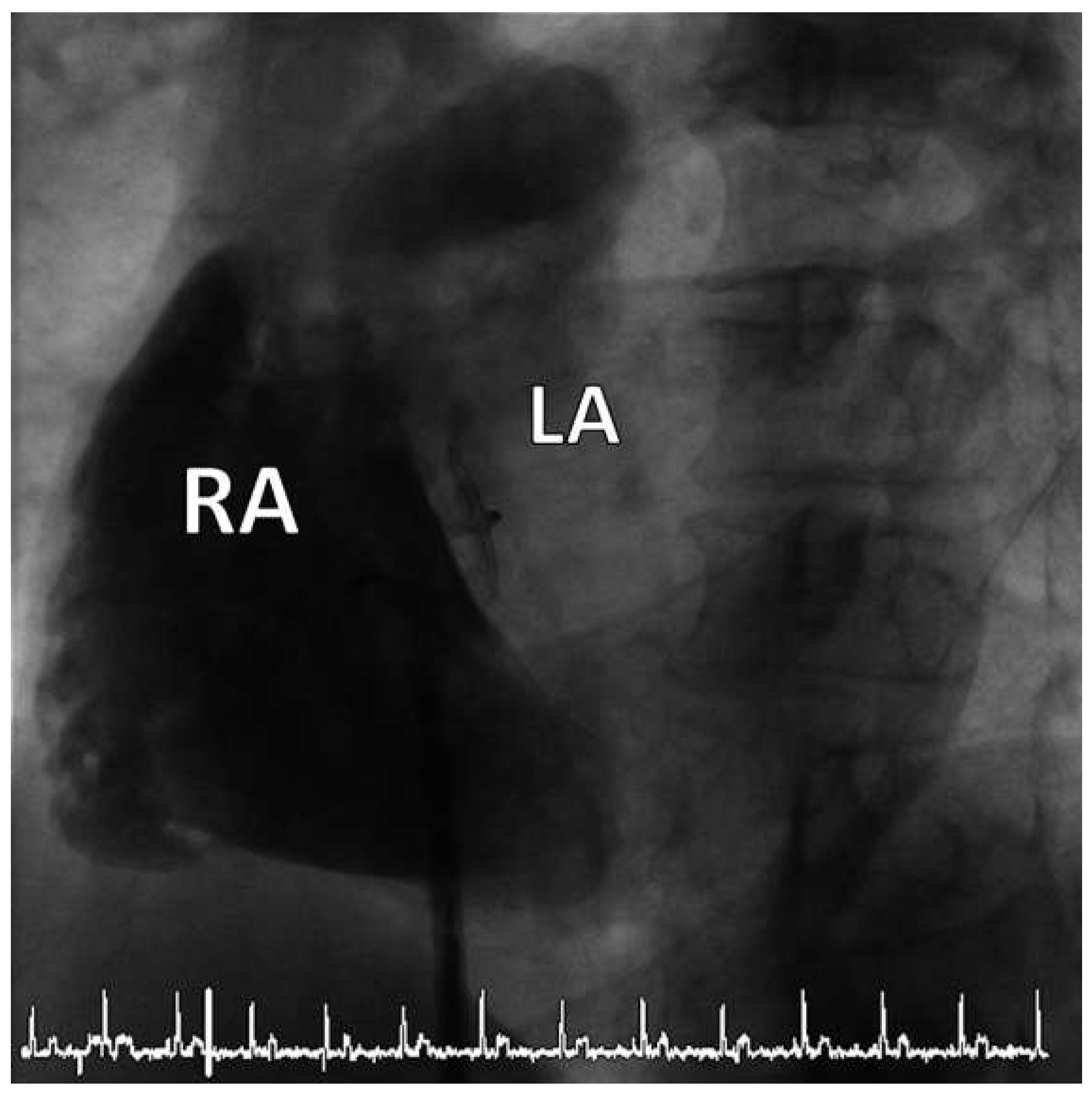
Case report
Discussion
Funding/potential competing interests
References
- Schneider, B.; Zeinkiewicz, T.; Jansen, V.; Hofmann, T.; Noltenius, H.; Meinertz, T. Diagnosis of patent foramen ovale by transesophageal echocardiography and correlation with autopsy findings. Am J Cardiol 1996, 77, 1202–1209. [Google Scholar] [CrossRef] [PubMed]
- Steiner, M.M.; Di Tullio, M.R.; Rundek, T.; Gan, R.; Chen, X.; Liguori, C.; et al. Patent foramen ovale size and embolic brain imaging findings among patinets with ischemic stroke. Stroke 1998, 29, 944–948. [Google Scholar] [CrossRef] [PubMed]
- Sacco, R.L.; Ellenberg, J.H.; Mohr, J.P.; Tatemichi, T.K.; Hier, D.B.; Price, T.R.; et al. Infarcts of undetermined cause: the NINCDS Stroke Data Bank. Ann Neurol 1989, 25, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Lechat, P.; Mas, J.L.; Lascault, G.; Loron, P.; Theard, M.; Klimczac, M.; et al. Prevalence of patent formane ovale in young stroke patients. N Engl J Med 1988, 2, 11–12. [Google Scholar]
- Webster, M.W.; Chancellor, A.M.; Smith, H.J.; Swift, D.L.; Sharpe, D.N.; Bass, N.M.; et al. Patent foramen ovale in young stroke patients. Lancet 1988, 2, 11–12. [Google Scholar] [CrossRef] [PubMed]
- De Belder, M.A.; Tourikis, L.; Leech, F.; Camm, A.J. Risk of patent foramen ovale for thomboembolic events in all age groups. Am J Cardiol 1992, 69, 1316–1320. [Google Scholar] [CrossRef] [PubMed]
- Di Tullio, M.; Sacco, R.L.; Gopal, A.; Mohr, J.P.; Homma, S. Patent formamen ovale as a risk factor for cryptogenic stroke. Ann Intern Med 1992, 117, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Hausmann, D.; Mugge, A.; Becht, I.; Daniel, W.G. Diagnosis of patent formaen ovale by transesophageal echocardiography and association with cerebral and peripheral embolic events. Am J Cardiol 1992, 70, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Cabanes, L.; Mas, J.L.; Cohen, A.; Amarenco, P.; Cabanes, P.A.; Oubary, P. Atrial septal aneurysm and patent foramen ovale as a risk factors for cryptogenic stroke in patients less than 55 years of age. A study using transesophageal echocardiography. Stroke 1993, 24, 1865–1873. [Google Scholar] [CrossRef] [PubMed]
- Homma, S.; Sacco, R.L.; Di Tullio, M.R.; Sciacca, R.R.; Mohr, J.P. Effect of medical treatment in stroke patients with patent foramen oval. Patent Foramen Ovale in Cryptogenic Stroke Study. Circulation 2002, 105, 2625–2631. [Google Scholar] [PubMed]
- Bogousslavsky, J.; Garazi, S.; Jeanrenaud, X.; Aebischer, N.; Van Melle, G. Stroke recurrence in patients with patent foramen ovale: the Lausanne Study. Lausanne Stroke with Paradoxal Embolism Study Group. Neurology 1996, 46, 1301–1305. [Google Scholar] [CrossRef] [PubMed]
- Mas, J.L.; Zuber, M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995, 130, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Nedeltchev, K.; Arnold, M.; Wahl, A.; Sturzenegger, M.; Vella, E.E.; Windecker, S.; et al. Outcome of patients with cryptogenic stroke and patent formane ovale. J Neurol Neurosurg Psychiatry 2002, 72, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Wahl, A.; Jüni, P.; Mono, M.; Kalesan, B.; Praz, F.; Geister, L.; et al. Long-term propensity score-matched comparison of percutaneous closure of patent foramen ovale with medical treatment after paradoxical embolism. Circulation 2012, 125, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Khairy, P.; O’Donnell, C.P.; Lanzberg, M.J. Transcatheter closure versus medical therapy of patent foramen ovale and presumed paradoxical thromboemboli: a systematic review. Ann Intern Med 2003, 139, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Wahl, A.; Praz, F.; Stirnimann, J.; Windecker, S.; Seiler, C.; Nedeltchev, K.; et al. Safety and feasibility of percutaneous closure of patent foramen ovale without intra-procedural echocardiography in 825 patients. Swiss Med Wkly 2008, 138, 567–572. [Google Scholar] [PubMed]
- Agarwal, S.; Bajaj, N.S.; Kumbhani, D.J.; Tuzcu Em Kapadia, S.R. Meta- analysis of transcatheter closure versus medical therapy for patent foramen ovale in prevention of recurrent neurological events after presumed paradoxical embolism. JACC Interv 2012, 5, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.J.; Reisman, M.; Massaro, J.; Mauri, L.; Adams, H.; Albers, G.W.; et al. Closure or medical therapy for dryptogenic stroke with patent foramen ovale. N Engl J Med 2012, 366, 991–999. [Google Scholar] [CrossRef] [PubMed]

© 2012 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Pilgrim, T.; Vogel, R.; Meier, B. Waiting for Evidence Seems to Make Sense—Except for the One Providing the Evidence. Cardiovasc. Med. 2012, 15, 258. https://doi.org/10.4414/cvm.2012.01697
Pilgrim T, Vogel R, Meier B. Waiting for Evidence Seems to Make Sense—Except for the One Providing the Evidence. Cardiovascular Medicine. 2012; 15(9):258. https://doi.org/10.4414/cvm.2012.01697
Chicago/Turabian StylePilgrim, Thomas, Rolf Vogel, and Bernhard Meier. 2012. "Waiting for Evidence Seems to Make Sense—Except for the One Providing the Evidence" Cardiovascular Medicine 15, no. 9: 258. https://doi.org/10.4414/cvm.2012.01697
APA StylePilgrim, T., Vogel, R., & Meier, B. (2012). Waiting for Evidence Seems to Make Sense—Except for the One Providing the Evidence. Cardiovascular Medicine, 15(9), 258. https://doi.org/10.4414/cvm.2012.01697



