A 59-year-old male patient presented with chest pain and electrocardiographic features of an acute inferolateral myocardial infarction. One week prior to admission an acute primary coronary intervention in the distal left circumflex artery (LCX) with implantation of a bare metal stent was performed in the setting of an acute inferolateral infarct.
Emergent coronary angiography showed a totally occluded distal LCX within the stented segment, with no collateral supply. Follow-on percutaneous coronary intervention (PCI) resulted in successful mechanical reperfusion with TIMI 3 flow in the infarct-related artery. There being suspicion of an intimal dissection at the stent outlet, an overlapping additional stent implantation was performed.
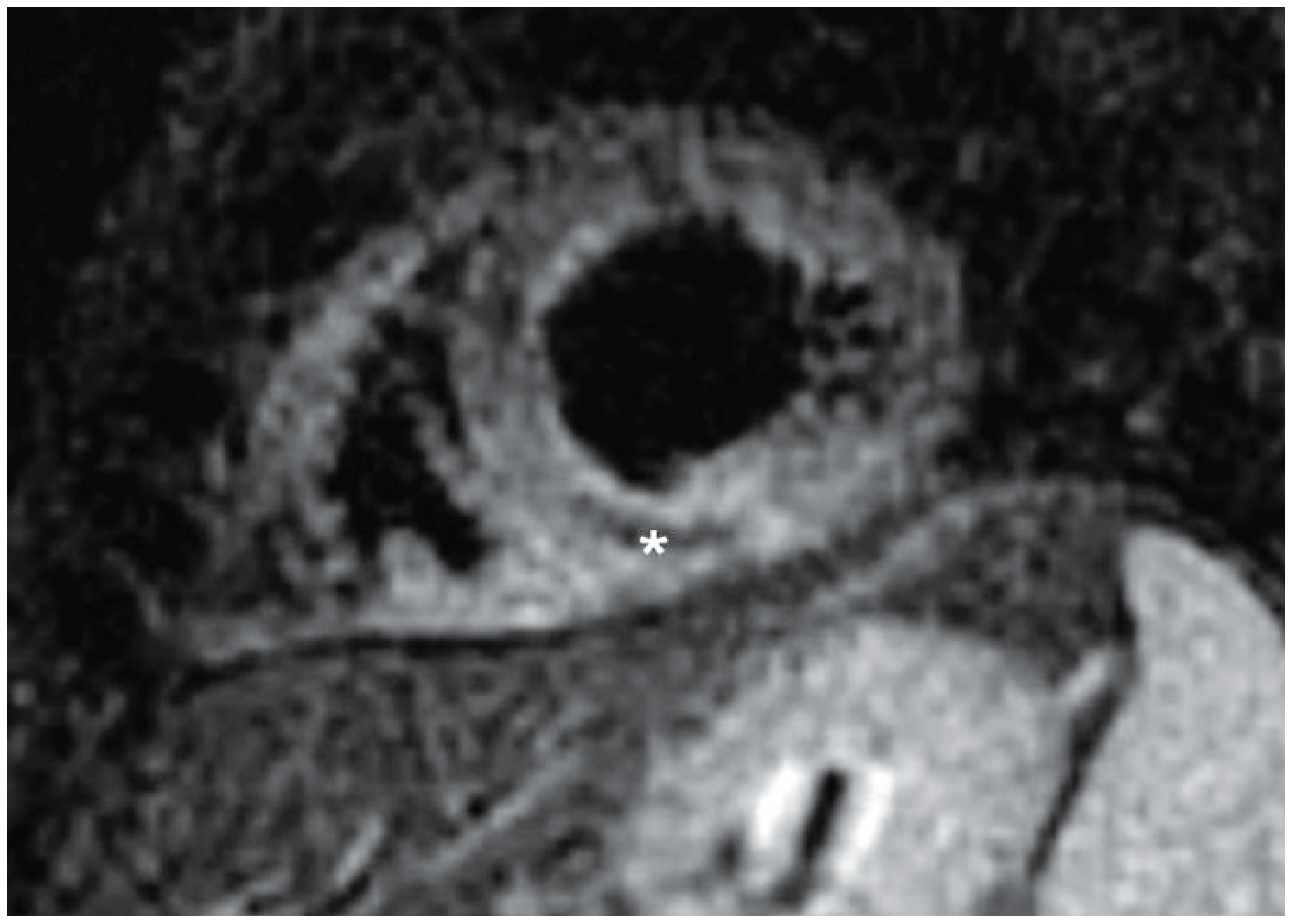
Three days after the emergent PCI cardiac magnetic resonance (CMR) imaging was performed on a clinical 1.5 Tesla scanner using a dedicated 8-element phased array cardiac coil. Cine imaging with steady state free precession gradient echo revealed overall normal systolic function of a mildly dilated left ventricle with only mild regional hypokinesis of the mid to distal inferior wall. T
2-weighted CMR was performed in the cardiac short-axis direction using dark-blood T
2-weighted STIR fast-spin echo, revealing an elevated signal intensity in the inferior segments extending to the inferolateral and inferoseptal walls, with right ventricular involvement consistent with tissue oedema. There was a central core of hypointense signal suggestive of intramyocardial haemorrhage (
Figure 1) Also, T
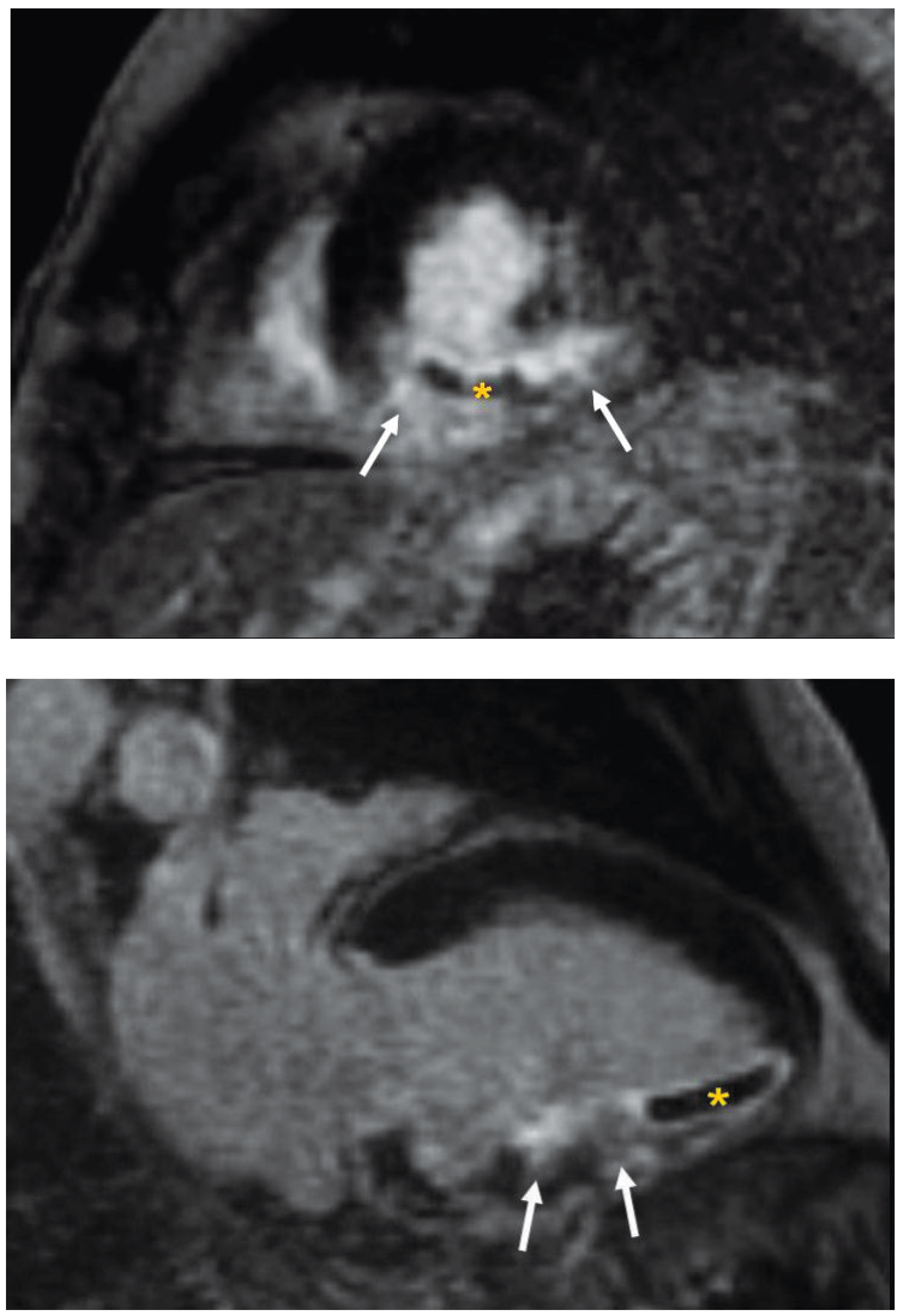
1-weighted contrast-enhanced inversion-recovery gradient echo was used to assess myocardial delayed enhancement obtained 10 minutes after contrast injection. The entire inferior und inferolateral wall showed transmural delayed contrast enhancement with associated microvascular obstruction (MVO) in the distal inferior wall (
Figure 2A,B).
Discussion
Despite sucessful mechanical recanalisation of the infarct-related artery by PCI, perfusion of the ischaemic myocardium is not always completely restored. MVO identified by CMR imaging is a putative mechanism for the no-reflow phenomenon, which is recognised angiographically as slow or no flow in the infarct-related artery despite successful restoration of its patency. MVO has been found to be a predictor of adverse left ventricular remodelling, congestive heart failure and death [
1]. MVO has also been shown to be an important adverse predictor of infarct healing [
2]. In contrast to non-perfused infarcts, reperfusion of ischaemic myocardium with irreversible microvascular damage may lead to intramyocardial haemorrhage, and this has also been shown to be an independent predictor of adverse left ventricular remodelling regardless of the infarct size [
3].
Deoxyhaemoglobin is deemed to shorten the T2 decay time and therefore represents a mechanism for non-invasive detection of intramyocardial haemorrhage, which will appear of low intensity on T2-weighted imaging. Since acute infarction is typically characterised by high signal intensity on T2-weighted imaging, a dark zone within this otherwise bright region can be readily identified and is likely to represent haemorrhage. Besides the unique CMR properties in demonstrating myocardial necrosis, scarring and MVO, this case report also shows the potential of T2-weighted magnetic resonance imaging to identify myocardial oedema with intramyocardial haemorrhage, using the paramagnetic properties of haemoglobin breakdown products.