Telehealth-Readiness, Healthcare Access, and Cardiovascular Health in the Deep South: A Spatial Perspective
Abstract
1. Introduction
1.1. Background
1.2. Literature Review
1.2.1. Rural Health Conditions and Structural Barriers
1.2.2. Digital Infrastructure as a Social Determinant of Health
1.2.3. Telehealth and Cardiovascular Outcomes
1.3. Theoretical Framework
1.4. Hypotheses
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Outcome Variables
2.3. Independent Variables
2.4. Statistical Analysis
3. Results
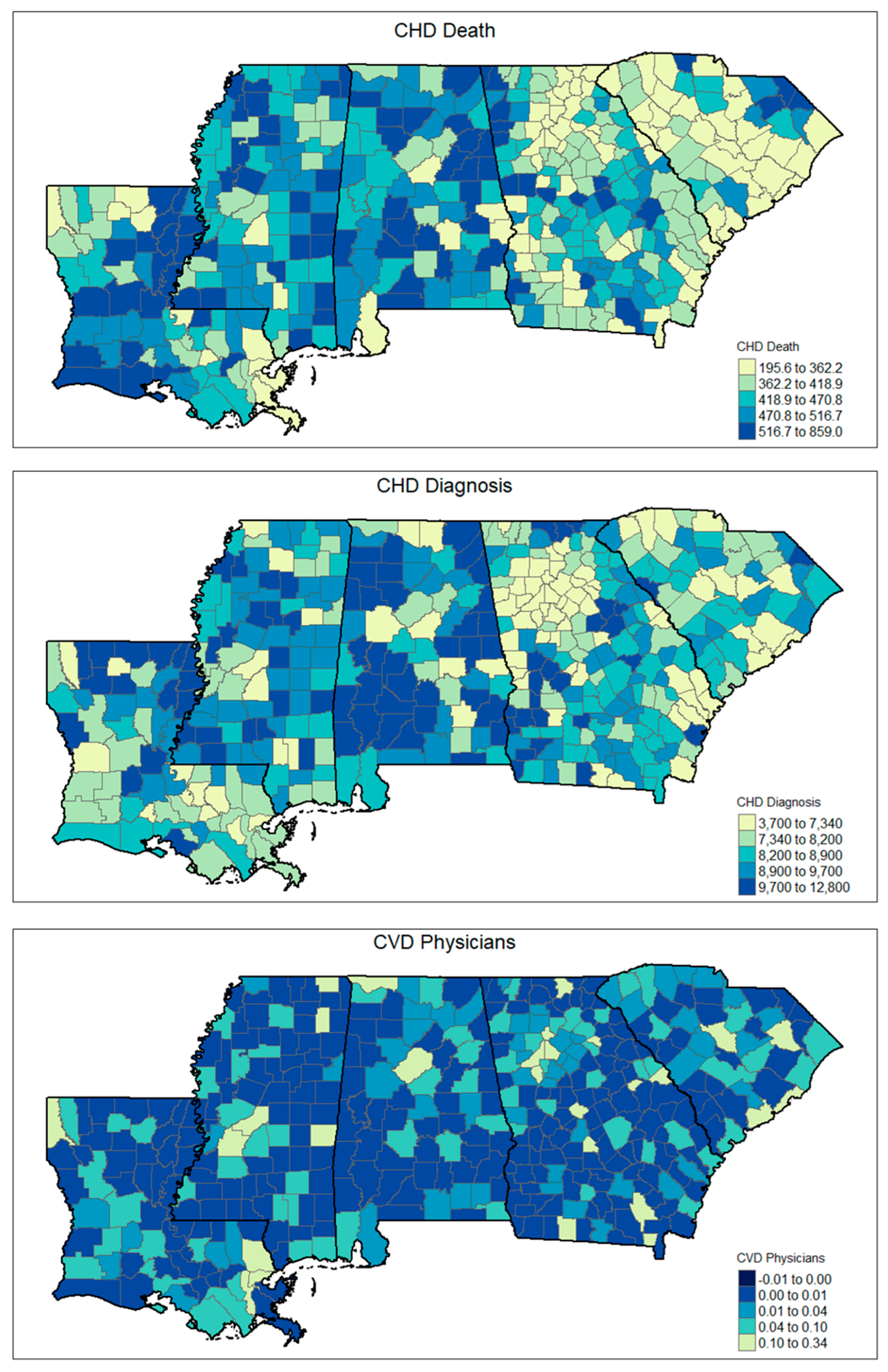
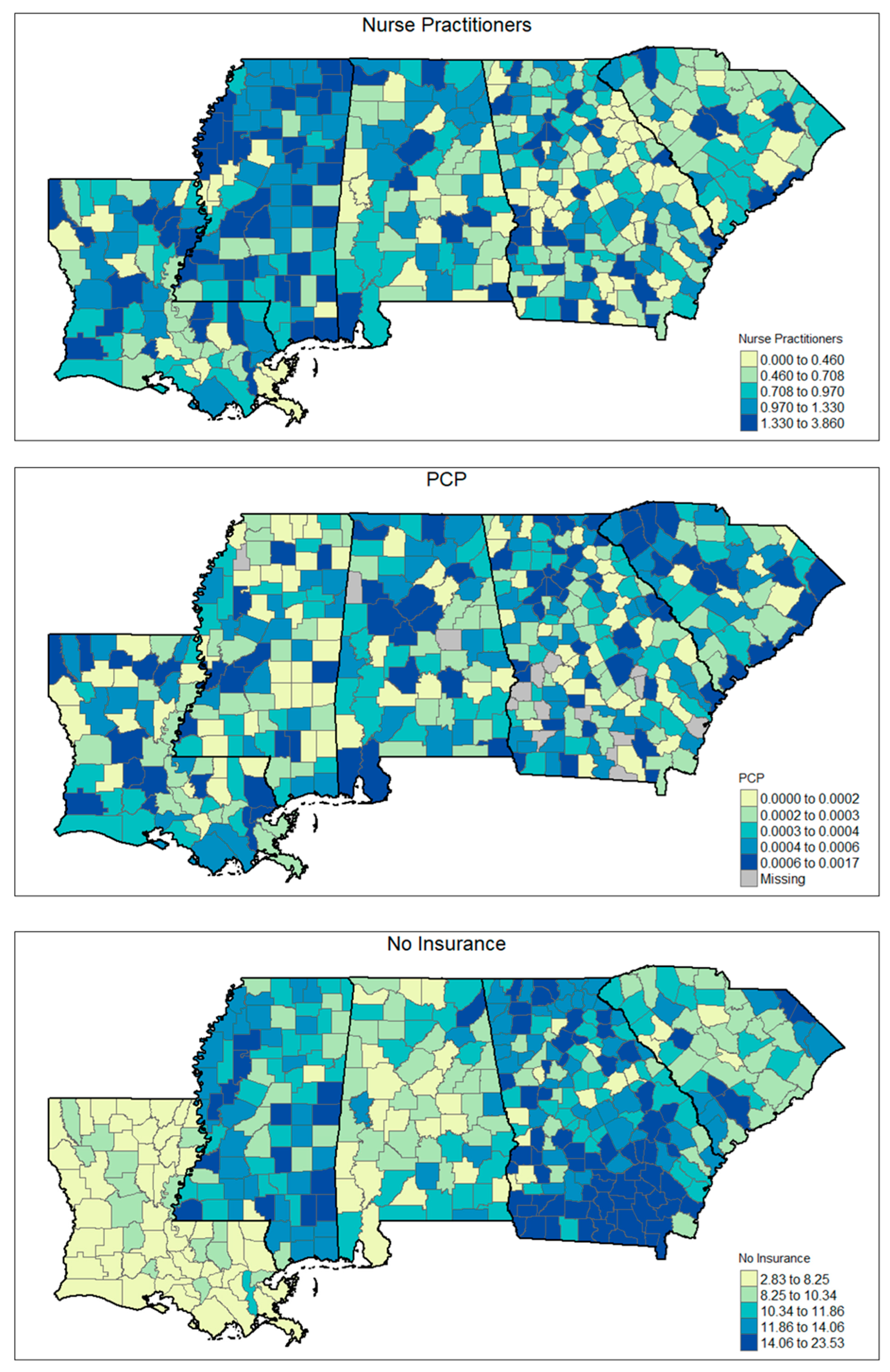
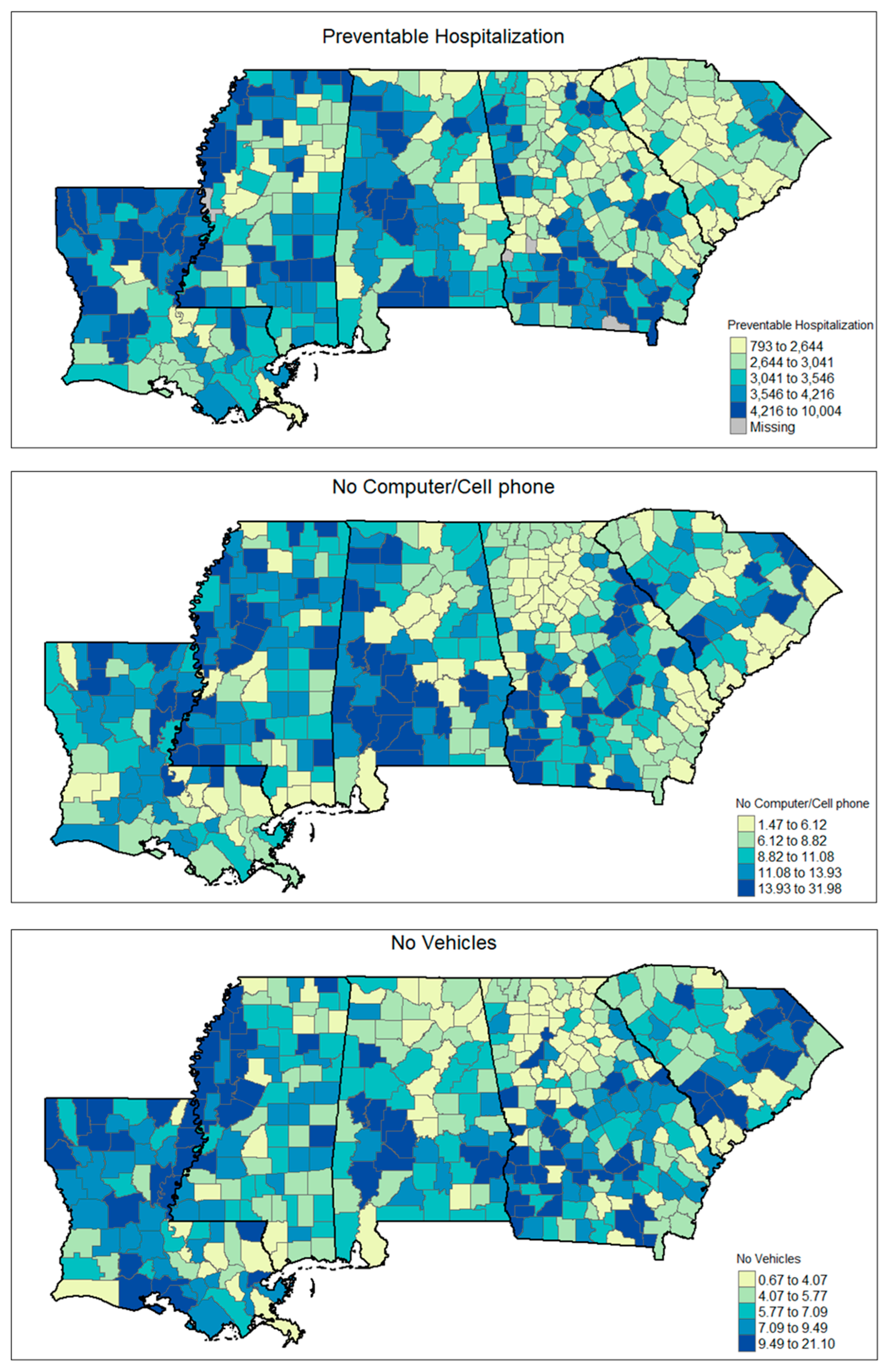
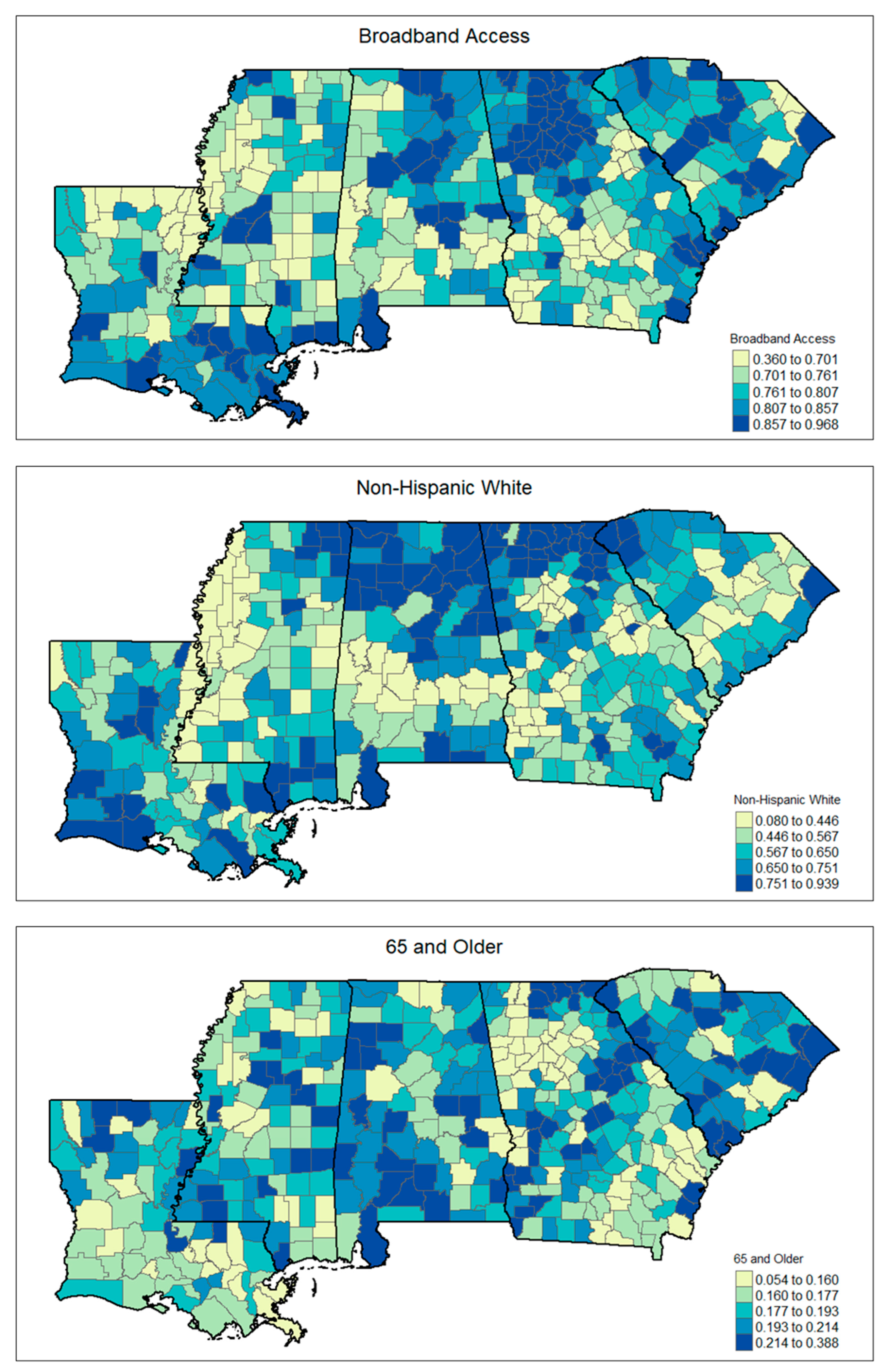
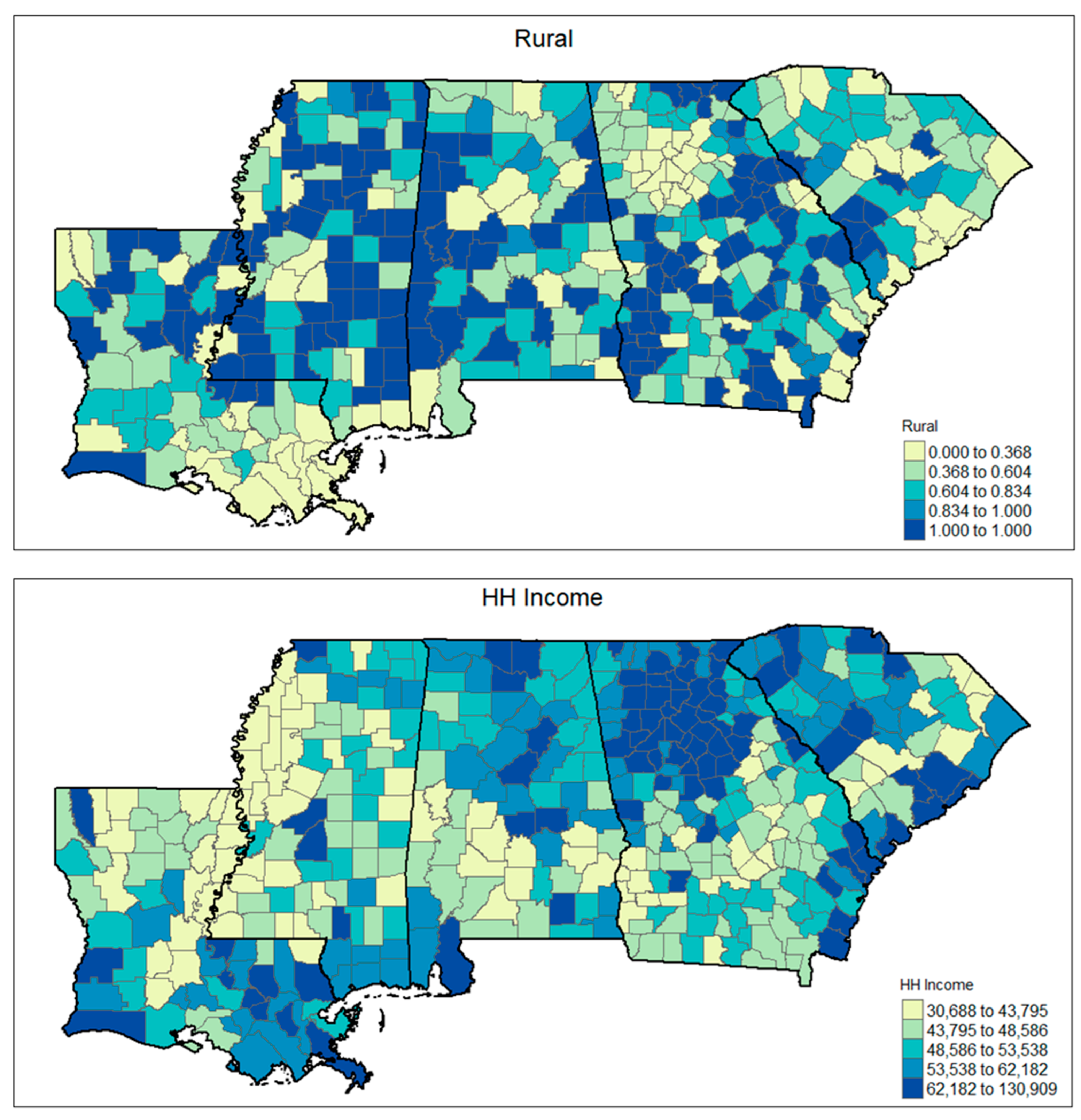
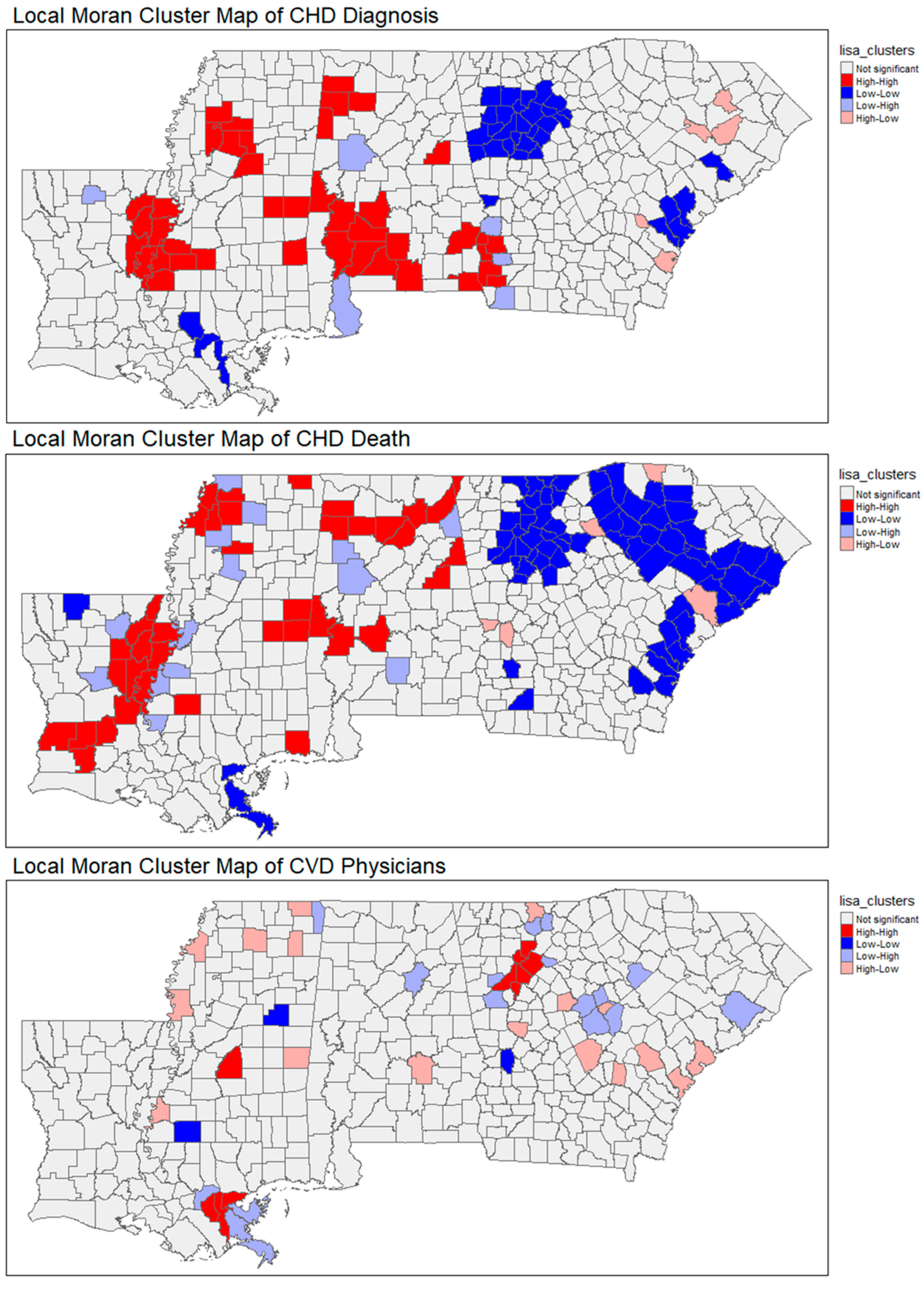
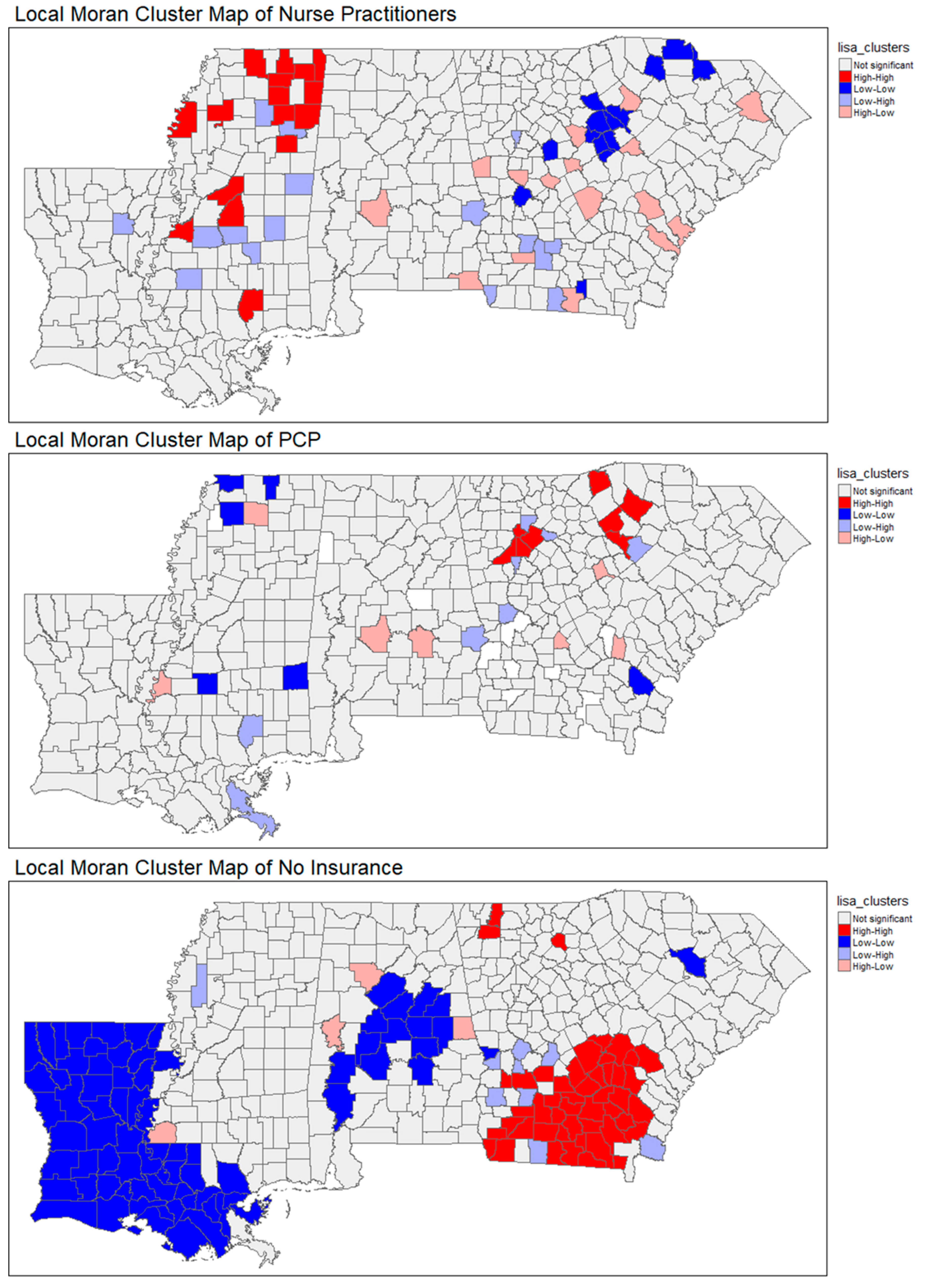
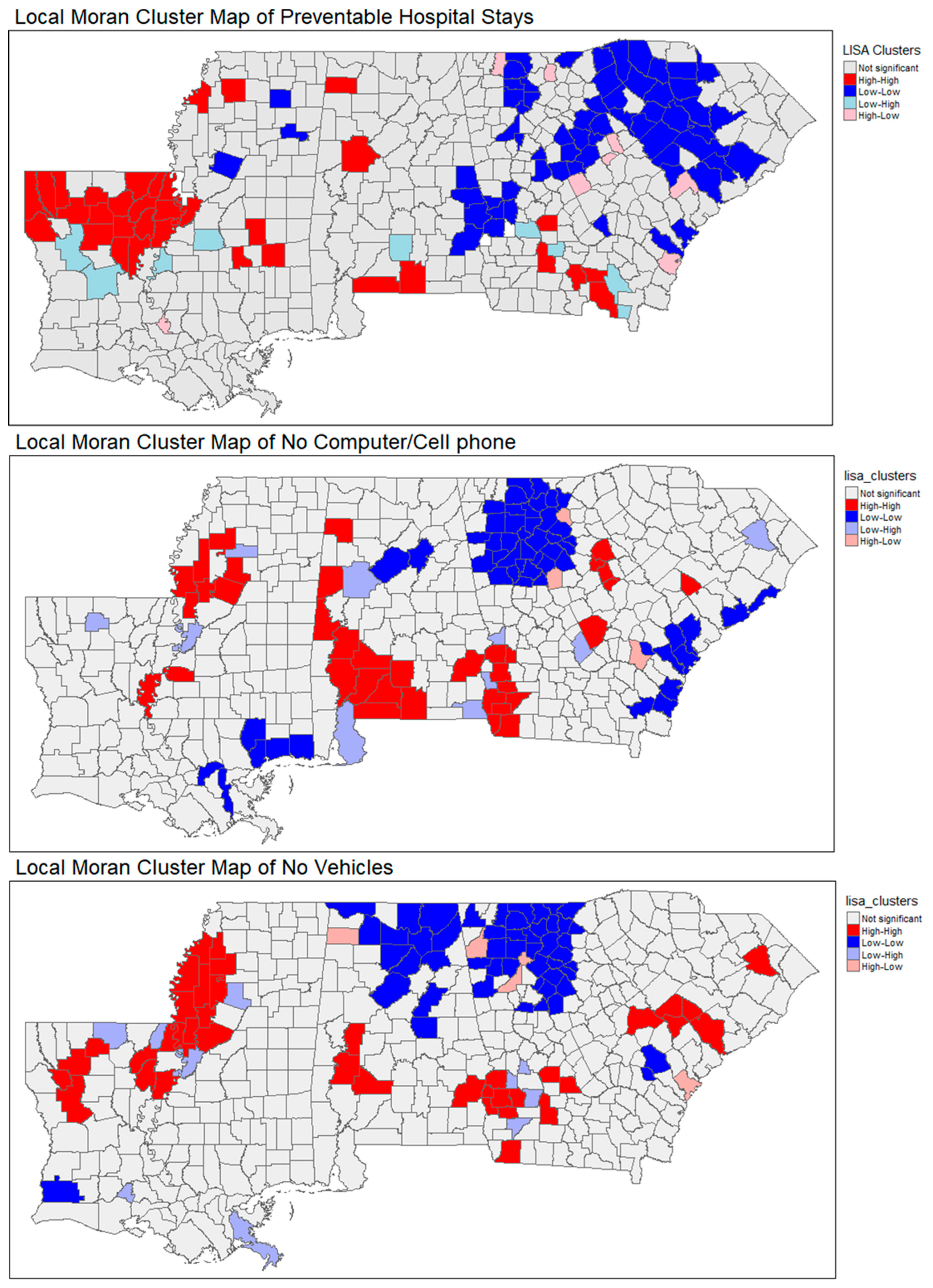
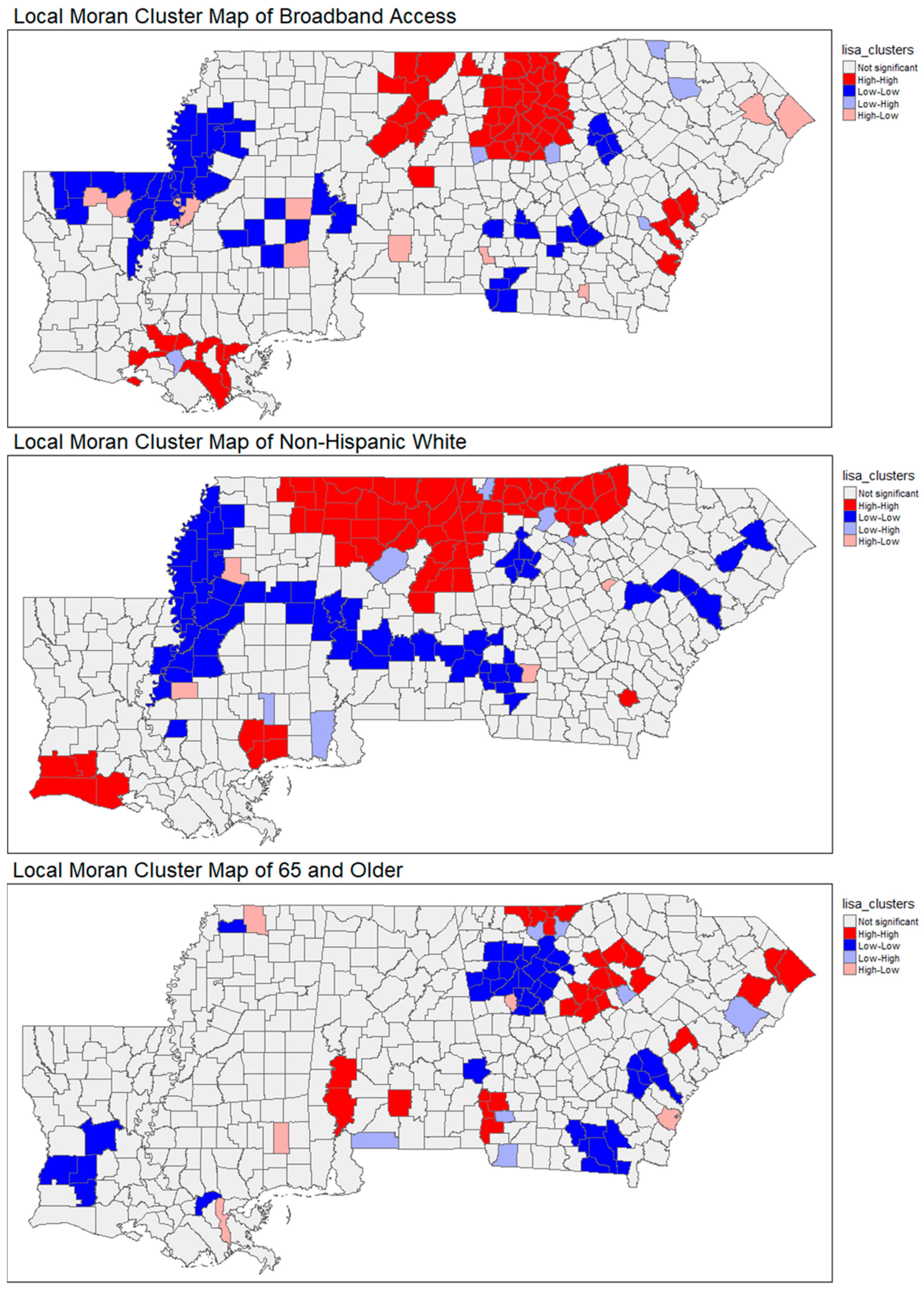
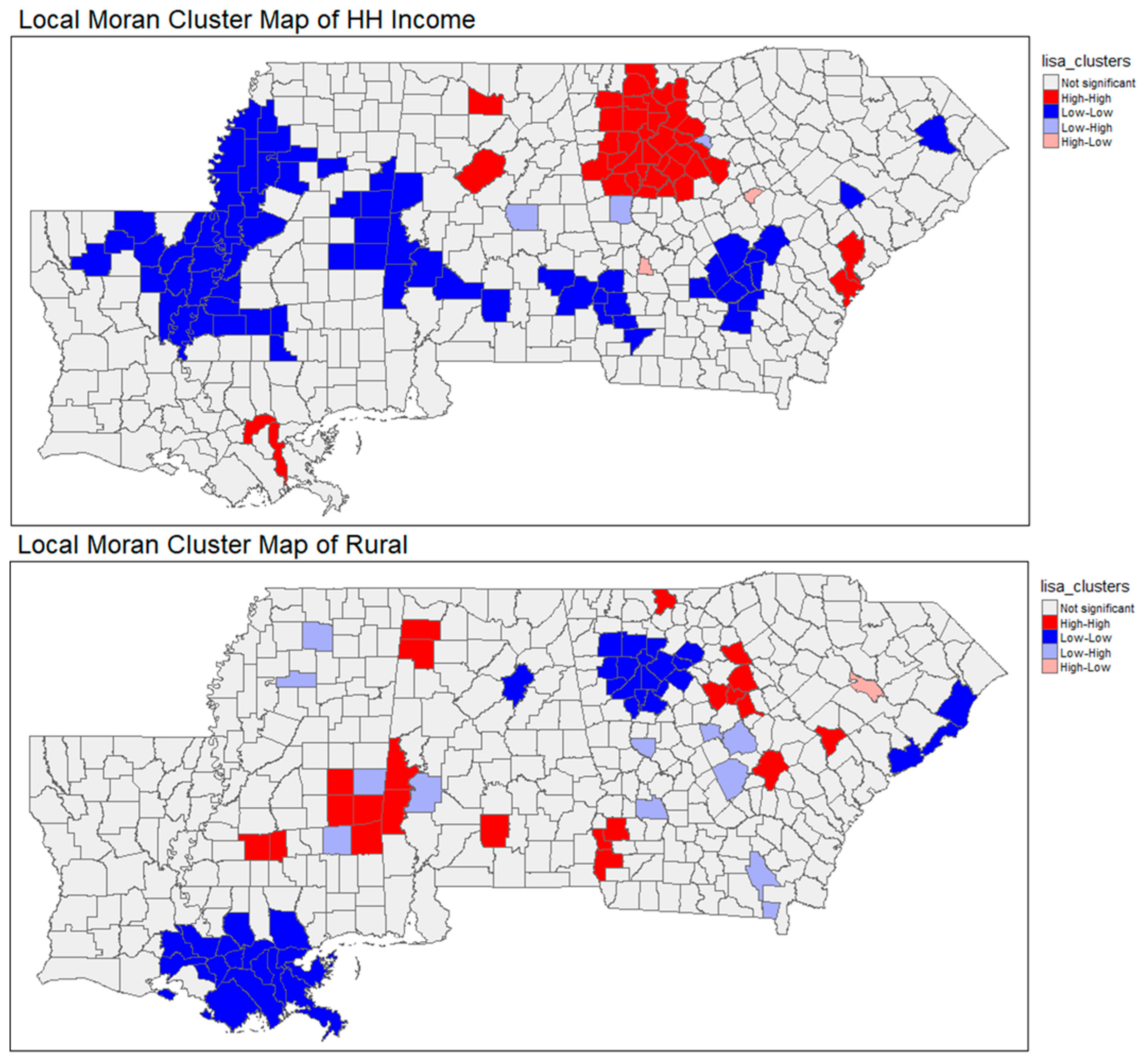
3.1. Spatial Patterns
3.2. Multivariable Regression Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Heart Disease Facts. 2024. Available online: https://www.cdc.gov/heart-disease/data-research/facts-stats/index.html (accessed on 23 May 2025).
- Mendy, V.L.; Rowell-Cunsolo, T.; Bellerose, M.; Vargas, R.; Enkhmaa, B.; Zhang, L. Cardiovascular Disease Mortality in Mississippi, 2000–2018. Prev. Chronic Dis. 2022, 19, E09. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.E.; Vasan, R.S. The southern rural health and mortality penalty: A review of regional health inequities in the United States. Soc. Sci. Med. 2021, 268, 113443. [Google Scholar] [CrossRef] [PubMed]
- Harrington, R.A.; Califf, R.M.; Balamurugan, A.; Brown, N.; Benjamin, R.M.; Braund, W.E.; Hipp, J.; Konig, M.; Sanchez, E.; Joynt Maddox, K.E. Call to Action: Rural Health: A Presidential Advisory from the American Heart Association and American Stroke Association. Circulation 2020, 141, e615–e644. [Google Scholar] [CrossRef]
- Troy, A.L.; Xu, J.; Wadhera, R.K. Access to Care and Cardiovascular Health in US Counties with Low Versus Higher Broadband Internet Availability. Am. J. Cardiol. 2023, 209, 190–192. [Google Scholar] [CrossRef]
- Balla, S.; Gomez, S.E.; Rodriguez, F. Disparities in Cardiovascular Care and Outcomes for Women from Racial/Ethnic Minority Backgrounds. Curr. Treat. Options Cardiovasc. Med. 2020, 22, 75. [Google Scholar] [CrossRef]
- Henning-Smith, C.; Tuttle, M.; Kozhimannil, K.B. Unequal Distribution of COVID-19 Risk Among Rural Residents by Race and Ethnicity. J. Rural Health 2021, 37, 224–226. [Google Scholar] [CrossRef] [PubMed]
- Rocque, G.B.; Henderson, N.L.; Hildreth, K.; Eltoum, N.; Whitlow, O.; Herring, L.; Ingram, S.; Chu, D.I.; Shao, C.C.; Hardy, C.; et al. Exploration of digital health literacy among community members and healthcare teams in the deep south: A quasi-experimental study. Digit. Health 2025, 11, 20552076251325581. [Google Scholar] [CrossRef]
- Pantalone, D.W.; Scanlon, M.L.; Brown, S.M.; Radhakrishnan, B.; Sprague, C. Unmet Mental Health and Social Service Needs of Formerly Incarcerated Women Living with HIV in the Deep South. J. Assoc. Nurses AIDS Care 2018, 29, 712–727. [Google Scholar] [CrossRef]
- Wills, M.J.; Whitman, M.V.; English, T.M. Travel Distance to Cancer Treatment Facilities in the Deep South. J. Healthc. Manag. 2017, 62, 30–43. [Google Scholar] [CrossRef]
- Johnson, K.A.; Binion, S.; Waller, B.; Sutton, A.; Wilkes, S.; Payne-Foster, P.; Carlson, C. Left behind in the U.S.’ Deep South: Addressing critical gaps in HIV and intimate partner violence prevention efforts targeting Black women. Front. Reprod. Health 2022, 4, 1008788. [Google Scholar] [CrossRef]
- Williams, G.R.; Al-Obaidi, M.; Harmon, C.; Dai, C.; Outlaw, D.; Gbolahan, O.; Khushman, M.d.; Nyrop, K.A.; Gilmore, N.; Bhatia, S.; et al. Racial disparities in frailty and geriatric assessment impairments in older adults with cancer in the Deep South: Results from the CARE Registry. Cancer 2022, 128, 2313–2319. [Google Scholar] [CrossRef]
- Allison, K.D.; Chaney, C.D.; Tillis, C.M. Racism and Inequality in the Deep South: The Health and Sociocultural Correlates of HIV/AIDS Among African Americans and the Legacy of Slavery. In Handbook of Racism, Xenophobia, and Populism: All Forms of Discrimination in the United States and Around the Globe; Akande, A., Ed.; Springer International Publishing: Cham, Switzerland, 2022; pp. 663–686. [Google Scholar]
- Pope, C.N.; Stavrinos, D.; Fazeli, P.L.; Vance, D.E. Transportation Barriers and Health-Related Quality of Life in a Sample of Middle-Aged and Older Adults Living with HIV in the Deep South. AIDS Behav. 2022, 26, 2148–2158. [Google Scholar] [CrossRef]
- Alzheimer’s Association. 2016 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2016, 12, 459–509. [Google Scholar] [CrossRef]
- Wolfe, M.K.; McDonald, N.C.; Holmes, G.M. Transportation Barriers to Health Care in the United States: Findings from the National Health Interview Survey, 1997–2017. Am. J. Public Health 2020, 110, 815–822. [Google Scholar] [CrossRef]
- Syed, S.T.; Gerber, B.S.; Sharp, L.K. Traveling towards disease: Transportation barriers to health care access. J. Community Health 2013, 38, 976–993. [Google Scholar] [CrossRef]
- Kaufman, B.G.; Thomas, S.R.; Randolph, R.K.; Perry, J.R.; Thompson, K.W.; Holmes, G.M.; Pink, G.H. The Rising Rate of Rural Hospital Closures. J. Rural Health 2016, 32, 35–43. [Google Scholar] [CrossRef]
- National Digital Inclusion Alliance. Get Started. NDIA Definitions. Available online: https://www.digitalinclusion.org/definitions/ (accessed on 23 May 2025).
- Benda, N.C.; Veinot, T.C.; Sieck, C.J.; Ancker, J.S. Broadband Internet Access Is a Social Determinant of Health! Am. J. Public Health 2020, 110, 1123–1125. [Google Scholar] [CrossRef]
- Whitacre, B.E.; Wheeler, D.; Landgraf, C. What Can the National Broadband Map Tell Us About the Health Care Connectivity Gap? J. Rural Health 2017, 33, 284–289. [Google Scholar] [CrossRef]
- U.S. Federal Communications Commission. Internet Access Services: Status as of June 30, 2023. 2024. Available online: https://docs.fcc.gov/public/attachments/DOC-405487A1.pdf (accessed on 23 May 2025).
- Kruse, C.S.; Krowski, N.; Rodriguez, B.; Tran, L.; Vela, J.; Brooks, M. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 2017, 7, e016242. [Google Scholar] [CrossRef]
- Gajarawala, S.N.; Pelkowski, J.N. Telehealth Benefits and Barriers. J. Nurse Pract. 2021, 17, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, E.A.; Schwamm, L.H.; Adeoye, O.M.; Alabi, O.; Jahangir, E.; Misra, S.; Still, C.H.; on behalf of the American Heart Association Council on Cardiovascular Radiology and Intervention, Council on Hypertension, Council on the Kidney in Cardiovascular Disease, and Stroke Council. An Overview of Telehealth in the Management of Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2022, 146, e558–e568. [Google Scholar] [CrossRef]
- Kuan, P.X.; Chan, W.K.; Fern Ying, D.K.; Rahman, M.A.A.; Peariasamy, K.M.; Lai, N.M.; Mills, N.L.; Anand, A. Efficacy of telemedicine for the management of cardiovascular disease: A systematic review and meta-analysis. Lancet Digit. Health 2022, 4, e676–e691. [Google Scholar] [CrossRef]
- Jackson, T.N.; Sreedhara, M.; Bostic, M.; Spafford, M.; Popat, S.; Lowe Beasley, K.; Jordan, J.; Ahn, R. Telehealth Use to Address Cardiovascular Disease and Hypertension in the United States: A Systematic Review and Meta-Analysis, 2011–2021. Telemed. Rep. 2023, 4, 67–86. [Google Scholar] [CrossRef] [PubMed]
- Emadi, F.; Dabliz, R.; Moles, R.; Carter, S.; Chen, J.; Grover, C.; Angley, M.; Elliott, R.A.; Criddle, D.; Rigby, D.; et al. Medication-focused telehealth interventions to reduce the hospital readmission rate: A systematic review. J. Pharm. Policy Pract. 2025, 18, 2457411. [Google Scholar] [CrossRef]
- Pandit, A.A.; Mahashabde, R.V.; Brown, C.C.; Acharya, M.; Shoults, C.C.; Eswaran, H.; Hayes, C.J. Association between broadband capacity and telehealth utilization among Medicare Fee-for-service beneficiaries during the COVID-19 pandemic. J. Telemed. Telecare 2025, 31, 41–48. [Google Scholar] [CrossRef]
- Bhaskar, S.; Bradley, S.; Chattu, V.K.; Adisesh, A.; Nurtazina, A.; Kyrykbayeva, S.; Sakhamuri, S.; Moguilner, S.; Pandya, S.; Schroeder, S.; et al. Telemedicine as the New Outpatient Clinic Gone Digital: Position Paper from the Pandemic Health System REsilience PROGRAM (REPROGRAM) International Consortium (Part 2). Front. Public Health 2020, 8, 410. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Li, X. Editorial: Aging and chronic disease: Public health challenge and education reform. Front. Public Health 2023, 11, 1175898. [Google Scholar] [CrossRef]
- Williams, D.R.; Rucker, T.D. Understanding and addressing racial disparities in health care. Health Care Financ. Rev. 2000, 21, 75–90. [Google Scholar]
- Banaji, M.R.; Fiske, S.T.; Massey, D.S. Systemic racism: Individuals and interactions, institutions and society. Cogn. Res. Princ. Implic. 2021, 6, 82. [Google Scholar] [CrossRef] [PubMed]
- Turkman, Y.E.; Williams, C.P.; Jackson, B.E.; Dionne-Odom, J.N.; Taylor, R.; Ejem, D.; Kvale, E.; Pisu, M.; Bakitas, M.; Rocque, G.B. Disparities in Hospice Utilization for Older Cancer Patients Living in the Deep South. J. Pain Symptom Manag. 2019, 58, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Zhang, J.; Li, Z.; Sun, X.; Ning, H.; Yang, X.; Weissman, S.; Olatosi, B.; Li, X. Residential Segregation and County-Level COVID-19 Booster Coverage in the Deep South: Surveillance Report and Ecological Study. JMIR Public Health Surveill. 2023, 9, e44257. [Google Scholar] [CrossRef]
- PolicyMap. Available online: https://www.policymap.com/ (accessed on 23 May 2025).
- Centers for Disease Control and Prevention. Interactive Atlas of Heart Disease and Stroke. Available online: https://nccd.cdc.gov/dhdspatlas/reports.aspx (accessed on 23 May 2025).
- United States Census Bureau. QuickFacts: United States. QuickFacts Provides Statistics for All States and Counties. Also for Cities and Towns with a Population of 5000 or More. Available online: https://www.census.gov/quickfacts/fact/table/US/EDU685223 (accessed on 23 May 2025).
- Anselin, L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Huda, N.M.; Imro’ah, N. COVID-19 case modeling in Java Island using a spatial model, GSTAR(1;1), with modified spatial weights: Queen contiguity weight matrix. AIP Conf. Proc. 2024, 2891, 090009. [Google Scholar]
- Oseran, A.S.; Sun, T.; Wadhera, R.K. Health Care Access and Management of Cardiovascular Risk Factors Among Working-Age Adults with Low Income by State Medicaid Expansion Status. JAMA Cardiol. 2022, 7, 708–714. [Google Scholar] [CrossRef]
- Stewart, J.; Addy, K.; Campbell, S.; Wilkinson, P. Primary prevention of cardiovascular disease: Updated review of contemporary guidance and literature. JRSM Cardiovasc. Dis. 2020, 9, 2048004020949326. [Google Scholar] [CrossRef]
- Loftus, J.; Allen, E.M.; Call, K.T.; Everson-Rose, S.A. Rural-Urban Differences in Access to Preventive Health Care Among Publicly Insured Minnesotans. J. Rural Health 2018, 34 (Suppl. 1), s48–s55. [Google Scholar] [CrossRef]
- Dennis, S.; Williams, A.; Taggart, J.; Newall, A.; Denney-Wilson, E.; Zwar, N.; Shortus, T.; Harris, M.F. Which providers can bridge the health literacy gap in lifestyle risk factor modification education: A systematic review and narrative synthesis. BMC Fam. Pract. 2012, 13, 44. [Google Scholar] [CrossRef]
- Keesara, S.; Jonas, A.; Schulman, K. COVID-19 and Health Care’s Digital Revolution. N. Engl. J. Med. 2020, 382, e82. [Google Scholar] [CrossRef]
- Piantadosi, S.; Byar, D.P.; Green, S.B. The ecological fallacy. Am. J. Epidemiol. 1988, 127, 893–904. [Google Scholar] [CrossRef]
| Variable | Description | Role | Variable Type | Source |
|---|---|---|---|---|
| Heart Disease Prevalence | Coronary Heart Disease Prevalence by County, 2022, as of 2022 in Deep South. | Outcome | Continuous | PolicyMap [37] |
| Heart Disease Mortality | Coronary Heart Disease mortality by County, 2022, as of 2022 in Deep South. | Outcome | Continuous | Centers for Disease Control and Prevention (CDC) [38] |
| Cardiologist | Cardiovascular Disease Physicians per 1000 People by County, 2020, as of 2021 in Deep South. | Covariate | Continuous | PolicyMap [37] |
| Nurse Practitioner | Nurse Practitioners per 1000 People by County, 2020, as of 2022 in Deep South. | Covariate | Continuous | PolicyMap [37] |
| PCP | Percentage of Adults Reporting to Have a Personal Doctor or Healthcare Provider by County, 2010, as of 2018 in Deep South | Covariate | Continuous | PolicyMap [37] |
| Uninsured population | Estimated percentage of all people without health insurance, between 2019 and 2023. | Covariate | Continuous | United States Census Bureau [39] |
| Houses with no vehicles | Estimated percentage of housing units for which no vehicles are available in 2019–2023. | Covariate | Continuous | United States Census Bureau [39] |
| HH without any type of computer | Estimated percentage of households without any type of computer, between 2019 and 2023. | Covariate | Continuous | United States Census Bureau [39] |
| Broadband access | Percentage of households with broadband internet connection. The 2025 Annual Data Release used data from 2019 to 2023 for this measure. | Covariate | Continuous | United States Census Bureau [39] |
| % White | Percentage of Non-Hispanic White Population by County, 2022, as of 2018–2022 in Deep South. | Covariate | Continuous | United States Census Bureau [39] |
| % Rural | The percentage of population living in a census-defined rural area, 2020. | Covariate | Continuous | United States Census Bureau [39] |
| HH Income | Median household income, 2023. | Covariate | Continuous | United States Census Bureau [39] |
| % 65 and Older | Percent of all people 65 or older, between 2019 and 2023. | Covariate | Continuous | United States Census Bureau [39] |
| Variable | Mean | Standard Deviation | Units |
|---|---|---|---|
| Heart Disease Prevalence | 8517 | 1450.30 | Per 100,000 population |
| Heart Disease Mortality | 446.95 | 98.70 | Per 100,000 population |
| Cardiologist | 0.02 | 0.01 | Per 1000 population |
| Nurse Practitioner | 0.95 | 0.61 | Per 1000 population |
| PCP | 0.04% | 0.03% | Percent (%) |
| Uninsured Population | 14.19% | 3.39% | Percent (%) |
| Houses with No Vehicles | 6.91% | 3.27% | Percent (%) |
| HH Without Any Type of Computer | 10.31% | 4.78% | Percent (%) |
| Broadband Access | 77.44% | 9.33% | Percent (%) |
| % White | 59.41% | 17.88% | Percent (%) |
| % Rural | 67.84% | 31.20% | Percent (%) |
| HH Income | $54,114 | $14,039 | USD (Median Household Income) |
| % 65 and Older | 18.92% | 3.92% | Percent (%) |
| 95% CI | |||||
|---|---|---|---|---|---|
| B | Lower Limit | Upper Limit | p Value | VIF | |
| (Intercept) | 430.20 ** | 243.55 | 616.83 | 0.000 | |
| Cardiovascular Disease Physicians | −190.60 | −440.34 | 59.09 | 0.134 | 1.86436 |
| Nurse Practitioners | −32.76 | −16.00 | 49.51 | 0.49 | 2.3033 |
| Primary Care Physicians | −54,430.00 * | −98,353.63 | −10,501.61 | 0.015 | 1.24876 |
| No Insurance | 2.78 | −5.14 | −0.41 | 0.21 | 2.38506 |
| Preventable Hospital Stays | 0.02 ** | 0.01 | 0.03 | 0.000 | 1.70738 |
| Households without Computer/Cell phone | 4.48 * | 0.93 | 8.02 | 0.013 | 3.1081 |
| Housing with No Vehicles | 2.60 | −1.15 | 6.34 | 0.173 | 1.7547 |
| Broadband Access | 61.22 | −105.20 | 227.65 | 0.470 | 1.09798 |
| % Non-Hispanic White | 127.70 | −71.48 | 183.85 | 0.100 | 3.41786 |
| % 65 and Older raw value | 373.90 ** | 628.72 | 119.13 | 0.004 | 3.79143 |
| Median Household Income | −0.003 ** | −0.001 | −0.005 | 0.000 | 1.59585 |
| % Rural | −0.10 | −42.34 | 42.14 | 0.996 | 2.92088 |
| 95% CI | |||||
|---|---|---|---|---|---|
| B | Lower Limit | Upper Limit | p Value | VIF | |
| (Intercept) | 5725.00 * | 4212.35 | 7237.34 | 0.0001 | |
| Cardiovascular Disease Physicians | −1059.00 | −3082.23 | 965.07 | 0.304 | 1.86436 |
| Nurse Practitioners | 99.47 | −36.31 | 235.24 | 0.151 | 2.3033 |
| Primary Care Physicians | −421,700.00 * | −77,7671.30 | −65,729.06 | 0.020 | 1.24876 |
| No Insurance | −3.53 | −22.69 | 15.65 | 0.718 | 2.38506 |
| Preventable Hospital Stays | 0.13 * | 0.06 | 0.19 | 0.000 | 1.70738 |
| Households without Computer/Cell phone | 39.33 * | 10.61 | 68.06 | 0.007 | 3.1081 |
| Housing with No Vehicles | 33.88 * | 3.53 | 64.22 | 0.029 | 1.7547 |
| Broadband Access | −912.60 | −2261.32 | 436.09 | 0.184 | 1.09798 |
| % Non-Hispanic White | 833.80 * | 378.53 | 1289.12 | 0.0001 | 3.41786 |
| % 65 and Older raw value | 17,980.00 * | 15,918.07 | 20,047.71 | 0.0001 | 3.79143 |
| Median Household Income | −0.03 * | −0.04 | −0.02 | 0.0001 | 1.59585 |
| % Rural | 476.90 * | 134.59 | 819.20 | 0.006 | 2.92088 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Juboori, R.; Barker, D.; Yockey, A.; Swindell, E.; Morgan, R.; Agarwala, N. Telehealth-Readiness, Healthcare Access, and Cardiovascular Health in the Deep South: A Spatial Perspective. Int. J. Environ. Res. Public Health 2025, 22, 1020. https://doi.org/10.3390/ijerph22071020
Al Juboori R, Barker D, Yockey A, Swindell E, Morgan R, Agarwala N. Telehealth-Readiness, Healthcare Access, and Cardiovascular Health in the Deep South: A Spatial Perspective. International Journal of Environmental Research and Public Health. 2025; 22(7):1020. https://doi.org/10.3390/ijerph22071020
Chicago/Turabian StyleAl Juboori, Ruaa, Dylan Barker, Andrew Yockey, Elizabeth Swindell, Riley Morgan, and Neva Agarwala. 2025. "Telehealth-Readiness, Healthcare Access, and Cardiovascular Health in the Deep South: A Spatial Perspective" International Journal of Environmental Research and Public Health 22, no. 7: 1020. https://doi.org/10.3390/ijerph22071020
APA StyleAl Juboori, R., Barker, D., Yockey, A., Swindell, E., Morgan, R., & Agarwala, N. (2025). Telehealth-Readiness, Healthcare Access, and Cardiovascular Health in the Deep South: A Spatial Perspective. International Journal of Environmental Research and Public Health, 22(7), 1020. https://doi.org/10.3390/ijerph22071020







