Abstract
The immune system plays a crucial role in defending the body against foreign invaders, and the balance of various polyunsaturated fatty acids, such as alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), can impact immune cell functions and overall immune responses. This study aimed to assess the effectiveness of mussel oil extracts in modulating inflammatory responses by analysing their effects on immune cell lines and cytokine expression. Four different mussel oil extracts were obtained using two extraction methods (organic solvent and supercritical CO2 extraction) from two tissue sources (fresh and commercial). These extracts were then tested at various concentrations on T lymphocyte (Jurkat) cells, monocytes, and macrophages (THP-1 and U-937). Cytokine levels were quantified using ELISA. The results showed that the solvent-extracted samples had a dose-dependent effect on tumour necrosis factor alpha (TNF-α) and interleukin-1 beta (IL-1β) cytokine secretion in THP-1 and U937 cells, with the extract from a commercial mussel powder being more efficient than the extract from fresh powder. However, supercritical CO2 samples showed elevated cytokine secretion levels despite their high omega-3 content. Furthermore, 100 ug/mL extract from fresh powder successfully reduced interleukin-2 (IL-2) secretion while maintaining cell viability after stimulation. The study demonstrated that solvent-extracted mussel oil can effectively regulate cytokine secretion, modulate immune cell activation, and alleviate inflammation. These findings offer valuable insights into using mussel oil extracts to treat inflammatory disorders and enhance immune responses.
1. Introduction
The immune system is a complex network of cells, chemicals, and processes that protect the body from foreign substances and maintain a healthy balance [1,2]. It comprises an initial nonspecific defence, an innate response, and specific and memory-based protection, the adaptive response [3,4]. The immune system responds to harmful pathogens by activating inflammatory cytokines that recruit immune cells and create effector and memory cells [1,4,5]. Inflammation management relies on macrophages and neutrophils during acute inflammation [6]. Untreated inflammation can trigger the activation of immune cells and lead to tissue damage, resulting in fibrosis, the formation of scar tissue, and the release of cytokines, signalling molecules that can exacerbate inflammation and lead to chronic inflammation and immune system imbalance [7,8]. During this process, lymphoid cells secrete cytokines, while macrophages release pro-inflammatory cytokines and enzymes [9]. The pathological condition involves lymphocyte infiltration, leading to tissue damage and the perpetuation of a persistent, low-grade inflammatory response. Macrophages accumulate in the affected area and act as antigen-presenting cells, releasing pro-inflammatory cytokines and chemokines [9]. Low-grade systemic chronic inflammation and non-communicable disease, recognized as the primary cause of death worldwide, contribute to over 50% of all fatalities. Medical research has established a link between the immune system, inflammatory processes, and various health issues, significantly impacting global morbidity and mortality [10].
The innate immune system triggers an inflammatory response through pattern recognition receptors (PRRs), gradually activating and recruiting immune cells [1,11]. The PRRs start complex pathways for inflammatory signalling and transcription factors upon activation [1,12]. The main pathway activated during the process is NF-κB-mediated inflammatory signalling. The pathway is responsible for regulating well-known target genes, including inducible nitric oxide synthase (iNOS), cyclooxygenase (COX), and various cytokines such as tumour necrosis factor-a (TNF-α), interleukin (IL)-6, and interleukin (IL)-1β [13]. Due to the immune system’s role in chronic illnesses, allopathic medicine has limited options for the treatment and prevention of chronic diseases and immune system imbalances [14]. Numerous studies have explored the impact of natural compounds on these genes, aiming to unravel the molecular mechanisms underlying their anti-inflammatory effectiveness [15].
The body contains various types of omega-3 fatty acids, including free fatty acids (FFA), ethyl ester (EE), phospholipids (PL), and triacylglycerol (TAG) [16]. Among these, PL and TAG are known for their biological properties [17]. The PL form, where FFAs are connected by a glycerol bridge, allows for unique biological functions. Meanwhile, omega-3 TAGs are found in cell membranes alongside PLs [16,18]. These compounds also impact the bioavailability of omega-3. TAGs have a higher bioavailability due to their chemical structure after breakdown, while PLs are more resistant to oxidative stress [16,19]. Omega-3 polyunsaturated fatty acids (PUFAs), such as a-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), have been studied for their regulatory impact on immune function [20,21]. Omega-3 competes with omega-6 fatty acids in enzymatic processes, affecting immune cell activities, integrating into cell membranes, influencing signalling, gene expression, lipid mediator production, and playing a role in gene transcription and lipid metabolism, thereby offering insights into immune modulation [22,23]. This lipid modification plays a crucial role in the functions of both innate and adaptive immune cells by affecting membrane composition, fluidity, and receptor interactions. Imbalances in fatty acid saturation levels and the n-6/n-3 polyunsaturated fatty acid ratio can disrupt the immune system, contributing to various diseases [24].
The New Zealand green-lipped mussel (Perna canaliculus) contains natural components extensively studied in vitro for their immunomodulatory properties [25,26,27,28,29,30] and in in vivo studies [29,31,32,33,34,35,36,37], demonstrating the presence of bioactive components in GLM extracts with immunomodulatory and anti-inflammatory properties. Few studies have explored the potential of GLM oil as an immunomodulatory agent [34]. In vitro experiments using cell lines have shown that GLM oil can modulate inflammatory pathways and cytokine release, specifically reducing the release of pro-inflammatory cytokines such as TNF-α, IL-6, and IL-1β, while also decreasing nitric oxide synthesis [30]. Despite these findings, discrepancies in therapeutic effectiveness persist, potentially due to the lack of standardized extraction and fractionation protocols and the possibility of multiple anti-inflammatory agents within GLM [27].
The research aimed to investigate a sample’s immunomodulatory and anti-inflammatory properties, employing monocytes/macrophages and lymphocyte cell lines. Specifically, the study sought to assess how the sample influenced immune responses, including regulating pro-inflammatory cytokines by monocytes/macrophages and T lymphocytes’ role in coordinating cytokine release. Analysing the activation data of these cells can provide insight into how extracts activate the immune system for pathogen elimination and tissue repair during inflammation. In vitro experiments were performed to investigate the impact of the extracts on immune cell functionality. The primary objective was to identify the type of extract demonstrating the most robust efficacy in regulating inflammatory responses in immune cell lines.
2. Materials and Methods
2.1. Extraction Methods and Characterization of Green-Lipped Mussel Oil
Mussel lipids were extracted using mechanical extraction (CO2 pressure extraction) and chemical extraction. The supercritical CO2 extraction was set at a temperature of 70 °C and a pressure of 500 bar for 2 h, using 150 g of mussel powder. The chemical extraction method was executed according to a protocol described previously [38]. Extracts were dried using a nitrogen flow evaporator and stored at −80 °C after yield quantification. Two different raw mussel powder were used: a commercial powder provided by Nelson Greenshell Mussel Farm, and a laboratory preparation using the lyophilization of live mussels.
Mussel lipid extracts were identified and quantified by thin-layer chromatography using the Iatroscan MK 6s (Iatron Laboratories, Tokyo, Japan). The samples were also analysed for fatty acid methyl esters (FAMEs) using gas chromatography. An aliquot of the lipid extract was subjected to transmethylation, and the resulting FAME samples were analysed in duplicate. Samples were diluted 1, 10, and 100 times. The analysis was performed using an Agilent 7890A gas chromatograph coupled to an Agilent 5975C inert XL mass spectrometer (Agilent Technologies, Santa Clara, CA, USA).
2.2. Green-Lipped Mussel Oil Extract Treatment
Four samples were generated using different extraction methodologies and named accordingly. The samples extracted using organic solvents were marked as “SOLV” and distinguished based on whether they were obtained from a fresh preparation or a commercial brand powder. Similarly, samples extracted using supercritical CO2 were labelled as “CO2” and identified based on the origin of the mussel powder. All samples were initially diluted in 2% absolute ethanol and then in an appropriate medium. The IC50 values were determined by analysing cell viability using a linear regression graph. The treatment concentrations ranged from 12.5 to 800 μg/mL, and the 2% ethanol used for sample dilution did not affect cell viability. The assessment of sample toxicity indicated that exposure to LPS (10 ng/mL) for 24 h did not impact cell viability. However, a concentration of 200 μg/mL generally resulted in up to 70% cell viability. Therefore, to obtain a more accurate assessment of potential sample effects on cell viability within a physiologically relevant range, the focus was on the concentration range of 12.5 to 100 μg/mL for immune cells stimulation.
2.3. Maintenance of Suspension Cells in Culture
The human monocyte THP-1 and U-937 cells and Jurkat T lymphoblast cells were obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). The suspension cells were cultured and sustained in RPMI media supplemented with 10% foetal bovine serum (FBS), 100 units/mL penicillin + 100 μg/mL streptomycin. The cells were incubated at 37 °C in an atmosphere of 5% CO2 and 90–95% humidity. Sub-culturing of the cells was performed every two to three days, not allowing the cell concentration to exceed 1 × 106 cells/mL.
2.4. Monocytes Differentiate into Macrophage Cells
THP-1 and U-937 cells were differentiated into macrophage-like cells (M0THP-1 and M0U-937) by incubation in the presence of 75 ng/mL PMA (Sigma-Aldrich, St. Louis, MO, USA). The cells were counted and seeded in 24-well plates at 200,000 cells/mL for 72 h, followed by washing with PBS and a 24 h rest period in fresh media before exposure to pre-treatment [39].
2.5. MTT Cell Viability to Differentiated Macrophage Cell Lines
Cell viability analysis was conducted on differentiated cell lines of human macrophages (U-937 and TPH-1) using the MTT assay, with triplicate measurements performed for each sample concentration. A 100 µL/well volume was prepared with 5 × 104 cells/mL in 96-well plates. After the differentiation procedure, the samples were diluted in 100 µL and added to the wells 24 h later, followed by incubation for 24 and 48 h. Following medium replacement, MTT was added at a final concentration of 0.5 mg/mL, and the cells were incubated at 37 °C and 5% CO2 for 4 h. Solid particles were dissolved in dimethyl sulfoxide (DMSO) and subsequently measured at a wavelength of 540 nm via a microplate reader. This procedure was replicated at various intervals to ensure accuracy and consistency.
2.6. Monocytes and PMA-Differentiated Cells Stimulation
The THP-1 monocyte and U-937 cells were seeded at a 200,000 cells/mL density in 24-well plates. Following the described protocol, the cells were treated with 75 ng/mL of PMA for 72 h with 24 h of rest. Pre-treatment of the cells (M0THP-1 and M0U-937) with the 4 samples at different concentrations (12.5, 25, 50, and 100 ug/mL) was performed, and after 1 h, they were incubated with LPS at a concentration of 100 ng/mL for 24 h. Dexamethasone at a 1 ug/mL concentration was used as a positive control to assess cytokine suppression. After 6 h of incubation, the plates were centrifuged at approximately 125× g for 5 min, and the supernatants were collected and stored at −80 °C until quantification. The experiment was conducted in duplicate, with each well being tested twice. Additionally, the entire experiment was repeated independently three times.
2.7. Jurkat Cell Line Stimulation
The experimental conditions for Jurkat cell stimulation were established, which involved the utilization of phytohemagglutinin (PHA—2 μg/mL) as the primary stimulant, along with the co-stimulator phorbol myristate acetate (PMA—20 ng/mL) and ionomycin (IoM—350 ng/mL). The cells were enumerated and seeded at 5 × 105 cells/mL density in 24-well plates. Before stimulation, the cells underwent pre-treatment with different concentrations of the samples (12.5, 25, 50, and 100 μg/mL) and were incubated for 1 h. Positive dexamethasone control at a concentration of 1 ug/mL was employed to evaluate cytokine suppression. Subsequently, the cells were exposed to the desired PMA + PHA + ionomycin concentration for 24 h. The plates were centrifuged at approximately 125× g for 5 min to collect the samples, and the supernatants were collected and stored at −80 °C until they were quantified. The experiment was conducted in duplicate, with each well being tested twice. Additionally, the entire experiment was repeated independently three times.
2.8. Apoptosis Assay
Cell apoptosis was evaluated using the Annexin V flow cytometry Kit from Thermo Fisher Scientific Inc. (Waltham, MA, USA) Jurkat cells were collected at a concentration of 5 × 106 cells/mL in a 1.5 mL tube after treatment and stimulation. The cells were centrifuged, and the supernatant was discarded. Subsequently, the cells were washed with PBS and centrifuged at 1000× g for 5 min. After removing the supernatant, the cells were resuspended in 1X Binding Buffer. Subsequently, 5 μL of fluorochrome-conjugated Annexin V was added to 100 μL of the cell suspension and incubated at room temperature for 10 min. Following the manufacturer’s protocol, the cells were analysed for cell apoptosis using a flow cytometer (Guava® Muse® Cell Analyzer, Fremont, CA, USA).
2.9. Enzyme-Linked Immunosorbent Assay (ELISA) of Proinflammatory Cytokines
The contents of TNF-α, IL-1β (monocytes/macrophage cells), and IL-2 (T lymphocyte cells) in the culture supernatants were measured using corresponding ELISA kits (Thermofisher, Waltham, MA, USA), according to the manufacturer’s protocol. Double tests were conducted on each well in the experiment.
2.10. Statistical Analysis
Mean ± SD values were obtained from at least two individual experiments for each triplicate test. One-way ANOVA (analysis of variance) with a post hoc Tukey HSD (honestly significant difference) test was used to assess statistical differences. The independent Student’s test was used to compare means between groups. A p-value of less than 0.05 was considered significant.
3. Results
3.1. Analysing the Lipid Content of Green-Lipped Mussel
The lipid compositions of the four samples varied depending on the preparation and extraction method (Table 1). The SCCO2 method extracted the highest proportion of FFA from powdered samples, yielding approximately 50% of the total lipid classes. Statistical analysis (ANOVA with Tukey’s test) showed a significant difference between samples prepared with commercial powder, with the mechanical extraction method proving more effective in FFA recovery than the organic solvent method (p = 0.014). Remarkably, the chemical method demonstrated superior efficiency in extracting phospholipids, with a 20-fold enhancement compared with SCCO2-extracted samples. The use of MTBE/Me (methyl tert-butyl ether/methanol) was found to be a more efficient strategy for phospholipid recovery (p = 0.001, ANOVA). Triacylglycerol and sterol recovery remained unaffected by the method or sample source, with no significant differences observed.

Table 1.
Classes of lipid recovery during the extraction process. Results are described as average percentages.
GC-MS analysis identified various fatty acids, including saturated, mono, and polyunsaturated types (Table 2). The commercial powder sample yielded the highest FFA content for both extraction methods. The primary FFA in all samples was 5,8,11,14,17-Eicosapentaenoic acid (cis-20:5 n-3, EPA), followed by Palmitic acid (16:0), 4,7,10,13,16,19-Docosahexaenoic acid (cis-22:6 n-3, DHA), and Palmitoleic acid (cis-16:1n-7). The predominant lipid class across all samples was polyunsaturated fatty acids (PUFAs), with omega-3 (Ꞷ-3) being the most abundant subclass. At the same time, the total amount of omega-6 (Ꞷ-6) was consistent for all samples and extraction conditions. Fresh powder exhibited a higher saturated FFA content compared with the commercial sample.

Table 2.
Fatty acid composition of crude oil extract from GLM obtained through two different methods in fresh and commercial powder samples.
Specifically, the commercial sample showed higher levels of 11,14,17-Eicosatrienoic acid (cis-20:3 n-3-ETE, Ꞷ-3), with 21% using SCCO2 and 16% with SOLV. Linoleic acid (cis-18:3 n-3-ALA, Ꞷ-3) had the highest content in commercial samples, but in smaller proportions (3% in solvent and 1.4% in SCCO2). Regardless of the sample, SCCO2 extraction was more effective in EPA recovery (p = 0.0002) than solvent extraction. However, for DHA recovery, the fresh sample was more efficient (p = 0.013), with CO2 being more effective than SOLV. Commercial samples had better recovery rates for some omega-6 FFAs (p = 0.01). Furthermore, the analysis revealed that the fresh crude oil sample contained significantly more monounsaturated fatty acids (MUFAs) than the commercial sample (p < 0.05).
Effects of Mussel Extracts on Cell Viability
The cytotoxicity of crude oils was used to evaluate the potential immunomodulatory effects of mussel oil on immune cells stimulated by LPS. Cell viability was measured after 24 and 48 h of exposure to serial dilutions of stock solutions prepared using supercritical CO2 and solvent oil extraction. Subsequently, 2% ethanol was used for emulsification, and cells treated with ethanol were used as controls. Following 24 h of exposure, no significant decrease in cell viability was observed. However, after 48 h, cell viability was impacted at higher dilutions compared with ethanol, possibly due to a proliferation-activating effect. The highest dilution rate of crude oil samples (100 ug/mL) that did not significantly affect cell viability was selected for further experimentation, consistent with a previous in vitro study [40].
3.2. Immune Cell Response to Mussel Oil
3.2.1. Monocytes
The precursor cells in bone marrow develop into monocytes, which enter connective tissue through capillary walls and transform into macrophages [41]. Monocytes are highly versatile cells that can alter their functional phenotype in response to external stimuli and are often recruited to tissue damage or infection sites [42]. These cells are crucial in inflammatory and homeostatic processes. Scientific evidence suggests that monocytes are the primary source of TNF-α in humans, and their activation is involved in developing various chronic human diseases [43,44].
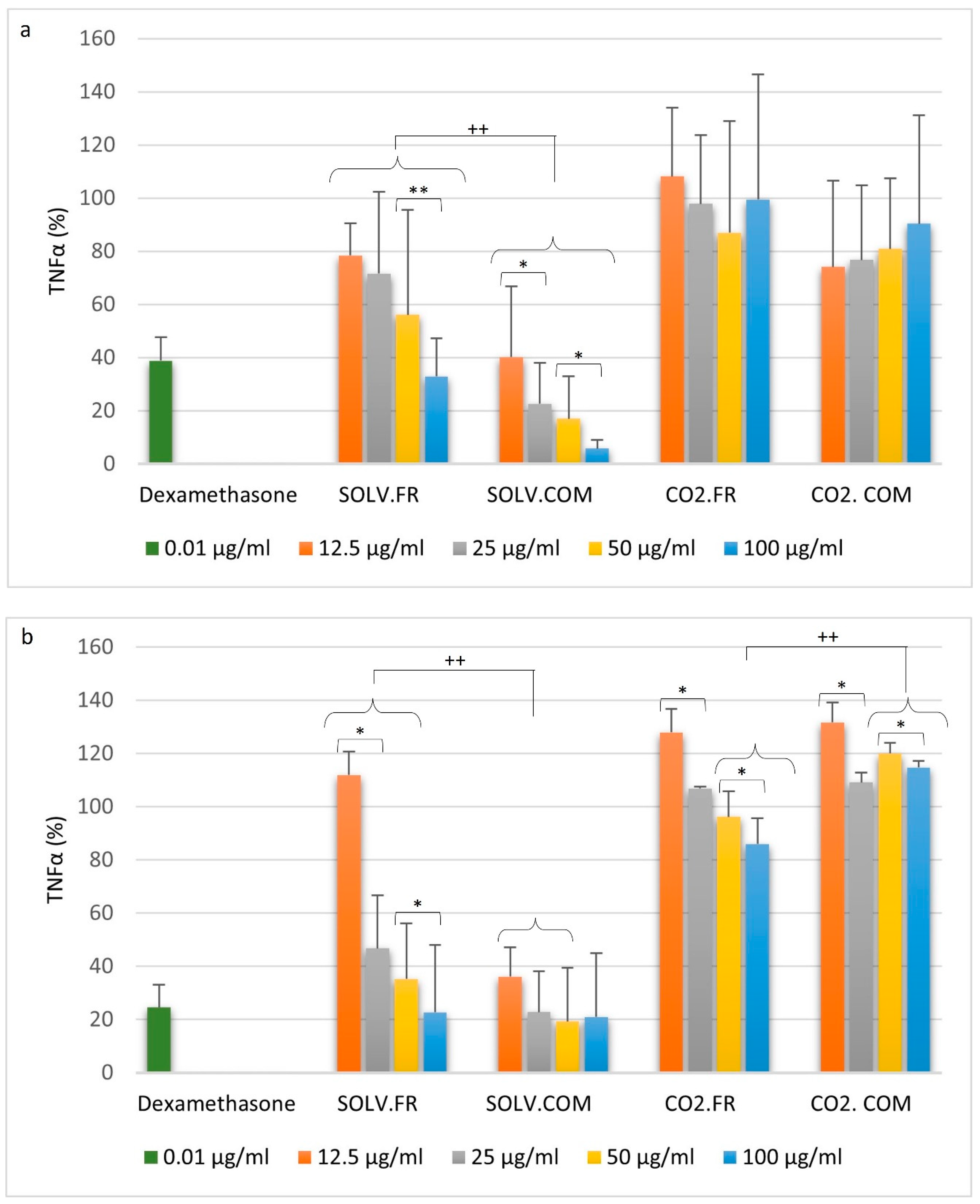
The study involved analysing samples to determine their impact on the expression of cytokines, specifically TNF-α, in cell lines THP-1 and U-937. We observed increased cytokine activity after administering 100 ng/mL of LPS treatment for 6 h. The positive control guided the range of suppression in cytokine secretion. The cytokine bioassay results (Figure 1a) showed that the SOLV samples had a dose-dependent effect on decreasing inflammatory cytokine levels compared with the LPS-treated control. At a concentration of 100 μg/mL of the SOLV.FR (solvent fresh) sample, the release of TNF-α showed a similar reduction to that of the positive control: 38.80 ± 8.8% and 32.89 ± 14.27%, respectively. Other dilutions displayed the potential to suppress cytokine release, although the rate was not comparable to that of the positive control. Nevertheless, the SOLV.COM (solvent commercial) sample showed more efficient management in TNF-α rescue for all dilutions. Treatment with 12.5 μg/mL resulted in a secretion rate of 40.17 ± 26.51%, but the difference from the positive control was not statistically significant. Treatment with 25 μg/mL resulted in a 22.56 ± 15.40% TNF-α secretion rate, which was statistically significant compared with the positive control (p < 0.05, t-test). The highest concentration showed significant cytokine reduction (16.96 ± 15.95% and 11.64 ± 6.30%) with a substantial difference between 50 μg/mL and 100 μg/mL (p = 0.05, Tukey test). In summary, the 25, 50, and 100 μg/mL concentrations of the SOLV.COM sample demonstrated a significant reduction in TNF-α secretion compared with the SOLV.FR dilutions (p < 0.05, Tukey test). The SCCO2 samples did not show a significant decrease in TNF-α release, with some dilutions of both samples presenting an increase in the secretion rate.
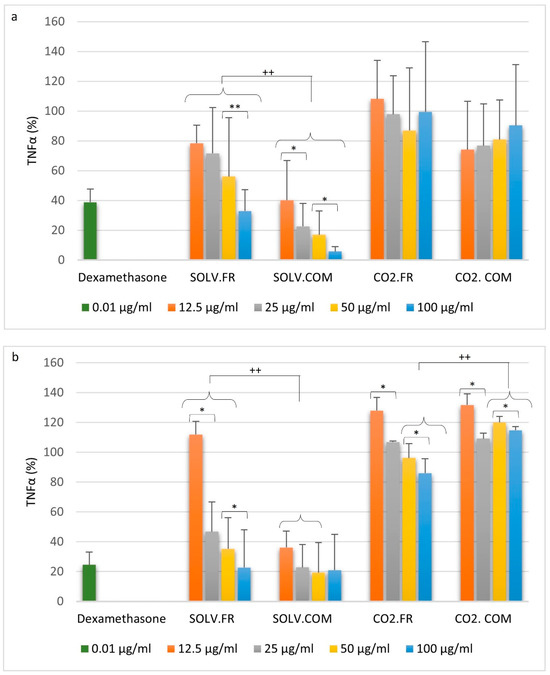
Figure 1.
Effect of crude oil on TNF-α secretion: THP-1 (a) and U937 (b) cells were pre-treated with the following samples: organic solvent—commercial powder (SOLV.COM), organic solvent—fresh powder (SOLV.FR), supercritical—commercial powder (CO2.COM), and supercritical—fresh powder (CO2.FR) in different concentrations then stimulated with LPS (100 ng/mL) for 6 h. Here, 1 μg/mL of dexamethasone was used as a positive control. *, **, indicate p < 0.05 and p < 0.01, respectively, comparing concentrations based on statistically significant differences; ++ indicates a p < 0.001 between-group comparison, demonstrating statistically significant differences by ANOVA and Tukey’s post hoc test.
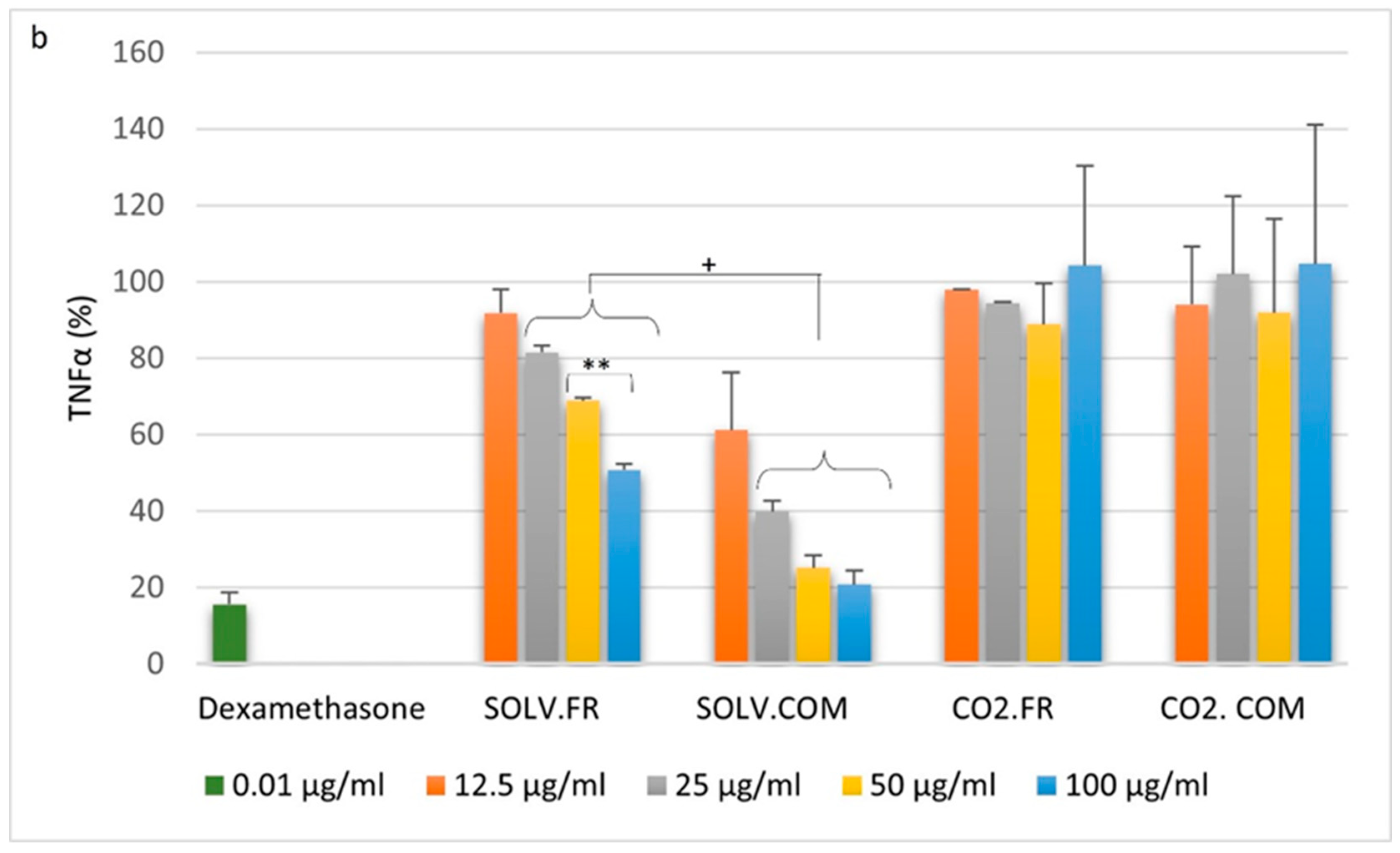
Upon analysing U-937 cells, a comparable pattern was observed in TNF-α secretion in THP-1 cells (Figure 1b). However, it was discovered that 12.5 μg/mL of SOLV.FR did not effectively reduce TNF-α secretion, with a recorded rate of 111.82 ± 8.97% (Figure 1b). Subsequent dilutions displayed a dose-dependent reduction in TNF-α release, with rates of 46.72 ± 19.95%, 35.24 ± 20.82%, and 22.66 ± 25.38%, respectively, and a p-value of 0.05. In contrast, the SOLV.COM sample showed a significant decrease in all concentrations. The four dilutions (12.5, 25, 50, and 100 μg/mL) achieved reduction rates (36.06 ± 10.97%, 22.78 ± 15.26%, 19.28 ± 20.21%, and 20.98 ± 24%, respectively) comparable to the positive control, and did not exhibit any statistical difference between their control rates. In a general comparison of the solvent group, it is possible to affirm that the samples generated by commercial powder have a statistically significant reduction compared with the fresh sample (p < 0.01). The CO2.FR sample also showed a dose-dependent reduction in secretion, although the rates recorded for all dilutions were higher (127.90 ± 8.93%, 106.85 ± 0.63%, 96.17 ± 9.63%, and 85.95 ± 9.60%, respectively) than most solvent samples. Furthermore, the samples obtained from CO2.COM demonstrated increased cytokine secretion across all dilutions, with levels reaching or surpassing the 100% induction rate achieved by the LPS induction control. This result suggests that CO2.COM had a significant impact on the increase in the cytokine production process.
3.2.2. Macrophages
Macrophages are immune cells that can engulf foreign particles and secrete cytokines such as TNF, IL-1, IL-6, IL-8, and IL-12. The purpose of these cytokines is to reinstate tissue homeostasis, and their production must remain balanced for the benefit of the host. Overproduction of these cytokines can trigger acute generalized or systemic chronic inflammation, which can harm the body [41,44].
A preliminary study on THP-1 macrophage cells showed that PMA differentiation followed by a 24 h rest period resulted in a 5-fold reduction in TNF-α production in untreated cells (from 5.812 ± 6.98% to 0.45 ± 1.22%). Treatment with dexamethasone and a 24 h rest period improved TNF-α release compared with no rest, although the difference was not statistically significant (33.56 ± 14.01% to 15.35 ± 19.12%). On the other hand, LPS stimulation led to a substantial increase in cytokine release from cells, with a 400-fold increase in TNF-α secretion after 24 h rest compared with untreated cells. Based on the—results, the following assays used a 72 h PMA incubation period followed by a 24 h rest period.
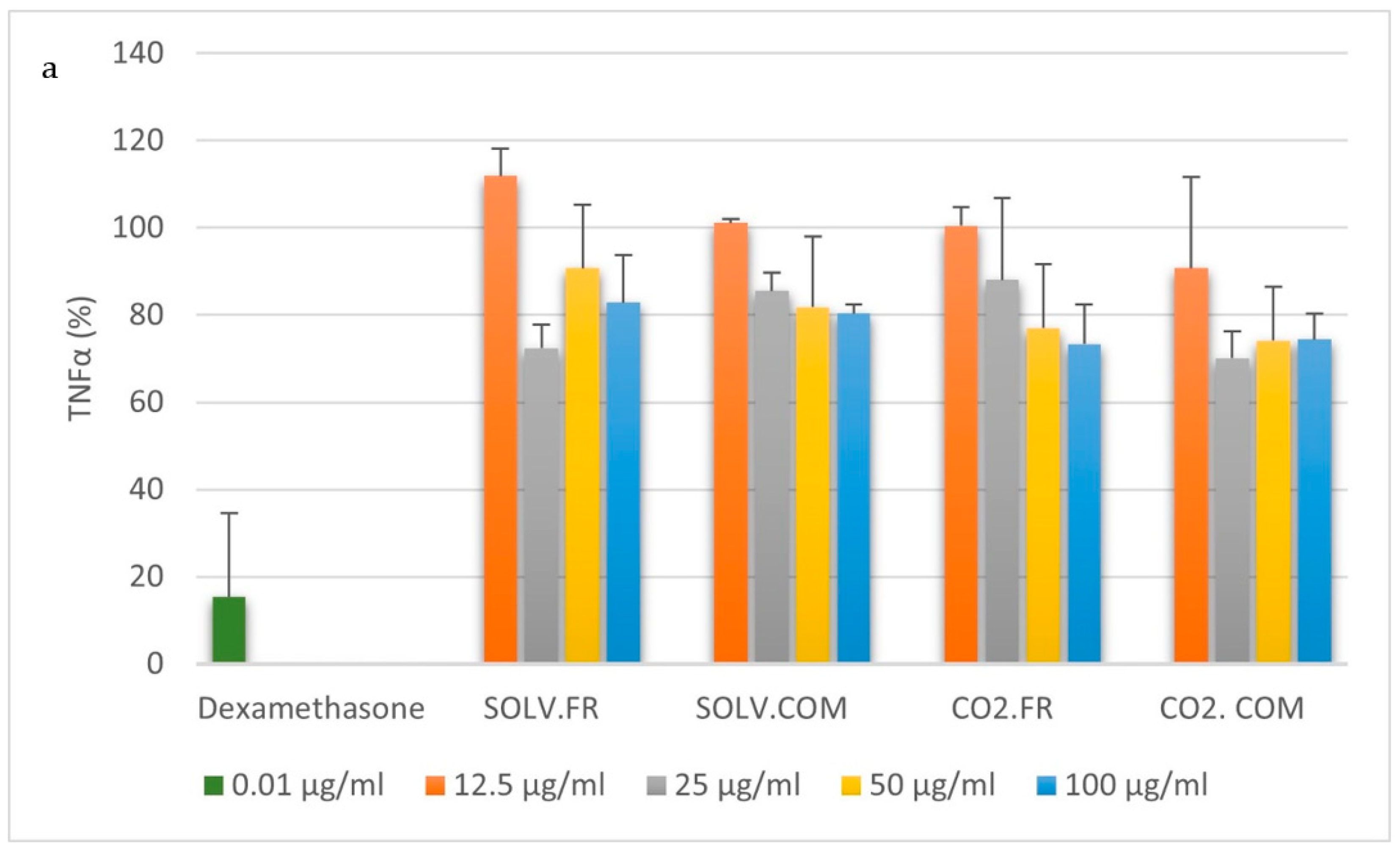
Following the administration of LPS treatment and subsequent M0THP-1 cell stimulation for 6 h, the positive control displayed an average inhibition of TNF-α secretion of 15.35 ± 19.12%. Notably, the samples exhibited reduced cytokine secretion, with the highest decrease recorded at 70.08 ± 6.19% compared with stimulation with LPS. The reduction in cytokine release did not display any statistically significant differences across the various sample dilutions. (Figure 2a). The M0U-937 cells demonstrated an effective suppression of dexamethasone within a range of 15.61 ± 3.18% for TNF-α secretion (Figure 2b). The cytokine expression within this cell line exhibited a response dependent on the dosage of solvent samples applied. The concentration of the solvent sample showed a gradual decrease, as evidenced by the values of 91.78 ± 6.24%, 81.46 ± 1.88%, 68.84 ± 0.95%, and 50.76 ± 1.65% (p < 0.05). However, despite this trend, the highest concentration remained beyond the dexamethasone suppression range. The results of the SOLV.COM sample analysis indicate its promising potential as a cytokine secretion controller. Following treatment with 25 μg/mL and 50 μg/mL oil concentrations, a range of 39.87 ± 2.82% and 25.12 ± 3.25% was achieved, respectively. Notably, the maximum oil concentration of 20.76 ± 3.68% produced a comparable range to the control range. An analysis of raw sources found that the SOLV.COM exhibited greater efficacy in regulating inflammatory processes initiated by LPS in macrophage cells, compared with SOLV.FR samples at concentrations of 25, 50, and 100 μg/mL (p < 0.05). The samples of CO2 did not exhibit a significant impact on the secretion of cytokines in the cells in comparison to the cells stimulated by LPS. The findings indicate that the CO2 samples did not significantly alter immune function. However, additional investigations are required to fully understand the impact of the solvent samples on cytokine production.
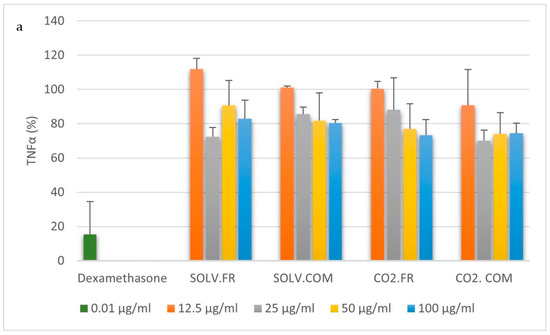
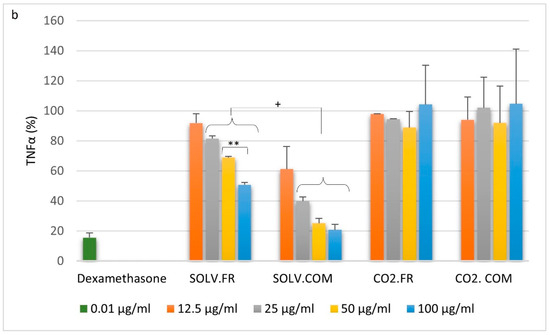
Figure 2.
Effect of crude oil on TNF-α secretion: M0THP-1 (a) and M0U-937 (b) cells were pre-treated with the samples: organic solvent—commercial powder (SOLV.COM), organic solvent—fresh powder (SOLV.FR), supercritical—commercial powder (CO2.COM), and supercritical—fresh powder (CO2.FR) in different concentrations then stimulated with LPS (100 ng/mL) for 6 h. Here, 1 μg/mL of dexamethasone was used as a positive control. ** indicates p < 0.01 comparing concentrations based on statistically significant differences and + indicates p < 0.05 between-group comparisons by ANOVA with Tukey’s post hoc test.
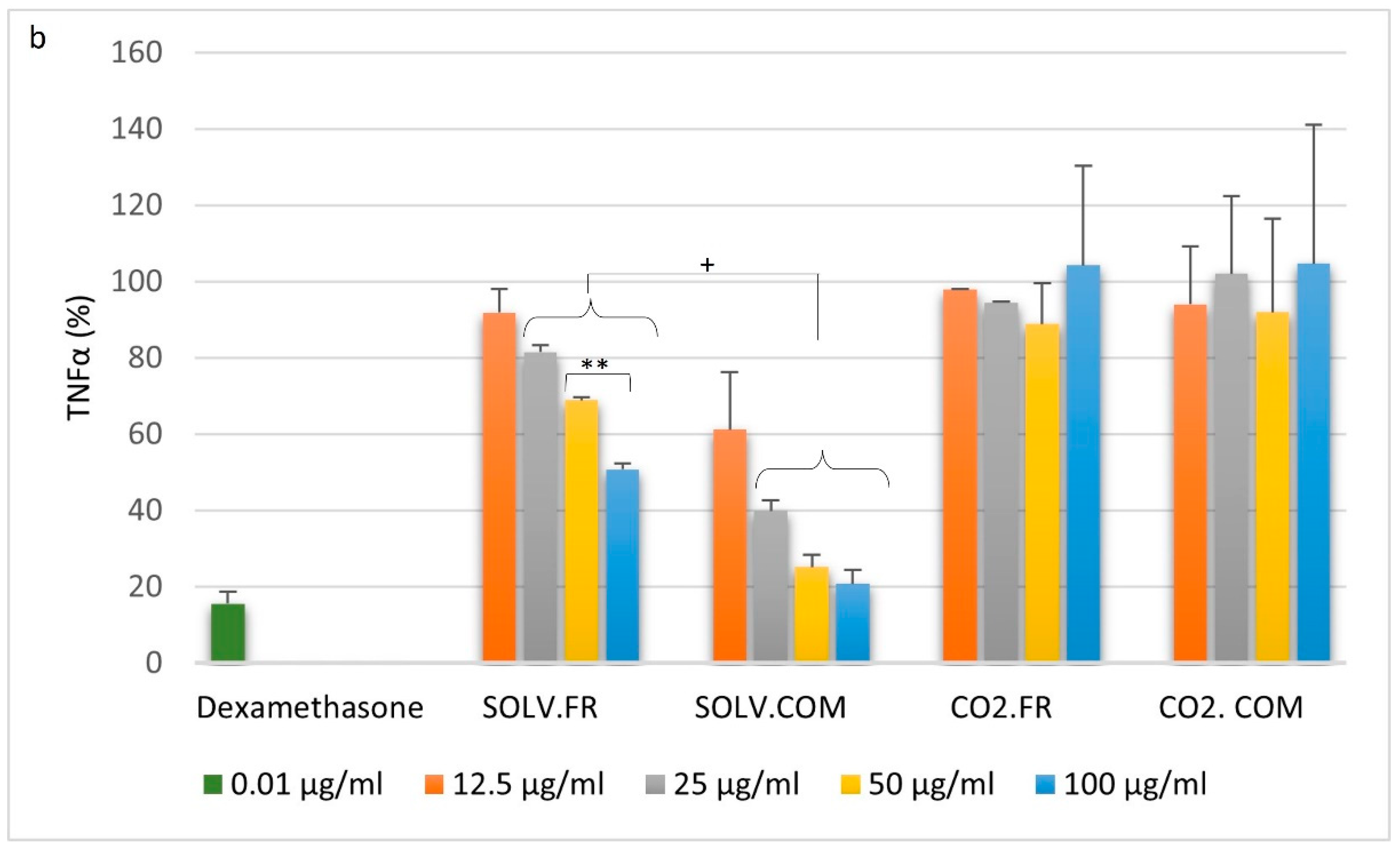
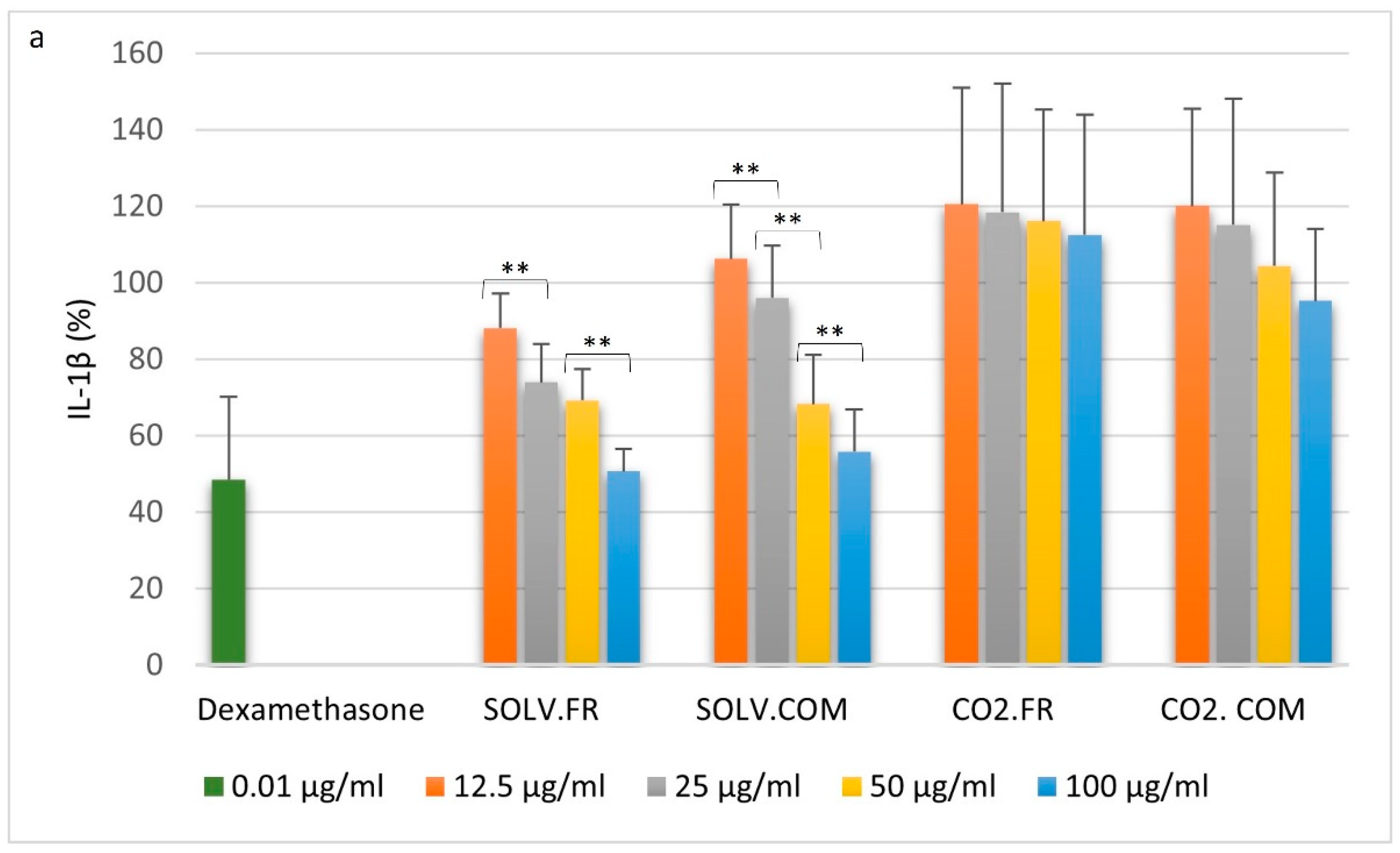
The results of the IL-1β secretion analysis indicated that the effectiveness of dexamethasone in suppressing cytokine release was lower in M0TPH-1 (48.41 ± 21.63%) and M0U-937 (90.94 ± 8.87%) compared with TNF-α (15.35 ± 28.88% and 15.61 ± 3.18%, respectively; p < 0.05) (Figure 3a). The results of the SOLV samples indicate a dose-dependent control of cytokine release. Upon analysis, no statistical difference was detected between the fresh and commercial powder at each respective concentration. The SOLV.FR exhibited a decrease in cytokine secretion range with increasing concentration. A significant difference was observed between the concentrations of 12.5 and 25 μg/mL and 50 and 100 μg/mL (88.05 ± 9.11%, 73.91 ± 9.97%, 69.26 ± 8.04%, and 50.69 ± 5.86%, respectively p < 0.05), while no statistical significance was found in the analysis of 25 and 50 μg/mL concentrations. The same downtrend could be observed in SOLV.COM. The release of cytokine range exhibited differences between concentrations of 12.5 and 25 μg/mL (106.22 ± 14.20% and 95.97 ± 13.68%, p < 0.006). Additionally, significant differences were observed between concentrations of 25 and 50 μg/mL (95.97 ± 13.68% and 68,18 ± 12.94%), as well as between concentrations of 50 and 100 μg/mL (68.18 ± 12.94% and 55.81 ± 11.10%), with a p-value equal to 0.006 (Figure 3a) The samples treated with CO2 exhibited elevated levels of cytokine secretion, regardless of concentration, reaching a level comparable to that of LPS-stimulated cells. These samples did not demonstrate efficacy in blocking the release of IL-1β in the M0THP-1 cell line. The analysis of both SOLV samples revealed that the cytokine suppression range at the highest concentration was similar to that of the positive control. These outcomes suggest that a concentration of 100 ug/mL would effectively regulate cytokine release in the cellular lines under consideration.
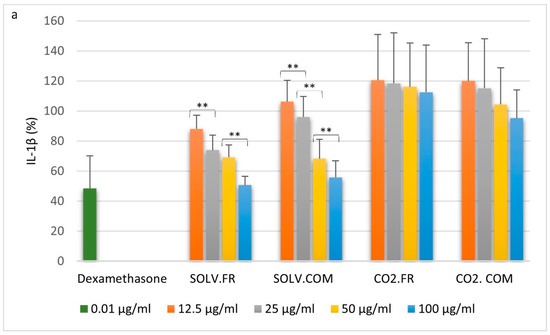
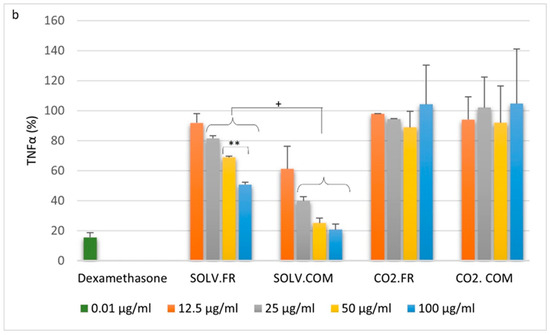
Figure 3.
Effect of crude oil on IL-1β secretion: M0THP-1 (a) and M0U-937 (b) cells were pre-treated with the samples: organic solvent—commercial powder (SOLV.COM), organic solvent—fresh powder (SOLV.FR), supercritical—commercial powder (CO2.COM), and supercritical—fresh powder (CO2.FR) in different concentrations then stimulated with LPS (100 ng/mL) for 6 h. Here, 1 μg/mL of dexamethasone was used as a positive control. ** indicates p < 0.01 comparing concentrations based on statistically significant differences, and + indicates p < 0.05 between-group comparison by ANOVA with Tukey’s post hoc test.
In the context of IL-1β secretion by M0U-937 cells, the analysed SOLV samples displayed a discrete reduction in the percentage of cytokine released (Figure 3b), notwithstanding the higher concentration of samples administered in the treatment of cells stimulated by LPS. In the context of IL-1β secretion by M0U-937 cells, the analysed SOLV samples displayed a discrete reduction in the percentage of cytokine released (Figure 3b), notwithstanding the higher concentration of samples administered in the treatment of cells stimulated by LPS.
The cell line analysis leads to the inference that despite a hesitant decrease in cytokine production, the sample presented a superior result in managing immunomodulation compared to dexamethasone (Figure 3b). The CO2 samples exhibit a similar trend to the TPH-1 results, showing elevated cytokine secretion levels regardless of concentration. The levels of cytokine production in the samples appear to exceed those of LPS-stimulated cells.
3.2.3. T lymphocytes
T lymphocyte cells are a critical component of cellular immunity, as they substantially impact inflammation and immune responses by producing cytokines [45]. During the immune activation, T cells become activated and multiply upon recognizing antigens on macrophage surfaces, which is crucial in regulating inflammatory responses [46]. Studies have demonstrated that delayed inflammatory reactions may be attributed to the interaction of various T cell subtypes, suggesting a potential role for these cells in developing immune-related disorders [45,47]. Among the cytokines these cells release, interleukin-2 (IL-2) promotes T-cell proliferation and differentiation while triggering inflammatory responses [46]. A more comprehensive understanding of cytokine regulation can yield novel therapeutic strategies for various human diseases [46,47].
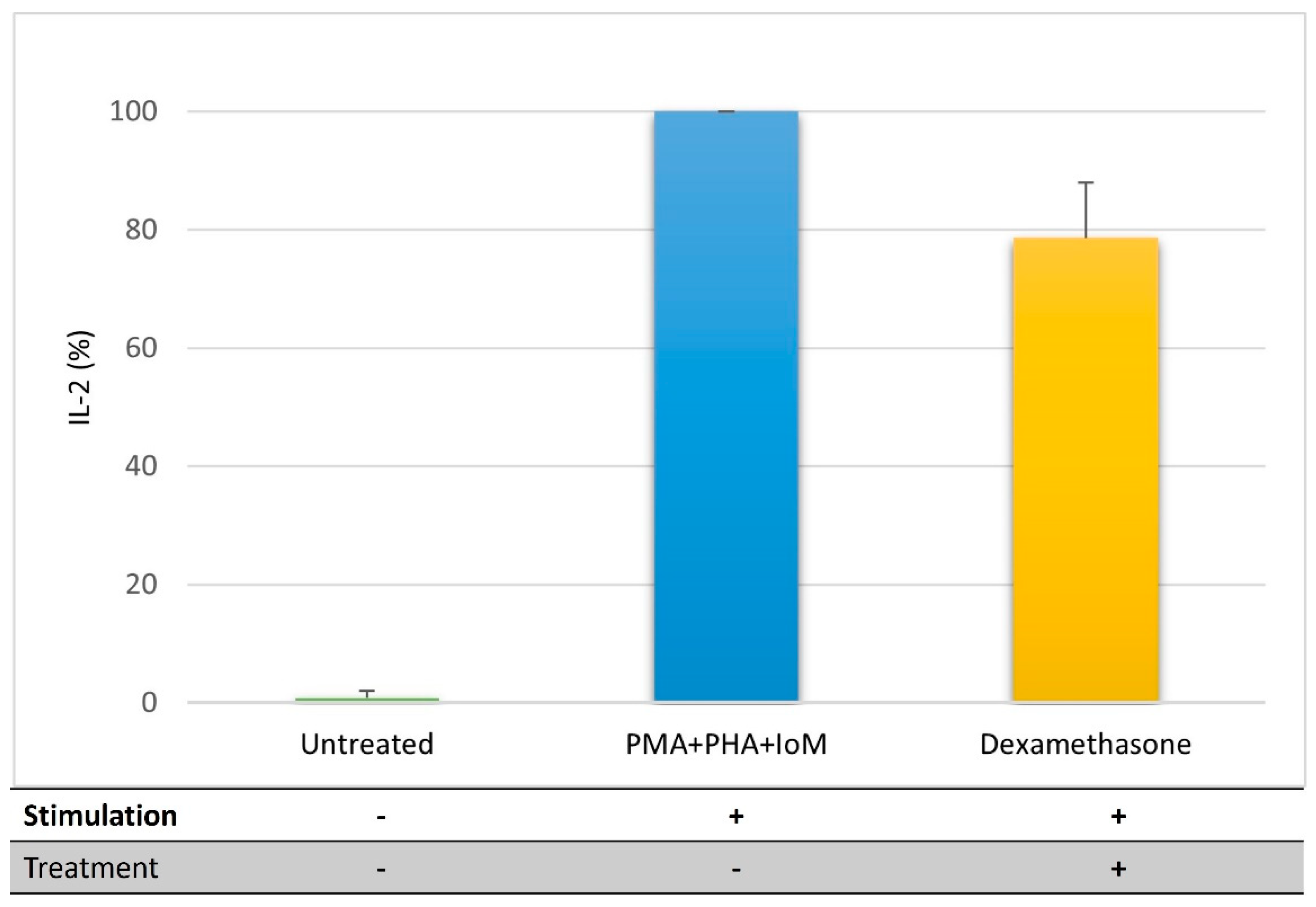
An initial assessment of the controls indicated that using PHA, PMA, and IoM resulted in a substantial elevation in IL-2 discharge in Jurkat cells, reaching 700 times higher compared with untreated cells (Figure 4). However, dexamethasone treatment did not effectively suppress the activation process, leading to a reduction of only 130 times in cytokine secretion, which was less compared with the combination of stimulant substances.
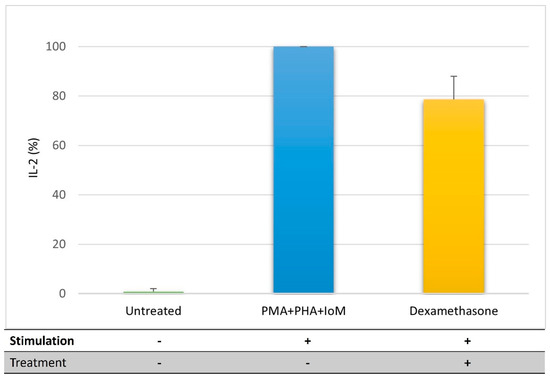
Figure 4.
Efficacy in activating cellular pathways for IL-2 secretion in a T lymphocyte cell line. Untreated—cells with no stimulation or treatment; PMA (20 ng/mL) + PHA (2 μg/mL) + IoM (350 ng/mL—phytohemagglutinin associated with phorbol myristate acetate and ionomycin; Positive control (dexamethasone).
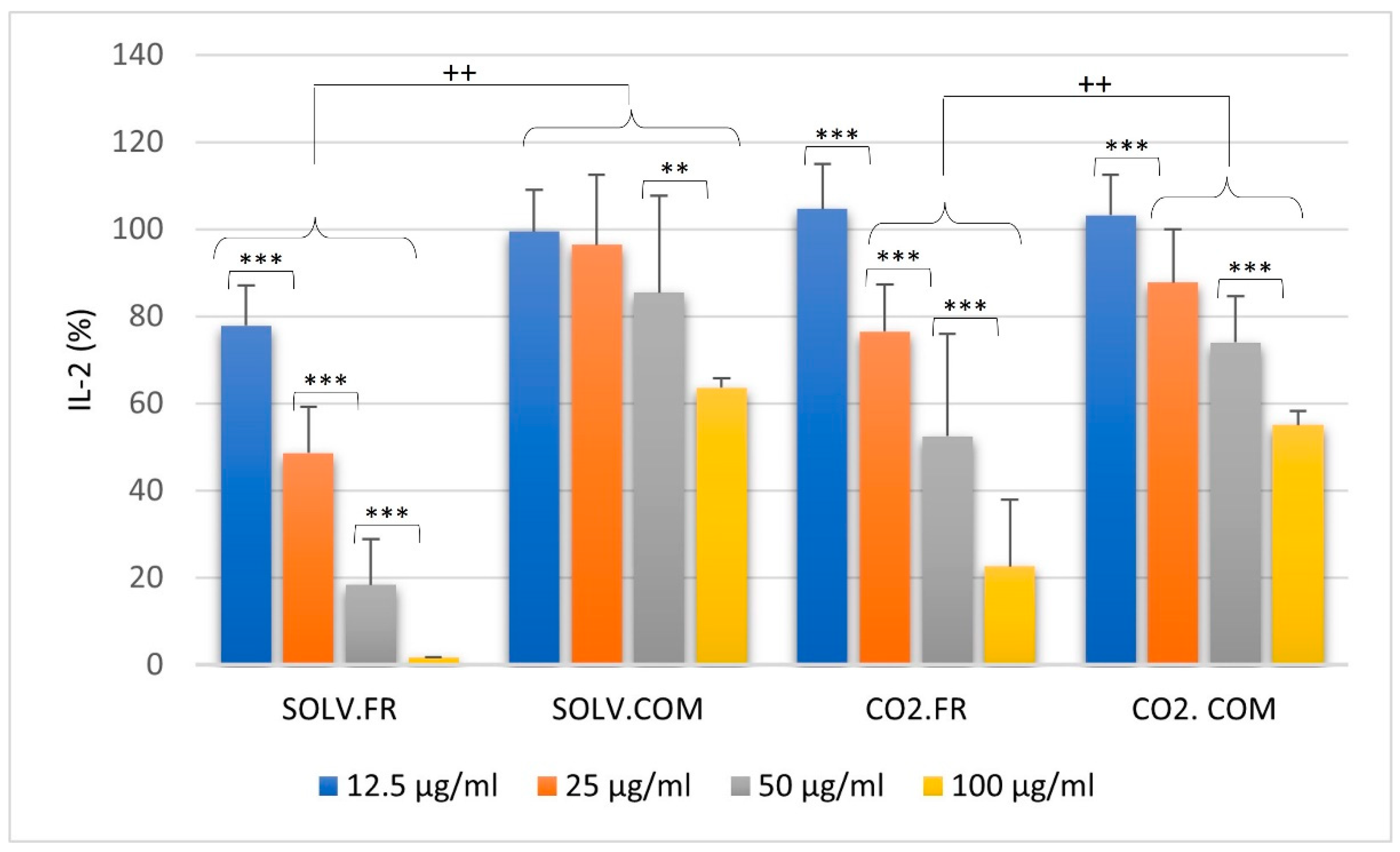
In all the samples presented, there was a trend of dosage dependence (12.5, 25, 50, and 100 μg/mL), where increased concentrations were associated with decreased cytokine secretion (Figure 5). Specifically, the SOLV.FR sample demonstrated a gradual decline in cytokine secretion levels (77.86 ± 9.24%, 48.61 ± 10.60%, 18.31 ± 10.64%, and 1.59 ± 0.08%, respectively, p < 0.001), with its highest concentration yielding a range similar to that of untreated cells. Meanwhile, the SOLV.COM sample proved less effective at suppressing secretion, with its highest concentration (63.63 ± 2.22%) falling within a range resembling that of the positive control (78.65 ± 9.37%). Furthermore, when analysing the powder source for the solvent extraction methodology, it was found that the SOLV.FR sample performed better in regulating lymphocyte cytokine secretion than the SOLV.COM at all concentrations (p < 0.01).
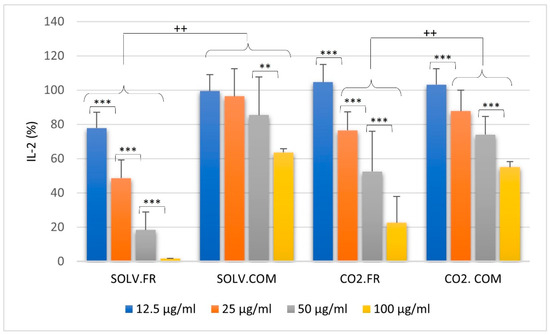
Figure 5.
Effect of crude oil on IL-2 secretion—Jurkat cells were pre-treated with the samples: organic solvent—commercial powder (SOLV.COM), organic solvent—fresh powder (SOLV.FR), supercritical—commercial powder (CO2.COM), and supercritical—fresh powder (CO2.FR) in different concentrations, then stimulated with PMA (20 ng/mL) + PHA (2 μg/mL) + IoM (350 ng/mL) for 24 h. Here, 1 ug/mL of dexamethasone was used as a positive control. ** and *** are p < 0.01 and p < 0.001, respectively, comparing concentrations based on statistically significant differences and ++ indicates p < 0.01 between-group comparison by ANOVA with Tukey’s post hoc test.
The CO2 samples with a concentration of 12.5 μg/mL did not have any noticeable effect in controlling the activation mechanisms of cellular pathways that lead to IL-2 release. Both samples maintained a range similar to the set of stimulators, with percentages of 104.64 ± 10.38% and 103.23 ± 9.26%. The CO2.FR sample showed a similar trend to the SOLV.FR sample. Still, it was less effective in suppressing the IL-2 release by Jurkat cells at concentrations of 25, 50, and 100 μg/mL (76.47 ± 10.78%, 52.43 ± 23.53%, and 22.59 ± 15.24%, respectively, p < 0.01). In comparison, the CO2.COM sample at the same concentrations had a more subtle suppression in the release (87.73 ± 12.29%, 73.95 ± 10.64%, and 55.09 ± 3.23%, respectively, p < 0.01). The highest concentration yielded better results for both samples than the positive control. This extraction methodology has shown similar performance in regulating lymphocyte IL-2 secretion, as observed in the solvents, with fresh samples exhibiting better regulation than commercial samples, except for the 12.5 μg/mL concentration (p < 0.01).
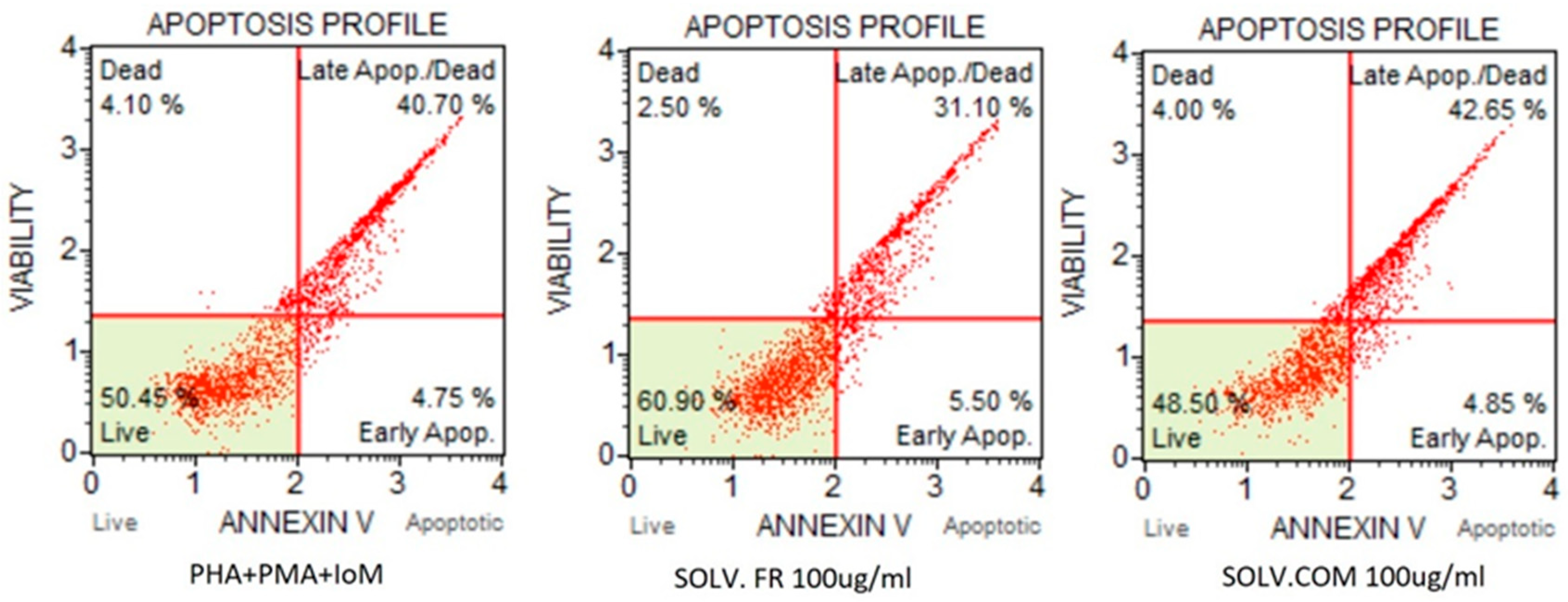
During the investigation into the apoptotic assay, it was observed that cell viability was decreased by 48% after stimulation treatment (Figure 6). Cell viability was assessed by treating the cells with SOLV samples to determine whether cytokine secretion was possible. The results revealed that fresh powder samples caused fewer late apoptotic cells (31.10%) than stimulated control cells. However, the dead cells were slightly decreased by commercial samples (42.65%). After a thorough analysis, it was observed that the decrease in IL-2 secretion in the fresh samples did not result from reduced cell viability post stimulation. As a result, it can be deduced that the SOLV.FR samples successfully reduced IL-2 stimulation while simultaneously maintaining cell viability.
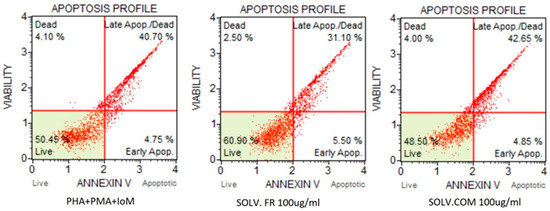
Figure 6.
Annexin V flow cytometry analysis for lymphocyte T cells after stimulation and pre-treatment with the samples: organic solvent—fresh powder (SOLV.FR), organic solvent—commercial powder (SOLV.COM).
4. Discussion
4.1. Impact of GLM Oil on Inflammation and Immune Regulation
As previously noted, inflammation is a natural immune response to combat invading pathogens, but it can also have detrimental effects when left uncontrolled. To effectively manage infections and restore tissue integrity, it is paramount to have a comprehensive understanding of the various types of immune cells and the factors that contribute to bolstering the immune system. This knowledge lets us discern disease patterns and re-compose the immune system’s health. The balance between saturated and unsaturated FAs is crucial for the functions of innate and adaptive immune cells, as it affects their membrane composition, fluidity, and interactions with specific receptors [2,12]. Disruption of FA saturation levels and the ratio of n-6/n-3 polyunsaturated FAs can lead to immune system imbalances and contribute to various diseases [24]. In analysing the impact of dietary fat composition on immune cell fluidity, crude oil containing various fatty acids could influence cytokine production and cell activity.
Some studies have demonstrated that the primary source of anti-inflammatory effectiveness in mussel oil is mainly found within the free fatty acids section of the oil. The most remarkable efficacy is observed within the polyunsaturated fatty acid (PUFA) category [26]. Extracting oils from whole GLM involves a multitude of complex and diverse lipids. As a result, a meticulous screening and purification process is necessary to isolate and identify the valuable bioactive compounds within the oil extracts. Although this procedure may take some time, it is crucial for obtaining high-quality results [27]. Moreover, the instability of specific bioactive compounds during oil extraction creates an additional challenge. Some lipid-based bioactive compounds require further investigation, which requires additional research to identify potential bioactive components and understand the mechanisms responsible for GLM oil’s impact on chronic inflammation-related conditions [30]. Persisting disparities in therapeutic efficacy observed across studies may result from multiple anti-inflammatory mediators in GLM. Consequently, the isolation and purification of specific oil components may not always represent optimal strategies, hypothetically overlooking the inclusion of undiscovered potential bioactive compounds [27]. The present study utilizes crude oil extracts to investigate the intricate interplay of diverse bioactive compounds through various extraction techniques.
In the inflammatory process, pro-inflammatory cytokines such as TNF-α, IL-6, and IL-1β play a significant role in the development of the inflammatory process [48]. In prior studies, the suppression of TNF-α and interferon (IFN)-γ expression by GLM oil was observed in an adjuvant-induced arthritis model in rats [33], as well as the inhibition of TNF-α and IL-12 expression in LPS-induced human THP-1 monocytes [25]. Additionally, Chen et al. (2017) demonstrated GLM oil’s inhibitory effect on TNF-α, IL-6, and IL-1β expression levels in LPS-stimulated macrophage RAW264.7 cells through ELISAs [30]. The anti-inflammatory properties of GLM oil have been attributed to its ability to modulate the NF-κB and MAPK signalling pathways in cells. These revelations provided a deeper understanding of the underlying mechanisms behind the anti-inflammatory efficacy of GLM oil [30]. According to a recent study, GLM oil extract has the potential to reduce inflammation, enhance glucose uptake, and effectively manage the release of inflammatory markers, namely, IL-6 and MMP-3, on human chondrocyte cell lines. This highlights the promising role of SOLV.COM in controlling reactive oxygen production, regulating glucose metabolism, and managing OA [40].
4.2. Comparative Analysis of Immune Modulation by GLM Lipid Extracts
The study of immune system regulation can be challenging when attempting to simulate the human system. Typically, peripheral blood mononuclear cells (PBMCs) are used to evaluate immune cell functions in metabolic disorders [49]. However, there are limitations associated with the utilization of human stem cells, such as ethical concerns with PBMCs [50]. The most significant factors that affect the use of PBMCs are accessibility to the material and higher inherent variability across donors. In this context, cell lines offer a reliable model for investigating immune cell functions, responses, and differentiation [51].
By virtue of their relative consistency and ease of handling, cell lines present a reliable tool for researchers seeking to study the complex workings of immune cells. Based on Riddy et al.’s (2018) data analysis, it was found that THP-1 and U-937 cells had a more similar protein expression pattern compared to PBMCs, especially after differentiation. However, the absolute expression levels varied considerably. The study concluded that most of the analysed genes were expressed similarly across cells, except for IL-6, which exhibited variation [49]. THP-1 and U937 cell lines are commonly used as macrophage precursor models in immunology research due to their ability to mimic macrophage differentiation and exhibit similarities to primary monocytes and macrophages [52]. According to Nascimento et al. (2022), in vitro studies using cell lines offer valuable insights into immune cell biology and its significance in different contexts, despite their inherent limitations [52].
Upon further examination of the literature review, it appears that there may be variations in mRNA levels during monocyte differentiation between immortalized and primary cells. However, for screening, it is feasible to use the immune cell line in the immunomodulation study. Considering the published data, it was decided to evaluate the impact of TNF-α and IL-1β expression levels on LPS-stimulated monocyte/macrophage THP-1 and U937 cell lines after treatment with GLM lipid extracts.
Furthermore, we delved deeper into the immunomodulatory function of IL-2 samples by examining their effects on lymphocyte Jurkat cells. Our findings provide valuable insights into the potential therapeutic applications of these samples in the context of immune system regulation. THP-1 and U-937 monocytes/macrophage cell lines were exposed to bacterial LPS, while the Jurkat T-cell line was exposed to a combination of stimulants (PHA, PMA, and IoM). The levels of cytokines released in the cell-cultured medium were measured, and the extract’s ability to modulate the synthesis of TNF-α, IL-1β, and IL-2 in a dose-dependent manner was analysed. The research data analysis indicates that the samples generated through solvent extraction effectively regulate immunity. Specifically, these samples demonstrated a reduction in TNF-α secretion in both TPH-1 and U-937 cell lines (monocytes and macrophages) after LPS stimulation. Furthermore, a dose-dependent effect was observed in the monocyte cells treated with these samples and in U-937 macrophage cells. Although the same samples also successfully decreased IL-1β secretion with increased concentration, this difference was not statistically significant for M0U-937. Upon analysing the powder source, it was found that both fresh and commercial samples had comparable effects on cells, exhibiting only minor variations between concentrations. During lymphocyte stimulation, it was observed that the solvent samples were also capable of managing immune regulation. Notably, the SOLV.FR samples outperformed those from SOLV.COM in this cell line.
4.3. Understanding Immune Modulation and Inflammation through GLM Extract Composition
The compositional analysis of the oil samples revealed that those obtained through solvent extraction demonstrated a higher ratio of n-3 to n-6, along with notable levels of palmitic acid (16:0), 20:5 n-3 (EPA), and 22:6 n-3 (DHA). Moreover, these samples exhibited a higher concentration of polar and negatively charged phospholipids, setting them apart from other samples.
The study results indicated that cytokine secretion levels were increased in monocytes/macrophage cells following treatment with CO2 samples, regardless of concentration. This suggests that despite containing a high concentration of omega-3, these oils may increase cytokine production, which goes against the initial expectation that the highest omega-3 concentration can suppress the inflammatory process in these cells. On the other hand, SOLV samples were more effective in managing cytokine secretion and promoting better immunomodulation. Phospholipids comprise glycerol, fatty acids, phosphate groups, and hydrophilic residues. These lipids have proven highly effective in providing fatty acid components for cell membranes [53]. A previous study indicated that incorporating this lipid group into immune cell membranes may result in an internal negative charge profile, leading to a dynamic equilibrium of T immune cells due to changes in transmembrane proteins’ activities [54]. Furthermore, other research suggests that this charge profile may activate an innate immune response in the macrophage cell cascade, which aids in controlling infection [55]. It has been suggested that supplementing with high-w-3 phospholipids can modulate the lipidome, proteome, and metabolome of macrophages, influencing multiple metabolic pathways in the immune response caused by inflammation [56]. In the future, conducting a thorough analysis of the phospholipid composition in mussel extracts could offer valuable information on whether this substance affects the immune cells’ immunomodulatory functions.
4.4. Effects of Fatty Acid Ratios on Immune Cells and Cytokine Regulation
Regarding the lipid composition of the samples, the n-3/n-6 ratio exceeds the recommended levels in the literature for maintaining health and preventing the onset of chronic low-grade inflammation. A systemic review revealed that the omega 3/omega 6 acid ratio in tissues significantly impacts chronic diseases and influences the microbiome in a transgenic mouse model, leading to various health disorders [57,58]. Thus, maintaining an appropriate balance in the dietary n-3/n-6 ratio is crucial to prevent excessive and prolonged inflammatory responses that may result in tissue damage and potential autoimmune disease [24,59].
Although studies suggest that the ratio of omega 3 to omega 6 can affect inflammation, this was not observed in the CO2 samples. These samples had a higher n-3/n-6 ratio than the solvent samples but did not reduce cytokine secretion from monocytes/macrophages. The results of the testing have revealed that there was a level of regulation in the release of IL-2 from the lymphocytes. However, it was found to be less efficient compared with the supernatant of cells that were treated with solvent samples.
Based on the conducted experiments, it has been observed that the extraction of varied samples from mussels could activate inflammatory cytokine pathways in immune cells in vitro. A 2021 study by Semenoglou et al. highlighted that crude oils obtained through supercritical CO2 extraction might contain impurities such as moisture, volatile compounds, proteins, minerals, and oxidation products. These impurities’ presence and extent depend upon the chosen extraction method and conditions. Interestingly, the study found that higher temperature and pressure during extraction resulted in greater oil yield and FA concentration. However, this also led to increased oxidation compared with conventional extracts. To avoid this issue, they suggest refining treatment as an effective way to remove impurities and increase the content of MUFA and PUFA. This study sheds light on the importance of refining techniques in the extraction process to ensure the purity and nutritional quality of the final product [60].
Upon examination of the regulation of IL-2 secretion, it has been observed that samples in the supercritical state display greater efficacy in reducing the release of this cytokine compared with the secretion of cytokines studied in monocytes and macrophages. Cytokine release may be initiated through various cellular receptors, including pattern recognition receptors such as TLRs and immunoglobulin- or complement-receptor-mediated signalling that pathogens may activate. Consequently, soluble mediators such as TNF-α, IL-1, and IL-2 are secreted through the activation of nuclear-factor- and NF-κB-mediated transcription activation [12]. Once the stimulatory agent for these cells triggers different receptors (TLRs in monocytes/macrophages and TCR in lymphocyte cells), incorporating FFA in the cell membrane could affect the pathways differently and generate different responses.
The fatty acid composition analysis of the samples Indicates that higher DHA concentrations can impact lymphocyte activation. This is evident in the data concerning IL-2 release control through the oils generated by fresh powder, where the solvent and CO2 contain higher DHA concentrations (18.04% and 18.34%, respectively) in comparison to commercial values (7.23% and 9.05%, for solvent and CO2, respectively). Verlengia et al. (2004) discovered that different fatty acids, including DHA and EPA, can modify the expression of a significant portion of genes, affecting signal transduction pathway activation and other cell functions. Their research showed that DHA and EPA reduced the production of IL-2 and INF-γ, whereas only EPA decreased the production of IL-10 [61].
Incorporating DHA and EPA into the diet has been shown to have health benefits. Other free fatty acids (FFAs), such as linoleic acid, have also been found to positively affect the body. It is widely recognized that including mono-unsaturated fatty acids, particularly oleic acid, in the diet can have physiological benefits and reduce the risk of chronic diseases [62,63]. Studies have demonstrated that the mechanisms of action of FFA vary depending on the cell type, impacting cellular signalling and functions [24]. Therefore, developing extracts containing a balanced combination of different FFA can benefit various cell types, including immune cells.
This initial analysis of the immune cell activation data can show which extract has the potential to be an anti-inflammatory agent and can activate the immune system effectively. Identifying and characterizing the properties of these extracts could lead to the development of more focused and efficient treatments for chronic inflammatory disorders, thus improving patient outcomes. GLM oils could potentially reduce TNF-α and IL-1β expression, contributing to anti-inflammatory responses. Additionally, the extracts can regulate lymphocyte cells and impact immune cell membranes and inflammatory pathways. The study found that the extraction method and the sample’s origin can impact the immuno-modulatory efficacy of the extracted oil. The results suggest that lipids derived from mussels through organic solvents can modulate cytokine secretion in TPH-1, U-937, and the Jurkat cell lines that have been treated. This indicates that these extracts may be effective therapeutic agents for managing inflammation and regulating immune cell activation. In summary, analysis of the data indicates that SOLV samples exhibit potential as a promising therapeutic agent for conditions arising from imbalances in the immune system.
Author Contributions
R.C.L. contributed to the conception, design, and statistics and drafted the manuscript; B.E. contributed to the conception, design, and revision of the manuscript; H.L. contributed to the methodology, supervision and revision of the manuscript. X.G. contributed to the funding, resource and revision of the manuscript; Y.L. contributed to the conception, supervision and critically revised the manuscript; and J.L. contributed to the conception, supervision, resource and critically revised the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the study. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Science Challenge, High Value Nutrition Fund, grant number HVN-1905. China Ministry of Education 2023 National Foreign Experts Programme, DL2023013002.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated for this study will be made available via reasonable request to the corresponding author.
Acknowledgments
Auckland University of Technology Doctoral Scholarships for Lessa, R.C.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Müller, L.; Di Benedetto, S.; Pawelec, G. Human Immune System in Aging. In Encyclopedia of Gerontology and Population Aging; Springer: Cham, Switzerland, 2019; pp. 1–12. [Google Scholar] [CrossRef]
- Margraf, A.; Perretti, M. Immune cell plasticity in inflammation: Insights into description and regulation of immune cell phenotypes. Cells 2022, 11, 1824. [Google Scholar] [CrossRef] [PubMed]
- Chaplin, D.D. Overview of the immune response. J. Allergy Clin. Immunol. 2010, 125 (Suppl. S2), S3–S23. [Google Scholar] [CrossRef]
- Calder, P.C. Immunomodulation by omega-3 fatty acids. Prostaglandins Leukot. Essent. Fat. Acids 2007, 77, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.S.; Warrington, R.; Watson, W.; Kim, H.L. An introduction to immunology and immunopathology. Allergy Asthma Clin. Immunol. 2018, 14 (Suppl. S2), 49. [Google Scholar] [CrossRef] [PubMed]
- Butterfield, T.A.; Best, T.M.; Merrick, M.A. The dual roles of neutrophils and macrophages in inflammation. J. Athl. Train. 2006, 41, 457–465. [Google Scholar] [PubMed]
- Luster, A.D.; Alon, R.; von Andrian, U.H. Immune cell migration in inflammation: Present and future therapeutic targets. Nat. Immunol. 2005, 6, 1182–1190. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, N.; Kobayashi, K. Macrophages in Inflammation. Curr. Drug Targets Inflamm. Allergy 2005, 4, 281–286. [Google Scholar] [CrossRef]
- Germolec, D.R.; Shipkowski, K.A.; Frawley, R.P.; Evans, E. Markers of Inflammation. Methods Mol. Biol. 2018, 1803, 57–79. [Google Scholar] [CrossRef]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef]
- Newton, K.; Dixit, V.M. Signaling in innate immunity and inflammation. Cold Spring Harb. Perspect. Biol. 2012, 4, a006049. [Google Scholar] [CrossRef]
- Lacy, P.; Stow, J.L. Cytokine release from innate immune cells: Association with diverse membrane trafficking pathways. Blood J. Am. Soc. Hematol. 2011, 118, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Hawiger, D.; Inaba, K.; Dorsett, Y.; Guo, M.; Mahnke, K.; Rivera, M.; Ravetch, J.V.; Steinman, R.M.; Nussenzweig, M.C. Dendritic cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. J. Exp. Med. 2001, 194, 769–779. [Google Scholar] [CrossRef] [PubMed]
- Haddad, P.S.; Azar, G.A.; Groom, S.; Boivin, M. Natural health products, modulation of immune function and prevention of chronic diseases. Evid.-Based Complement. Altern. Med. 2005, 2, 513–520. [Google Scholar] [CrossRef]
- Murakami, A.; Ohigashi, H. Targeting NOX, INOS and COX-2 in inflammatory cells: Chemoprevention using food phytochemicals. Int. J. Cancer 2007, 121, 2357–2363. [Google Scholar] [CrossRef]
- Afroze, S.; Janakiraman, A.K.; Gunasekaran, B.; Djearamane, S.; Wong, L.S. Potentials of omega-3 fatty acids as therapeutic drugs and its obstacles in the pathway: A critical review. J. Pharm. Pharmacogn. Res. 2024, 12, 120–145. [Google Scholar] [CrossRef]
- Minton, S.T.; Almada, A.L.; Evans, J.L.; Laidlaw, M.; Opheim, J. Comparative membrane incorporation of omega-3 fish oil triglyceride preparations differing by degree of re-esterification: A sixteen-week randomized intervention trial. PLoS ONE 2023, 18, e0265462. [Google Scholar] [CrossRef]
- Barchi, J.J., Jr.; Strain, C.N. The effect of a methyl group on structure and function: Serine vs. threonine glycosylation and phosphorylation. Front. Mol. Biosci. 2023, 10, 1117850. [Google Scholar] [CrossRef]
- Cholewski, M.; Tomczykowa, M.; Tomczyk, M. A Comprehensive Review of Chemistry, Sources and Bioavailability of Omega-3 Fatty Acids. Nutrients 2018, 10, 1662. [Google Scholar] [CrossRef]
- Yaqoob, P.; Calder, P.C. Fatty acids and immune function: New insights into mechanisms. Br. J. Nutr. 2007, 98, S41–S45. [Google Scholar] [CrossRef]
- Utami, K.P.; Wasityastuti, W.; Soesatyo, M.H. The Involvement of Lipids in Immune System Regulation: A Mini-Review. JKKI J. Kedokt. Dan Kesehat. Indones. 2021, 12, 68–78. [Google Scholar] [CrossRef]
- Gutiérrez, S.; Svahn, S.L.; Johansson, M.E. Effects of omega-3 fatty acids on immune cells. Int. J. Mol. Sci. 2019, 20, 5028. [Google Scholar] [CrossRef]
- Johnson, W.T.; Dorn, N.C.; Ogbonna, D.A.; Bottini, N.; Shah, N.J. Lipid-based regulators of immunity. Bioeng. Transl. Med. 2022, 7, e10288. [Google Scholar] [CrossRef]
- Radzikowska, U.; Rinaldi, A.O.; Celebi Sozener, Z.; Karaguzel, D.; Wojcik, M.; Cypryk, K.; Akdis, M.; Akdis, C.A.; Sokolowska, M. The Influence of Dietary Fatty Acids on Immune Responses. Nutrients 2019, 11, 2990. [Google Scholar] [CrossRef]
- Lawson, B.R.; Belkowski, S.M.; Whitesides, J.F.; Davis, P.; Lawson, J.W. Immunomodulation of murine collagen-induced arthritis by N, N-dimethylglycine and a preparation of Perna canaliculus. BMC Complement. Altern. Med. 2007, 7, 20. [Google Scholar] [CrossRef] [PubMed]
- McPhee, S.; Hodges, L.D.; Wright, P.F.; Wynne, P.M.; Kalafatis, N.; Harney, D.W.; Macrides, T.A. Anti-cyclooxygenase effects of lipid extracts from the New Zealand green-lipped mussel, Perna canaliculus. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2007, 146, 346–356. [Google Scholar] [CrossRef]
- Mani, S.; Lawson, J.W. In vitro modulation of inflammatory cytokine and IgG levels by extracts of Perna canaliculus. BMC Complement. Altern. Med. 2006, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Treschow, A.P.; Hodges, L.D.; Wright, P.F.; Wynne, P.M.; Kalafatis, N.; Macrides, T.A. Novel anti-inflammatory omega-3 PUFAs from the New Zealand green-lipped mussel, Perna canaliculus. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2007, 147, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, M.W.; Macrides, T.A.; Kalafatis, N.; Betts, W.H.; Haynes, D.R.; Broadbent, J. Anti-inflammatory activity of a lipid fraction (lyprinol) from the NZ green-lipped mussel. Inflammopharmacology 1997, 5, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Bao, C.; Cho, S.H.; Lee, H.J. Green lipped mussel oil complex suppresses lipopolysaccharide stimulated inflammation via regulating nuclear factor-κB and mitogen activated protein kinases signaling in RAW264. 7 murine macrophages. Food Sci. Biotechnol. 2017, 26, 815–822. [Google Scholar] [CrossRef]
- Bierer, T.L.; Bui, L.M. Improvement of arthritic signs in dogs fed green-lipped mussel (Perna canaliculus). J. Nutr. 2002, 132, 1634S–1636S. [Google Scholar] [CrossRef]
- Bui, L.M.; Bierer, T.L. Influence of green lipped mussels (Perna canaliculus) in alleviating signs of arthritis in dogs. Vet. Ther. 2003, 4, 397–407. [Google Scholar] [PubMed]
- Lee, C.-H.; Lum, J.H.-K.; Ng, C.K.-C.; McKay, J.; Butt, Y.K.-C.; Wong, M.-S.; Lo, S.C.-L. Pain controlling and cytokine-regulating effects of lyprinol, a lipid extract of Perna canaliculus, in a rat adjuvant-induced arthritis model. Evid.-Based Complement. Altern. Med. 2009, 6, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Fu, Y.; Zheng, J.; Li, D. Anti-inflammatory activity and mechanism of a lipid extract from hard-shelled mussel (Mytilus coruscus) on chronic arthritis in rats. Mar. Drugs 2014, 12, 568–588. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Li, H.; Song, X.; Kuang, X.; Liu, S.; Zhu, S.; Li, D. The preventive effect of mussel oil on gestational diabetes mellitus in pregnant mice fed by a high-fat and high-sucrose diet. Food Funct. 2023, 14, 1198–1208. [Google Scholar] [CrossRef]
- Miller, T.E.; Ormrod, D. The anti-inflammatory activity of Perna canaliculus (NZ green lipped mussel). N. Z. Med. J. 1980, 92, 187–193. [Google Scholar]
- Miller, T.; Dodd, J.; Ormrod, D.; Geddes, R. Anti-inflammatory activity of glycogen extracted from Perna canaliculus (NZ green-lipped mussel). Agents Actions 1993, 38, C139–C142. [Google Scholar] [CrossRef]
- Balkrishna, A.; Das, S.K.; Pokhrel, S.; Joshi, A.; Laxmi; Verma, S.; Sharma, V.K.; Sharma, V.; Sharma, N.; Joshi, C.S. Colchicine: Isolation, LC-MS QTof Screening, and Anticancer Activity Study of Gloriosa superba Seeds. Molecules 2019, 24, 2772. [Google Scholar] [CrossRef] [PubMed]
- Baxter, E.W.; Graham, A.E.; Re, N.A.; Carr, I.M.; Robinson, J.I.; Mackie, S.L.; Morgan, A.W. Standardized protocols for differentiation of THP-1 cells to macrophages with distinct M(IFNγ+LPS), M(IL-4) and M(IL-10) phenotypes. J. Immunol. Methods 2020, 478, 112721. [Google Scholar] [CrossRef]
- Lessa, R.C.; Ebrahimi, B.; Guan, X.; Li, Y.; Lu, J. Exploring the In Vitro Protective Effects of Green-Lipped Mussel (GLM) Oil Extract against Biomarkers of Glucose Metabolism and Inflammation in Chondrocyte Cells. Nutraceuticals 2023, 4, 1–22. [Google Scholar] [CrossRef]
- Arango Duque, G.; Descoteaux, A. Macrophage cytokines: Involvement in immunity and infectious diseases. Front. Immunol. 2014, 5, 491. [Google Scholar] [CrossRef]
- Gomez-Olarte, S.; Bolanos, N.I.; Echeverry, M.; Rodriguez, A.N.; Cuellar, A.; Puerta, C.J.; Marino, A.; Gonzalez, J.M. Intermediate Monocytes and Cytokine Production Associated with Severe Forms of Chagas Disease. Front. Immunol. 2019, 10, 1671. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, L.; Yu, C.; Yang, X.F.; Wang, H. Monocyte and macrophage differentiation: Circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomark. Res. 2014, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Austermann, J.; Roth, J.; Barczyk-Kahlert, K. The Good and the Bad: Monocytes’ and Macrophages’ Diverse Functions in Inflammation. Cells 2022, 11, 1979. [Google Scholar] [CrossRef] [PubMed]
- Dong, C. Cytokine Regulation and Function in T Cells. Annu. Rev. Immunol. 2021, 39, 51–76. [Google Scholar] [CrossRef] [PubMed]
- Gholijani, N.; Gharagozloo, M.; Kalantar, F.; Ramezani, A.; Amirghofran, Z. Modulation of cytokine production and transcription factors activities in human Jurkat T cells by thymol and carvacrol. Adv. Pharm. Bull. 2015, 5 (Suppl. S1), 653. [Google Scholar] [CrossRef] [PubMed]
- Street, N.E.; Mosmann, T.R. Functional diversity of T lymphocytes due to secretion of different cytokine patterns. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 1991, 5, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Risbud, M.V.; Shapiro, I.M. Role of cytokines in intervertebral disc degeneration: Pain and disc content. Nat. Rev. Rheumatol. 2014, 10, 44–56. [Google Scholar] [CrossRef]
- Riddy, D.M.; Goy, E.; Delerive, P.; Summers, R.J.; Sexton, P.M.; Langmead, C.J. Comparative genotypic and phenotypic analysis of human peripheral blood monocytes and surrogate monocyte-like cell lines commonly used in metabolic disease research. PLoS ONE 2018, 13, e0197177. [Google Scholar] [CrossRef]
- de Bardet, J.C.; Cardentey, C.R.; González, B.L.; Patrone, D.; Mulet, I.L.; Siniscalco, D.; Robinson-Agramonte, M.d.l.A. Cell Immortalization: In Vivo Molecular Bases and In Vitro Techniques for Obtention. BioTech 2023, 12, 14. [Google Scholar] [CrossRef]
- Chanput, W.; Mes, J.J.; Wichers, H.J. THP-1 cell line: An in vitro cell model for immune modulation approach. Int. Immunopharmacol. 2014, 23, 37–45. [Google Scholar] [CrossRef]
- Nascimento, C.R.; Fernandes, N.A.R.; Maldonado, L.A.G.; Junior, C.R. Comparison of monocytic cell lines U937 and THP-1 as macrophage models for in vitro studies. Biochem. Biophys. Rep. 2022, 32, 101383. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.-Y.; Rakariyatham, K. Phospholipids-Reference Module in Food Science. In Encyclopedia of Food Chemistry; Fereidoon, S., Melton, L., Varelis, P., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 546–549. [Google Scholar] [CrossRef]
- Ma, Y.; Poole, K.; Goyette, J.; Gaus, K. Introducing Membrane Charge and Membrane Potential to T Cell Signaling. Front. Immunol. 2017, 8, 1513. [Google Scholar] [CrossRef] [PubMed]
- Cauvi, D.M.; Hawisher, D.; Dores-Silva, P.R.; Lizardo, R.E.; De Maio, A. Macrophage reprogramming by negatively charged membrane phospholipids controls infection. FASEB J. 2019, 33, 2995–3009. [Google Scholar] [CrossRef] [PubMed]
- Mauricio, T.; Aveiro, S.; Guedes, S.; Lopes, D.; Melo, T.; Neves, B.M.; Domingues, R.; Domingues, P. Multi-Omic Profiling of Macrophages Treated with Phospholipids Containing Omega-3 and Omega-6 Fatty Acids Reveals Complex Immunomodulatory Adaptations at Protein, Lipid and Metabolic Levels. Int. J. Mol. Sci. 2022, 23, 2139. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Park, K. Omega-3 and omega-6 polyunsaturated fatty acids and metabolic syndrome: A systematic review and meta-analysis. Clin. Nutr. 2020, 39, 765–773. [Google Scholar] [CrossRef]
- Liput, K.P.; Lepczynski, A.; Ogluszka, M.; Nawrocka, A.; Polawska, E.; Grzesiak, A.; Slaska, B.; Pareek, C.S.; Czarnik, U.; Pierzchala, M. Effects of Dietary n-3 and n-6 Polyunsaturated Fatty Acids in Inflammation and Cancerogenesis. Int. J. Mol. Sci. 2021, 22, 6965. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; O’Keefe, J. The Importance of Maintaining a Low Omega-6 Omega-3 Ratio for Reducing the Risk of Inflammatory Cytokine Storms. Mo. Med. 2020, 117, 539–542. [Google Scholar]
- Semenoglou, I.; Eliasson, L.; Uddstål, R.; Tsironi, T.; Taoukis, P.; Xanthakis, E. Supercritical CO2 extraction of oil from Arctic charr side streams from filleting processing. Innov. Food Sci. Emerg. Technol. 2021, 71, 102712. [Google Scholar] [CrossRef]
- Verlengia, R.; Gorjao, R.; Kanunfre, C.C.; Bordin, S.; Martins De Lima, T.; Martins, E.F.; Curi, R. Comparative effects of eicosapentaenoic acid and docosahexaenoic acid on proliferation, cytokine production, and pleiotropic gene expression in Jurkat cells. J. Nutr. Biochem. 2004, 15, 657–665. [Google Scholar] [CrossRef]
- Hidalgo, M.A.; Carretta, M.D.; Burgos, R.A. Long Chain Fatty Acids as Modulators of Immune Cells Function: Contribution of FFA1 and FFA4 Receptors. Front. Physiol. 2021, 12, 668330. [Google Scholar] [CrossRef]
- Ander, B.P.; Dupasquier, C.M.; Prociuk, M.A.; Pierce, G.N. Polyunsaturated fatty acids and their effects on cardiovascular disease. Exp. Clin. Cardiol. 2003, 8, 164. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).