Preserved Cerebral Function After Resuscitation and Induction of Hypothermia with Packed Snow †
Abstract
Introduction
Case reports
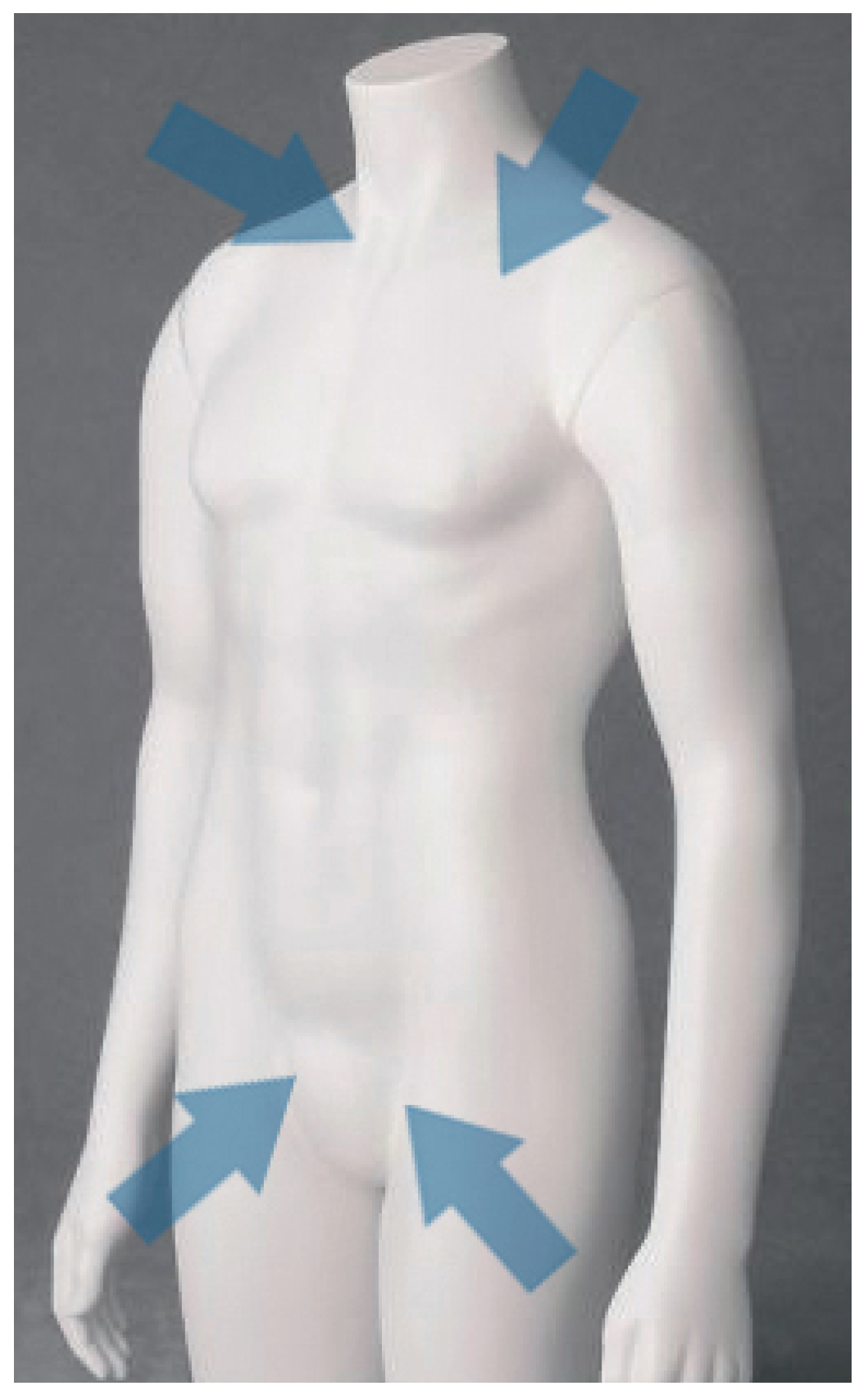
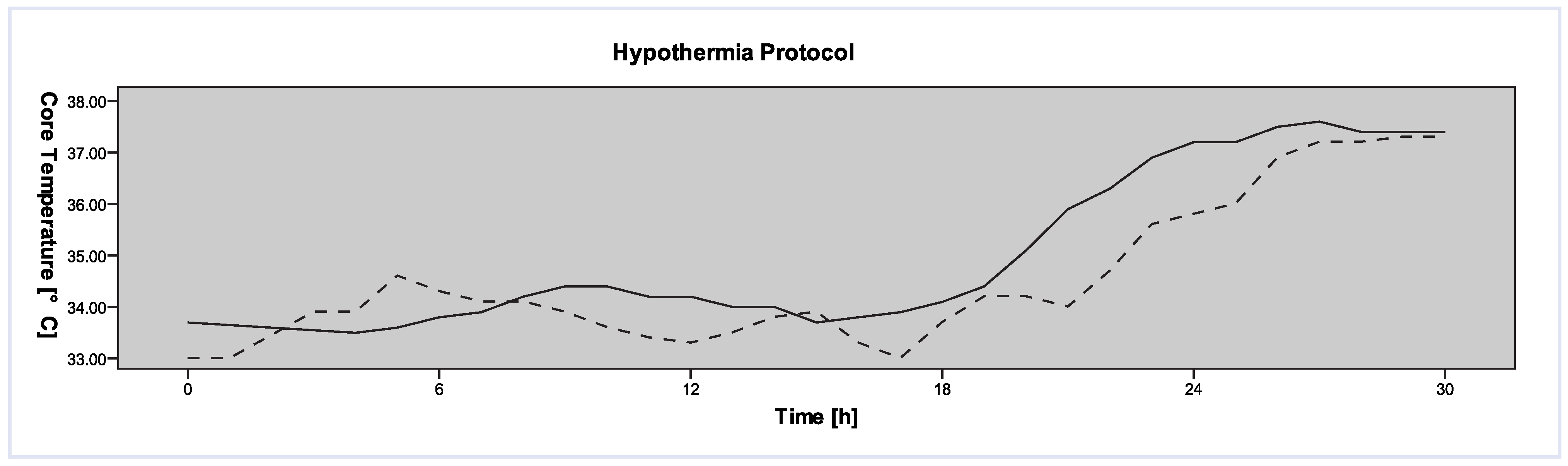
- Case 1
- Case 2
Discussion
References
- Davis, D.P.; Fisher, R.; Aguilar, S.; Metz, M.; Ochs, G.; McCallum-Brown, L.; et al. The feasibility of a regional cardiac arrest receiving system. Resuscitation. 2007, 74(1), 44–51. [Google Scholar] [CrossRef] [PubMed]
- Dunne, R.B.; Compton, S.; Zalenski, R.J.; Swor, R.; Welch, R.; Bock, B.F. Outcomes from out-of-hospital cardiac arrest in Detroit. Resuscitation. 2007, 72(1), 59–65. [Google Scholar] [CrossRef] [PubMed]
- Horsted, T.I.; Rasmussen, L.S.; Meyhoff, C.S.; Nielsen, S.L. Long-term prognosis after out-of-hospital cardiac arrest. Resuscitation. 2007, 72(2), 214–218. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, M.; Stratton, S.J.; Chan, L.S. Cardiac Arrest Resuscitation Evaluation in Los Angeles: CARE-LA. Ann Emerg Med. 2005, 45(5), 504–509. [Google Scholar] [CrossRef] [PubMed]
- Bernard, S.A.; Gray, T.W.; Buist, M.D.; Jones, B.M.; Silvester, W.; Gutteridge, G.; Smith, K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002, 346(8), 557–563. [Google Scholar] [CrossRef] [PubMed]
- Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002, 346(8), 549–556. [CrossRef] [PubMed]
- Boddicker, K.A.; Zhang, Y.; Zimmerman, M.B.; Davies, L.R.; Kerber, R.E. Hypothermia improves defibrillation success and resuscitation outcomes from ventricular fibrillation. Circulation. 2005, 111(24), 3195–3201. [Google Scholar] [CrossRef] [PubMed]
- Soar, J.; Nolan, J.P. Mild hypothermia for post cardiac arrest syndrome. Bmj. 2007, 335(7618), 459–460. [Google Scholar] [CrossRef] [PubMed]
- Abella, B.S.; Rhee, J.W.; Huang, K.N.; Vanden Hoek, T.L.; Becker, L.B. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation. 2005, 64(2), 181–186. [Google Scholar] [CrossRef]
- Nolan, J.P.; Morley, P.T.; Vanden Hoek, T.L.; Hickey, R.W.; Kloeck, W.G.; Billi, J.; et al. Therapeutic hypothermia after cardiac arrest: an advisory statement by the advanced life support task force of the International Liaison Committee on Resuscitation. Circulation. 2003, 108(1), 118–121. [Google Scholar]
- Flint, A.C.; Hemphill, J.C.; Bonovich, D.C. Therapeutic hypothermia after cardiac arrest: performance characteristics and safety of surface cooling with or without endovascular cooling. Neurocrit Care. 2007, 7(2), 109–118. [Google Scholar] [CrossRef]
- Suffoletto, B.P.; Salcido, D.D.; Menegazzi, J.J. Use of Prehospital-Induced Hypothermia After Out-of-Hospital Cardiac Arrest: A Survey of the National Association of Emergency Medical Services Physicians. Prehosp Emerg Care. 2008, 12(1), 52–56. [Google Scholar] [CrossRef] [PubMed]
- Edman, K.A. AL/CF-TR-1996-0118: Testing and Evaluation of the Protocol Systems Propaq 106EL Physiologic Patient Monitor. United States Air Force, Armstrong Laboratory (AFMC), Crew Systems Directorate, Crew Technology Division, Systems Research Branch: Brooks, Texas, USA, 1996. http://www.dtic.mil/cgibin/GetTRDoc?AD=ADA317189&Location=U2&doc=GetTRDoc.pdf.
- Bernard, S.A.; Rosalion, A. Therapeutic hypothermia induced during cardiopulmonary resuscitation using large-volume, ice-cold intravenous fluid. Resuscitation. 2008, 76(2), 311–313. [Google Scholar] [CrossRef] [PubMed]
- Oddo, M.; Schaller, M.D.; Feihl, F.; Ribordy, V.; Liaudet, L. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006, 34(7), 1865–1873. [Google Scholar] [CrossRef] [PubMed]
- Froehler, M.T.; Geocadin, R.G. Hypothermia for neuroprotection after cardiac arrest: mechanisms, clinical trials and patient care. J Neurol Sci. 2007, 261(1–2), 118–126. [Google Scholar] [CrossRef] [PubMed]
- Belliard, G.; Catez, E.; Charron, C.; Caille, V.; Aegerter, P.; Dubourg, O.; et al. Efficacy of therapeutic hypothermia after out-of-hospital cardiac arrest due to ventricular fibrillation. Resuscitation. 2007, 75(2), 252–259. [Google Scholar] [CrossRef] [PubMed]
© 2010 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Pfister, A.J.; Schwab, P.R.; Wahl, A.; Takala, J.; Meier, B.; Höfliger, C. Preserved Cerebral Function After Resuscitation and Induction of Hypothermia with Packed Snow. Cardiovasc. Med. 2010, 13, 284. https://doi.org/10.4414/cvm.2010.01524
Pfister AJ, Schwab PR, Wahl A, Takala J, Meier B, Höfliger C. Preserved Cerebral Function After Resuscitation and Induction of Hypothermia with Packed Snow. Cardiovascular Medicine. 2010; 13(9):284. https://doi.org/10.4414/cvm.2010.01524
Chicago/Turabian StylePfister, Alexander J., Patrik R. Schwab, Andreas Wahl, Jukka Takala, Bernhard Meier, and Carlo Höfliger. 2010. "Preserved Cerebral Function After Resuscitation and Induction of Hypothermia with Packed Snow" Cardiovascular Medicine 13, no. 9: 284. https://doi.org/10.4414/cvm.2010.01524
APA StylePfister, A. J., Schwab, P. R., Wahl, A., Takala, J., Meier, B., & Höfliger, C. (2010). Preserved Cerebral Function After Resuscitation and Induction of Hypothermia with Packed Snow. Cardiovascular Medicine, 13(9), 284. https://doi.org/10.4414/cvm.2010.01524



