Abstract
Today exposure to high altitudes is relatively common. Thus, basic knowledge is important also for physicians that are not specialised in this topic. Exercise capacity is limited at high altitude, mainly due to hypoxia. Additional factors (circumstances) may aggravate the problem. Still, day trips to altitudes up to 3000–3500 m are relatively safe even in patients with cardiovascular diseases, unless patients are not stable. Unstable patients are not suited for hypoxia exposure although direct evidence is largely lacking. Overnight stay at high altitude increases the risk. Also, patients with moderate to severe pulmonary hypertension, irrespective of the underlying cause, should limit exposure to altitudes of not more than 1500–2000 m. With respect to flying, similar limitations apply. Moreover, circumstances of travel must be taken into account (e.g., limited access to medical help) and sufficient medication (in duplicate at different places) should be taken with the patient. As discussed in the last part of this review, subjects that are susceptible to develop high altitude pulmonary edema should avoid rapid ascent to high altitude, or should be treated prophylactically. To what extent research in these subjects is relevant for pathophysiology of pulmonary hypertension at normoxia needs further investigation.
Introduction
It might be argued that research of high altitudes is relevant for a very small proportion of subjects in clinical practice only. This assumption is, however, not true because of different reasons. Thus, trips to and also stays at high altitude are increasingly popular. Importantly, many people live at altitudes above 1500 m and relatives living at low altitude wish to visit them. Both healthy subjects and even more so patients with cardiovascular problems may suffer from serious problems when exposed. Moreover, airline travel is nowadays part of daily life and also patients with cardiac diseases want or have to fly. Finally, it may also serve as a model of pulmonary hypertension that may be extrapolated to low altitudes. Thus, several aspects of high altitudes are relevant to a significant proportion of the population.
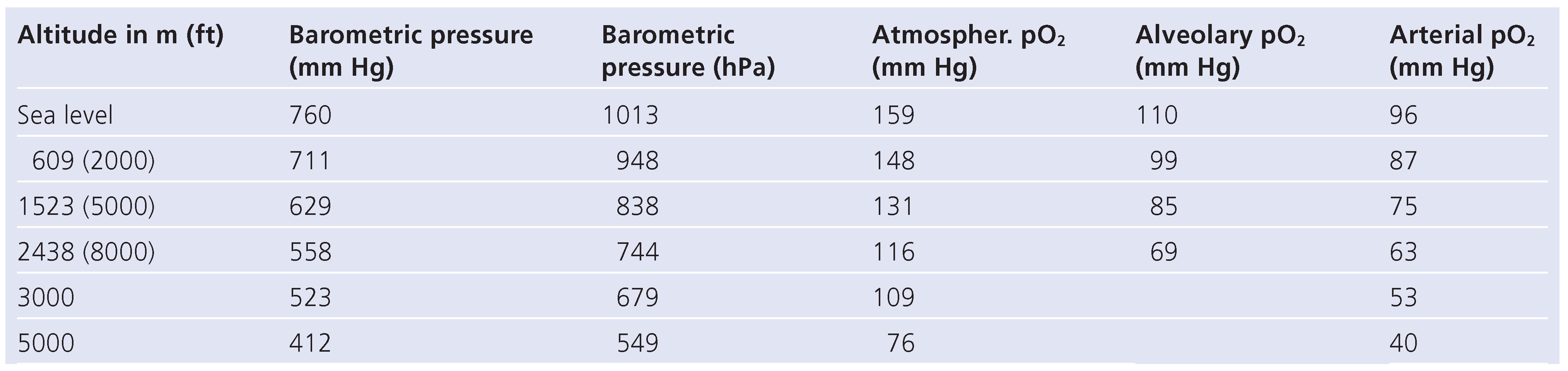
Various factors are different at high altitudes that may cause problems such as higher ultra violet radiation, lower temperature and rapid changes of the environment. Most importantly, however, oxygen partial pressure is diminished with increasing altitude (Table 1) [1], resulting in hypoxia. Some subjects may be susceptible to hypoxia even when healthy. Moreover, hypoxia may be less well tolerated by patients with cardiovascular and pulmonary diseases.

Table 1.
Pressure at different levels of altitude [1].
Cardiovascular adaptation to high altitudes
When exposed to reduced oxygen content, there are several changes that occur rapidly [2]. As a consequence, the oxygen content in the arterial blood decreases, i.e. hypoxia occurs (Table 1). Because of the S-shape of the haemoglobin dissociation curve, patients will experience oxygen desaturation at elevations above 3000 m. During exercise, however, desaturation may occur at much lower altitudes, particularly in the elderly patient and in patients with cardiovascular and pulmonary diseases [3]. Total oxygen demand for a given workload, however, is independent of altitude. Thus, cardiac output must increase to maintain oxygen delivery for a given workload, given the reduced arterial oxygen content of the blood.
As a result of hypoxia, ventilation increases to compensate for the reduced arterial oxygen content in part. This results in hypocapnia and respiratory alkalosis as well as an increase in 2.3 di-phospho-glycerate (DPG). There is also an increase in sympathetic tone and circulating levels of both noradrenaline and adrenaline, possibly via stimulation of peripheral chemoreceptors. This results in an increase in cardiac output and coronary flow, but also myocardial work and myocardial ox-ygen consumption. On the other hand, hypoxemia has a direct vasodilatory effect on the systemic circulation, counteracting the increase in blood pressure that would be expected as a result of sympathetic stimulation with considerable individual variation. In contrast, due to the Euler-Lillestrand reflex, there is vasoconstriction of the pulmonary vascular bed. This is most pronounced in the resistance vessels of the pulmonary circulation and much less on the venous side. Respiratory alkalosis counteracts this response, but the net effect is an increase in pulmonary arterial pressure, which is significantly enhanced in some subjects (see below).
After several days, adaptation to hypoxia is present, usually occurring within app. 4 days. Thus, oxygen content in the arterial blood increases and there is a reduction in pulmonary artery pressure. Still, there is no complete resolution present even after long-lasting stays at high altitude. The reduction in hypoxia results in less systemic vasodilation and because sympathetic tone remains elevated to some extent, there may be an increase in systemic blood pressure [2]. Importantly, intermittent hypoxia (4-day stay at high altitude and 3 days at low altitude), even over longer period of time, does not prevent acute effects of hypoxia during reexposure [4].
One of the questions regarding effects of high altitudes raised, is the extent and reason for limitation of exercise capacity. Obviously, limited availability of oxygen is most important, but hypoxia does not fully explain limitations when exposed to altitude of ≥4000 m, as there is a disproportional decrease in exercise capacity as measured by peak oxygen consumption (peak VO2). Also, maximal cardiac output at these altitudes is reduced, but the question is why. Different factors have been discussed to be responsible for the disproportional limitation, such as decreased stroke volume, limited maximal heart rate by enhanced parasympathetic neural activity [5], decreased peripheral demand due to altered matching of convectional and diffusional O2 transport systems [6], and a decreased central command. An impaired right ventricular function could also be involved, as inhibition of hypoxic pulmonary vasoconstriction by the phosphodiesterase-5 inhibitor sildenafil might improve maximum workload in hypoxia [7]. Alternatively, improvement in ventilation-perfusion mismatch might explain this increase in maximum workload. However, improved hypoxic exercise capacity by sildenafil decreases over time and is not clearly related to changes in pulmonary vascular resistance. More recently, we found that improvement in exercise capacity in subjects with exacerbated pulmonary vascular response was related to the extent of medical reduction in pulmonary artery pressure [8]. Based on ergospirometric and echocardiographic findings, it seemed that the pulmonary circulation including ventilation/perfusion mismatch is the main mechanism of disproportional limitation in exercise capacity. Reduced cardiac output seems, therefore, rather be a consequence than a cause. In addition to understanding adaptation to high altitudes, this may also be important to understand limited exercise capacity in patients with pulmonary hypertension at low altitudes.
Pathophysiology of high altitudes
There are several factors that may aggravate hypoxia in both healthy and sick. In the latter, however, such aggravation may become clinically relevant since reserves are already reduced. Thus, among the most important aggravating factors are cardiovascular and pulmonary diseases. There are other factors that may be important particularly when patients are exposed to high altitudes. Thus, smoking is very relevant as the uptake of carbon monoxide further reduces O2 uptake in the blood. Moreover, smoking results in a left-shift of the O2-dissociation curve, reducing the peripheral availability of oxygen. In addition, alcohol use increases hypoxia, probably due to the reduction in respiratory drive [9].
Physical activity, particularly strenuous exercise reduces the arterial O2 content as mentioned above (e.g. [8]). This is seen in all subjects, not only in subjects that are susceptible to hypoxia exposure or patients with cardiovascular or pulmonary diseases. Still, it is obviously more relevant in the latter groups. Medication may also influence O2 saturation when exposed to high altitude, although studies addressing this important issue directly are very limited. Thus, β-blockers may reduce O2 saturation as compared to placebo at high altitude. Oxygen saturation was significantly lower with both nebivolol and carvedilol during a 3-day stay at 4559 m in a crossover study in healthy subjects who were treated 2 weeks before and during the stay at high altitudes [10]. Whether this also applies to shorter stays and at lower altitudes has not yet been properly tested. On the other hand, the observed increase in (24-h) blood pressure was partly counteracted by the use of the two β-blockers. Thus, the net effect of medication in patients at high altitude remains to be determined.
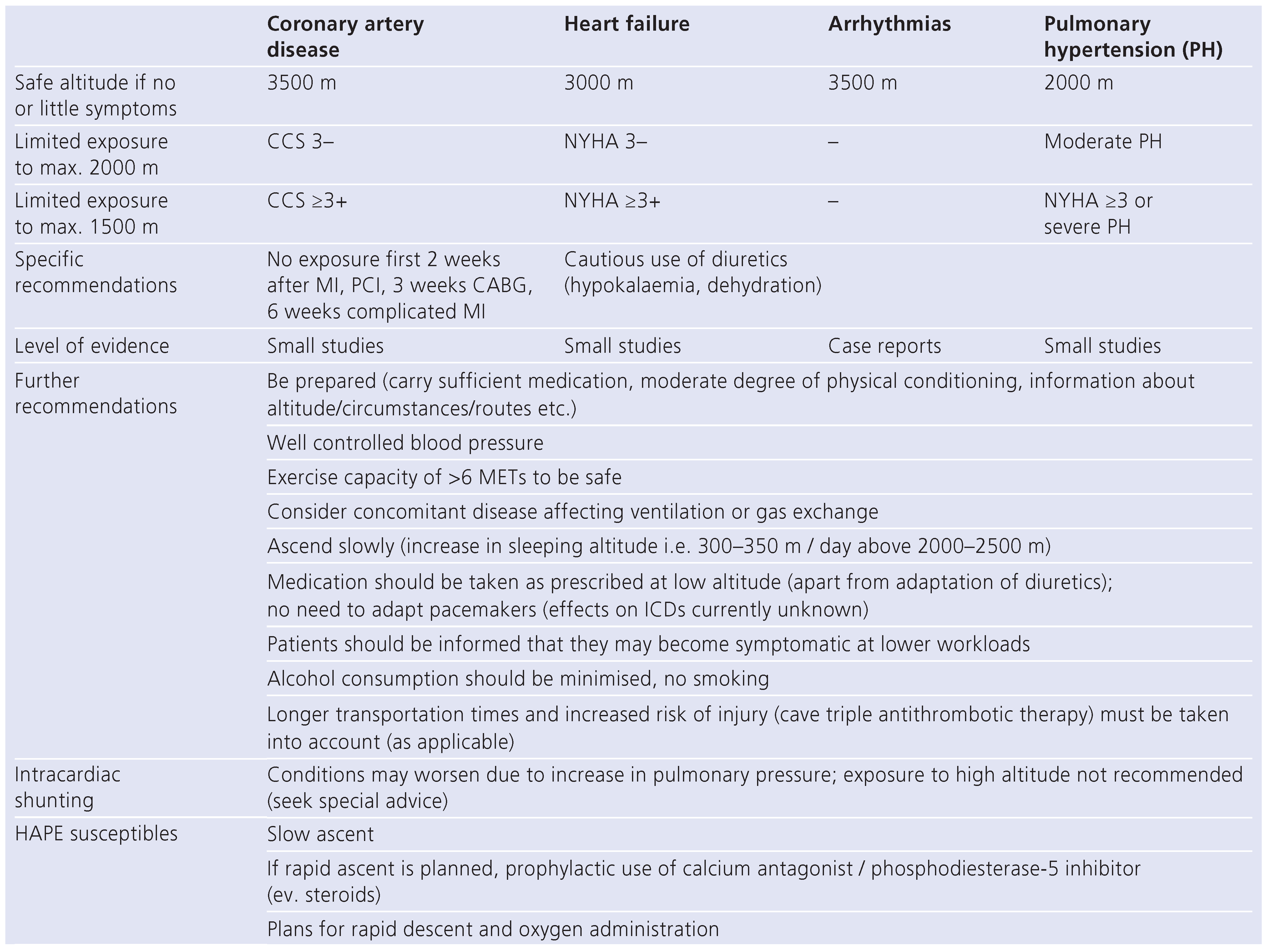
Reduced O2 partial pressure may exacerbate preexisting conditions and patients may become symptomatic at lower levels of exercise or even at rest (Figure 1). Obviously, patients with little exercise capacity at low altitudes are most prone to develop symptoms at high altitudes. Accordingly, the general recommendation is that patients that are symptomatic at low levels of exercise in normoxia should not be exposed to hypoxia.
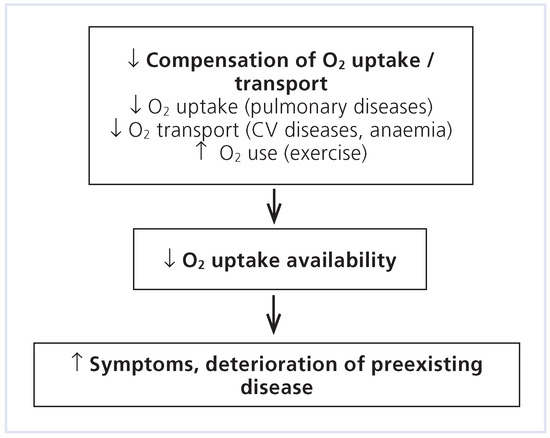
Figure 1.
Response of acute reduction in oxygen partial pressure in patients with cardiovascular (CV) and pulmonary diseases.
There are, however, additional aspects that may be important in patients. Thus, dehydration may occur because humidity is usually lower at high altitude (during aircraft travel this is usually even more extreme, see below), resulting in further activation of sympathetic activity. Dehydration may exacerbate hypotension and orthostatic response, which is particularly relevant in patients with (advanced) heart failure (HF). The cold environment may increase the energy demand and cardiac output by (further) increasing sympathetic activation.
Exposure to high altitudes in patients with coronary heart disease
The activation of the sympathetic nervous system, together with the above mentioned dehydration, may theoretically activate thrombocytes and, as a consequence, increase the risk of thromboembolic events including acute coronary syndrome. However, based on epidemiological data and small pathophysiological studies, this does not seem to be the case up to altitudes of app. 4000 m [11], although this was obviously not tested in proper prospective trials.
In healthy subjects, coronary flow reserve is increased, even in subjects susceptible to high altitude pulmonary edema (HAPE) that show an exacerbated response of the pulmonary vasculature to high altitudes but not the coronary vasculature. Only immediately prior to HAPE, a reduce flow reserve was seen [12]. In patients with coronary artery disease, however, some although not all studies described a reduced coronary flow reserve at high altitude [13]. Whether this is of clinical relevance is debated. Still, exercise testing during hypoxia in stable patients with coronary artery disease showed little ST-deviation, at least if ischaemia was absent at low to moderate exercise at low altitudes. Also, exercise response did not differ from low altitudes in such patients [14]. Thus, heart rate u blood pressure product did not differ and the same lactate levels were achieved. Most previous, though small studies, showed ST-deviations at a similar heart rate u blood pressure product as at low altitude [11]. A small study even showed that intermittent exposure to hypoxia may reduce the ischaemia score in patients with stable coronary artery disease. These subjects had once a week 4 h exposure to hypoxia starting at simulated altitude of 2400 m with weekly increase of 300 m (total 14 sessions) [15]. Obviously, more studies are required before such an approach can be recommended to reduce ischaemic burden. Nevertheless, limited exposure to hypoxia in patients with stable coronary artery disease seems to be safe, but no experience exists in unstable patients and due to the above mentioned theoretical considerations, such patients may well be at significant risk.
Exposure to high altitudes in patients with heart failure
Patients with HF may tolerate exposure to high altitudes less well than healthy subjects. Obviously, reduced O2 may further reduce already limited exercise capacity, but relative reduction in peak VO2 may even be disproportionate compared to healthy subjects (Figure 2) [16]. The underlying cause of this is not yet precisely known. Patients with HF show an exacerbated respiratory response to exercise even at normoxia, expressed as pathologic increase in VE/VCO2 during exercise. This may be further increased at high altitude. Moreover, some HF patients may have out-of-proportion pulmonary hypertension, which further limits tolerability of high altitude. However recently, Schmid et al. found no serious adverse reactions in stable HF patients exercising at 3454 m altitude. They included patients with stable HF NYHA II and non-severely reduced exercise capacity (peak VO2 >50% of predicted value). Exercise capacity fell by 22%, thus not showing excess reduction [17]. Taken together, patients with stable, little symptomatic (NYHA ≤ II) HF not showing pulmonary hypertension may well be exposed to high altitude (up to 3000 m, possibly 3500 m), although data are very limited.
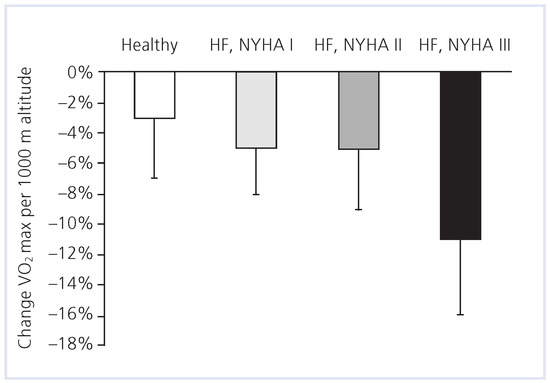
Figure 2.
Change in exercise capacity (% reduction per 1000 m altitude) in healthy subjects as compared to patients with different severity of heart failure (HF). (Adapted from [16]: Agostoni P, Cattadori G, Guazzi M, et al. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am J Med. 2000;109:450–5. © Elsevier, reprint with kind permission.
Risk of arrhythmias at high altitudes
Again, direct evidence is very scarce and sufficiently supported recommendations cannot be made. However, arrhythmias do not seem to be a major problem in subjects exposed to high altitude. Theoretically, the activation of the sympathetic activity may increase the risk of (serious) arrhythmias. This might be further increased due to the fact that the alkalosis due to hyperventilation results in a shift of potassium to the intracellular space and thereby increases the risk of hypokaliaemia. Moreover, pulmonary hypertension and the theoretical increased risk of acute coronary syndrome may contribute to the risk of serious arrhythmias. Clinically, there are reports of increased numbers of both ventricular and supraventricular ectopic beats, but there are only case reports of serious arrhythmias and sudden cardiac death during exposure to high altitude. Patients prone to serious arrhythmias, particularly ventricular tachycardias, however, should not be exposed to altitude above 3000–3500 m.
Additional aspects when travelling, general recommendations
Another important aspect when travelling to remote places is the limited access to medical treatment if required. Thus, medication should be carried during travelling in duplicate, stored at different places. Availability of medical services should be checked prior to travel and decisions whether to travel should be based on this and the potential risk of individual patients.
In light of the lack of data, it is always better to be cautious in case of doubt. In general, patients with cardiac diseases should not go to high altitudes in an unstable disease state [18]. In addition, patients should be advised that they may become symptomatic at an earlier stage, as heart rate u blood pressure product reflects physical load and not workload itself. When stable and well compensated, risk is not significantly increased by the altitude-related hypoxia up to app. 3000 m for patients with HF and 3500 m for patients with stable coronary artery disease; however, patients have to account for the particular circumstances of a stay at high altitudes. A stress test prior to exposure may help to risk stratify patients, as suggested by several small studies in patients with coronary artery disease prior to ascent [11, 18]. Symptoms or ischaemia must not occur at light to moderate exercise. Above 3500 m, there is a considerable decrease of exercise capacity and therefore, in addition to a stable disease, preserved left ventricular function and exercise capacity clearly above normal are required for a safe stay. Even then, patients with cardiovascular heart disease should generally be advised not to go higher than 4500 m. Patients with pulmonary hypertension are very sensitive to hypoxia and even an altitude of 1500 m may cause problems [19]. This limit also applies to unstable patients in general. It is important to note that this does not only refer to patients with pulmonary hypertension class 1 according to WHO classification, but also secondary to other diseases including HF. Figure 3 and Table 2 show general recommendations for safe travel to high altitudes in patients with different diseases [18].
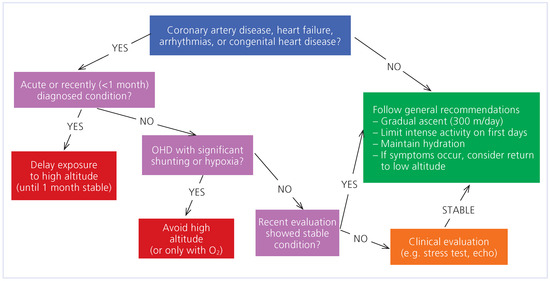
Figure 3.
Algorithm if patients with cardiovascular diseases travel to high altitudes. (Adapted from [18]: Higgins JP, Tuttle T, Higgins JA. Altitude and the heart: is going high safe for your cardiac patient? Am Heart J. 2010;159:25–32. © Elsevier, reprint with kind permission.

Table 2.
Advice for exposure of high altitude (and air-travelling) in cardiac patients.
Recommendations for flying
When flying in commercial aircraft, cabin pressure is higher than the pressure of the actual altitude. Nevertheless, cabin pressure is lower than pressure at low altitude. Thus, pressure usually corresponds to an altitude between 5000 ft and 7000 ft (i.e., 1524 m and 2134 m), never exceeding 10 000 ft (3048 m). There are, however, additional potential problems related to commercial flights. Thus, immobility, together with the increased risk of dehydration, increases the thrombotic risk. Dehydration occurs because humidity is very low during flights (progressive decrease during flights down to 5–10% relative humidity), since the absolute content of water in the air outside the aircraft is very limited. Moreover, subjects may be stressed during flights with the accompanied increase in sympathetic tone. Patients that are handicapped may have difficulties to board and leave an aircraft, but may also be very limited during flights. Also, possibilities to provide care in case of emergencies in an aircraft are very limited and it may take hours to bring a patient to hospital. Table 2 summarises recommendations for travelling to high altitude, which may also be used (as applicable) for aircraft travelling.
These aspects must be considered when patients want to fly. Patients who do not tolerate altitudes above 2000 m should not fly (e.g., patient with clinically relevant pulmonary hypertension [19]). If flying is absolutely necessary, oxygen supply during the flight is required and airlines should be contacted as early as possible. In general, patients who are not stable are unable to fly (i.e., unstable angina, first two weeks after uncomplicated infarction, six weeks in complicated infarction, first two weeks post coronary catheter interventions [PCI] and at least 3 weeks post bypass surgery, HF NYHA III+; similar recommendations for patients with congenital heart diseases. Cave pulmonary hypertension) [18, 20]. Intake of alcohol may reduce tolerability [9].
Despite the potentially increased risk, severe complications are rarely seen [21, 22]. Thus, death rate was as little as 0.31 per million passengers of which the majority (77%) were not known to have health problems (i.e., 399 of 515 deaths; in additional 62 deaths no information was available on history) [21]. Moreover, only 25% of health care problems among commercial air travelers occurred during flight and required only rarely unscheduled landings (7 in one year at an international airport in the US) [22]. Another study found more acutely ill patients during flight compared to stay at the airport, but with a rate of 0.0002%, it was very low. Cardiac arrest occurred in 0.00015% of passengers in aircraft [23]. Although these are rather old data, it is very unlikely that this picture has changed significantly since. It is likely that precautions taken are, at least in part, responsible for the very low complication rate, indicating that the measures taken are probably efficient, but well required.
High altitude pulmonary edema (HAPE)—relevant for lowlanders?
HAPE is a serious problem, accompanied even with mortality when untreated, among subjects staying at altitudes >2500 m without acclimatisation (i.e., ascent within <24h). With increasing altitude, the risk increases and is between 5% and 10% at an altitude of 4500 m in the general population, but 60–70% in those known to be susceptible (HAPE-susceptible). HAPE usually occurs after an overnight stay at high altitudes. It is accompanied by excess pulmonary arterial and to a lesser extent pulmonary venous vasoconstriction. Since vasoconstriction is inhomogeneous, it leaves areas of the pulmonary vasculature unprotected [24]. The individual vascular response to hypoxia might be genetically determined since we found a correlation of the increase in pulmonary artery pressure between fathers and their kids [25].
If HAPE occurs, the person concerned should be brought to lower altitudes as quickly as possible. Oxygen should be given and patients treated with high doses of nifedipine or alternatively other agents that showed to prevent HAPE if given prophylactically. The most important measure to prevent HAPE is acclimatisation. Thus, subjects should not increase more than 300 m/day (sleeping altitude) above 2500 m altitude. This is a general recommendation applicable not only to HAPE-susceptibles, but often not really feasible. Thus, HAPE-susceptibles often require medical prevention which encompasses nifedipine 3 × 20 mg and as alternatives dexamethasone 2 × 8 mg, tadalafil 2 × 10 mg, or inhaled salmeterol 5 × 125 µg, starting the day before ascent [26]. All these measures successfully reduce the risk of HAPE, but the studies were too small to know which of the interventions is most effective.
Research of HAPE-susceptibility may also be of interest to improve understanding of pathophysiology of pulmonary hypertension. Thus, we found that the function of the left ventricle, both systolic and diastolic, as well as perfusion are not altered even when pulmonary pressure is significantly elevated (i.e. >60 mm Hg systolic pulmonary artery pressure). Moreover, it may shed further light in the limitation of exercise capacity when pulmonary pressure is elevated [8]. More importantly, it may highlight the potential importance of exercise-induced pulmonary hypertension, which is believed to be a relatively rare disease. We found, however, that HAPE-susceptibles show slightly, but significantly dilated right-sided cardiac cavaties as compared to matched control subjects (Figure 4) [27]. Since elevation of pulmonary pressure was found to be elevated already at intensities corresponding to daily life activities (increase in systolic pulmonary arterial pressure at 40% of peak exercise 23 ± 6 versus 11 ± 5 mm Hg in non-susceptibles, p < 0.001) [27] and the relative commonness of HAPE-susceptiblity as mentioned above, exercise-induced might be a significantly underestimated problem. Thus, patients with heart failure and preserved ejection fraction were found to have (slightly) increased pulmonary artery pressures at rest [28]. It may be speculated that there is a link between these two entities which would give new opportunities for treating these patients. Obviously, further research is required to investigate this aspect and to see if HAPE-susceptibility may also be of importance in diseases associated with hypoxia (e.g., COPD). Taken together, susceptibility to HAPE may well be of relevance in various circumstances at low altitude, but further research is required to specifically address this important issue.
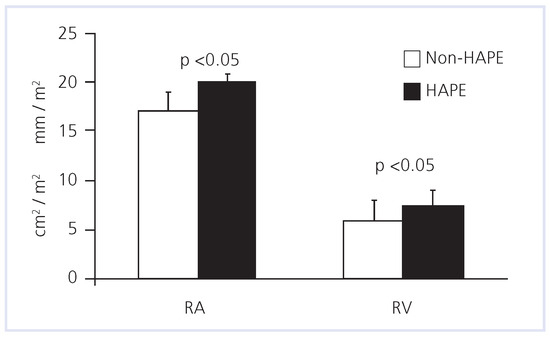
Figure 4.
Subjects who are susceptible to develop high-altitude pulmonary edema (HAPE) when staying overnight at altitude of >2500 m show significantly (p < 0.05) dilated right ventricle (RV) and right atrium (RA) as compared to age-matched subjects who tolerated altitude of 4559 m well.
Conclusions
Nowadays, exposure to high altitudes is relatively common. Thus, basic knowledge is important also for physicians that are not specialised in this topic. Exercise capacity is limited at high altitude, mainly due to hypoxia. Additional factors (circumstances) may aggravate the problem. Day trips to altitudes up to 3000–3500 m are probably relatively safe even in patients with cardiovascular diseases, unless patients are not stable. Unstable patients are not suited for hypoxia exposure although direct evidence is largely lacking.
Subjects that are susceptible to develop HAPE should avoid rapid ascent to high altitude, or should be treated prophylactically. To what extent research in these subjects is relevant for pathophysiology of pulmonary hypertension at normoxia needs further investigation.
Funding/potential competing interests
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Bernheim, A. Höhe und Herzkrankheiten. Praxis (Bern 1994) 2005, 94, 1760–1764. [Google Scholar] [CrossRef]
- Bartsch, P.; Gibbs, J.S. Effect of altitude on the heart and the lungs. Circulation 2007, 116, 2191–2202. [Google Scholar] [CrossRef]
- Burtscher, M.; Bachmann, O.; Hatzl, T.; et al. Cardiopulmonary and metabolic responses in healthy elderly humans during a 1-week hiking programme at high altitude. Eur J Appl Physiol. 2001, 84, 379–386. [Google Scholar] [CrossRef]
- Brito, J.; Siques, P.; Leon-Velarde, F.; De La Cruz, J.J.; Lopez, V.; Herruzo, R. Chronic intermittent hypoxia at high altitude exposure for over 12 years: assessment of hematological, cardiovascular, and renal effects. High Alt Med Biol. 2007, 8, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Boushel, R.; Calbet, J.A.; Radegran, G.; Sondergaard, H.; Wagner, P.D.; Saltin, B. Parasympathetic neural activity accounts for the lowering of exercise heart rate at high altitude. Circulation 2001, 104, 1785–1791. [Google Scholar] [CrossRef] [PubMed]
- Wagner, P.D. Reduced maximal cardiac output at altitude – mechanisms and significance. Respir Physiol. 2000, 120, 1–11. [Google Scholar] [CrossRef]
- Ghofrani, H.A.; Reichenberger, F.; Kohstall, M.G.; et al. Sildenafil increased exercise capacity during hypoxia at low altitudes and at Mount Everest base camp: a randomized, double-blind, placebo-controlled crossover trial. Ann Intern Med. 2004, 141, 169–177. [Google Scholar] [CrossRef]
- Fischler, M.; Maggiorini, M.; Dorschner, L.; et al. Dexamethasone but not tadalafil improves exercise capacity in adults prone to high-altitude pulmonary edema. Am J Respir Crit Care Med. 2009, 180, 346–352. [Google Scholar] [PubMed]
- Roeggla, G.; Roeggla, H.; Roeggla, M.; Binder, M.; Laggner, A.N. Effect of alcohol on acute ventilatory adaptation to mild hypoxia at moderate altitude. Ann Intern Med. 1995, 122, 925–927. [Google Scholar]
- Bilo, G.; Caldara, G.; Styczkiewicz, K.; et al. Effects of selective and nonselective beta-blockade on 24-h ambulatory blood pressure under hypobaric hypoxia at altitude. J Hypertens. 2011, 29, 380–387. [Google Scholar] [CrossRef]
- Dehnert, C.; Bartsch, P. Can patients with coronary heart disease go to high altitude? High Alt Med Biol. 2010, 11, 183–188. [Google Scholar]
- Kaufmann, B.A.; Bernheim, A.M.; Kiencke, S.; et al. Evidence supportive of impaired myocardial blood flow reserve at high altitude in subjects developing high-altitude pulmonary edema. Am J Physiol Heart Circ Physiol. 2008, 294, H1651–7. [Google Scholar][Green Version]
- Wyss, C.A.; Koepfli, P.; Fretz, G.; Seebauer, M.; Schirlo, C.; Kaufmann, P.A. Influence of altitude exposure on coronary flow reserve. Circulation 2003, 108, 1202–1207. [Google Scholar] [CrossRef] [PubMed]
- Schmid, J.P.; Noveanu, M.; Gaillet, R.; Hellige, G.; Wahl, A.; Saner, H. Safety and exercise tolerance of acute high altitude exposure (3454 m) among patients with coronary artery disease. Heart 2006, 92, 921–925. [Google Scholar] [CrossRef] [PubMed]
- del, P.V.; Garcia-Godos, F.; Woolcott, O.O.; et al. Improvement of myocardial perfusion in coronary patients after intermittent hypobaric hypoxia. J Nucl Cardiol. 2006, 13, 69–74. [Google Scholar]
- Agostoni, P.; Cattadori, G.; Guazzi, M.; et al. Effects of simulated-altitude induced hypoxia on exercise capacity in patients with chronic heart failure. Am J Med. 2000, 109, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Schmid, J.P.; Nobel, D.; Novak, J.; Palau, P.; Trepp, A.; Saner, H. Safety and tolerance of high altitude exposure (3454 m) in non-acclimatized patients with chronic heart failure. International Foundation HFSJG. Act. Rep. 2009, 125–126. [Google Scholar]
- Higgins, J.P.; Tuttle, T.; Higgins, J.A. Altitude and the heart: is going high safe for your cardiac patient? Am Heart J. 2010, 159, 25–32. [Google Scholar] [CrossRef]
- Luks, A.M. Can patients with pulmonary hypertension travel to high altitude? High Alt Med Biol. 2009, 10, 215–219. [Google Scholar] [CrossRef]
- Possick, S.E.; Barry, M. Evaluation and management of the cardiovascular patient embarking on air travel. Ann Intern Med. 2004, 141, 148–154. [Google Scholar] [CrossRef]
- Cummins, R.O.; Chapman, P.J.; Chamberlain, D.A.; Schubach, J.A.; Litwin, P.E. In-flight deaths during commercial air travel. How big is the problem? JAMA 1988, 259, 1983–1988. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.O.; Schubach, J.A. Frequency and types of medical emergencies among commercial air travelers. JAMA 1989, 261, 1295–1299. [Google Scholar] [CrossRef] [PubMed]
- O’Rourke, M.F.; Donaldson, E.; Geddes, J.S. An airline cardiac arrest program. Circulation 1997, 96, 2849–2853. [Google Scholar] [CrossRef]
- Maggiorini, M.; Melot, C.; Pierre, S.; et al. High-altitude pulmonary edema is initially caused by an increase in capillary pressure. Circulation 2001, 103, 2078–2083. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Jansen, C.; Linka, A.; et al. Higher pulmonary artery pressure in children than in adults upon fast ascent to high altitude. Eur Respir J. 2008, 32, 664–669. [Google Scholar] [CrossRef]
- Maggiorini, M.; Brunner-La Rocca, H.P.; Peth, S.; et al. Both tadalafil and dexamethasone may reduce the incidence of high-altitude pulmonary edema: a randomized trial. Ann Intern Med. 2006, 145, 497–506. [Google Scholar] [CrossRef]
- Kiencke, S.; Bernheim, A.; Maggiorini, M.; et al. Exercise-induced pulmonary artery hypertension. A rare finding? J Am Coll Cardiol. 2008, 51, 513–514. [Google Scholar]
- Lam, C.S.; Roger, V.L.; Rodeheffer, R.J.; Borlaug, B.A.; Enders, F.T.; Redfield, M.M. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009, 53, 1119–1126. [Google Scholar] [CrossRef]
© 2012 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.