Sedentary Behavior, Physical Inactivity, and the Prevalence of Hypertension, Diabetes, and Obesity During COVID-19 in Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Type of Study and Context
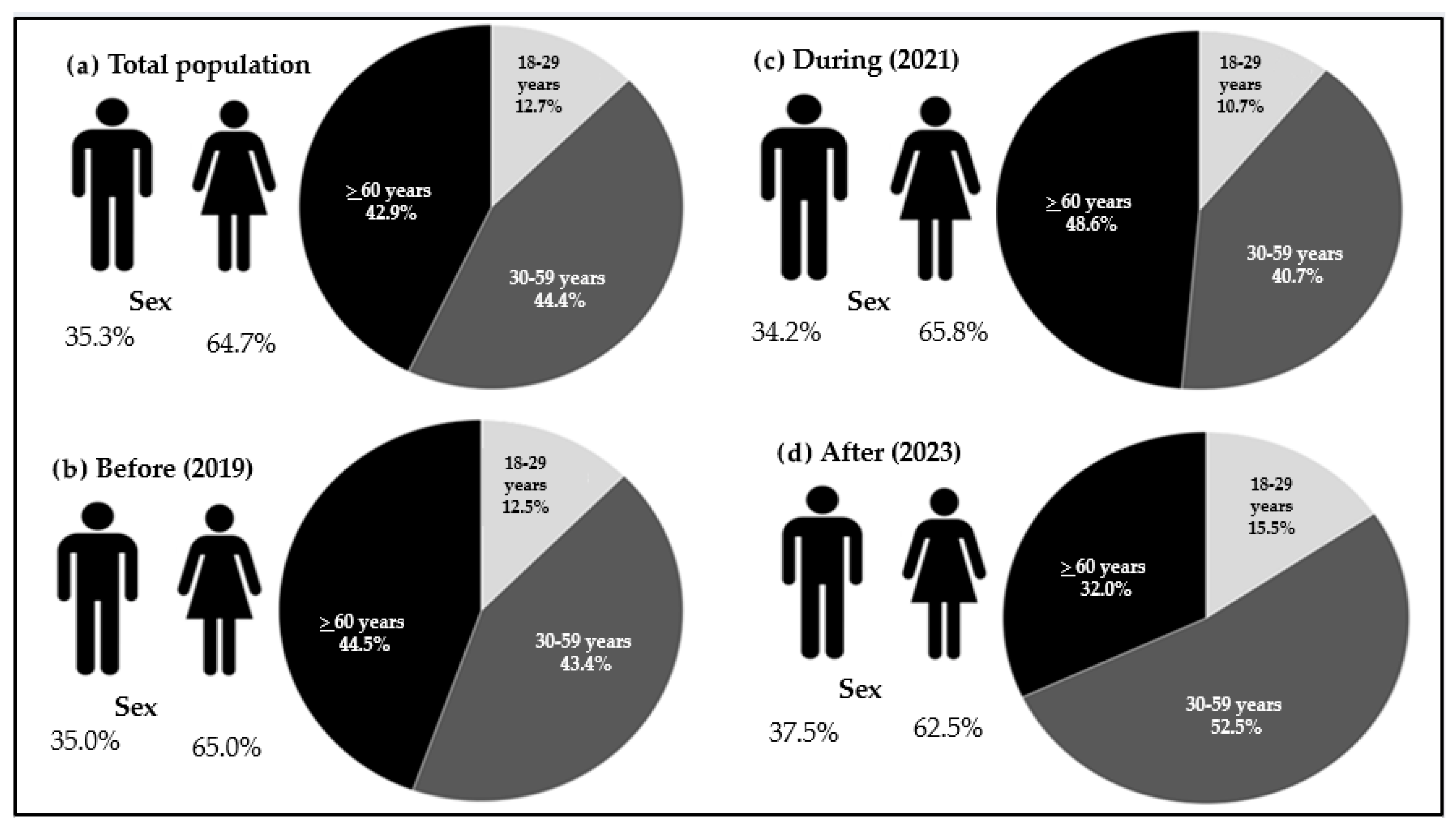
2.2. Study Population and Sampling
2.3. Data Collection and Organization
2.4. Self-Reported Arterial Hypertension
2.5. Self-Reported Diabetes Mellitus
2.6. Obesity
2.7. Insufficient Physical Activity Variables
2.8. Statistical Analysis
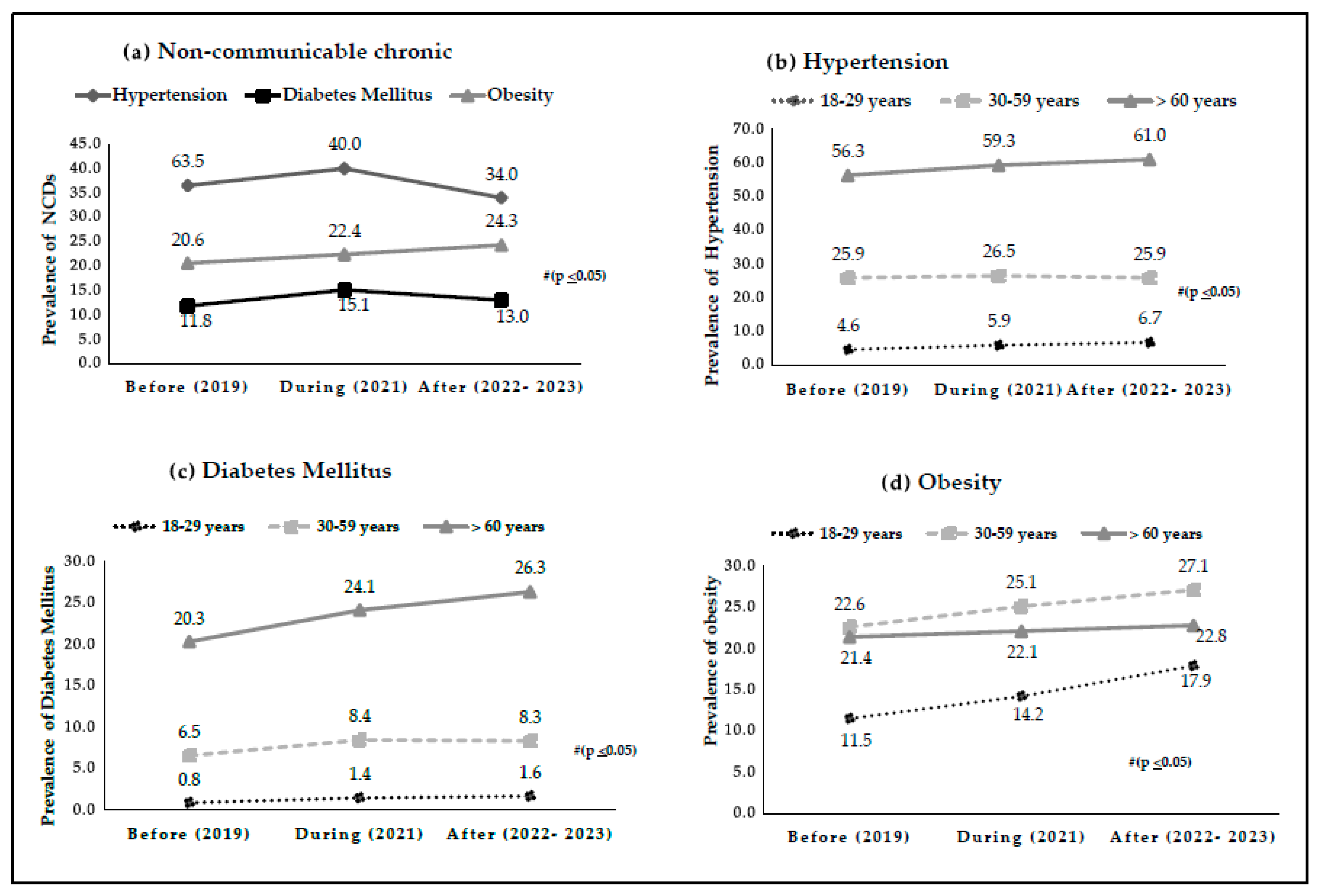
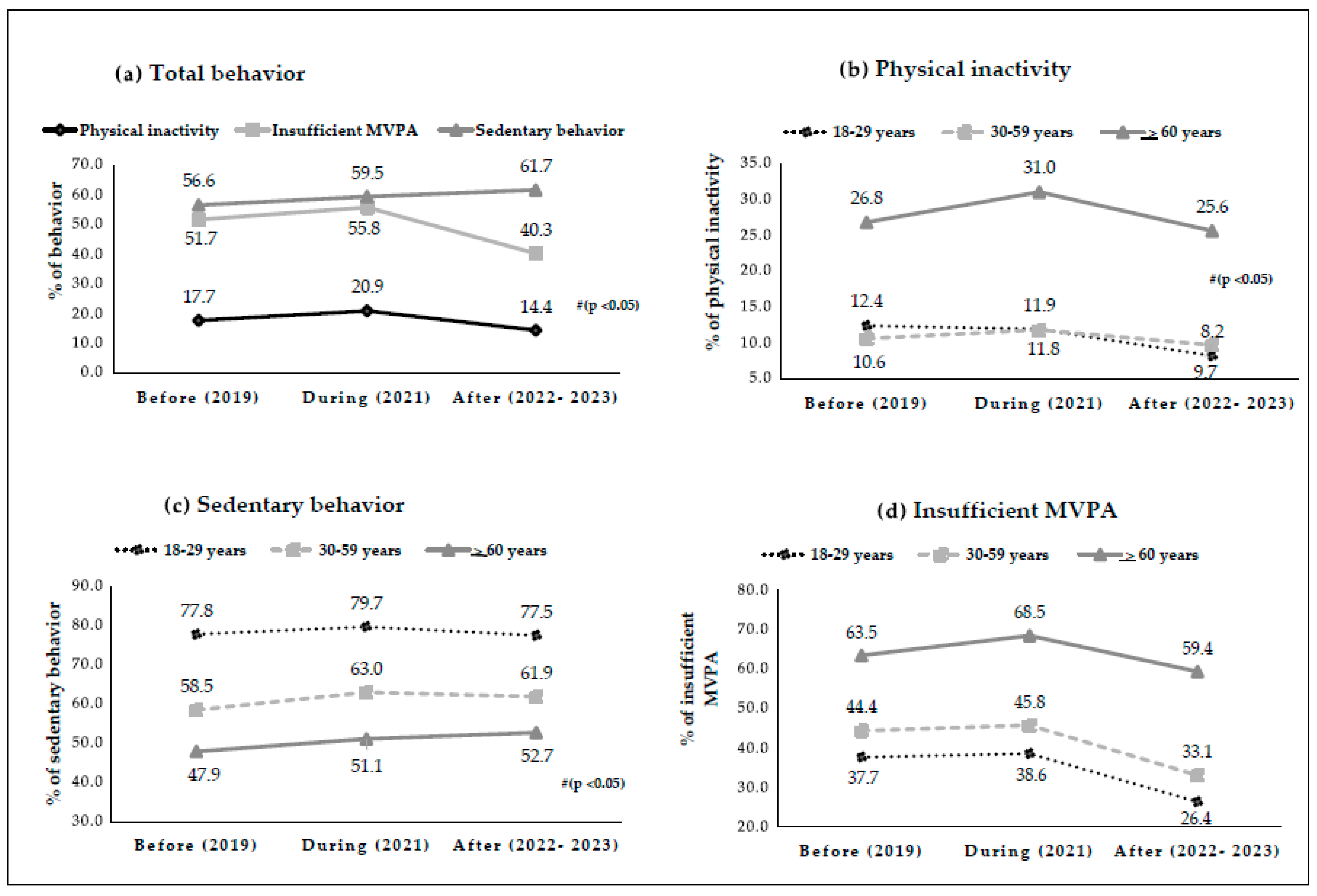
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NCDs | NCDs Communicable Diseases |
| IMDIS | Implementation of Social Isolation and Distancing Measures |
| PI | Physical Inactivity |
| MVPA | Moderate to Vigorous Physical Activity |
| SB | Sedentary Behavior |
| AH | Arterial Hypertension |
| DM | Diabetes Mellitus |
| OB | Obesity |
| AP | Physical Activity |
| VIGITEL | System for Risk and Protective Factors for Chronic Diseases by Telephone Survey |
| ANATEL | National Telecommunications Agency |
| OR | Odds Ratio |
| 95%CI | 95% confidence interval |
References
- Gomide, E.B.G.; Abdalla, P.P.; Pisa, M.F.; Schneider, G.; Vieira, L.G.; Mazzonetto, L.F.; Oliveira, A.S.; Sebastiao, E.; Santos, A.P. The role of physical activity in the clinical outcomes of people diagnosed with COVID-19: A systematic review. JSAMS Plus 2022, 1, 100007. [Google Scholar] [CrossRef] [PubMed]
- Rosa, R.J.; Ferezin, L.P.; de Campos, M.C.T.; Moura, H.S.D.; Berra, T.Z.; Ribeiro, N.M.; Arcêncio, R.A. Perception of risk for developing severe illness or complications from COVID-19 in Brazil: Focus on factors linked to socially vulnerable populations, 2020–2023. Int. J. Environ. Res. Public Health 2025, 22, 251. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. About the WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/about (accessed on 12 January 2024).
- Ministério da Saúde. Painel de Casos de Doença Pelo Coronavírus 2019 (COVID-19) no Brasil Pelo Ministério da Saúde. Versão v2.0. Available online: https://covid.saude.gov.br/ (accessed on 12 January 2024).
- Faria, T.M.T.R.; Silva, A.G.D.; Claro, R.M.; Malta, D.C. Tendências temporais e mudanças pós-pandemia de COVID-19 na prevalência de atividade física e comportamento sedentário em adultos brasileiros entre 2006 e 2021. Rev. Bras. Epidemiol. 2023, 26, e230011. [Google Scholar] [CrossRef] [PubMed]
- Dantas, R.C.C.; de Campos, P.A.; Rossi, I.; Ribas, R.M. Implications of social distancing in Brazil in the COVID-19 pandemic. Infect. Control Hosp. Epidemiol. 2022, 43, 953–954. [Google Scholar] [CrossRef]
- Cortinez-O’Ryan, A.; Moran, M.R.; Rios, A.P.; Anza-Ramirez, C.; Slovic, A.D. Could severe mobility and park use restrictions during the COVID-19 pandemic aggravate health inequalities? Insights and challenges from Latin America. Cad. Saúde Pública 2020, 36, e00185820. [Google Scholar] [CrossRef]
- Caputo, E.L.; Feter, N.; Doring, I.R.; Leite, J.S.; Cassuriaga, J.; Rombaldi, A.J.; Reichert, F.F. How has COVID-19 social distancing impacted physical activity patterns? Data from the PAMPA cohort, Brazil. J. Exerc. Sci. Fit. 2021, 19, 252–258. [Google Scholar] [CrossRef]
- Gonçalves, L.; Lima, T.R.D.; Quadros, T.M.B.D.; Rech, C.R.; Silva, D.A.S. Counseling on physical activity before and during the COVID-19 pandemic among users of the Brazilian community health promotion program. Ciência Saúde Coletiva 2025, 30, e04072023. [Google Scholar] [CrossRef]
- Silva, D.R.P.D.; Werneck, A.O.; Malta, D.C.; Souza Júnior, P.R.B.D.; Azevedo, L.O.; Barros, M.B.D.A.; Szwarcwald, C.L. Mudanças na prevalência de inatividade física e comportamento sedentário durante a pandemia da COVID-19: Um inquérito com 39.693 adultos brasileiros. Cad. Saúde Pública 2021, 37, e00221920. [Google Scholar] [CrossRef]
- Togni, G.; Puccinelli, P.J.; Costa, T.; Seffrin, A.; de Lira, C.A.B.; Vancini, R.L.; Andrade, M.S. Factors associated with reduction in physical activity during the COVID-19 pandemic in São Paulo, Brazil: An internet-based survey conducted in June 2020. Int. J. Environ. Res. Public Health 2021, 18, 11397. [Google Scholar] [CrossRef]
- Malta, D.C.; Gomes, C.S.; Prates, E.J.S.; Bernal, R.T.I. Changes in chronic diseases and risk and protective factors before and after the third wave of COVID-19 in Brazil. Ciênc. Saúde Colet. 2023, 28, 3659–3671. [Google Scholar] [CrossRef]
- Pereira, Z.S.; da Silva, A.S.; Melo, J.C.D.N.; Dos Santos, J.C.; Sewo Sampaio, P.Y.; Silva, R.J.D.S.; de Oliveira Araújo, R.H.; Sampaio, R.A.C. Differential Factors Are Associated with Physical Activity in Older Adults in Brazil with and without Non-Communicable Chronic Diseases: A Cross-Sectional Analysis of the 2019 National Health Survey. Int. J. Environ. Res. Public Health 2023, 20, 6329. [Google Scholar] [CrossRef]
- Ferreira, A.P.D.S.; Szwarcwald, C.L.; Damacena, G.N.; Souza Júnior, P.R.B.D. Increasing trends in obesity prevalence from 2013 to 2019 and associated factors in Brazil. Rev. Bras. Epidemiol. 2021, 24, e210009. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1· 9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Friedenreich, C.; Shiroma, E.J.; Lee, I.M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br. J. Sports Med. 2022, 56, 101–106. [Google Scholar] [CrossRef]
- Sapkota, B.P.; Baral, K.P.; Rehfuess, E.A.; Parhofer, K.G.; Berger, U. Effects of age on non-communicable disease risk factors among Nepalese adults. PLoS ONE 2023, 18, e0281028. [Google Scholar] [CrossRef] [PubMed]
- Wunsch, K.; Kienberger, K.; Niessner, C. Changes in physical activity patterns due to the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 2250. [Google Scholar] [CrossRef]
- Park, S.; Kim, H.J.; Kim, S.; Rhee, S.Y.; Woo, H.G.; Lim, H.; Cho, W.; Yon, D.K. National trends in physical activity among adults in South Korea before and during the COVID-19 Pandemic, 2009–2021. JAMA Netw. Open 2023, 6, e2316930. [Google Scholar] [CrossRef]
- Miranda, C.; Sousa, T.M.; Caldeira, T.C.M.; Claro, R.M. Health risk factors among adult individuals with and without diabetes in Brazil: Vigitel (2020–2023). Public Health 2024, 234, 120–125. [Google Scholar] [CrossRef]
- VIGITEL. Vigitel Brasil 2019: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico; Ministério da Saúde: Brasília, Brazil, 2019.
- VIGITEL. Vigitel Brasil 2021: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico; Ministério da Saúde: Brasília, Brazil, 2021.
- VIGITEL. Vigitel Brasil 2023: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico; Ministério da Saúde: Brasília, Brazil, 2023.
- Graham, K. Compensating for Missing Survey Data; Institute for Social Research, The University of Michigan: Ann Arbor, MI, USA, 1983. [Google Scholar]
- World Health Organization Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 1998.
- Wellman, N.S. The nutrition screening initiative. Nutr. Rev. 1994, 52, S44. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Willumsen, J.F. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Trimarco, V.; Izzo, R.; Pacella, D.; Trama, U.; Manzi, M.V.; Lombardi, A.; Piccinocchi, R.; Gallo, P.; Esposito, G.; Piccinocchi, G.; et al. Incidence of new-onset hypertension before, during, and after the COVID-19 pandemic: A 7-year longitudinal cohort study in a large population. BMC Med. 2024, 22, 127. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.; Pan, Y.; Chapman, M.; Spaulding, A.; Stallings-Smith, S. Changes in obesity prevalence among US adults after the COVID-19 pandemic by state and territorial stay-at-home order level and sociodemographic characteristics. Am. J. Health Promot. 2024, 38, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, M.; Woo, S.; Park, J.; Kim, H.J.; Kwon, R.; Koyanagi, A.; Smith, L.; Kim, M.S.; Sánchez, G.F.L.; et al. National and Regional Trends in the Prevalence of Hypertension in South Korea Amid the Pandemic, 2009–2022: Nationwide Study of Over 3 Million Individuals. JMIR Public Health Surveill. 2024, 10, e51891. [Google Scholar] [CrossRef]
- Karagiannidis, A.G.; Theodorakopoulou, M.P.; Ferro, C.J.; Ortiz, A.; Soler, M.J.; Halimi, J.-M.; Januszewicz, A.; Persu, A.; Kreutz, R.; Sarafidis, P. Impact of public restrictive measures on hypertension during the COVID-19 pandemic: Existing evidence and long-term implications. Clin. Kidney J. 2023, 16, 619–634. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.M.; Yadav, U.N.; Khanam, F.; Huda, N.; Lim, D.; Chowdhury, A.A.; Sarma, H. Changes in Prevalence and Determinants of Self-Reported Hypertension among Bangladeshi Older Adults during the COVID-19. Pandemic 2022, 19, 13475. [Google Scholar] [CrossRef]
- Quesada-Caballero, M.; Carmona-Garcia, A.; Chami-Pena, S.; Caballero-Mateos, A.M.; Fernandez-Martin, O.; Cañadas-De la Fuente, G.A.; Romero-Bejar, J.L. Telemedicine in elderly hypertensive and patients with chronic diseases during the COVID-19 pandemic: A systematic review and meta-analysis. J. Clin. Med. 2023, 12, 6160. [Google Scholar] [CrossRef]
- Civitelli, G.; Tarsitani, G.; Rinaldi, A.; Marceca, M. Long-term impact of Global Health educational experiences in Rome: An attempt of measurement. Arch. Public Health 2020, 78, 78–90. [Google Scholar] [CrossRef]
- Nshimirimana, D.A.; Kokonya, D.; Gitaka, J.; Wesonga, B.; Mativo, J.N.; Rukanikigitero, J.M.V. Impact of COVID-19 on health-related quality of life in the general population: A systematic review and meta-analysis. PLoS Glob. Public Health 2023, 3, e0002137. [Google Scholar] [CrossRef]
- Jenssen, B.P.; Kelly, M.K.; Powell, M.; Bouchelle, Z.; Mayne, S.L.; Fiks, A.G. COVID-19 and changes in child obesity. Pediatrics 2021, 147, e2021050123. [Google Scholar] [CrossRef]
- Balci, B.; Aktar, B.; Buran, S.; Tas, M.; Colakoglu, B.D. Impact of the COVID-19 pandemic on physical activity, anxiety, and depression in patients with Parkinson’s disease. Int. J. Rehabil. Res. 2021, 44, 173–176. [Google Scholar] [CrossRef]
- Sarda, B.; Delamaire, C.; Serry, A.J.; Ducrot, P. Changes in home cooking and culinary practices among the French population during the COVID-19 lockdown. Appetite 2022, 168, 105743. [Google Scholar] [CrossRef]
- Ghram, A.; Briki, W.; Mansoor, H.; Al-Mohannadi, A.S.; Lavie, C.J.; Chamari, K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad. Med. 2021, 133, 469–480. [Google Scholar] [CrossRef]
- Alharthi, S.K.; Alyusuf, E.Y.; Alguwaihes, A.M.; Alfadda, A.; Al-Sofiani, M.E. The impact of a prolonged lockdown and use of telemedicine on glycemic control in people with type 1 diabetes during the COVID-19 outbreak in Saudi Arabia. Diabetes Res. Clin. Pract. 2021, 173, 108682. [Google Scholar] [CrossRef]
- Vallée, A. The impact of the COVID-19 pandemic on the socioeconomic gradient of hypertension. J. Public Health Policy 2024, 45, 413–430. [Google Scholar] [CrossRef]
- Ayele, T.A.; Alamneh, T.S.; Shibru, H.; Sisay, M.M.; Yilma, T.M.; Melak, M.F.; Shitu, K. Effect of COVID-19 pandemic on missed medical appointment among adults with chronic disease conditions in Northwest Ethiopia. PLoS ONE 2022, 17, e0274190. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, K.; Suzuki, K.; Sakamoto, Y.; Sasaki, K. Physical activity and sedentary behavior among children and adolescents living in an area affected by the 2011 Great East Japan earthquake and tsunami for 3 years. Prev. Med. Rep. 2015, 2, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Eberle, C.; Stichling, S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: A systematic review. Diabetol. Metab. Syndr. 2021, 13, 95. [Google Scholar] [CrossRef] [PubMed]
- Baumhardt, M.; Dreyhaupt, J.; Winsauer, C.; Stuhler, L.; Thiessen, K.; Stephan, T.; Rattka, M. The effect of the lockdown on patients with myocardial infarction during the COVID-19 pandemic: A systematic review and meta-analysis. Dtsch. Arztebl. Int. 2021, 118, 447. [Google Scholar]
- Oduro, J.K.; Okyere, J.; Nyador, J.K.M.T. Risky health behaviours and chronic conditions among aged persons: Analysis of SAGE selected countries. BMC Geriatr. 2023, 23, 145. [Google Scholar] [CrossRef]
- Melo, S.P.D.S.D.C.; Cesse, E.Á.P.; Lira, P.I.C.; Rissin, A.; Cruz, R.D.S.B.L.C.; Batista Filho, M. Doenças crônicas não transmissíveis e fatores associados em adultos numa área urbana de pobreza do nordeste brasileiro. Ciênc. Saúde Colet. 2019, 24, 3159–3168. [Google Scholar] [CrossRef]
- Griep, R.H.; Nobre, A.A.; Alves, M.G.D.M.; da Fonseca, M.D.J.M.; Cardoso, L.D.O.; Giatti, L.; Chor, D. Job strain and unhealthy lifestyle: Results from the baseline cohort study, Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). BMC Public Health 2015, 15, 309. [Google Scholar] [CrossRef]
- Song, J.J.; Ma, Z.; Wang, J.; Chen, L.X.; Zhong, J.C. Gender differences in hypertension. J. Cardiovasc. Transl. Res. 2020, 13, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Reckelhoff, J.F. Mechanisms of sex and gender differences in hypertension. J. Hum. Hypertens. 2023, 37, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Gomes, G.A.D.O.; Papini, C.B.; Nakamura, P.M.; Teixeira, I.P.; Kokubun, E. Barreiras para prática de atividade física entre mulheres atendidas na Atenção Básica de Saúde. Rev. Bras. Ciênc. Esporte 2019, 41, 263–270. [Google Scholar] [CrossRef]
- Pereira, A.; Silva, M.; Freitas, V. Barreiras para a prática de exercício físico em adultos. Psych. Tech. Health J. 2020, 3, 39–54. [Google Scholar] [CrossRef]
- Blond, K.; Brinkløv, C.F.; Ried-Larsen, M.; Crippa, A.; Grøntved, A. Association of high amounts of physical activity with mortality risk: A systematic review and meta-analysis. Br. J. Sports Med. 2020, 54, 1195–1201. [Google Scholar] [CrossRef]
- Biddle, S.J.; Bengoechea García, E.; Pedisic, Z.; Bennie, J.; Vergeer, I.; Wiesner, G. Screen time, other sedentary behaviours, and obesity risk in adults: A review of reviews. Curr. Obes. Rep. 2017, 6, 134–147. [Google Scholar] [CrossRef]
- Curran, F.; Davis, M.E.; Murphy, K.; Tersigni, N.; King, A.; Ngo, N.; O’Donoghue, G. Correlates of physical activity and sedentary behavior in adults living with overweight and obesity: A systematic review. Obes. Rev. 2023, 24, e13615. [Google Scholar] [CrossRef]
- Melo, C.M.D.; Tirapegui, J.; Ribeiro, S.M.L. Gasto energético corporal: Conceitos, formas de avaliação e sua relação com a obesidade. Arq. Bras. Endocrinol. Metab. 2008, 52, 452–464. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Correia, R.R.; Veras, A.S.C.; Tebar, W.R.; Rufino, J.C.; Batista, V.R.G.; Teixeira, G.R. Strength training for arterial hypertension treatment: A systematic review and meta-analysis of randomized clinical trials. Sci. Rep. 2023, 13, 201. [Google Scholar] [CrossRef]
- Nadal, I.P.; Angkurawaranon, C.; Singh, A.; Choksomngam, Y.; Sadana, V.; Kock, L.; Kinra, S. Effectiveness of behaviour change techniques in lifestyle interventions for non-communicable diseases: An umbrella review. BMC Public Health 2024, 24, 3082. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.; Durstine, J.L. Physical activity, exercise, and chronic diseases: A brief review. Sports Med. Health Sci. 2019, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Xingyu, Z. Optimizing chronic disease management: The comprehensive role and impact of exercise interventions in public health. Int. J. Educ. Humanit. 2024, 4, 328–337. [Google Scholar] [CrossRef]
- Bjarnason-Wehrens, B.; Schwaab, B. Physical activity in youth is determinant of cardiovascular health in adulthood. Eur. J. Prev. Cardiol. 2024, 31, 458–460. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; He, J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Chenarides, L.; Grebitus, C.; Lusk, J.L.; Printezis, I. Food consumption behavior during the COVID-19 pandemic. Agribusiness 2021, 37, 44–81. [Google Scholar] [CrossRef]
- Moreira, A.D.; Gomes, C.S.; Machado, Í.E.; Malta, D.C.; Felisbino-Mendes, M.S. Cardiovascular health and validation of the self-reported score in Brazil: Analysis of the National Health Survey. Ciênc. Saúde Colet. 2020, 25, 4259–4268. [Google Scholar] [CrossRef]
- Carvalho, A.M.D.; Piovezan, L.G.; Selem, S.S.; de Castro, A.; Fisberg, R.M.; Marchioni, D.M.L. Validação e calibração de medidas de peso e altura autorreferidas por indivíduos da cidade de São Paulo. Rev. Bras. Epidemiol. 2014, 17, 735–746. [Google Scholar] [CrossRef]
| Arterial Hypertension | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Before (2019) | During (2022) | After (2022–2023) | |||||||
| OR | IC95% | p-Value | OR | IC95% | p-Value | OR | IC95% | p-Value | ||
| Age Group | ||||||||||
| 18–29 years | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| 30–59 years | 7.05 | 6.25–7.94 | <0.001 | 5.52 | 4.70–6.48 | <0.001 | 4.74 | 4.11–5.46 | <0.001 | |
| ≥60 years | 9.02 | 8.65–9.64 | <0.001 | 8.59 | 7.86–9.39 | <0.001 | 8.80 | 8.06–9.61 | <0.001 | |
| Sex | ||||||||||
| Male | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Female | 1.14 | 1.10–1.19 | <0.001 | 1.10 | 1.03–1.16 | 0.002 | 1.12 | 1.06–1.21 | <0.001 | |
| Insufficient MVPA | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.29 | 1.23–1.34 | <0.001 | 1.35 | 1.27–1.44 | <0.001 | 1.33 | 1.23–1.43 | <0.001 | |
| Physical Inactivity | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.24 | 1.17–1.31 | <0.001 | 1.17 | 1.08–1.25 | <0.001 | 1.15 | 1.04–1.02 | 0.005 | |
| Sedentary Behavior | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 0.97 | 0.93–1.00 | 0.081 | 0.94 | 0.89–0.99 | 0.028 | 0.97 | 0.91–1.04 | 0.379 | |
| Diabetes Mellitus | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Before (2019) | During (2022) | After (2022–2023) | |||||||
| OR | IC95% | p-Value | OR | IC95% | p-Value | OR | IC95% | p-Value | ||
| Age Group | ||||||||||
| 18–29 years | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| 30–59 years | 8.34 | 6.35–10.96 | <0.001 | 6.25 | 4.56–8.58 | <0.001 | 5.37 | 4.07–7.08 | <0.001 | |
| ≥60 years | 9.54 | 8.28–10.99 | <0.001 | 7.75 | 6.58–9.14 | <0.001 | 7.93 | 6.81–9.22 | <0.001 | |
| Sex | ||||||||||
| Male | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Female | 0.92 | 0.86–0.97 | 0.003 | 1.01 | 0.93–1.09 | 0.815 | 1.12 | 1.02–1.22 | 0.013 | |
| Insufficient MVPA | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.27 | 1.19–1.36 | <0.001 | 1.25 | 1.15–1.36 | <0.001 | 1.38 | 1.25–1.52 | <0.001 | |
| Physical Inactivity | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.43 | 1.33–1.53 | 0.005 | 1.35 | 1.23–1.47 | <0.001 | 1.29 | 1.15–1.45 | <0.001 | |
| Sedentary Behavior | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 0.97 | 0.91–1.02 | 0.205 | 0.97 | 0.90–1.04 | 0.374 | 0.93 | 0.86–1.02 | 0.110 | |
| Obesity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Before (2019) | During (2022) | After (2022–2023) | |||||||
| OR | IC95% | p-Value | OR | IC95% | p-Value | OR | IC95% | p-Value | ||
| Age Group | ||||||||||
| 18–29 years | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| 30–59 years | 2.29 | 2.10–2.48 | <0.001 | 2.02 | 1.81–2.27 | <0.001 | 1.71 | 1.55–1.89 | <0.001 | |
| ≥60 years | 1.32 | 1.25–1.39 | <0.001 | 1.10 | 1.02–1.18 | 0.011 | 0.95 | 0.88–1.03 | 0.203 | |
| Sex | ||||||||||
| Male | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Female | 0.96 | 0.92–1.01 | 0.114 | 1.05 | 0.99–1.12 | 0.101 | 1.02 | 0.96–1.09 | 0.442 | |
| Insufficient MVPA | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.28 | 1.21–1.34 | <0.001 | 1.32 | 1.23–1.41 | <0.001 | 1.28 | 1.19–1.39 | <0.001 | |
| Physical Inactivity | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.25 | 1.18–1.33 | <0.001 | 1.21 | 1.11–1.30 | <0.001 | 1.22 | 1.11–1.35 | <0.001 | |
| Sedentary Behavior | ||||||||||
| No | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||||||
| Yes | 1.14 | 1.09–119 | <0.001 | 1.14 | 1.07–1.21 | <0.001 | 1.17 | 1.10–1.25 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anjos, J.R.C.d.; Correia, I.M.; de Moraes, C.A.L.C.; Cordeiro, J.F.C.; Trapé, A.A.; Mota, J.; Machado, D.R.L.; Santos, A.P.d. Sedentary Behavior, Physical Inactivity, and the Prevalence of Hypertension, Diabetes, and Obesity During COVID-19 in Brazil. Int. J. Environ. Res. Public Health 2025, 22, 1367. https://doi.org/10.3390/ijerph22091367
Anjos JRCd, Correia IM, de Moraes CALC, Cordeiro JFC, Trapé AA, Mota J, Machado DRL, Santos APd. Sedentary Behavior, Physical Inactivity, and the Prevalence of Hypertension, Diabetes, and Obesity During COVID-19 in Brazil. International Journal of Environmental Research and Public Health. 2025; 22(9):1367. https://doi.org/10.3390/ijerph22091367
Chicago/Turabian StyleAnjos, Jeferson Roberto Collevatti dos, Igor Massari Correia, Chimenny Auluã Lascas Cardoso de Moraes, Jéssica Fernanda Corrêa Cordeiro, Atila Alexandre Trapé, Jorge Mota, Dalmo Roberto Lopes Machado, and André Pereira dos Santos. 2025. "Sedentary Behavior, Physical Inactivity, and the Prevalence of Hypertension, Diabetes, and Obesity During COVID-19 in Brazil" International Journal of Environmental Research and Public Health 22, no. 9: 1367. https://doi.org/10.3390/ijerph22091367
APA StyleAnjos, J. R. C. d., Correia, I. M., de Moraes, C. A. L. C., Cordeiro, J. F. C., Trapé, A. A., Mota, J., Machado, D. R. L., & Santos, A. P. d. (2025). Sedentary Behavior, Physical Inactivity, and the Prevalence of Hypertension, Diabetes, and Obesity During COVID-19 in Brazil. International Journal of Environmental Research and Public Health, 22(9), 1367. https://doi.org/10.3390/ijerph22091367







