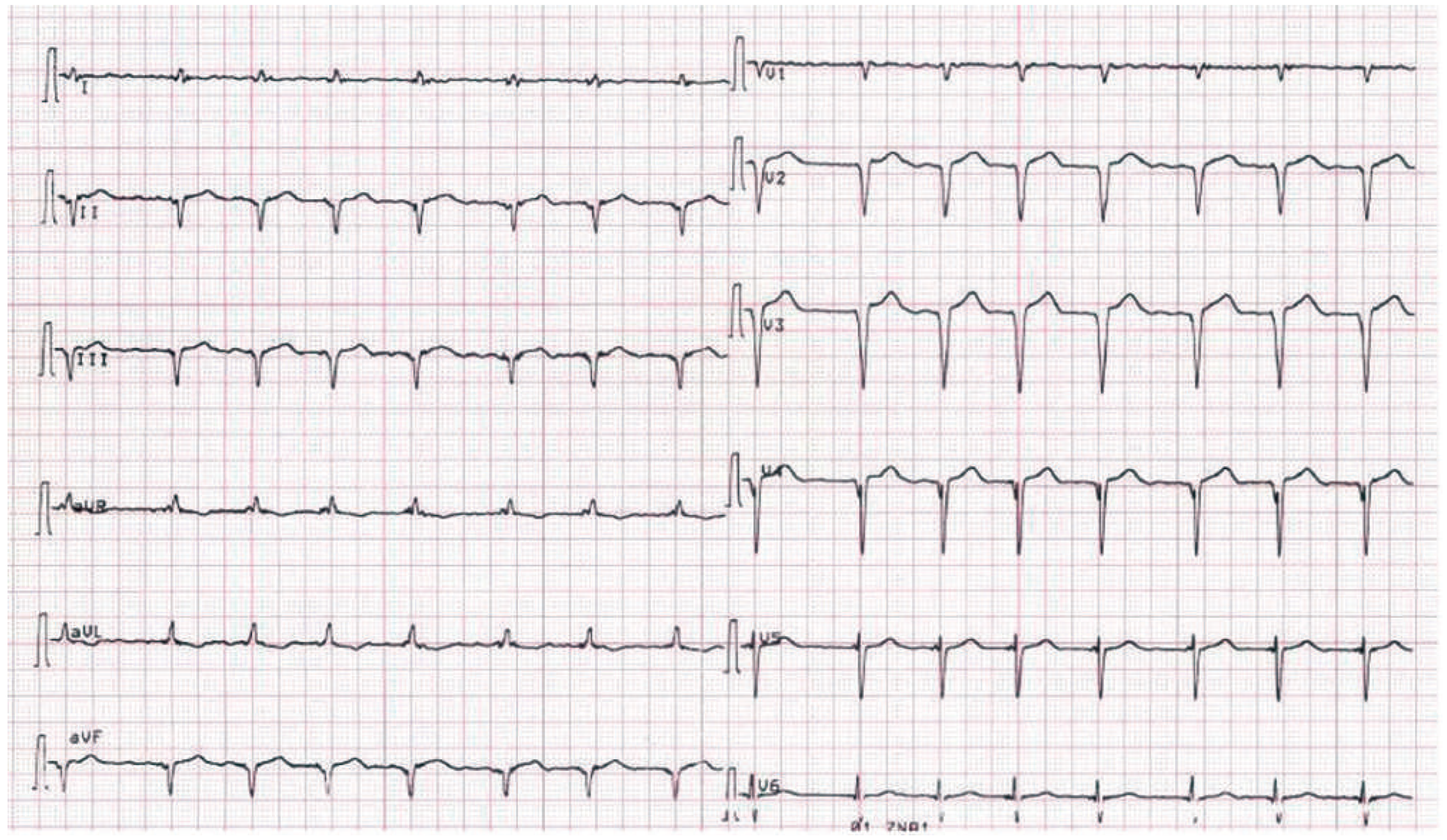
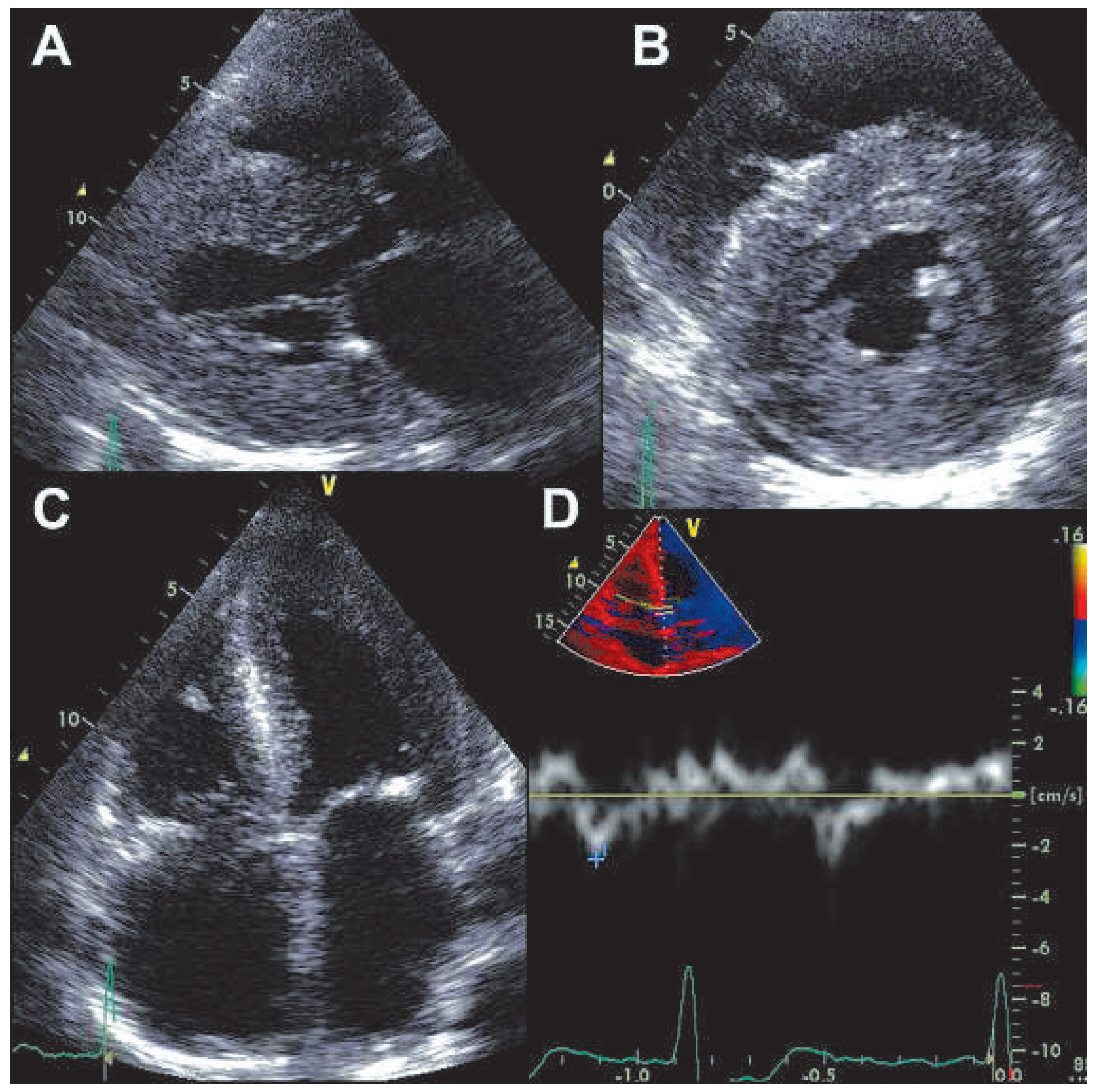
Pseudoinfarction
Case report
Discussion
Funding/potential competing interests
References
- Roberts, W.C.; Waller, B.F. Cardiac amyloidosis causing cardiac dysfunction: analysis of 54 necropsy patients. Am J Cardiol. 1983, 52, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Rahman, J.E.; Helou, E.F.; Gelzer-Bell, R.; Thompson, R.E.; Kuo, C.; Rodriguez, R.; et al. Noninvasive diagnosis of biopsy-proven cardiac amyloidosis. J Am Coll Cardiol. 2004, 43, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Hongo, M.; Yamamoto, H.; Kohda, T.; Takeda, M.; Kinoshita, O.; Uchikawa, S.; et al. Comparison of electrocardiographic findings in patients with AL (primary) amyloidosis and in familial amyloid polyneuropathy and anginal pain and their relation to histopathologic findings. Am J Cardiol. 2000, 85, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Disperenzi, A.; Kyle, R.A.; Gertz, M.A.; Therneau, T.M.; Miller, W.L.; Chandrasekaran, K.; et al. Survival in patients with primary systemic amyloidosis and raised serum cardiac troponins. Lancet 2003, 361, 1787–1789. [Google Scholar] [CrossRef] [PubMed]
© 2012 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Attinger, A.; Maeder, M.T. Pseudoinfarction. Cardiovasc. Med. 2012, 15, 30. https://doi.org/10.4414/cvm.2012.01637
Attinger A, Maeder MT. Pseudoinfarction. Cardiovascular Medicine. 2012; 15(1):30. https://doi.org/10.4414/cvm.2012.01637
Chicago/Turabian StyleAttinger, Adrian, and Micha T. Maeder. 2012. "Pseudoinfarction" Cardiovascular Medicine 15, no. 1: 30. https://doi.org/10.4414/cvm.2012.01637
APA StyleAttinger, A., & Maeder, M. T. (2012). Pseudoinfarction. Cardiovascular Medicine, 15(1), 30. https://doi.org/10.4414/cvm.2012.01637


