A Resistance Training Program on Patients with Liver Cirrhosis: A Randomized Clinical Trial
Abstract
1. Introduction
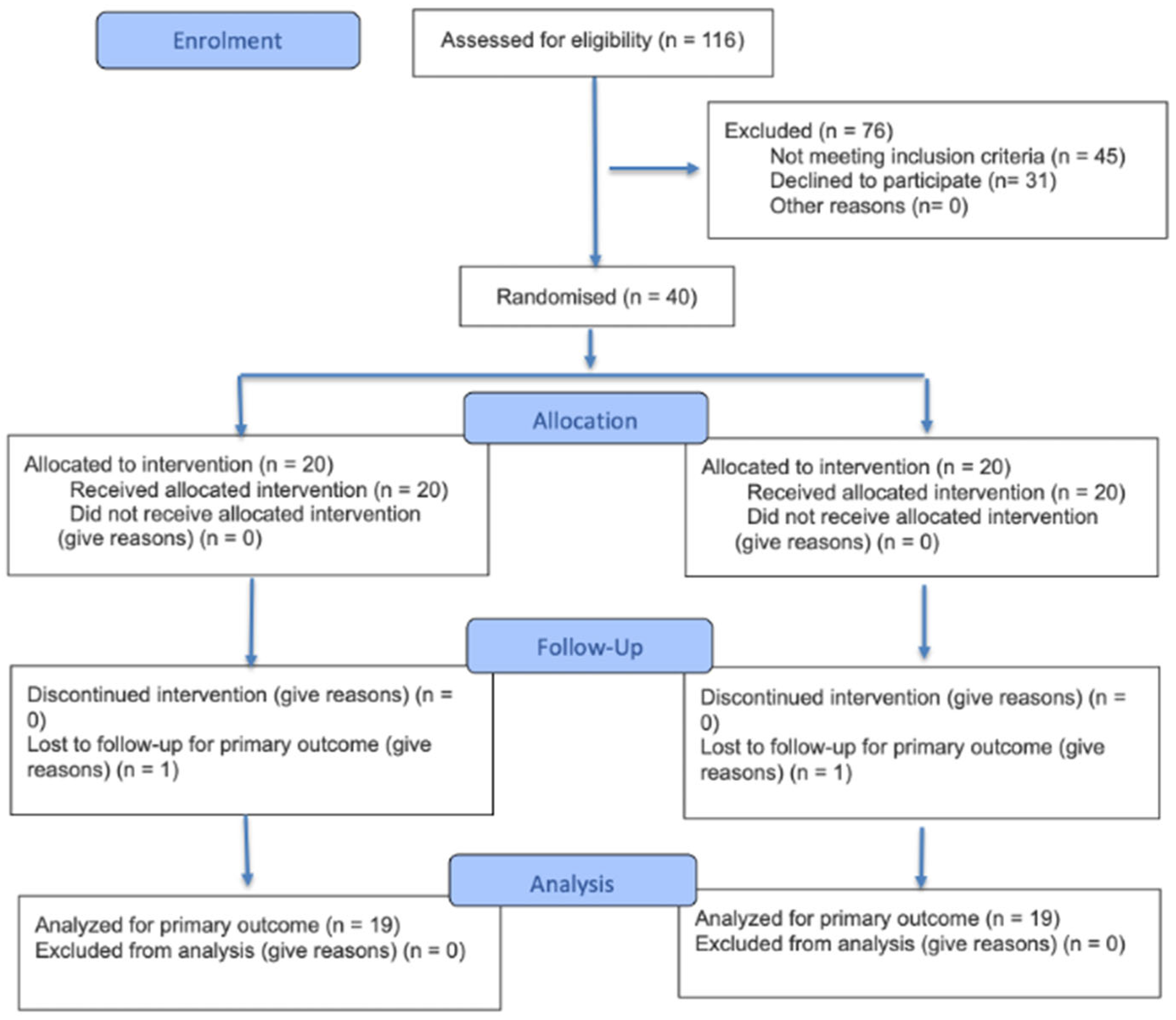
2. Materials and Methods
2.1. Participants
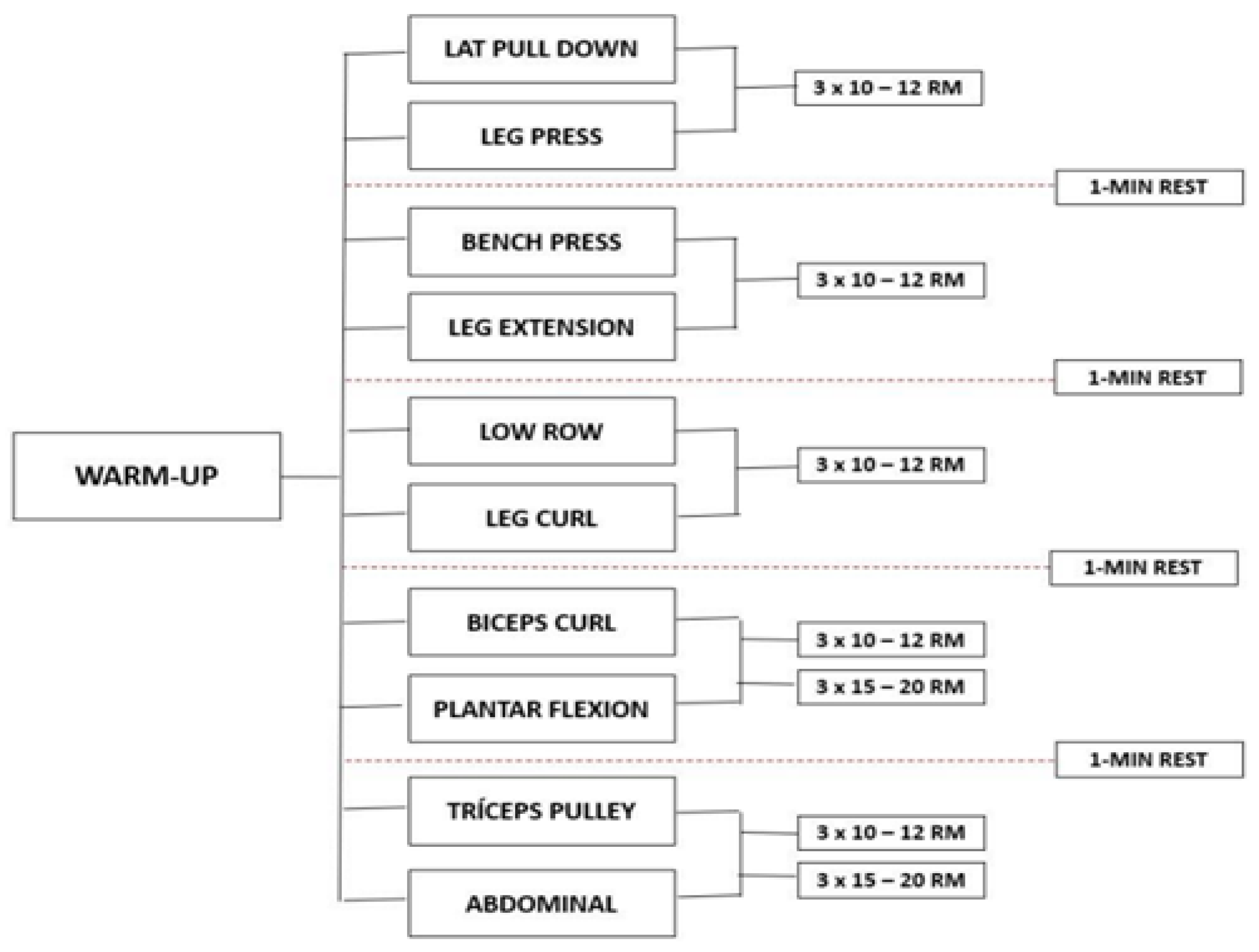
2.2. Experimental Procedure
2.3. Measures and Procedures
2.4. Statistical Analysis
3. Results
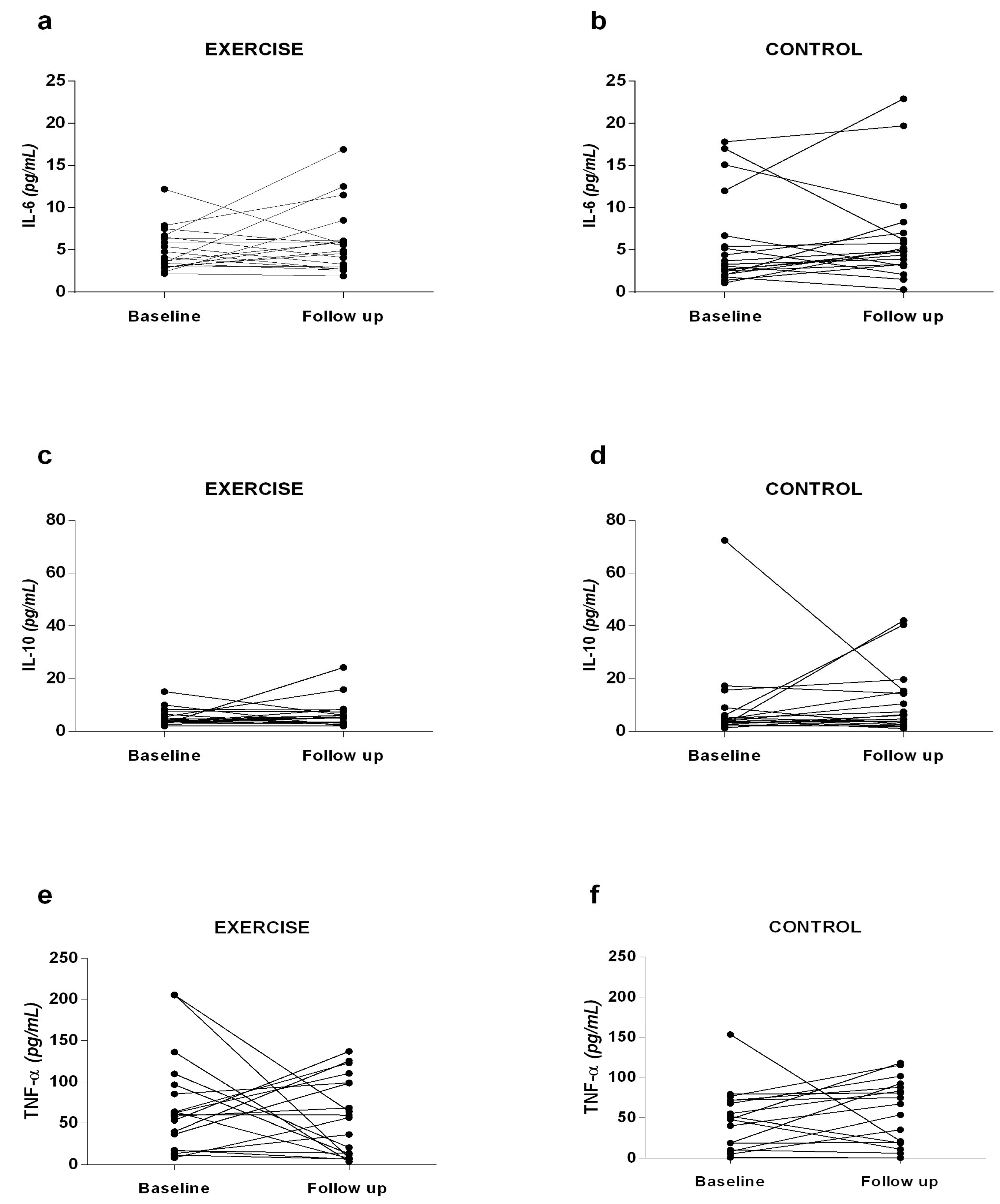
3.1. Inflammatory Profile
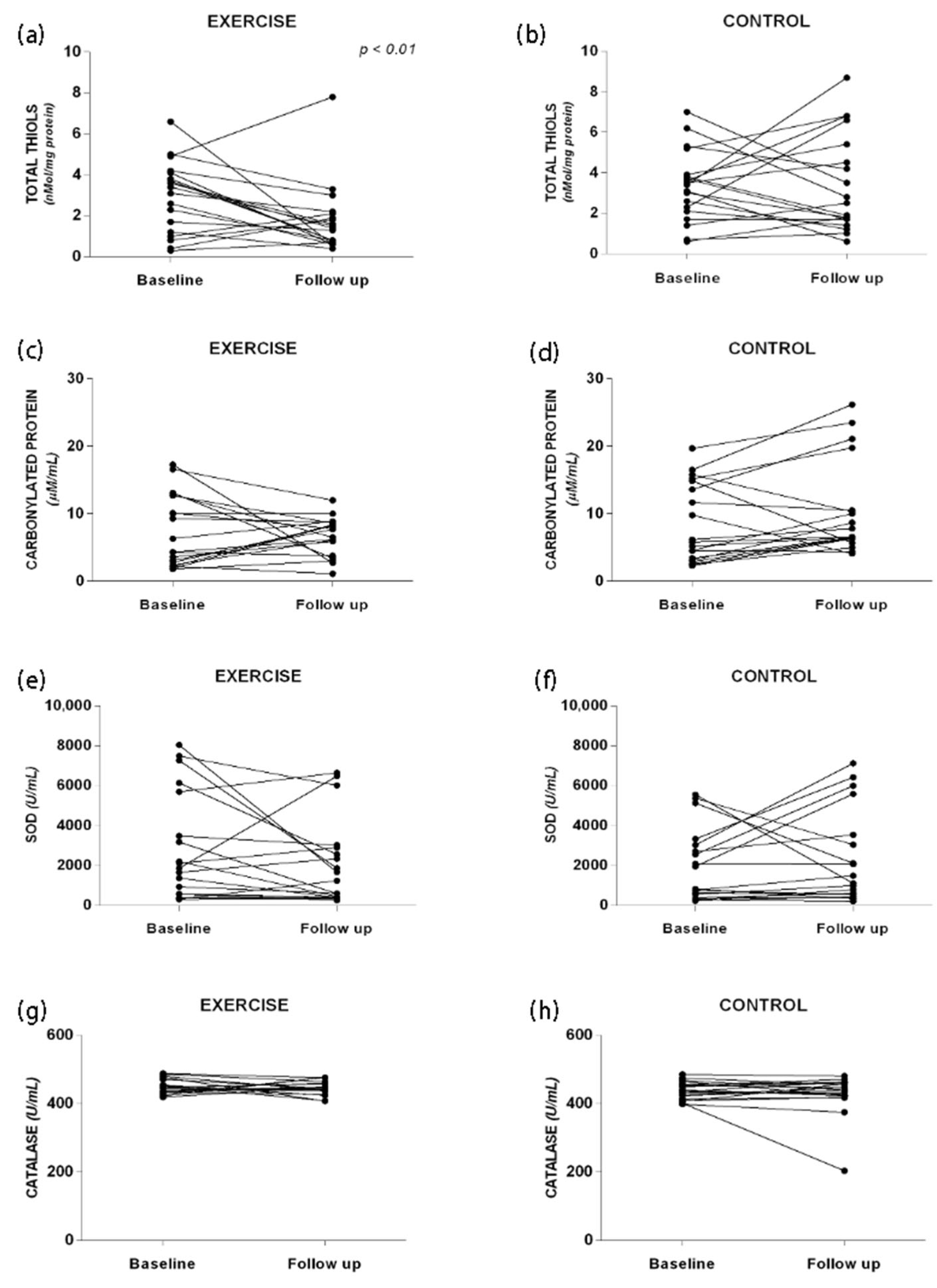
3.2. Oxidative Stress
3.3. Blood Analysis and Body Composition
3.4. Muscle Strength
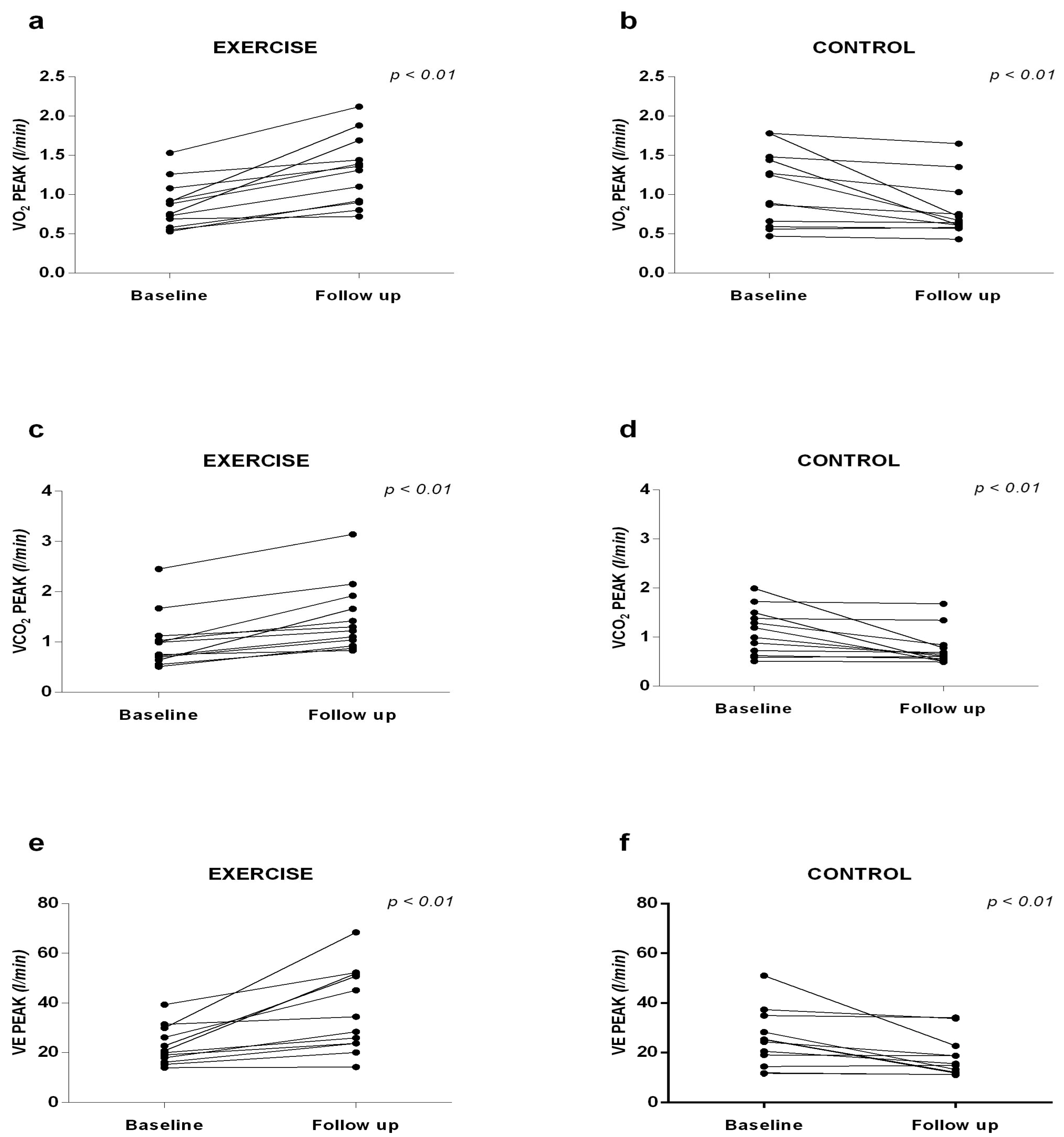
3.5. Cardiorespiratory Capacity
3.6. Exercise Capacity
3.7. Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EG | Experimental Group |
| CG | Control Group |
| BMI | Body Mass Index |
| IL | Interleukin |
| TNF-α | Necrosis Factor Alpha |
| PC | Protein Carbonyls |
| SOD | Enzymes Superoxide Dismutase |
References
- Debette-Gratien, M.; Tabouret, T.; Antonini, M.T.; Dalmay, F.; Carrier, P.; Legros, R.; Jacques, J.; Vincent, F.; Sautereau, D.; Samuel, D.; et al. Personalized adapted physical activity before liver transplantation: Acceptability and results. Transplantation 2014, 99, 145–150. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine. ACSMs Exercise Management for Persons with Chronic Diseases and Disabilities, 4th ed.; Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- Kawaguchi, T.; Kawaguchi, A.; Hashida, R.; Nakano, D.; Tsutsumi, T.; Kawaguchi, M.; Koya, S.; Hirota, K.; Tomita, M.; Tsuchihashi, J.; et al. Resistance exercise in combination with aerobic exercise reduces the incidence of serious events in patients with liver cirrhosis: A meta-analysis of randomized controlled trials. J. Gastroenterol. 2024, 59, 216–228. [Google Scholar] [CrossRef] [PubMed]
- Clària, J.; Stauber, R.E.; Coenraad, M.J.; Moreau, R.; Jalan, R.; Pavesi, M.; Amorós, Á.; Titos, E.; Alcaraz-Quiles, J.; Oettl, K.; et al. Systemic inflammation in decompensated cirrhosis: Characterization and role in acute-on-chronic liver failure. Hepatology 2016, 64, 1249–1264. [Google Scholar] [CrossRef] [PubMed]
- Sak, J.J.; Prystupa, A.; Bis-Wencel, H.; Kiciński, P.; Luchowska-Kocot, D.; Krukowski, H.; Nowicki, G.J.; Panasiuk, L. Oxidative stress-induced growth inhibitor 1 in alcohol-induced liver cirrhosis. Ann. Agric. Environ. Med. 2021, 28, 676–680. [Google Scholar] [CrossRef]
- Bala, S.; Csak, T.; Saha, B.; Zatsiorsky, J.; Kodys, K.; Catalano, D.; Satishchandran, A.; Szabo, G. The pro-inflammatory effects of miR-155 promote liver fibrosis and alcohol-induced steatohepatitis. J. Hepatol. 2016, 64, 1378–1387. [Google Scholar] [CrossRef]
- Hao, Y.; Song, K.; Tan, X.; Ren, L.; Guo, X.; Zhou, C. Reactive Oxygen Species-Responsive Polypeptide Drug Delivery System Targeted Activated Hepatic Stellate Cells to Ameliorate Liver Fibrosis. ACS Nano 2022, 16, 20739–20757. [Google Scholar] [CrossRef]
- Solanki, N.; Salvi, A.; Patki, G.; Salim, S. Modulating Oxidative Stress Relieves Stress-Induced Behavioral and Cognitive Impairments in Rats. Int. J. Neuropsychopharmacol. 2017, 20, 550–561. [Google Scholar] [CrossRef]
- Azizbeigi, K.; Azarbayjani, M.A.; Atashak, S.; Stannard, S.R. Effect of moderate and high resistance training intensity on indices of inflammatory and oxidative stress. Res. Sports Med. 2015, 23, 73–87. [Google Scholar] [CrossRef]
- Arazi, H.; Taati, B.; Suzuki, K. A Review of the Effects of Leucine Metabolite (β-Hydroxy-β-methylbutyrate) Supplementation and Resistance Training on Inflammatory Markers: A New Approach to Oxidative Stress and Cardiovascular Risk Factors. Antioxidants 2018, 7, 148. [Google Scholar] [CrossRef]
- Ryrsø, C.K.; Thaning, P.; Siebenmann, C.; Lundby, C.; Lange, P.; Pedersen, B.K.; Hellsten, Y.; Iepsen, U.W. Effect of endurance versus resistance training on local muscle and systemic inflammation and oxidative stress in COPD. Scand. J. Med. Sci. Sports 2018, 28, 2339–2348. [Google Scholar] [CrossRef]
- Oh, S.; Tanaka, K.; Warabi, E.; Shoda, J. Exercise reduces inflammation and oxidative stress in obesity-related liver diseases. Med. Sci. Sports Exerc. 2013, 45, 2214–2222. [Google Scholar] [CrossRef]
- Farinha, J.B.; Ramis, T.R.; Vieira, A.F.; Macedo, R.C.O.; Rodrigues-Krause, J.; Boeno, F.P.; Schroeder, H.T.; Muller, C.H.; Boff, W.; Krause, M.; et al. Glycemic, inflammatory and oxidative stress responses to different high-intensity training protocols in type 1 diabetes: A randomized clinical trial. J. Diabetes Complicat. 2018, 32, 1124–1132. [Google Scholar] [CrossRef]
- Corrêa, H.L.; Moura, S.R.G.; Neves, R.V.P.; Tzanno-Martins, C.; Souza, M.K.; Haro, A.S.; Costa, F.; Silva, J.A.B.; Stone, W.; Honorato, F.S.; et al. Resistance training improves sleep quality, redox balance and inflammatory profile in maintenance hemodialysis patients: A randomized controlled trial. Sci. Rep. 2020, 10, 11708. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, C.S.; Oliveira, R.; Bento, F.; Geraldo, D.; Rodrigues, J.V.; Marcos, J.C. Simplified 2,4-dinitrophenylhydrazine spectrophotometric assay for quantification of carbonyls in oxidized proteins. Anal. Biochem. 2014, 458, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Porter, C.; Reidy, P.T.; Bhattarai, N.; Sidossis, L.S.; Rasmussen, B.B. Resistance Exercise Training Alters Mitochondrial Function in Human Skeletal Muscle. Med. Sci. Sports Exerc. 2015, 47, 1922–1931. [Google Scholar] [CrossRef] [PubMed]
- Groennebaek, T.; Vissing, K. Impact of Resistance Training on Skeletal Muscle Mitochondrial Biogenesis, Content, and Function. Front. Physiol. 2017, 8, 713. [Google Scholar] [CrossRef]
- Calle, M.C.; Fernandez, M.L. Effects of resistance training on the inflammatory response. Nutr. Res. Pract. 2010, 4, 259–269. [Google Scholar] [CrossRef]
- Kim, S.D.; Yeun, Y.R. Effects of Resistance Training on C-Reactive Protein and Inflammatory Cytokines in Elderly Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public. Health 2022, 19, 3434. [Google Scholar] [CrossRef]
- American College of Sports Medicine. ACSM Position Stand: Progression Models in Resistance Training for Healthy Adults. Med. Sci. Sports Exerc. 2009, 41, 687–708. [Google Scholar] [CrossRef]
- Aebi, H. Catalase in vitro. Methods Enzymol. 1984, 105, 121–126. [Google Scholar]
- Misra, H.P.; Fridovich, I. The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar] [CrossRef]
- Figueiredo, I.M.; Sampaio, R.F.; Mancini, M.C.; Silva, F.C.M.; Souza, M.A.P. Teste de força de preensão utilizando o dinamômetro Jammar. Acta Fisiatr. 2007, 14, 104–110. [Google Scholar] [CrossRef]
- Neder, J.A.; Nery, L.E. Fisiologia Clínica do Exercício: Teoria e Prática, 1st ed.; Artes Médicas: São Paulo, Brazil, 2002. [Google Scholar]
- ATS—American Thoracic Society. Guidelines for the 6-minute walk test. Am. J. Crit. Care 2002, 166, 111–117. [Google Scholar]
- Ware Jr, J.E.; Sherbourne, D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Adorno, M.L.G.R.; Brasil-Neto, J.P. Avaliação da qualidade de vida com o instrumento SF-36 em lombalgia crônica. Acta Ortop. Bras. 2013, 21, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.J.; Wang, X.Z. Interleukin-10 and chronic liver disease. World J. Gastroenterol. 2006, 12, 1681–1685. [Google Scholar] [CrossRef] [PubMed]
- Hammerich, L.; Tacke, F. Interleukins in chronic liver disease: Lessons learned from experimental mouse models. Clin. Exp. Gastroenterol. 2014, 7, 297–306. [Google Scholar] [CrossRef]
- Cichoz-Lach, H.; Michalak, A. Oxidative stress as a crucial factor in liver diseases. World J. Gastroenterol. 2014, 20, 8082–8091. [Google Scholar] [CrossRef]
- Hadi Yasa, M.; Kacmaz, M.; Serda Ozturk, H.; Durak, I. Antioxidant status of erythrocytes from patients with cirrhosis. Hepatogastroenterology 1999, 46, 2460–2463. [Google Scholar]
- Singh, R.; Singh, R.K.; Tripathi, A.K.; Cornelissen, G.; Schwartzkopff, O.; Otsuka, K.; Halberg, F. Chronomics of circulating plasma lipid peroxides and antioxidant enzymes and other related molecules in cirrhosis of liver. In the memory of late Shri Chetan Singh. Biomed. Pharmacother. 2005, 59, 229–235. [Google Scholar] [CrossRef]
- Pandey, K.B.; Rizvi, S.I. Markers of oxidative stress in erythrocytes and plasma during aging in humans. Oxid. Med. Cell Longev. 2010, 3, 2–12. [Google Scholar] [CrossRef]
- Warner, A.; Bencosme, A.; Healy, D.; Verme, C. Prognostic role of antioxidant enzymes in sepsis: Preliminary assessment. Clin. Chem. 1995, 41, 867–871. [Google Scholar] [CrossRef]
- Dasarathy, S. Exercise and physical activity in cirrhosis: Opportunities or perils. J. Appl. Physiol. (1985) 2020, 128, 1547–1559. [Google Scholar]
- Jones, D.A.; Rutherford, O.M.; Parker, D.F. Physiological changes in skeletal muscle as a result of strength training. Q. J. Exp. Physiol. 1989, 74, 365–371. [Google Scholar] [CrossRef]
- Aamann, L.; Dam, G.; Borre, M.; Drljevic-Nielsen, A.; Overgaard, K.; Andersen, H.; Vilstrup, H.; Aagaard, N. Resistance Training Increases Muscle Strength and Muscle Size in Patients with Liver Cirrhosis. Clin. Gastroenterol. Hepatol. 2019, 18, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.C.; Coombes, J.S.; Macdonald, G.A. Exercise capacity and muscle strength in patients with cirrhosis. Liver Transpl. 2012, 18, 146–151. [Google Scholar] [CrossRef]
- Hiraoka, A.; Michitakaa, K.; Kiguchib, D.; Izumotoa, H.; Uekia, H.; Kanetoa, M.; Kitahataa, S.; Aibikia, T.; Okudairaa, T.; Tomidaa, H.; et al. Efficacy of branched-chain amino acid supplementation and walking exercise for preventing sarcopenia in patients with liver cirrhosis. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1416–1423. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.T.A.; Oliver, J.L.; Lloyd, R.; Pedley, J.S.; Radnor, J.M. The Influence of Growth, Maturation and Resistance Training on Muscle-Tendon and Neuromuscular Adaptations: A Narrative Review. Sports 2021, 9, 59. [Google Scholar] [CrossRef] [PubMed]
- Matos, F.; Amaral, J.; Martinez, E.; Canário-Lemos, R.; Moreira, T.; Cavalcante, J.; Peixoto, R.; Pinheiro, B.N.; Scipião Junior, L.; Uchoa, P.; et al. Changes in Muscle Thickness after 8 Weeks of Strength Training, Electromyostimulation, and Both Combined in Healthy Young Adults. Int. J. Environ. Res. Public. Health 2022, 19, 3184. [Google Scholar] [CrossRef]
- Lacio, M.; Vieira, J.G.; Trybulski, R.; Campos, Y.; Santana, D.; Elias Filho, J.; Novaes, J.; Vianna, J.M.; Wilk, M. Effects of Resistance Training Performed with Different Loads in Untrained and Trained Male Adult Individuals on Maximal Strength and Muscle Hypertrophy: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 11237. [Google Scholar] [CrossRef]
- Deliceoğlu, G.; Kabak, B.; Çakır, V.O.; Ceylan, H.I.; Raul-Ioan, M.; Alexe, D.I.; Stefanica, V. Respiratory Muscle Strength as a Predictor of VO2max and Aerobic Endurance in Competitive Athletes. Appl. Sci. 2024, 14, 8976. [Google Scholar] [CrossRef]
- Artero, E.G.; Lee, D.-C.; Lavie, C.J.; España-Romero, V.; Sui, X.; Church, T.C.; Blair, S.N. Effects of muscular strength on cardiovascular risk factors and prognosis. J. Cardiopulm. Rehabil. Prev. 2012, 32, 351–358. [Google Scholar] [CrossRef]
- Carey, E.J.; Steidley, D.E.; Aqel, B.A.; Byrne, T.J.; Mekeel, K.L.; Rakela, J.; Vargas, H.E.; Douglas, D. Six-Minute Walk Distance Predicts Mortality in Liver Transplant Candidates. Liver Transpl. 2010, 16, 1373–1378. [Google Scholar] [CrossRef]
- Marchesini, G.; Bianchi, G.; Amodio, P.; Salerno, F.; Merli, M.; Panella, M.; Loguercio, C.; Apolone, G.; Niero, M.; Abbiati, R. Factors Associated with Poor Health-Related Quality of Life of Patients with Cirrhosis. Gastroenterology 2001, 120, 170–178. [Google Scholar] [CrossRef]
- Román, E.; Torrades, M.T.; Nadal, M.J.; Cárdenas, G.; Nieto, J.C.; Vidal, S.; Bascunãna, H.; Juárez, C.; Guamer, C.; Córdoba, J.; et al. Randomized pilot study: Effects of an exercise programme and leucine supplementation in patients with cirrhosis. Dig. Dis. Sci. 2014, 59, 1966–1975. [Google Scholar] [CrossRef]
- Zenith, L.; Meena, N.; Ramadi, A.; Yavari, M.; Harvey, A.; Carbonneau, M.; Ma, M.; Abraldes, J.G.; Paterson, I.; Haykowsky, M.J.; et al. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 2014, 12, 1920–1926. [Google Scholar] [CrossRef]
| Exercise Group | Control Group | p Value | |
|---|---|---|---|
| Gender, n (female, male) | 12/7 | 12/7 | 1.00 |
| Age, years | 58.9 ± 10.1 | 59.6 ± 8.8 | 0.35 |
| Weight, Kg | 75.8 ± 17.3 | 76.4 ± 14.8 | 0.37 |
| Height, cm | 158 ± 12 | 162 ± 8 | 0.51 |
| BMI, Kg/m2 | 29.9 ± 5.3 | 27.9 ± 4.5 | 0.11 |
| Etiology of Cirrhosis, n | |||
| Hepatitis C Virus | 10 | 10 | 1.00 |
| Non-Alcoholic Steatohepatitis | 8 | 8 | 1.00 |
| Alcohol | 1 | 1 | 1.00 |
| Child–Pugh class, n | |||
| Child–Pugh A | 19 | 18 | 1.00 |
| Child-Pugh B | 0 | 1 | 1.00 |
| Use of Propranolol (yes/no) | 4/15 | 9/10 | 0.91 |
| Previous Ascites (yes/no) | 1/18 | 2/17 | 0.60 |
| Previous of Edema (yes/no) | 0/19 | 0/19 | 1.00 |
| Variceal Bleeding (yes/no) | 4/13 | 4/15 | 1.00 |
| Portal Vein Thrombosis (yes/no) | 2/17 | 1/18 | 1.00 |
| Esophageal Varices (yes/no) | 7/12 | 11/9 | 0.19 |
| Encephalopathy (yes/no) | 0/19 | 1/18 | 0.48 |
| Glucose, mg/dL | 111 ± 26 | 112 ± 46 | 0.70 |
| Albumin Serum, g/dL | 4.2 ± 0.4 | 3.9 ± 0.8 | 0.13 |
| Prothrombin Time, % | 81 ± 14 | 79 ± 20 | 0.80 |
| INR | 1.14 ± 0.13 | 1.19 ± 0.15 | 0.37 |
| Serum Bilirubin, mg/dL | 1.03 ± 1.05 | 1.12 ± 1.09 | 0.81 |
| AST, U/L | 52 ± 35 | 41 ± 19 | 0.18 |
| ALT, U/L | 56 ± 36 | 45 ± 17 | 0.60 |
| Exercise Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p Value | Baseline | Follow-Up | p Value | |
| Body Composition | ||||||
| BMI, Kg/m2 | 30.0 ± 5.3 | 29.5 ± 5.0 * | <0.01 * | 28.0 ± 4.5 | 28.1 ± 5.1 | 0.40 |
| Lean Mass, kg | 27.7 ± 7.6 | 27.0 ± 7.0 | 0.66 | 27.1 ± 7.1 | 27.1 ± 6.1 | 0.90 |
| Fat Mass, Kg | 28.2 ± 10.6 | 27.4 ± 10.7 | 0.33 | 25.5 ± 9.0 | 25.4 ± 9.5 | 0.91 |
| Exercise Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p Value | Baseline | Follow-Up | p Value | |
| Muscle Strength | ||||||
| Handgrip, Kgf | 27.4 ± 13.9 | 30.0 ± 15.5 | <0.01 * | 25.6 ± 9.2 | 21.3 ± 9.0 | <0.01 * |
| Total Training Volume | ||||||
| Lat Pull-down | 464 ± 227 | 862 ± 320 | <0.01 * | - | - | |
| Leg Press | 615 ± 270 | 1297 ± 443 | <0.01 * | - | - | |
| Bench Press | 248 ± 153 | 416 ± 264 | <0.01 * | - | - | |
| Leg Extension | 558 ± 359 | 1080 ± 491 | <0.01 * | - | - | |
| Low Row | 473 ± 226 | 826 ± 326 | <0.01 * | - | - | |
| Leg Curl | 530 ± 314 | 1051 ± 371 | <0.01 * | - | - | |
| Biceps Curl | 701 ± 280 | 1165 ± 336 | <0.01 * | - | - | |
| Tríceps Pulley | 445 ± 283 | 786 ± 546 | <0.01 * | - | - | |
| Exercise Capacity | ||||||
| 6 min Walk Test, m | 456 ± 95 | 525 ± 95 | <0.01 | 476 ± 51 | 461 ± 75 | 0.18 |
| Exercise Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p Value | Baseline | Follow-Up | p Value | |
| Quality of Life | ||||||
| Physical Function | 74 ± 23 | 90 ± 8 | <0.01 * | 74 ± 19 | 71 ± 20 | 0.49 |
| Role Physical | 59 ± 41 | 96 ± 12 | <0.01 * | 58 ± 47 | 61 ± 44 | 0.72 |
| Bodily Pain | 52 ± 23 | 70 ± 14 | <0.01 * | 52 ± 27 | 61 ± 23 | 0.16 |
| General Health | 64 ± 23 | 76 ± 19 | <0.01 * | 64 ± 17 | 65 ± 17 | 0.87 |
| Vitality | 68 ± 23 | 80 ± 16 | 0.06 | 56 ± 23 | 60 ± 24 | 0.45 |
| Social Function | 81 ± 23 | 95 ± 10 | 0.03 * | 65 ± 36 | 68 ± 30 | 0.67 |
| Role Emotional | 54 ± 43 | 91 ± 27 | <0.01 * | 47 ± 47 | 56 ± 47 | 0.39 |
| Mental Health | 71 ± 15 | 81 ± 13 | 0.03 * | 62 ± 25 | 64 ± 30 | 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, A.; Dias, I.; da Silva Novaes, J.; Sant’Ana, L.; Felix, B.P.; Cahuê, F.; Brito-Azevedo, A.; Reis, M.S.; Lopes, A.J.; Salerno, V.; et al. A Resistance Training Program on Patients with Liver Cirrhosis: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2025, 22, 1257. https://doi.org/10.3390/ijerph22081257
Brown A, Dias I, da Silva Novaes J, Sant’Ana L, Felix BP, Cahuê F, Brito-Azevedo A, Reis MS, Lopes AJ, Salerno V, et al. A Resistance Training Program on Patients with Liver Cirrhosis: A Randomized Clinical Trial. International Journal of Environmental Research and Public Health. 2025; 22(8):1257. https://doi.org/10.3390/ijerph22081257
Chicago/Turabian StyleBrown, Amanda, Ingrid Dias, Jefferson da Silva Novaes, Leandro Sant’Ana, Bruno Perez Felix, Fabio Cahuê, Anderson Brito-Azevedo, Michel Silva Reis, Agnaldo José Lopes, Verônica Salerno, and et al. 2025. "A Resistance Training Program on Patients with Liver Cirrhosis: A Randomized Clinical Trial" International Journal of Environmental Research and Public Health 22, no. 8: 1257. https://doi.org/10.3390/ijerph22081257
APA StyleBrown, A., Dias, I., da Silva Novaes, J., Sant’Ana, L., Felix, B. P., Cahuê, F., Brito-Azevedo, A., Reis, M. S., Lopes, A. J., Salerno, V., Simão, R., Monteiro, E. R., & Perez, R. d. M. (2025). A Resistance Training Program on Patients with Liver Cirrhosis: A Randomized Clinical Trial. International Journal of Environmental Research and Public Health, 22(8), 1257. https://doi.org/10.3390/ijerph22081257









