Coronary Steal Phenomenon Due to Ipsilateral Upper Extremity Arteriovenous Fistula in a Patient with Internal Thoracic Artery Bypass Graft—An Alternative Treatment Strategy
Summary
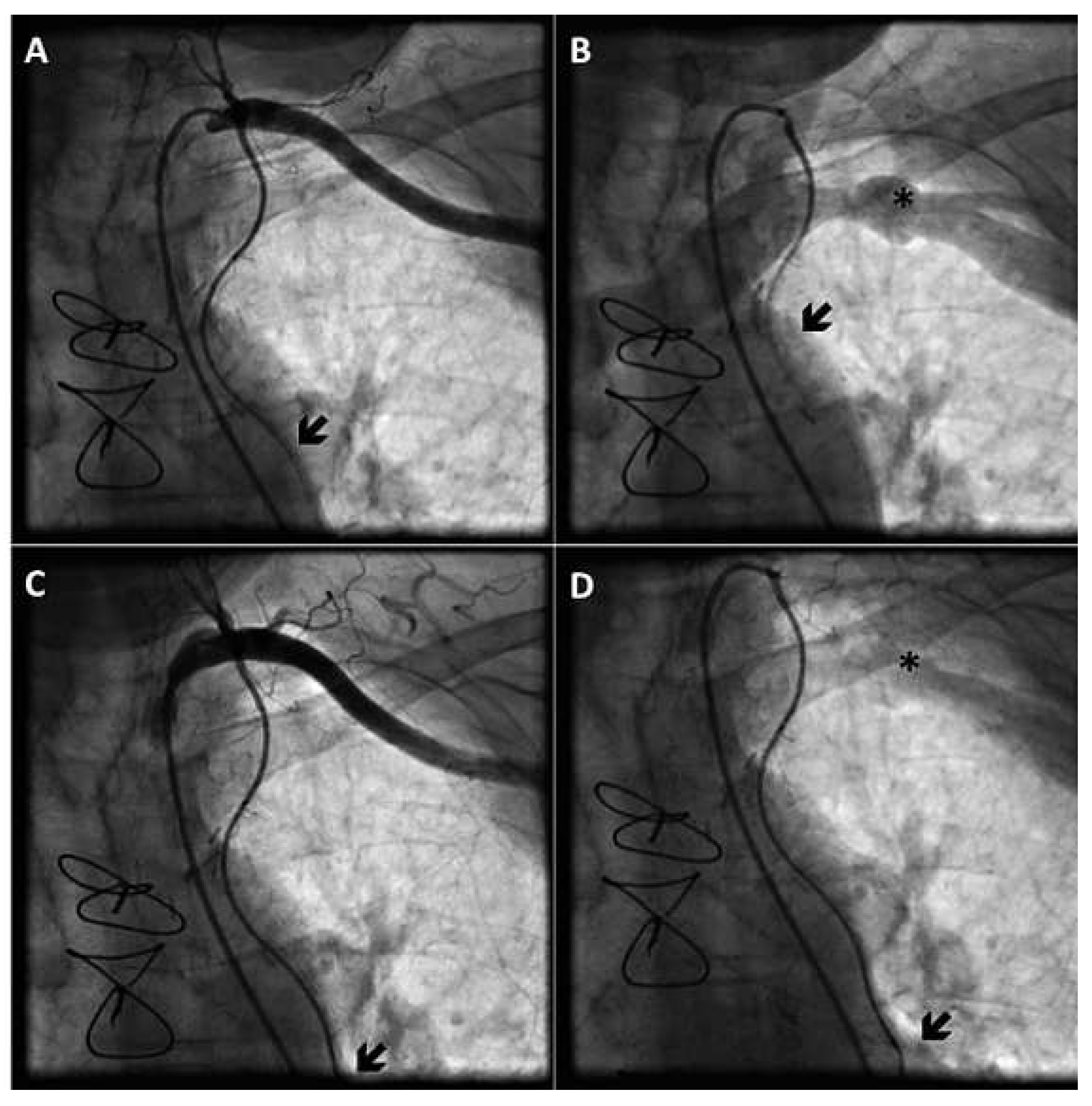
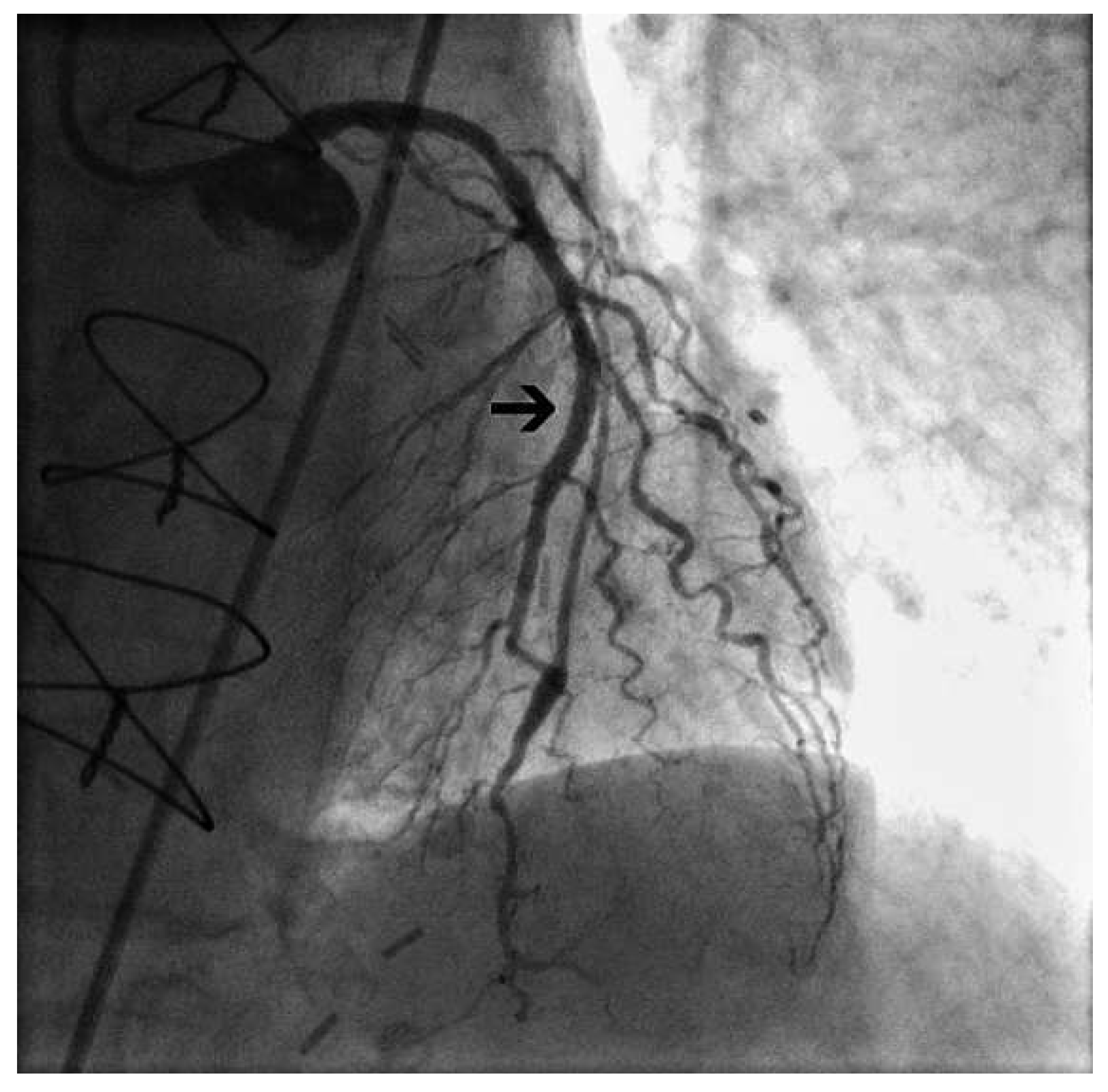
Case Report
Discussion
Conflicts of Interest
References
- Gaudino, M.; Serricchio, M.; Luciani, N.; Giungi, S.; Salica, A.; Pola, R.; et al. Risks of using internal thoracic artery grafts in patients in chronic hemodialysis via upper extremity arteriovenous fistula. Circulation 2003, 107, 2653–2655. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, R.; McGee, W.R.; Birdas, T.J.; Muluk, S.; Magovern, J.; Maher, T. Upper extremity arteriovenous fistulas induce modest hemodynamic effect on the in situ internal thoracic artery. Ann. Thorac. Surg. 2006, 81, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Kato, H.; Ikawa, S.; Hayashi, A.; Yokoyama, K. Internal mammary artery steal in a dialysis patient. Ann. Thorac. Surg. 2003, 75, 270–271. [Google Scholar] [CrossRef] [PubMed]
- Ginzburg, V.; Margulis, G.; Greenberg, G.; Mayzler, O.; Wolak, T.; Tovbin, D.; et al. Preserving the left arm vein in cases of hemodialysis access generating left internal mammary artery steal syndrome. J. Vasc. Access. 2004, 5, 133–135. [Google Scholar] [CrossRef] [PubMed]


© 2012 by the author. Attribution-Non-Commercial-NoDerivatives 4.0.
Share and Cite
D’Amore, S.M.; Zipponi, M.; Hagne, C.; Pedrazzini, G.B. Coronary Steal Phenomenon Due to Ipsilateral Upper Extremity Arteriovenous Fistula in a Patient with Internal Thoracic Artery Bypass Graft—An Alternative Treatment Strategy. Cardiovasc. Med. 2012, 15, 365. https://doi.org/10.4414/cvm.2012.00111
D’Amore SM, Zipponi M, Hagne C, Pedrazzini GB. Coronary Steal Phenomenon Due to Ipsilateral Upper Extremity Arteriovenous Fistula in a Patient with Internal Thoracic Artery Bypass Graft—An Alternative Treatment Strategy. Cardiovascular Medicine. 2012; 15(12):365. https://doi.org/10.4414/cvm.2012.00111
Chicago/Turabian StyleD’Amore, Sergio Musto, Manuel Zipponi, Christian Hagne, and Giovanni B. Pedrazzini. 2012. "Coronary Steal Phenomenon Due to Ipsilateral Upper Extremity Arteriovenous Fistula in a Patient with Internal Thoracic Artery Bypass Graft—An Alternative Treatment Strategy" Cardiovascular Medicine 15, no. 12: 365. https://doi.org/10.4414/cvm.2012.00111
APA StyleD’Amore, S. M., Zipponi, M., Hagne, C., & Pedrazzini, G. B. (2012). Coronary Steal Phenomenon Due to Ipsilateral Upper Extremity Arteriovenous Fistula in a Patient with Internal Thoracic Artery Bypass Graft—An Alternative Treatment Strategy. Cardiovascular Medicine, 15(12), 365. https://doi.org/10.4414/cvm.2012.00111



