Abstract
Background: Breast cancer is one of the most prevalent neoplasms among women, often requiring mastectomy, a procedure with a significant impact on functionality, self-esteem, and quality of life. Objective: This study aimed to map the main interventions performed by the Rehabilitation Nursing Specialist in the follow-up care of mastectomised women. Methods: A review was conducted according to the Joanna Briggs Institute methodology. The search included 11 articles published between 2019 and 2024 in Portuguese, English, and Spanish, available on the EBSCO platform (MEDLINE with Full TEXT, CINAHL). The descriptors used were (Mastectomy OR Breast Removal) AND (Rehabilitation Nursing OR Nursing Intervention). Results: The Rehabilitation Nursing Specialist interventions focused on education regarding upper limb mobilisation, medication administration, lymphedema prevention, strategies for performing Daily Life Activities with less effort and pain, implementation of rehabilitation plans with physical exercises, and emotional support in accepting body image changes. Hospital discharge planning and caregiver education also emerged as key elements to ensure continuity of care. Most studies (six) identify performing exercises to strengthen muscles and prevent lymphoedema as a very important intervention for nurses, followed by education on care for upper limb mobilisation and lymphoedema prevention (five) and emotional and social support (four), among other interventions. Conclusions: The Rehabilitation Nursing Specialist interventions are fundamental for promoting functionality, emotional well-being, and quality of life in mastectomised women, reinforcing the importance of a multidisciplinary, person-centred approach supported by scientific evidence.
1. Introduction
Breast cancer is the most common malignant neoplasm among women worldwide and represents one of the leading causes of cancer death in the female population. According to the World Health Organisation (WHO) [1], over 2.3 million new cases of breast cancer were diagnosed in 2020, resulting in approximately 685,000 deaths globally. This disease represents a significant public health problem with substantial physical, emotional, and social implications.
In Portugal, breast cancer accounts for approximately 30% of all cancer cases in women [2]. Mastectomy involves the removal of the breast, usually associated with axillary dissection [2], and is the most common method used in breast cancer treatment [3]. The breast is a gland composed of various structures, including lymphatic vessels. The surgery may be performed to remove the tumour, screen for axillary lymph node invasion, or alleviate symptoms in advanced-stage disease [4].
As a consequence of this surgical procedure, women develop alterations in self-image and self-esteem, as well as fear regarding these bodily changes and the impact they may have on their social and professional lives [5]. Rehabilitation nursing can significantly improve health-related quality of life for patients with chronic diseases by addressing complex care needs and improving patient coping strategies, ultimately leading to better management of chronic conditions and improved patient outcomes [6,7].
Rehabilitation nurses play a crucial role in healthcare organisations, requiring a diverse set of skills to effectively support patients. The changing healthcare landscape emphasises not only technical proficiency but also cultural competence, effective communication, and interprofessional collaboration. Culturally competent Rehabilitation Nurses should possess skills, knowledge, and attitudes that enhance understanding of patients‘ values, awareness of personal biases, and the ability to tailor care to patients’ expectations and preferences, ensuring effective and respectful healthcare delivery [8].
Rehabilitation nurses must have skills in effective communication, interprofessional collaboration, the use of supportive technology, providing patient- and family-centred care and promoting self-management, which includes evidence-based practice, collaboration in interprofessional teams, and proficiency in assessing and improving the quality of care, all aimed at improving patients’ quality of life [9,10]. These competencies are essential for promoting safe and effective transitions of care in various healthcare settings and improving patient outcomes [9,11].
Functional re-education is a standard of quality care defined by the Order of Portuguese Nurses (https://www.ordemenfermeiros.pt/, accessed on: 1 March 2025), as well as one of the quality standards for specialised care in rehabilitation nursing. Therefore, the Rehabilitation Nurse, together with the care recipient, should develop functional re-education processes aimed at self-care, quality of life, reintegration, and societal participation [12,13]. Upper limb rehabilitation nursing programmes positively impact quality of life in post-mastectomy breast cancer patients, improving functioning and symptoms [14,15], as well as improving quality of life [16].
There are not many studies that more clearly identify the role of Rehabilitation Nurses in training mastectomised women in self-care. Our study aims to address this gap.
The aim of this study was to map the main interventions carried out by the Rehabilitation Nurse Specialist in the follow-up of mastectomised women.
This systematic literature review is registered on the PROSPERO platform under registration number CRD420250652280.
2. Methodology
2.1. Study Design
The proposed review was conducted according to the updated methodology of the Joanna Briggs Institute (JBI) [17] and consisted of the following steps:
2.1.1. Research
Research in MEDLINE with Full TEXT and CINAHL databases.
2.1.2. Research Question
The question guiding this review was, “What are the interventions of the Rehabilitation Nurse in empowering mastectomised women for self-care?”.
2.1.3. Strategy PCC
The PCC strategy from the Joanna Briggs Institute [17] was used, where the following applies:
- Population (P): Mastectomised women;
- Concept (C): Interventions of the Rehabilitation Nurse;
- Context (C): Empowerment for self-care.
2.1.4. Inclusion Criteria
Only studies available in full text, published in Portuguese, English, or Spanish, between 1 January 2019 and 31 December 2024, were included to obtain the recent and updated literature. This time limit was considered appropriate given the objectives of the review and the question that guided it [18]. This is because, in recent years, there has been a greater increase in the role of the Rehabilitation Nurse for a few reasons, including medical and technological advances in the surgical approach, a greater focus on quality of life and patient autonomy, and patient education and self-management where the role of the Rehabilitation Nurse has been emphasised. We also wanted to avoid reporting older or outdated practices compared to current ones.
Studies that did not fulfil the inclusion criteria were excluded. Two independent reviewers assessed the eligibility of the studies. If there was any disagreement about the inclusion and/or exclusion of a study, a third reviewer was consulted.
2.1.5. Study Types
All types of articles were considered: studies with quantitative, qualitative, and mixed methodologies, including primary studies and reviews.
2.1.6. Search Strategy
We carried out the search using the terms DeCS/MESH used as descriptors: (“Mastectomy” OR “Breast Removal”) AND (“Rehabilitation Nursing” OR “Nursing Intervention”). After the search, all identified articles were imported into the Mendeley (v2.134.0)® reference manager, and duplicates were removed.
2.1.7. Study Selection Process
According to Levac, Colquhoun, and O’Brien (2010) [19], two independent reviewers assessed the titles and abstracts based on the inclusion criteria. Selected articles were subsequently analysed in full text. In case of doubt regarding the inclusion of any article, a third reviewer was consulted.
2.1.8. Data Analysis and Extraction
The results of the different stages of the selection process were organised according to the PRISMA Flow Diagram model [20]. Data extraction from each article was performed using a grid that included the following parameters: author, year of publication, country of origin, study type, study location, objectives, methodology, population/number of participants, definition of Rehabilitation Nurse, definition of mastectomy, main interventions, main results, and conclusions.
2.1.9. Data Synthesis and Evaluating the Quality of Studies
The review presented a set of interventions by the Rehabilitation Nursing Specialist obtained through the analysis and interpretation of the included articles.
A descriptive synthesis was prepared, highlighting the most relevant interventions in the process of empowering mastectomised women for self-care, aiming to improve their quality of life. A descriptive analysis of each study was carried out using a form designed for this purpose. This form underwent a pilot test, where it was found to be a suitable tool and enabled the information to be extracted in accordance with the research question. Data extraction was carried out independently by the reviewers responsible for selecting the studies, and in the event of a disagreement, another reviewer was consulted. The data extracted contains specific details on authors, years, titles, objectives, study design, methods, results, and conclusion.
The quality assessment of the studies to be included in this review followed the critical appraisal tools of the JBI, which help assess the reliability, relevance, and results of published articles, and the checklist was completed according to the type of study [21]. Two independent reviewers assessed the studies based on the checklist criteria. In case of doubt, a third reviewer was consulted.
We chose to draw up a synthesis of all the nursing interventions that the selected studies described as appropriate, i.e., those that promote the empowerment of mastectomised women for self-care. The reader has access to all the interventions reported in the selected studies and can choose, if they wish, to implement the ones they consider most appropriate in the context of their clinical practice.
Synthesising the data in this review involved analysing and interpreting the 11 articles selected to identify the most relevant interventions carried out by the Rehabilitation Nurse Specialist in the process of empowering mastectomised women to self-care. The main aim of the synthesis was to highlight the interventions that contribute to improving the quality of life of these women.
3. Results
The search was carried out in the MEDLINE with Full TEXT and CINAHL databases, identifying 523 articles. From a total of 523 studies, 63 duplicate studies were removed, leaving 460. Of the 460 studies, 263 were excluded by reading the title, and 184 studies were excluded by reading the abstract. Of the 13 studies selected, 2 were also excluded because they did not fit the theme. The final number of studies selected was 11 (7 in Portuguese and 4 in English) (Figure 1. PRISMA flow diagram of the study selection process).
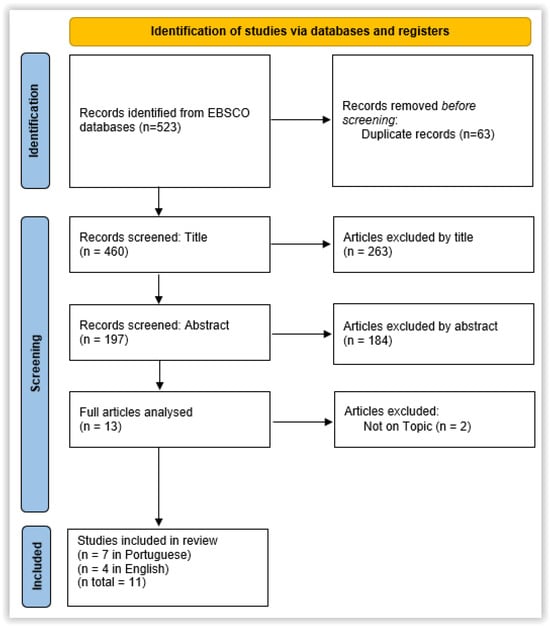
Figure 1.
PRISMA flow diagram of the study selection process.
To facilitate understanding and application of the interventions, the data were organised and presented in Table 1 (Description of included studies). This table provides an overview of each study, including references, objectives, specific interventions, and level of evidence.

Table 1.
Description of the included studies.
In terms of quality assessment, all 11 studies had a low risk of bias/high quality, i.e., the studies met most or all the methodological criteria in the respective JBI checklist depending on the type of study, and the decision was made to include them in the review [32].
The interventions were categorised based on recurring themes in the articles, such as education, promotion of functionality, prevention of complications, and psychosocial support. The synthesis sought to present all the interventions that the selected studies described as suitable for promoting self-care training for mastectomised women.
After analysing the 11 articles presented in Table 1, we were able to define common interventions such as educating the woman undergoing mastectomy, empowerment, and promoting self-care.
Promoting the woman’s functionality and autonomy is achieved by providing strategies to perform ADL with less effort and pain and adapting tasks to ensure the patient’s independence in daily life.
Recommending practices that respect the patient’s autonomy and values: We also highlight the implementation of physical exercise plans for lymphedema prevention, post-surgery, and when at home, planning the discharge with the woman undergoing the surgical procedure and her family/caregivers.
Emotional support, the implementation of strategies to promote self-image and self-confidence, and the creation of discussion groups are interventions present in the various analysed articles.
All interventions, as shown in Table 2, must always consider the individual’s uniqueness, use a multidisciplinary approach, and be applicable in all phases of the pre-operative, peri-operative, and post-operative processes.

Table 2.
Identified interventions.
4. Discussion
Mastectomy is considered the main treatment for breast cancer and brings physical and psychological changes for women, requiring a coordinated and holistic intervention by health professionals [3].
Empowerment and the promotion of self-care appear as central themes in several studies, aiming to maintain and promote functionality by finding strategies for performing daily life activities with less pain and effort [23,24,29]. Our results are in line with previous studies regarding very important dimensions in the provision of post-mastectomy care [33,34,35]. In fact, promoting self-care has numerous benefits for physical, mental, and emotional health, improving quality of life, productivity, relationships, and self-esteem. Self-care helps to reduce stress and anxiety, as well as increase resilience and well-being, which are very important for mastectomised women.
To empower the woman undergoing mastectomy, their participation in the process of preventing complications, recovery, and rehabilitation should begin immediately after surgery, addressing strategies aimed at maintaining the woman’s functionality [28].
Following surgery, there is a reduction in the range of motion of the shoulder joint, making the adaptation of tasks to ensure the woman’s independence in performing daily life activities significantly important [15,23,24,25]. It is, therefore, crucial to perform an assessment of the shoulder joint’s range of motion and the muscle strength of the affected upper limb post-mastectomy using goniometry and dynamometry, respectively [31]. In the same vein, previous studies have emphasised that assessing the range of motion of the shoulder joint, with the aim of restoring functionality as much as possible, is important for promoting self-care and autonomy [36,37,38]. We consider this aspect to be very relevant, as improving shoulder range of motion and muscle strength has a positive impact on women’s functionality and on regaining their autonomy.
Previous studies have emphasised the role of rehabilitation nursing in functional rehabilitation programmes for the shoulder joint, which not only restores function to patients but also improves their quality of life [39,40]. Rehabilitation nursing significantly improves the quality of life of post-mastectomy breast cancer patients by addressing the physical, psychological, and social consequences, promoting self-confidence, and facilitating social connections, ultimately helping with the transition to normal daily life and improving general well-being [41].
Thus, a personalised exercise plan should be developed and implemented, considering needs and preventing potential complications [22,25,30,31] through joint mobilisation, stretching, and exercises aimed at muscle strengthening [30]. Rehabilitation nursing significantly improves the quality of life of post-mastectomy breast cancer patients. One study reports that most patients reported positive influences on their daily functioning and general well-being, with 92% recognising the beneficial impact of rehabilitation on their quality of life [42].
Empowering women to perform these exercises at home should be considered an extremely important intervention by the Rehabilitation Nursing Specialist, requiring teaching and training the woman to correctly follow the developed plan [23,29]. These exercises, besides aiming to improve the range of motion and, consequently, the functionality of the affected upper limb, also aim to reduce and prevent lymphedema [29].
Lymphedema, thus, emerges as the main complication associated with mastectomy, causing changes in body image, discomfort, and reducing the independence of the mastectomised woman. It is, therefore, necessary to address strategies that minimise these effects. Previous studies have reported the advantages of training women in exercises that allow them to increase the range of motion of the shoulder joint and, thus, recover as much function as possible [43,44].
Therefore, the use of compression sleeves, performing lymphatic drainage, as well as performing and teaching exercises aimed at reducing oedema can be approaches used to minimise these consequences [15,23,31]. Detailed explanations should be provided to women about specific practices and guidelines such as mobilisation, the use of assistive devices, and methods for lymphedema control [15,23,24,25,31]. Lymphoedema greatly limits a woman’s functionality and autonomy and, consequently, interferes with self-care. Therefore, interventions to reduce or eliminate lymphoedema are very important when caring for these women.
Rehabilitation nursing programmes have led to significant improvements in physical health indicators, such as increased range of movement in the upper limbs and a reduction in lymphoedema, as well as a reduction in fatigue and an increase in functionality [16,45].
In addition, given the possible physical alterations previously mentioned resulting from mastectomy, intervening in the psychological and emotional recovery and well-being of the mastectomised woman should be considered a priority by the Rehabilitation Nursing Specialist [22], which was already recommended in previous studies [46,47].
The fear of losing her role as a woman and, if applicable, as a mother, as well as the inherent fear of dying, are frequent thoughts among these women, increasing the prevalence of anxiety in this population [24]. Therefore, reducing anxiety using relaxation methods can be equally important in maintaining the psychological well-being of these women [22].
In this sense, active listening and welcoming, encouraging self-reflection, defining strategies to aid self-image acceptance, and referring to support groups where topics such as self-acceptance, sexuality, and even the breast cancer diagnosis itself are discussed are interventions performed by the RNS aimed at improving psychological well-being and promoting body acceptance, reducing complications that could arise from them [23,24,25,28,29]. In fact, considering the changes in self-image that mastectomy causes, interventions aimed at improving psychological well-being, in addition to physical well-being, can promote the mental health of these women and prevent depressive symptoms associated with self-image and possible physical limitations.
We infer, then, that the empowerment and education of mastectomised women assume great importance in the rehabilitation process, providing adaptive strategies that promote the maintenance of functionality and self-care, preventing physical complications, and promoting a safe environment so that women can maintain the highest possible level of autonomy and independence in ADL. Figure 2 summarises the interventions carried out by rehabilitation nursing.
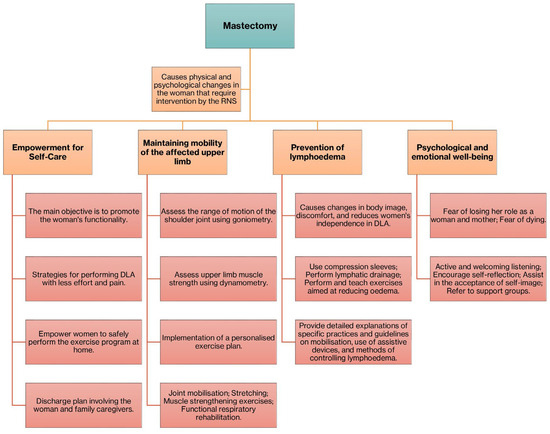
Figure 2.
Summary diagram of interventions carried out by rehabilitation nursing.
We identified some limitations. Although the included studies had good methodological quality, they did not clarify some important aspects, such as the frequency of nurses’ interventions and how long they were implemented.
The implications for clinical practice of the results and subsequent discussion of this review are as follows: Multidisciplinary and person-centred approach: It is essential that Rehabilitation Nurses work as part of a multidisciplinary team, ensuring that the care provided is individualised and adapted to the needs of each mastectomised woman. The promotion of self-care and functionality: Interventions should focus on empowering women to self-care through education on upper limb mobilisation, medication administration, and the prevention of lymphoedema. The aim is for women to perform Activities of Daily Living (ADL) with less effort and pain, promoting their independence. The implementation of physical rehabilitation plans: It is crucial to develop and implement personalised physical exercise plans for muscle strengthening and lymphoedema prevention, both post-operatively and at home. Assessment of shoulder joint range of motion and muscle strength is essential for regaining functionality. Psychosocial and emotional support: Emotional support is a key intervention to help women cope with changes in body image, acceptance of self-esteem, and a reduction in anxiety. Active listening, welcoming, and encouraging self-reflection and referral to support groups are important practices. Hospital discharge planning: The Rehabilitation Nurse should actively participate in hospital discharge planning together with the woman and her family/carers, ensuring continuity of care and education about post-operative care and warning signs. Education for family members/carers: Educating family members and carers is a key element in ensuring continuity of care and support for women in their recovery process. Use of scientific evidence: Interventions must be based on scientific evidence in accordance with the guidelines and quality standards defined by the Portuguese Order of Nurses for Rehabilitation Nursing. Intervention at all stages of the process: Interventions should be applied at all stages of the pre-operative, peri-operative, and post-operative processes, with a view to early rehabilitation and effective management of suffering.
5. Study Limitations
This review only included studies in English, Portuguese, and Spanish, so linguistic bias may have affected the comprehensiveness of our review. Likewise, only studies from 2019 to 2024 were included, so the results may be limited by the time frame; in other words, this time frame may have limited the scope of the evidence.
6. Conclusions
The Rehabilitation Nurse Specialist plays a decisive role in empowering mastectomised women, promoting self-care, and contributing to a full recovery, thus increasing quality of life.
It is concluded that the nurse is a fundamental piece in the recovery and rehabilitation of mastectomised women. The RNS acts as a facilitator for improving quality of life, promoting not only physical recovery but also self-acceptance and emotional support for women. These professionals play an essential role in organising and managing care, highlighting their importance in the multidisciplinary team.
Furthermore, evidence indicates that strategies such as the use of devices and multidisciplinary approaches expand the possibilities for social reintegration and the recovery of self-esteem. Therefore, it is crucial that rehabilitation care is based on evidence-based practices, as suggested by the College of the Specialty of Rehabilitation Nursing of the Order of Portuguese Nurses (https://www.ordemenfermeiros.pt/a-ordem/col%C3%A9gios/mcee-de-reabilita%C3%A7%C3%A3o/, accessed on 1 March 2025). The RNS, as a facilitating agent, plays a vital role in organising and implementing patient-centred interventions, contributing to strengthening their self-confidence and autonomy.
The texts converge in emphasising that the Rehabilitation Nurse possesses crucial competencies for the comprehensive care of mastectomised women. This professional is responsible for developing strategies that promote early rehabilitation, the effective management of suffering, a reduction in complications, and the recovery of quality of life. Moreover, emotional support, family integration, and empowerment for self-care reinforce the positive impact of nursing interventions, demonstrating the relevance of individualised, evidence-based programs.
Author Contributions
All the authors contributed to the study as follows: M.R., I.D. and R.D. initiated the study design; P.B. and D.C. collaborated on the study design and reviewed the study. M.R., I.D. and R.D. wrote the review, and P.B. and D.C. revised the manuscript. R.F., C.S. and C.F. provided guidance and theoretical, practical, and research knowledge. All authors contributed to refining the study and approving the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Acknowledgments
The authors would like to thank their institutions and the Comprehensive Health Research Centre—CHRC-UÉ for all their collaboration in the development and implementation of this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Watkins, E.J. Overview of breast cancer. JAAPA 2019, 32, 13–17. [Google Scholar] [CrossRef]
- Harfouche, A.; Silva, S.; Faria, J.; Araújo, R.; Gouveia, A.; Lacerda, M.; D’Orey, L. Cancro de Mama: Valor em Saúde, Custos e Financiamento. Acta Med. Port. 2017, 30, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Pereira, D.; Martinelli Braga, A.A. A Mastectomia E A Ressignificação do Corpo no Feminino. Rev. Psicol. Divers. e Saúde 2016, 5, 47–64. [Google Scholar] [CrossRef]
- Gupta, M.; Goyal, N. Applied Anatomy of Breast Cancer. In Breast Cancer; Springer Nature: Singapore, 2022; pp. 23–35. [Google Scholar]
- IPO Mastectomia. Lisboa. 2019. Available online: https://www.ipolisboa.min-saude.pt/wp-content/uploads/2020/04/Cancro-Mama_Mastectomia.pdf (accessed on 21 April 2025).
- Hobson, P.; Meara, J. Quality of life in chronic disease rehabilitation. Rev. Clin. Gerontol. 2004, 14, 317–325. [Google Scholar] [CrossRef]
- Al Aateibi, B.S.; Sadoun, M.M.; Alnuaimi, N.R.; Alghamdi, S.A.S.; Alharthi, M.F.A.; Khayat, H.M.; Almatrafi, R.J.S.; Falattah, M.M.B.; Ridha, W.A.A.; Albariqi, N.A.A.; et al. Comprehensive Review of Nurses’ Role in Chronic Disease Management: Collaborative Care Approaches. J. Ecohumanism 2024, 3, 6651–6659. [Google Scholar] [CrossRef]
- Galanti, G.-A. Culturally Competent Rehabilitation Nursing. Rehabil. Nurs. 2005, 30, 123–126. [Google Scholar] [CrossRef]
- Camicia, M. Transforming Health Care through Improving Care Transitions: A Duty To Embrace. Rehabil. Nurs. 2015, 40, 1–2. [Google Scholar] [CrossRef]
- Vaughn, S.; Rye, J.; Allen, A.; Bok, A.; Mauk, K.; Park, L.; Pierce, L.; Wintersgill Holler, W. Inside Looking Out. Rehabil. Nurs. 2023, 48, 23–38. [Google Scholar] [CrossRef]
- Vaughn, S.; Mauk, K.L.; Jacelon, C.S.; Larsen, P.D.; Rye, J.; Wintersgill, W.; Cave, C.E.; Dufresne, D. The Competency Model for Professional Rehabilitation Nursing. Rehabil. Nurs. 2016, 41, 33–44. [Google Scholar] [CrossRef]
- OE. Padrões de Qualidade dos Cuidados de Enfermagem. Lisboa, 2001. Available online: https://www.ordemenfermeiros.pt/media/8903/divulgar-padroes-de-qualidade-dos-cuidados.pdf (accessed on 21 April 2025).
- OE. Padrões de Qualidade dos Cuidados Especializados em Enfermagem de Reabilitação. Lisboa, 2018. Available online: https://diariodarepublica.pt/dr/detalhe/regulamento/350-2015-67552234 (accessed on 21 April 2025).
- Wang, T.-C.; Chang, P.-H.; Chen, W.H.; Hung, C.-C.; Chen, J.-P.; Lin, Y.-C.; Chiou, A.-F. The Effectiveness of an Upper Limb Rehabilitation Program on Quality of Life in Breast Cancer Patients after Mastectomy: A Randomized Controlled Trial. Semin. Oncol. Nurs. 2023, 39, 151512. [Google Scholar] [CrossRef]
- Rodrigues, T.; Moreira, M.T.; Lima, A.; Fernandes, R.; Gomes, B. Contributions of a Rehabilitation Nursing Program in the Self-Care of Women Undergoing Breast Surgery. Nurs. Rep. 2023, 13, 913–922. [Google Scholar] [CrossRef]
- Tang, X. The effect of multi-supportive nursing on the postoperative rehabilitation of breast cancer patients. Am. J. Transl. Res. 2021, 13, 7327–7334. [Google Scholar] [PubMed]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Sampaio, R.; Mancini, M. Estudos de revisão sistemática: Um guia para síntese criteriosa da evidência científica. Rev. Bras. Fisioter. 2007, 11, 83–89. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- JBI. Critical Appraisal Tools. Joanna Briggs Institute. Available online: https://jbi.global/critical-appraisal-tools (accessed on 1 June 2025).
- da Silva, C.H.H.C.; de Araújo Cunha, T.A.; Dantas, C.S.; de Jesus, C.S. A importância da enfermagem no pós-operatório de mulheres mastectomizadas com dissecção de linfonodos axilares: Revisão integrativa. Res. Soc. Dev. 2021, 10, e57210616177. [Google Scholar] [CrossRef]
- Merêncio, K.; Ventura, M. Vivências da mulher mastectomizada: A enfermagem de reabilitação na promoção da autonomia. Rev. Enferm. Ref. 2020, 2, 1–8. [Google Scholar]
- dos Santos Cesário, J.M.; de Oliveira Hernandes, L.; Botion, B.M.; da Silva, G.K.A.; da Cunha, A.P.; Gomes, D.M.; da Silva Vitorino, P.G.; de Paula Flauzino, V.H. A prática clínica do enfermeiro na reabilitação estética de pacientes mastectomizadas. Res. Soc. Dev. 2022, 11, e504111032865. [Google Scholar] [CrossRef]
- Panobianco, M.S.; Felipe, I.D.O.; Canete, A.C.S.; Nunes, L.C.; Prado, M.A.S. Assistência de enfermagem em núcleo de reabilitação: O papel do enfermeiro. Rev. Enferm. UERJ 2020, 28, e51082. [Google Scholar] [CrossRef]
- Baldaia, C.; Fernandes, C.; Ferreira, L. Exergames na reabilitação da pessoa mastectomizada: Uma scoping review. Onconews 2024, 47. Available online: https://scielo.pt/scielo.php?script=sci_arttext&pid=S2183-69142023000200003 (accessed on 21 April 2025).
- Sun, L.-H. Application value of Neuman’s nursing model in the perioperative period of radical mastectomy. Am. J. Transl. Res. 2024, 16, 4928–4938. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Scofano, B.; Almeida de Lima, A.; Dos Reis Silva, R.; Garcia Penna, L.H.; Silva de Andrade, K.B.; Brito Pinheiro, A.P. Ações/plano de alta da enfermagem í mulher submetida í mastectomia. Nursing 2020, 23, 3736–3744. [Google Scholar] [CrossRef]
- Zúñiga-Tapia, R.; Panobianco, M.S.; Prado, M.A.S.; Henríquez, P.C. Experience in a rehabilitation center for mastectomized women at the start of the COVID-19 pandemic. Rev. Gaúcha Enferm. 2021, 42, e20200331. [Google Scholar] [CrossRef]
- Casassola, G.M.; Gonçalves, G.R.; Stallbaum, J.H.; Pivetta, H.M.F.; Braz, M.M. Intervenções fisioterapêuticas utilizadas na reabilitação funcional do membro superior de mulheres pós-mastectomia. Fisioter. Bras. 2020, 21, 93–103. [Google Scholar] [CrossRef]
- Mathieu, J.; Daneau, C.; Lemeunier, N.; Doyon, A.; Marchand, A.-A.; Descarreaux, M. Conservative interventions and clinical outcome measures used in the perioperative rehabilitation of breast cancer patients undergoing mastectomy: A scoping review. BMC Womens Health 2022, 22, 343. [Google Scholar] [CrossRef]
- JBI. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. Adelaide. 2014. Available online: https://jbi.global/sites/default/files/2019-05/JBI%20Levels%20of%20Evidence%20Supporting%20Documents-v2.pdf (accessed on 1 June 2025).
- Zeighami Mohammadi, S.; Mohammad Khan Kermanshahi, S.; Vanaki, Z. Reconstruction of feminine identity: The strategies of women with breast cancer to cope with body image altered. Int. J. Women’s Health 2018, 10, 689–697. [Google Scholar] [CrossRef] [PubMed]
- Latifi, M.; Salimi, S.; Barahmand, N.; Fahimnia, F.; Allahbakhshian Farsani, L. Postmastectomy Information Needs and Information-seeking Motives for Women with Breast Cancer. Adv. Biomed. Res. 2018, 7, 75. [Google Scholar]
- Fu, M.R.; Axelrod, D.; Guth, A.A.; Rampertaap, K.; El-Shammaa, N.; Hiotis, K.; Scagliola, J.; Yu, G.; Wang, Y. mHealth self-care interventions: Managing symptoms following breast cancer treatment. mHealth 2016, 2, 28. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.M.; Dwyer, K. Shoulder Impairment Before Breast Cancer Surgery. J. Women’s Health Phys. Therap. 2014, 38, 118–124. [Google Scholar] [CrossRef]
- Lee, M.; Kim, S.; Shim, J. Comparison of Shoulder Range of Motion, Pain, Function, Scapular Position Between Breast Cancer Surgery and Shoulder Surgery Female Patients. Phys. Ther. Korea 2015, 22, 9–18. [Google Scholar] [CrossRef]
- Crosbie, J.; Kilbreath, S.L.; Dylke, E.; Refshauge, K.M.; Nicholson, L.L.; Beith, J.M.; Spillane, A.J.; White, K. Effects of Mastectomy on Shoulder and Spinal Kinematics During Bilateral Upper-Limb Movement. Phys. Ther. 2010, 90, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Zhao, L.; Chen, M.; Li, S.; Liao, Y. The effects of rapid rehabilitation nursing on improving postoperative rehabilitation effect and life quality of early breast cancer patients. Medicine 2024, 103, e40533. [Google Scholar] [CrossRef] [PubMed]
- Truong, A.N. Rehabilitation of Patients with Breast Cancer. In Breast Cancer; Springer: New York, NY, USA, 2001; pp. 430–451. [Google Scholar]
- Kamusińska, E.; Ciosek, M.; Karwat, I.D. The importance of rehabilitation in the treatment of breast cancer. Med. Stud. 2014, 3, 214–220. [Google Scholar] [CrossRef]
- Kuliński, W.; Kosno, M. Quality of life in women after mastectomy. clinical and social study. Wiadomości Lek. 2021, 74, 429–435. [Google Scholar] [CrossRef]
- Mehta, J.; Vaghela, N.; Patel, H. The effect of physiotherapy in patients with modified radical mastectomy. Natl. J. Physiol. Pharm. Pharmacol. 2017, 8, 163–166. [Google Scholar] [CrossRef]
- Ahmed, E.; Sayed, A.; Mekkawy, M. Effect of Applying Shoulder Exercises on Shoulder Function after Modified Radical Mastectomy. Assiut Sci. Nurs. J. 2017, 5, 74–84. [Google Scholar]
- Park, H.S.; Cho, G.Y.; Park, K.Y. The Effects of a Rehabilitation Program on Physical Health, Physiological Indicator and Quality of Life in Breast Cancer Mastectomy Patients. J. Korean Acad. Nurs. 2006, 36, 310. [Google Scholar] [CrossRef]
- Elder, E.E.; Brandberg, Y.; Björklund, T.; Rylander, R.; Lagergren, J.; Jurell, G.; Wickman, M.; Sandelin, K. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: A prospective study. Breast 2005, 14, 201–208. [Google Scholar] [CrossRef]
- Soanes, L.; White, I.D. Sexual Consequences of Cancer and Its Treatment in Adolescents and Young Adults. In Cancer in Adolescents and Young Adults; Springer International Publishing: Cham, Switzerland, 2017; pp. 603–631. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).