Heat Stress and Determinants of Kidney Health Among Agricultural Workers in the United States: An Integrative Review
Abstract
1. Introduction
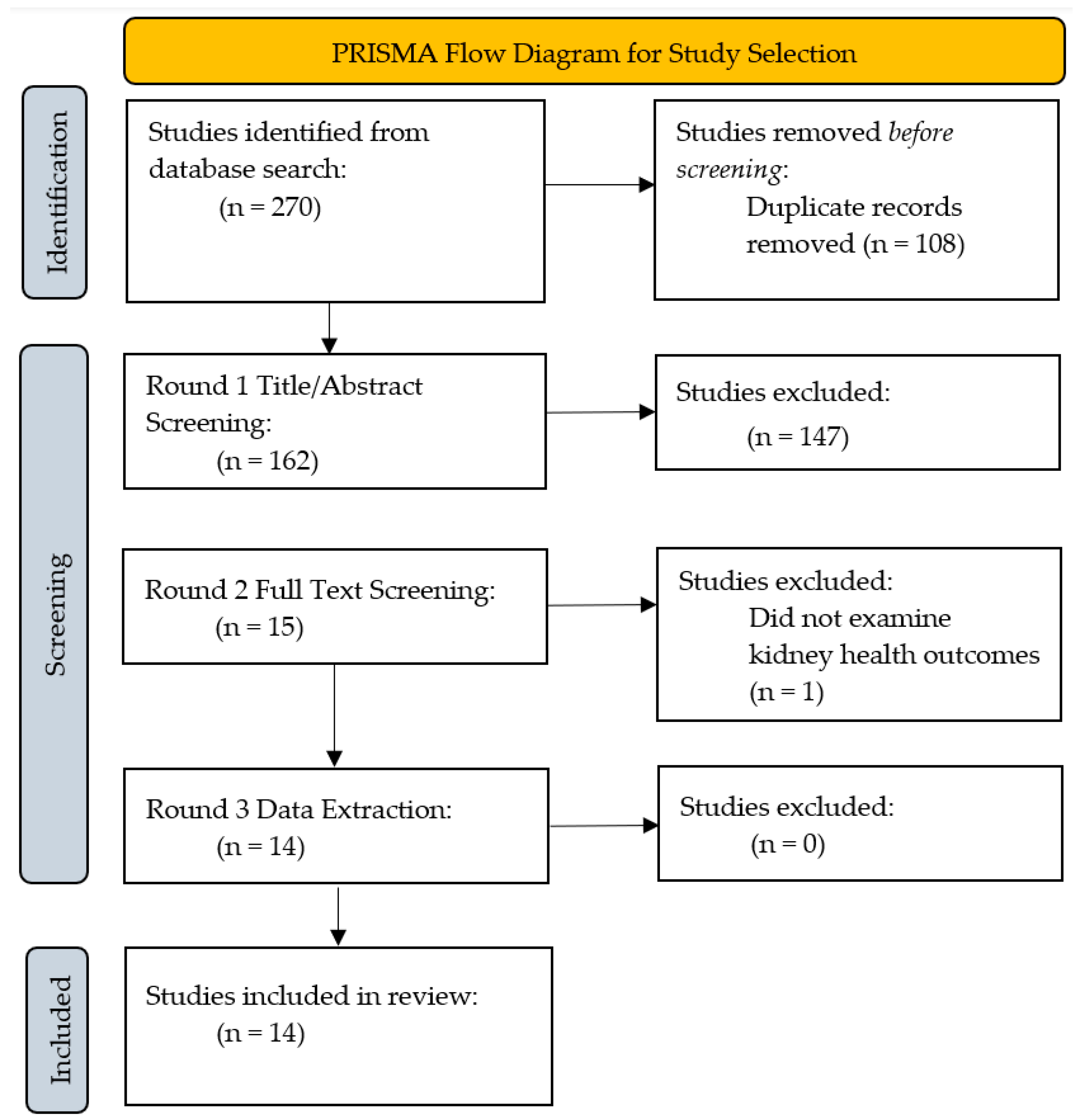
2. Materials and Methods
2.1. Problem Identification
2.2. Literature Search
2.3. Data Evaluation
2.4. Data Analysis
3. Results
3.1. Characteristics of Studies
| Author (Year) | Purpose | Design | State | Sample | Biomarkers of AKI/Dehydration | Key Findings |
|---|---|---|---|---|---|---|
| Moyce, et al. (2020) [28] | To test the associations between workload and heat with acute kidney dysfunction. | Cross-sectional measuring pre- and post-shift | California | 471 agricultural workers | Pre- and post-shift serum creatinine |
|
| Moyce, et al. (2017) [29] | To investigate the associations between heat strain, volume depletion, and kidney function | Cross-sectional measuring pre- and post-shift | California | 283 agricultural workers | Pre- and post-shift serum creatinine |
|
| Albu, et al. (2024) [30] | To evaluate the rate of retention and identify predictors associated with retention in a longitudinal study of agricultural workers | Longitudinal | Florida | 119 agricultural workers | Pre- and post-shift serum creatinine; estimated glomerular filtration rate (eGFR) |
|
| Mix, et al. (2018) [31] | To examine hydration status and kidney function in Florida agricultural workers | Longitudinal | Florida | 192 agricultural workers | Pre- and post-shift serum creatinine, eGFR, and urine specific gravity |
|
| Houser, et al. (2021) [32] | To evaluate dehydration and markers of inflammation, muscle damage, and renal function in agricultural workers | Cross-sectional measuring pre- and post-shift | Florida | 32 agricultural workers who self-identified as Hispanic | Pre- and post-shift serum creatinine; baseline urine specific gravity |
|
| Chicas, et al. (2024) [33] | To investigate the associations between renal function and AKI over time in U.S. agricultural workers | Longitudinal | Florida | 115 agricultural workers | Pre- and post-shift serum creatinine, eGFR, and urine specific gravity |
|
| Abasilim, et al. (2024) [34] | To investigate hydration status during typical workdays and identify risk factors associated with increased dehydration in migrant farmworkers in Florida | Longitudinal | Florida | 111 agricultural workers | Pre-, mid-, and post-shift urine specific gravity |
|
| Moyce, et al. (2020) [35] | To assess hydration choices during work shifts and investigate associations between rehydration with sugary beverages and AKI | Cross-sectional measuring pre- and post-shift | California | 445 agricultural workers | Pre- and post-shift serum creatinine |
|
| Chicas, et al. (2021) [36] | To examine the effectiveness of cooling devices at preventing agricultural workers from exceeding a core body temperature threshold of 38 °C and attenuating HRI symptoms | Cross-sectional measuring pre- and post-shift | Florida | 84 agricultural workers | No biomarkers |
|
| Moyce, et al. (2016) [37] | To investigate the cumulative incidence of AKI over one shift among California agricultural workers | Cross-sectional measuring pre- and post-shift | California | 295 agricultural workers | Pre- and post-shift serum creatinine |
|
| Chicas, et al. (2021) [38] | To explore agricultural workers’ perceptions and experiences with the cooling devices from the pilot study | Cross-sectional post-shift | Florida | 61 agricultural workers | No biomarkers |
|
| Flocks, et al. (2018) [39] | To present a case of renal failure in a farmworker and illustrate how academic-community collaborations can be clinically beneficial | Case study | Florida | 1 agricultural worker | Baseline creatinine |
|
| Chicas, et al. (2023) [40] | To examine the impact of heat exposure on renal biomarkers and the metabolome among agricultural workers and non-agricultural workers | Cross-sectional measuring pre- and post-shift | Florida | 63 agricultural workers and 27 non-agricultural workers | Pre- and post-shift serum creatinine, eGFR, and urine specific gravity |
|
| Chicas, et al. (2022) [41] | To evaluate the impact of hydration interventions on post-workday hydration status and AKI incidence | Cross-sectional measuring pre- and post-shift | Florida | 30 agricultural workers | Pre- and post-shift serum creatinine, eGFR, and urine specific gravity |
|
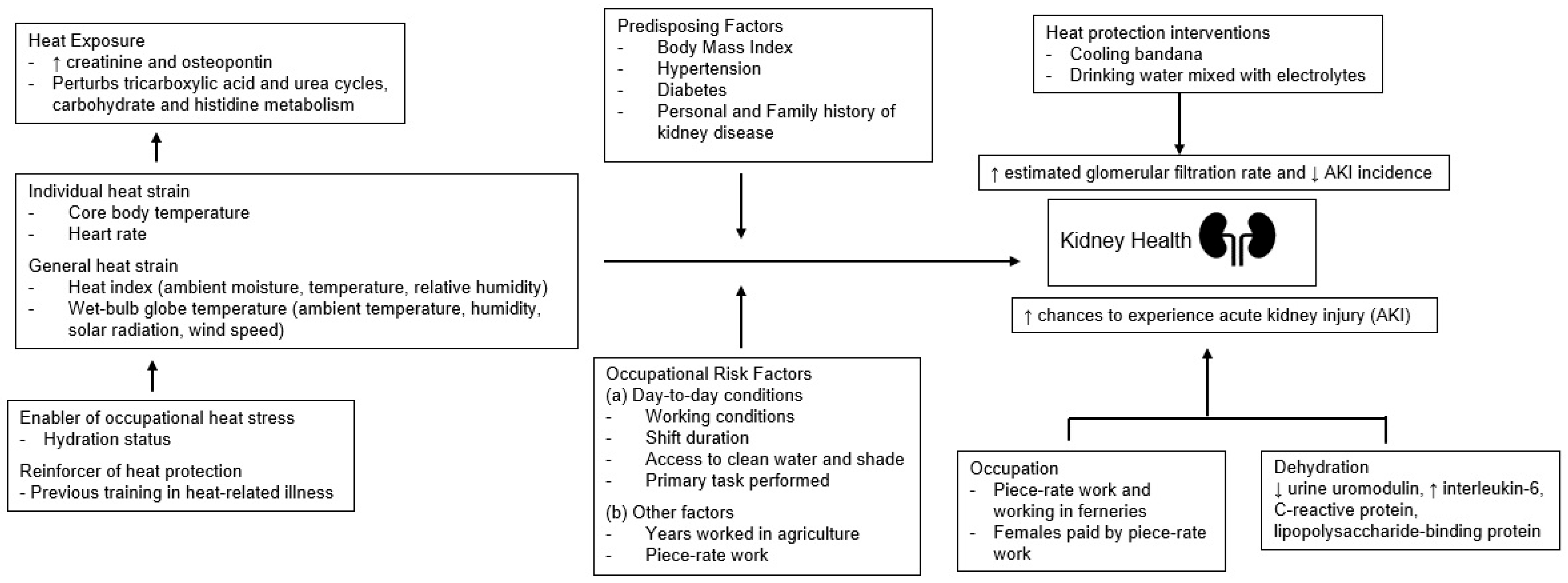
3.2. Heat as a Climate Stressor
3.3. Health Status and Dehydration as Risk Factors
3.4. Occupational Risk Factors
3.5. Social Factors
3.6. Pathophysiologic Processes
3.7. Kidney Health Outcomes
3.8. Heat Protection Interventions for Agricultural Workers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AKI | Acute kidney injury |
| HRI | Heat-related illness |
| CKD | Chronic kidney disease |
| KDIGO | Kidney Disease: Improving Global Outcome |
| GFR | Glomerular filtration rate |
| CRP | C-reactive protein |
| BMI | Body mass index |
| WBGT | Wet-bulb globe temperature |
| TCA | Tricarboxylic acid |
| eGFR | Estimated glomerular filtration rate |
| PHS | Predicted heat strain |
| CKDu | Chronic kidney disease of unknown etiology |
References
- Agricultural Employment Under the Fair Labor Standards Act (FLSA). Available online: https://www.dol.gov/agencies/whd/fact-sheets/12-agricultural-employment-flsa#:~:text=Coverage,ingredients%2C%20may%20be%20secondary%20agriculture (accessed on 26 May 2025).
- Bureau of Labor Statistics. Agricultural Workers. Available online: https://www.bls.gov/ooh/farming-fishing-and-forestry/agricultural-workers.htm (accessed on 26 May 2025).
- Heat Stress and Workers. Available online: https://www.cdc.gov/niosh/heat-stress/about/index.html#:~:text=Overview,may%20lead%20to%20additional%20exposures (accessed on 26 May 2025).
- Farm Labor. Available online: https://www.ers.usda.gov/topics/farm-economy/farm-labor (accessed on 26 May 2025).
- Fleischer, N.L.; Tiesman, H.M.; Sumitani, J.; Mize, T.; Amarnath, K.K.; Bayakly, A.R.; Murphy, M.W. Public health impact of heat-related illness among migrant farmworkers. Am. J. Prev. Med. 2013, 44, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Castillo, F.; Mora, A.M.; Kayser, G.L.; Vanos, J.; Hyland, C.; Yang, A.R.; Eskenazi, B. Environmental Health Threats to Latino Migrant Farmworkers. Annu. Rev. Public Health 2021, 42, 257–276. [Google Scholar] [CrossRef] [PubMed]
- Frank, A.L.; Liebman, A.K.; Ryder, B.; Weir, M.; Arcury, T.A. Health care access and health care workforce for immigrant workers in the agriculture, forestry, and fisheries sector in the southeastern US. Am. J. Ind. Med. 2013, 56, 960–974. [Google Scholar] [CrossRef] [PubMed]
- Hoerster, K.D.; Mayer, J.A.; Gabbard, S.; Kronick, R.G.; Roesch, S.C.; Malcarne, V.L.; Zuniga, M.L. Impact of Individual-, Environmental-, and Policy-Level Factors on Health Care Utilization Among US Farmworkers. Am. J. Public Health 2011, 101, 685–692. [Google Scholar] [CrossRef]
- Levey, A.S.; Eckardt, K.-U.; Dorman, N.M.; Christiansen, S.L.; Hoorn, E.J.; Ingelfinger, J.R.; Inker, L.A.; Levin, A.; Mehrotra, R.; Palevsky, P.M.; et al. Nomenclature for kidney function and disease: Report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int. 2020, 97, 1117–1129. [Google Scholar] [CrossRef]
- Smith, J.H.; Robinson, S.; Pearcy, M. Renal responses to exercise, heat and dehydration. J. Appl. Physiol. 1952, 4, 659–665. [Google Scholar] [CrossRef]
- Liu, J.; Varghese, B.M.; Hansen, A.; Borg, M.A.; Zhang, Y.; Driscoll, T.; Morgan, G.; Dear, K.; Gourley, M.; Capon, A.; et al. Hot weather as a risk factor for kidney disease outcomes: A systematic review and meta-analysis of epidemiological evidence. Sci. Total Environ. 2021, 801, 149806. [Google Scholar] [CrossRef]
- Chapman, C.L.; Hess, H.W.; Lucas, R.A.I.; Glaser, J.; Saran, R.; Bragg-Gresham, J.; Wegman, D.H.; Hansson, E.; Minson, C.T.; Schlader, Z.J. Occupational heat exposure and the risk of chronic kidney disease of nontraditional origin in the United States. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2021, 321, R141–R151. [Google Scholar] [CrossRef]
- Glaser, J.; Lemery, J.; Rajagopalan, B.; Diaz, H.F.; Garcia-Trabanino, R.; Taduri, G.; Madero, M.; Amarasinghe, M.; Abraham, G.; Anutrakulchai, S.; et al. Climate Change and the Emergent Epidemic of CKD from Heat Stress in Rural Communities: The Case for Heat Stress Nephropathy. Clin. J. Am. Soc. Nephrol. 2016, 11, 1472–1483. [Google Scholar] [CrossRef]
- Kazancioğlu, R. Risk factors for chronic kidney disease: An update. Kidney Int. Suppl. 2013, 3, 368–371. [Google Scholar] [CrossRef]
- Kjellstrom, T.; Holmer, I.; Lemke, B. Workplace heat stress, health and productivity—An increasing challenge for low and middle-income countries during climate change. Glob. Health Action 2009, 2, 2047. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.S.; Kim, W.S.; Lim, Y.H.; Hong, Y.C. High Temperatures and Kidney Disease Morbidity: A Systematic Review and Meta-analysis. J. Prev. Med. Public Health 2019, 52, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, R.M.; Proietti, S.; Traxer, O.; Archer, M.; Somani, B.K. Worldwide Impact of Warmer Seasons on the Incidence of Renal Colic and Kidney Stone Disease: Evidence from a Systematic Review of Literature. J. Endourol. 2017, 31, 729–735. [Google Scholar] [CrossRef] [PubMed]
- de Lorenzo, A.; Liaño, F. High temperatures and nephrology: The climate change problem. Nefrologia 2017, 37, 492–500. [Google Scholar] [CrossRef]
- Smith, D.J.; Pius, L.M.; Plantinga, L.C.; Thompson, L.M.; Mac, V.; Hertzberg, V.S. Heat Stress and Kidney Function in Farmworkers in the US: A Scoping Review. J. Agromedicine 2022, 27, 183–192. [Google Scholar] [CrossRef]
- El Khayat, M.; Halwani, D.A.; Hneiny, L.; Alameddine, I.; Haidar, M.A.; Habib, R.R. Impacts of Climate Change and Heat Stress on Farmworkers’ Health: A Scoping Review. Front. Public Health 2022, 10, 782811. [Google Scholar] [CrossRef]
- Berberian, A.G.; Gonzalez, D.J.X.; Cushing, L.J. Racial Disparities in Climate Change-Related Health Effects in the United States. Curr. Environ. Health Rep. 2022, 9, 451–464. [Google Scholar] [CrossRef]
- Ramos, A.K. A Human Rights-Based Approach to Farmworker Health: An Overarching Framework to Address the Social Determinants of Health. J. Agromedicine 2018, 23, 25–31. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 340, c332. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; et al. The CARE guidelines: Consensus-based clinical case reporting guideline development. Glob. Adv. Integr. Med. Health 2013, 2, 38–43. [Google Scholar] [CrossRef]
- Green, L.W.; Kreuter, M.W. Health Program Planning: An Educational and Ecological Approach, 4th ed.; McGraw-Hill Companies: New York, NY, USA, 2005. [Google Scholar]
- Moyce, S.; Armitage, T.; Mitchell, D.; Schenker, M. Acute kidney injury and workload in a sample of California agricultural workers. Am. J. Ind. Med. 2020, 63, 258–268. [Google Scholar] [CrossRef]
- Moyce, S.; Mitchell, D.; Armitage, T.; Tancredi, D.; Joseph, J.; Schenker, M. Heat strain, volume depletion and kidney function in California agricultural workers. Occup. Environ. Med. 2017, 74, 402–409. [Google Scholar] [CrossRef]
- Albu, I.; Elon, L.; Xiuhtecutli, N.; McCauley, L.; Chicas, R. Retention of Agricultural Workers Participating in a Renal Longitudinal Study. J. Agromedicine 2024, 29, 26–33. [Google Scholar] [CrossRef]
- Mix, J.; Elon, L.; Vi Thien Mac, V.; Flocks, J.; Economos, E.; Tovar-Aguilar, A.J.; Stover Hertzberg, V.; McCauley, L.A. Hydration Status, Kidney Function, and Kidney Injury in Florida Agricultural Workers. J. Occup. Environ. Med. 2018, 60, e253–e260. [Google Scholar] [CrossRef]
- Houser, M.C.; Mac, V.; Smith, D.J.; Chicas, R.C.; Xiuhtecutli, N.; Flocks, J.D.; Elon, L.; Tansey, M.G.; Sands, J.M.; McCauley, L.; et al. Inflammation-Related Factors Identified as Biomarkers of Dehydration and Subsequent Acute Kidney Injury in Agricultural Workers. Biol. Res. Nurs. 2021, 23, 676–688. [Google Scholar] [CrossRef]
- Chicas, R.C.; Elon, L.; Xiuhtecutli, N.; Liang, D.; Houser, M.C.; Mwarumba, T.; Berra, L.; Hertzberg, V.; Sands, J.M.; McCauley, L. Longitudinal Renal Function Degradation Among Florida Agricultural Workers. J. Occup. Environ. Med. 2024, 66, 694–705. [Google Scholar] [CrossRef]
- Abasilim, C.; Friedman, L.S.; Martin, M.C.; Madigan, D.; Perez, J.; Morera, M.; Tovar, A.; Roka, F.; Xiuhtecutli, N.; Forst, L.; et al. Risk factors associated with indicators of dehydration among migrant farmworkers. Environ. Res. 2024, 251, 118633. [Google Scholar] [CrossRef]
- Moyce, S.; Mitchell, D.; Vega, A.; Schenker, M. Hydration Choices, Sugary Beverages, and Kidney Injury in Agricultural Workers in California. J. Nurs. Scholarsh. 2020, 52, 369–378. [Google Scholar] [CrossRef]
- Chicas, R.; Xiuhtecutli, N.; Elon, L.; Scammell, M.K.; Steenland, K.; Hertzberg, V.; McCauley, L. Cooling Interventions Among Agricultural Workers: A Pilot Study. Workplace Health Saf. 2021, 69, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Moyce, S.; Joseph, J.; Tancredi, D.; Mitchell, D.; Schenker, M. Cumulative Incidence of Acute Kidney Injury in California’s Agricultural Workers. J. Occup. Environ. Med. 2016, 58, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Chicas, R.; Xiuhtecutli, N.; Dickman, N.E.; Flocks, J.; Scammell, M.K.; Steenland, K.; Hertzberg, V.; McCauley, L. Cooling Interventions Among Agricultural Workers: Qualitative Field-Based Study. Hisp. Health Care Int. 2021, 19, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Flocks, J.; Tovar, J.A.; Economos, E.; Mac, V.V.T.; Mutic, A.; Peterman, K.; McCauley, L. Lessons Learned from Data Collection as Health Screening in Underserved Farmworker Communities. Prog. Community Health Partnersh. 2018, 12, 93–100. [Google Scholar] [CrossRef]
- Chicas, R.C.; Wang, Y.; Weil, E.J.; Elon, L.; Xiuhtecutli, N.; Houser, M.C.; Jones, D.P.; Sands, J.M.; Hertzberg, V.; McCauley, L.; et al. The impact of heat exposures on biomarkers of AKI and plasma metabolome among agricultural and non-agricultural workers. Environ. Int. 2023, 180, 108206. [Google Scholar] [CrossRef]
- Chicas, R.; Suarez, J.; Elon, L.; Xiuhtecutli, N.; House, M.C.; Berra, L.; Sands, J.M.; Hertzberg, V.; McCauley, L. Hydration Interventions Among Agricultural Workers: A Pilot Study. J. Occup. Environ. Med. 2022, 64, e357–e359. [Google Scholar] [CrossRef]
- Heat and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-heat-and-health (accessed on 26 May 2025).
- Liljegren, J.C.; Carhart, R.A.; Lawday, P.; Tschopp, S.; Sharp, R. Modeling the Wet Bulb Globe Temperature Using Standard Meteorological Measurements. J. Occup. Environ. Hyg. 2008, 5, 645–655. [Google Scholar] [CrossRef]
- Gubernot, D.M.; Anderson, G.B.; Hunting, K.L. Characterizing occupational heat-related mortality in the United States, 2000–2010: An analysis using the census of fatal occupational injuries database. Am. J. Ind. Med. 2015, 58, 203–211. [Google Scholar] [CrossRef]
- Kuiper, J.R.; O’Brien, K.M.; Ferguson, K.K.; Buckley, J.P. Urinary specific gravity measures in the U.S. population: Implications for the adjustment of non-persistent chemical urinary biomarker data. Environ. Int. 2021, 156, 106656. [Google Scholar] [CrossRef]
- Lam, M.; Krenz, J.; Palmández, P.; Negrete, M.; Perla, M.; Murphy-Robinson, H.; Spector, J.T. Identification of barriers to the prevention and treatment of heat-related illness in Latino farmworkers using activity-oriented, participatory rural appraisal focus group methods. BMC Public Health 2013, 13, 1004. [Google Scholar] [CrossRef]
- Lebov, J.F.; Valladares, E.; Peña, R.; Peña, E.M.; Sanoff, S.L.; Cisneros, E.C.; Colindres, R.E.; Morgan, D.R.; Hogan, S.L. A Population-Based Study of Prevalence and Risk Factors of Chronic Kidney Disease in León, Nicaragua. Can. J. Kidney Health Dis. 2015, 2, 6. [Google Scholar] [CrossRef]
- Sanoff, S.L.; Callejas, L.; Alonso, C.D.; Hu, Y.; Colindres, R.E.; Chin, H.; Morgan, D.R.; Hogan, S.L. Positive association of renal insufficiency with agriculture employment and unregulated alcohol consumption in Nicaragua. Ren. Fail. 2010, 32, 766–777. [Google Scholar] [CrossRef]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. Exercise and Fluid Replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Taylor, A.J.; Leiper, J.B.; Maughan, R.J. Post-exercise rehydration in man: Effects of volume consumed and drink sodium content. Med. Sci. Sports Exerc. 1996, 28, 1260–1271. [Google Scholar] [CrossRef] [PubMed]
- Kellum, J.A.; Lameire, N.; Group, K.A.G.W. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit. Care 2013, 17, 204. [Google Scholar] [CrossRef] [PubMed]
- Waikar, S.S.; Bonventre, J.V. Creatinine Kinetics and the Definition of Acute Kidney Injury. J. Am. Soc. Nephrol. 2009, 20, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Ostermann, M.; Zarbock, A.; Goldstein, S.; Kashani, K.; Macedo, E.; Murugan, R.; Bell, M.; Forni, L.; Guzzi, L.; Joannidis, M.; et al. Recommendations on AKI Biomarkers From the Acute Disease Quality Initiative Consensus Conference. JAMA Netw. Open 2020, 3, e2019209. [Google Scholar] [CrossRef]
- Anthony, M.; Williams, J.M.; Avery, A.M. Health Needs of Migrant and Seasonal Farmworkers. J. Community Health Nurs. 2008, 25, 153–160. [Google Scholar] [CrossRef]
- Langer, C.E.; Mitchell, D.C.; Armitage, T.L.; Moyce, S.C.; Tancredi, D.J.; Castro, J.; Vega-Arroyo, A.J.; Bennett, D.H.; Schenker, M.B. Are Cal/OSHA Regulations Protecting Farmworkers in California From Heat-Related Illness? J. Occup. Environ. Med. 2021, 63, 532–539. [Google Scholar] [CrossRef]
- Marquez, D.; Krenz, J.E.; Santos, E.C.; Torres, E.; Palmández, P.; Sampson, P.D.; Blancas, M.; Carmona, J.; Spector, J.T. The effect of participatory heat education on agricultural worker knowledge. J. Agromedicine 2022, 28, 187–198. [Google Scholar] [CrossRef]
- Nerbass, F.B.; Pecoits-Filho, R.; Clark, W.F.; Sontrop, J.M.; McIntyre, C.W.; Moist, L. Occupational Heat Stress and Kidney Health: From Farms to Factories. Kidney Int. Rep. 2017, 2, 998–1008. [Google Scholar] [CrossRef]
- Crowe, J.; Wesseling, C.; Solano, B.R.; Umaña, M.P.; Ramírez, A.R.; Kjellstrom, T.; Morales, D.; Nilsson, M. Heat exposure in sugarcane harvesters in Costa Rica. Am. J. Ind. Med. 2013, 56, 1157–1164. [Google Scholar] [CrossRef] [PubMed]
- Peraza, S.; Wesseling, C.; Aragon, A.; Leiva, R.; García-Trabanino, R.A.; Torres, C.; Jakobsson, K.; Elinder, C.G.; Hogstedt, C. Decreased Kidney Function Among Agricultural Workers in El Salvador. Am. J. Kidney Dis. 2012, 59, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Flores, S.; Rider, A.C.; Alter, H.J. Mesoamerican nephropathy: A novel case of kidney failure in a US ED. Am. J. Emerg. Med. 2016, 34, 1323.e5–1323.e6. [Google Scholar] [CrossRef] [PubMed]
- Occupational Employment and Wage Statistics. Available online: https://www.bls.gov/oes/2023/may/oes450000.htm (accessed on 26 May 2025).
- Havenith, G.; Fiala, D. Thermal Indices and Thermophysiological Modeling for Heat Stress. Compr. Physiol. 2015, 6, 255–302. [Google Scholar] [CrossRef]
- Parsons, K. Occupational Health Impacts of Climate Change: Current and Future ISO Standards for the Assessment of Heat Stress. Ind. Health 2013, 51, 86–100. [Google Scholar] [CrossRef]
- Gao, C.; Kuklane, K.; Östergren, P.-O.; Kjellstrom, T.; Gao, C.; Kuklane, K.; Östergren, P.-O.; Kjellstrom, T. Occupational heat stress assessment and protective strategies in the context of climate change. Int. J. Biometeorol. 2017, 62, 359–371. [Google Scholar] [CrossRef]
- Chang, C.-J.; Yang, H.-Y. Chronic Kidney Disease Among Agricultural Workers in Taiwan: A Nationwide Population-Based Study. Kidney Int. Rep. 2023, 8, 2677–2689. [Google Scholar] [CrossRef]
- Keogh, S.A.; Leibler, J.H.; Sennett Decker, C.M.; Amador Velázquez, J.J.; Jarquin, E.R.; Lopez-Pilarte, D.; Garcia-Trabanino, R.; Delgado, I.S.; Petropoulos, Z.E.; Friedman, D.J.; et al. High prevalence of chronic kidney disease of unknown etiology among workers in the Mesoamerican Nephropathy Occupational Study. BMC Nephrol. 2022, 23, 238. [Google Scholar] [CrossRef]
- Chawla, L.S.; Kimmel, P.L. Acute kidney injury and chronic kidney disease: An integrated clinical syndrome. Kidney Int. 2012, 82, 516–524. [Google Scholar] [CrossRef]
- Wesseling, C.; Crowe, J.; Hogstedt, C.; Jakobsson, K.; Lucas, R.; Wegman, D.H. Resolving the Enigma of the Mesoamerican Nephropathy: A Research Workshop Summary. Am. J. Kidney Dis. 2014, 63, 396–404. [Google Scholar] [CrossRef]
- Valcke, M.; Levasseur, M.-E.; Soares da Silva, A.; Wesseling, C. Pesticide exposures and chronic kidney disease of unknown etiology: An epidemiologic review. Environ. Health 2017, 16, 49. [Google Scholar] [CrossRef] [PubMed]
- Lebov, J.F.; Engel, L.S.; Richardson, D.; Hogan, S.L.; Hoppin, J.A.; Sandler, D.P. Pesticide use and risk of end-stage renal disease among licensed pesticide applicators in the Agricultural Health Study. Occup. Environ. Med. 2016, 73, 3–12. [Google Scholar] [CrossRef]
- Kim, S.-J.; Gil, H.-W.; Yang, J.-O.; Lee, E.-Y.; Hong, S.-Y. The clinical features of acute kidney injury in patients with acute paraquat intoxication. Nephrol. Dial. Transplant. 2009, 24, 1226–1232. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, F.; Endre, Z.H.; Pickering, J.W.; Jayamanne, S.; Palangasinghe, C.; Shahmy, S.; Chathuranga, U.; Wijerathna, T.; Shihana, F.; Gawarammana, I.; et al. Mechanism-specific injury biomarkers predict nephrotoxicity early following glyphosate surfactant herbicide (GPSH) poisoning. Toxicol. Lett. 2016, 258, 1–10. [Google Scholar] [CrossRef]
- Stratton, S.J. Population Research: Convenience Sampling Strategies. Prehospital Disaster Med. 2021, 36, 373–374. [Google Scholar] [CrossRef]
- Noyes, J. The trials and tribulations of trial registration and reporting: Why are some nursing trials still slipping through the net? J. Adv. Nurs. 2021, 77, e38–e40. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, J.J.; Leyva, E.W.; Wong, K.A.; Kataoka-Yahiro, M.; Saligan, L.N. Heat Stress and Determinants of Kidney Health Among Agricultural Workers in the United States: An Integrative Review. Int. J. Environ. Res. Public Health 2025, 22, 1268. https://doi.org/10.3390/ijerph22081268
Zhao JJ, Leyva EW, Wong KA, Kataoka-Yahiro M, Saligan LN. Heat Stress and Determinants of Kidney Health Among Agricultural Workers in the United States: An Integrative Review. International Journal of Environmental Research and Public Health. 2025; 22(8):1268. https://doi.org/10.3390/ijerph22081268
Chicago/Turabian StyleZhao, Justin J., Erwin W. Leyva, Kamomilani A. Wong, Merle Kataoka-Yahiro, and Leorey N. Saligan. 2025. "Heat Stress and Determinants of Kidney Health Among Agricultural Workers in the United States: An Integrative Review" International Journal of Environmental Research and Public Health 22, no. 8: 1268. https://doi.org/10.3390/ijerph22081268
APA StyleZhao, J. J., Leyva, E. W., Wong, K. A., Kataoka-Yahiro, M., & Saligan, L. N. (2025). Heat Stress and Determinants of Kidney Health Among Agricultural Workers in the United States: An Integrative Review. International Journal of Environmental Research and Public Health, 22(8), 1268. https://doi.org/10.3390/ijerph22081268






