Evaluation of Acute Peri-Myocarditis with Cardiac Magnetic Resonance Imaging
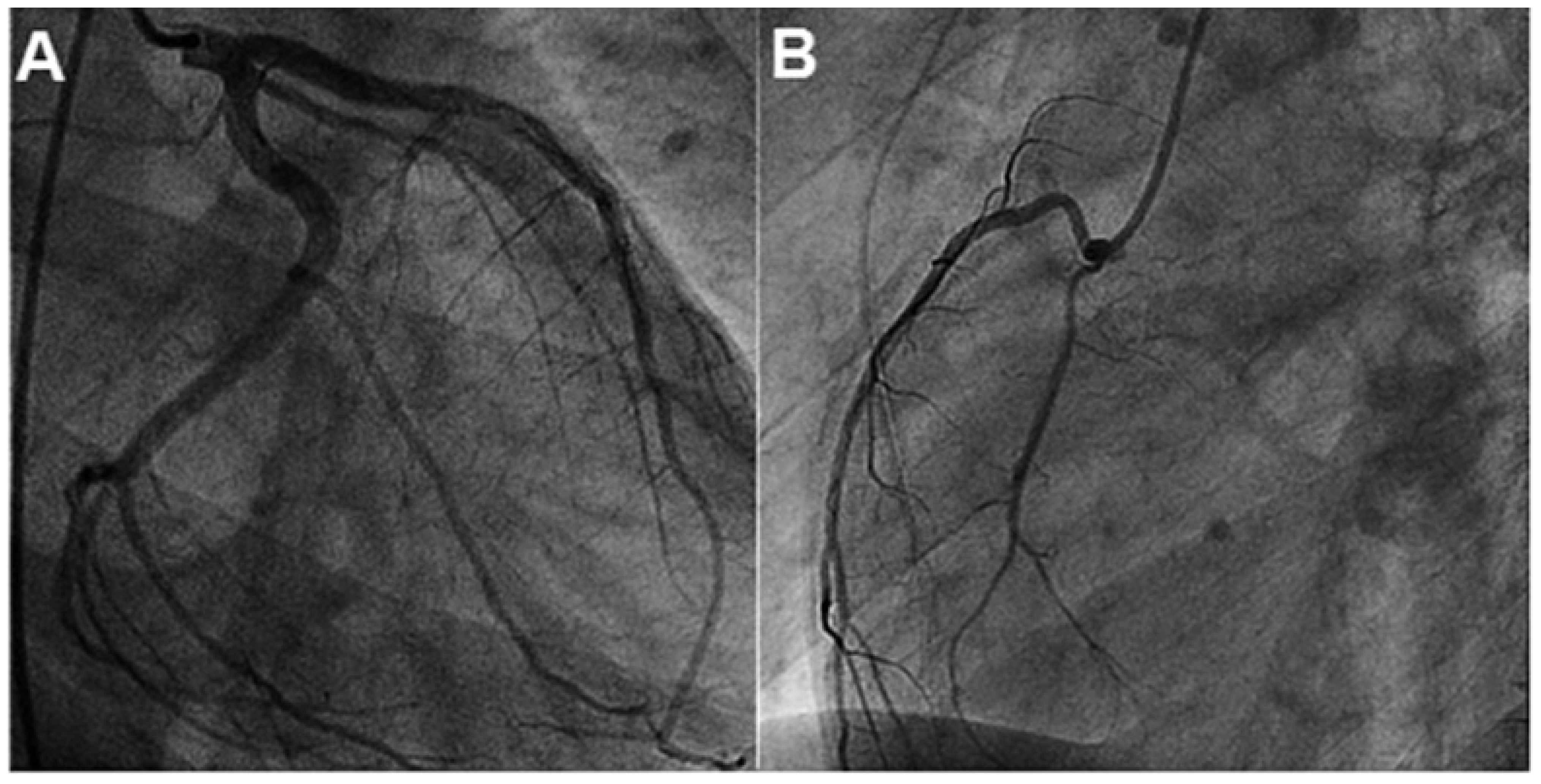
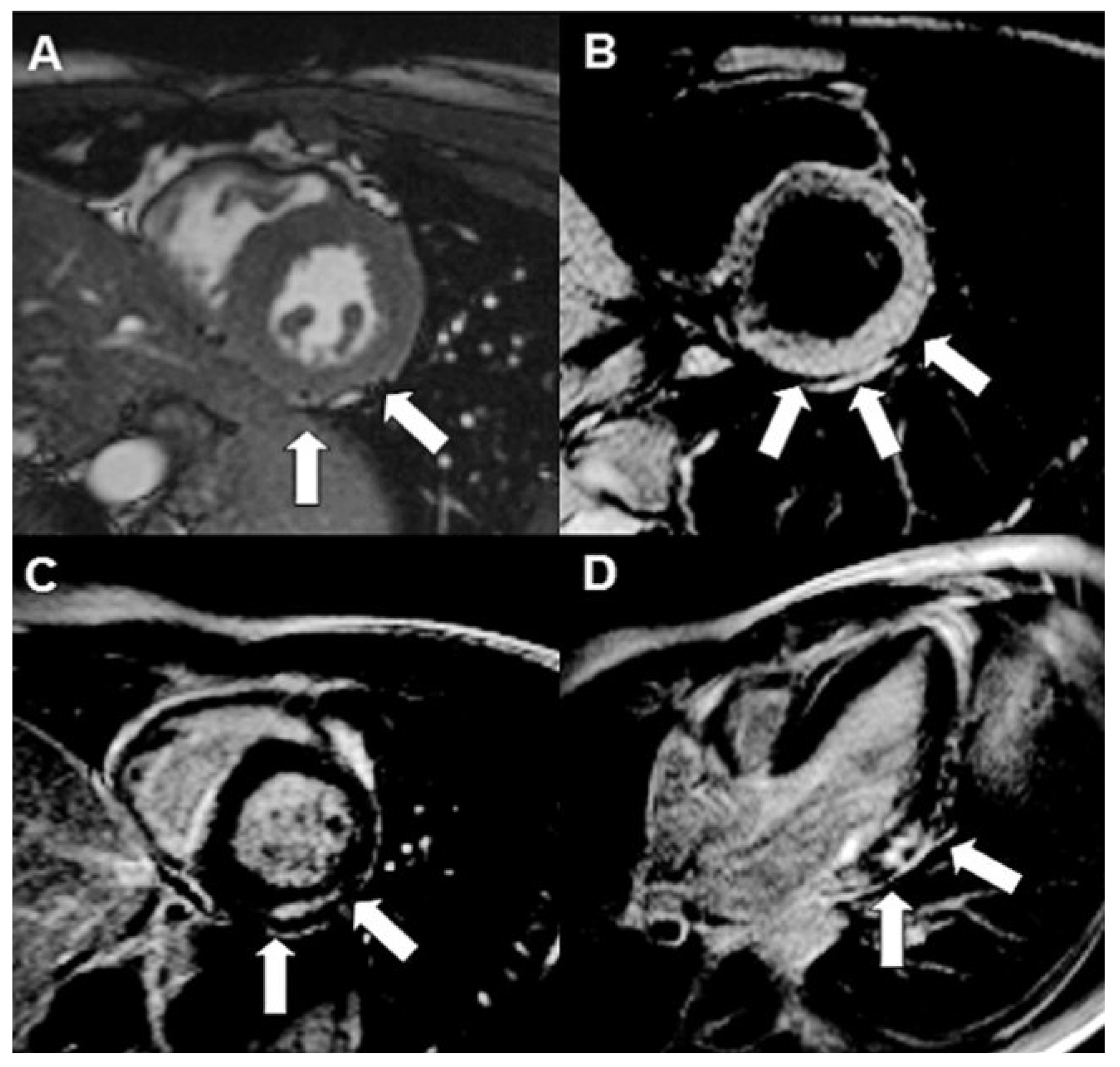
Case report
Discussion
Funding/Potential Competing Interests
References
- Cooper, L.T., Jr. Myocarditis. N Engl J Med. 2009, 360, 1526–1538. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M.; Trinchero, R. Myopericarditis: Etiology, management, and prognosis. Int J Cardiol. 2008, 127, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J.; Ackerman, M.J.; Nishimura, R.A.; Pyeritz, R.E.; Towbin, J.A.; Udelson, J.E. Task Force 4: HCM and other cardiomyopathies, mitral valve prolapse, myocarditis, and Marfan syndrome. J Am Coll Cardiol. 2005, 45, 1340–1345. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Corrado, D.; Bjornstad, H.H.; Panhuysen-Goedkoop, N.; Urhausen, A.; Carre, F.; et al. Recommendations for participation in competitive sport and leisure-time physical activity in individuals with cardiomyopathies, myocardial and pericarditis. Eur J Cardiovasc Prev Rehabil. 2006, 13, 876–885. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Aty, H.; Boyc, P.; Zagrosek, A.; Wassmuth, R.; Kumar, A.; Messrophil, D.; et al. Diagnostic performance of cardiovascular magnetic Resonance in patients with suspected acute myocarditis: Comparison of different approaches. J Am Coll Cardiol. 2005, 45, 1815–1822. [Google Scholar] [CrossRef] [PubMed]
- Gutherlet, M.; Spors, B.; Thoms, T.; Bertram, H.; Denecke, T.; Felix, R.; et al. Suspected chronic myocarditis at cardiac MR: Diagnostic accuracy and association with immunohistologically detected inflammation and viral persistence. Radiology. 2008, 246, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, M.G.; Bevilacqua, M.; Di Renzi, P.; Picardo, S.; Passariello, R.; Marcelletti, C. Usefulness of magnetic resonance imaging for diagnosis of acute myocarditis in infants and children, and comparison with endomyocardial biopsy. Am J Cardiol. 1991, 68, 1089–1091. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.G.; Strohm, O.; Schulz-Menger, J.; Marchiaki, H.; Luft, P.C.; Dietz, R. Contra media enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation. 1998, 97, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- De Cobelli, F.; Pieroni, M.; Esposito, A.; et al. Delayed gadolinium-enhanced cardiac magnetic resonance in patients with chronic myocarditis presenting with heart failure or recurrent arrhythmias. J Am Coll Cardiol. 2006, 47, 1649–1654. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, H.; Goedecke, C.; Wagner, A.; et al. Cardiovascular magnetic resonance assessment of human myocarditis: A comparison to histology and molecular pathology. Circulation. 2004, 106, 1250–1258. [Google Scholar]
- Rathore, S.S.; Curtis, J.P.; Chen, J.; Wang, Y.; Nallamchou, B.K.; Epstein, A.J.; et al. Association of door-to-ballroom time and mortality in patients admitted to hospital with ST elevation myocardial infarction: National cohort study. BMJ. 2009, 328, b1807. [Google Scholar] [CrossRef] [PubMed]
- Goiteiro, O.; Matetzky, S.; Behran, R.; Di Segni, E.; Hod, H.; Bentancur, A.; et al. Acute myocarditis: Noninvasive evaluation with cardiac MRI and transitoracic echocardiography. AJR Am J Roentgenol. 2009, 192, 254–258. [Google Scholar]
- Cooper, L.T.; Baughman, K.L.; Feldman, A.M.; Frustaci, A.; Jessup, M.; Kuhl, U.; et al. The role of endomyocardial biopsy in the management of cardiovascular disease: A scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation. 2007, 116, 2216. [Google Scholar] [CrossRef] [PubMed]
- Narula, J.; Khaw, B.A.; Dec, G.W.; et al. Diagnostic accuracy of antimyosin scintigraphy in suspected myocarditis. J Nucl Cardiol. 1996, 3, 371–81. [Google Scholar] [CrossRef] [PubMed]
- Mavrogeni, S.; Spargias, C.; Bratis, C.; Kolovon, G.; Markussis, V.; Papadopoulou, E.; et al. Myocarditis as a precipitating factor for heart failure: Evaluation and 1-year follow-up using cardiovascular magnetic resonance and endomyocardial biopsy. Eur J Heart Fall. 2011, hfr052v1–hfr052. [Google Scholar] [CrossRef] [PubMed]
© 2011 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Scharen, E.; Paul, M.; Lüscher, T.F.; Corti, R.; Manka, R. Evaluation of Acute Peri-Myocarditis with Cardiac Magnetic Resonance Imaging. Cardiovasc. Med. 2011, 14, 266. https://doi.org/10.4414/cvm.2011.01609
Scharen E, Paul M, Lüscher TF, Corti R, Manka R. Evaluation of Acute Peri-Myocarditis with Cardiac Magnetic Resonance Imaging. Cardiovascular Medicine. 2011; 14(9):266. https://doi.org/10.4414/cvm.2011.01609
Chicago/Turabian StyleScharen, Eva, Matthias Paul, Thomas F. Lüscher, Roberto Corti, and Robert Manka. 2011. "Evaluation of Acute Peri-Myocarditis with Cardiac Magnetic Resonance Imaging" Cardiovascular Medicine 14, no. 9: 266. https://doi.org/10.4414/cvm.2011.01609
APA StyleScharen, E., Paul, M., Lüscher, T. F., Corti, R., & Manka, R. (2011). Evaluation of Acute Peri-Myocarditis with Cardiac Magnetic Resonance Imaging. Cardiovascular Medicine, 14(9), 266. https://doi.org/10.4414/cvm.2011.01609



