Abstract
Background The COVID-19 epidemic had a deleterious impact on mental health and substance abuse and led to an increase in several forms of violence, including self-harm and interpersonal violence among youth from low- and middle-income countries. Nevertheless, the relationship between the variables and their directionality has not been recognized. This study describes the relationship directionality between these variables among 18- to 20-year-old Mexican youths during the COVID-19 pandemic. Methods The longitudinal cohort study comprises an evolving group of young Mexican adults: 1390 participants aged 18 in 2021, 654 aged 19 in 2022, and 442 aged 20 in 2023. Proportions by sex—50% were matched in every cohort, and the evolution–age sample accomplishment accounted for 47% in 2022 and 32% in 2023. Results According to a structural equation model, which fit the data from 195 iterations with 246 parameters (X2[2722] = 8327.33, p < 0.001), yielding a CFI of 0.946, a TLI of 0.943, and an RMSEA of 0.029 [0.028–0.029]), perpetrating intimate violence, preceded by suffering intimate violence, combined with suffering anxiety symptoms, was associated with self-harm–suicide thoughts and behaviors (ShSTB), marked distress, dysfunction, and somatization symptoms. The relationship was stronger in women and 20-year-old Mexicans. In men, this pathway was exclusively associated with ShSTB. Suffering from intimate violence has been associated with depression, anxiety, and PTSD symptoms, as well as harmful alcohol use. Conclusions During an epidemic, prevention programs should be designed to warn about self-harm–suicide thoughts and behaviors, not only to ensure the safety of the victims of intimate personal-violence but also to prevent the suicidal behavior of perpetrators.
1. Introduction
The COVID-19 pandemic directed attention to self-harm and suicidal thoughts and behaviors (ShSTB), in addition to the increase in perpetrating–suffering intimate-interpersonal violence, mental health symptoms, and harmful alcohol use (HAU) in youth from low and middle-income countries (LMICs). Previous data suggest a relationship between perpetrating–suffering intimate violence and ShSTB, with alcohol use and mental health symptoms as associated factors. Describing trends and relationship directionality between violence, ShSTB, mental health symptomatology, and HAU is needed to contribute to the development of effective self-harm–suicide prevention programs in young people in LMICs suffering or perpetrating violence.
The mental health Gap Action Programme [1] has stated that suicide is the act of deliberately killing oneself, and that self-harm is intentional self-inflicted poisoning or injury, which may or may not have a fatal intent or outcome. In such context, suicide is the fourth leading cause of death among 15–29-year-olds, with 77% of global suicides occurring in LMICs [2]. In Mexico, self-harm accounted for 5.3 (95% UI 4.28–6.46) deaths per 100,000 population in 2019, showing an upward trend since 2000 [3], with 2.2 (95% UI 1.73–2.70) and 8.7 deaths per 100,000 population (95% UI 7.06–10.60) for women and men, respectively. These disease burden levels place Mexico in the 3.40 to 60 quintiles across all countries. In a previous study of 18,449 Mexicans during the COVID-19 pandemic, we reported that 33.30% of our participants presented at least one ShSTB symptom, 4.20% had had previous self-harm thoughts and behaviors (PShTB), while 38.30% reported marked distress, dysfunction, and somatization (MDDS) [4].
The World Health Organization (WHO) [5] defined violence as occurring among individuals who may or may not know each other, including a range of acts from bullying and physical fighting to more severe sexual and physical assault. Youths aged 10–29 have experienced at least one type of assault [5]. The United Nations Office on Drugs and Crime Research—Data Portal—Violent and Sexual Crime (UNODC [6]) indicated a tendency for sexual violence based on the unique violent offense data available for Mexico, with a rate of 2.47 per 100,000 population in 2015, 3.46 in 2016, 2.89 in 2017, 2.82 in 2018, 1.96 in 2019, 3.71 in 2020, 6.00 in 2021, and 7.22 in 2022. In a recent study of 7420 Mexicans aged 18–24, we found that 23.48% of young participants perpetrated interpersonal violence and 15.38% perpetrated intimate violence, while 25.26% had experienced intimate violence in 2023 [7].
Regarding the American Psychiatric Association [8], Major Depressive Disorder is when sadness, interest loss, guilt or worthlessness, energy loss, concentration loss, appetite change, psychomotor agitation or retardation, sleep change, and suicidal thoughts occur, lasting for at least two weeks [8]. Generalized Anxiety Disorder is defined as symptomatology referring to excessive worry most days, and three out of six symptoms, such as restlessness, fatigue, decreased concentration, irritability, tension, or insomnia, that interfere with work or social functioning, all for at least six months [8]. Regarding Posttraumatic Stress Disorder, APA [8] has identified four groups of symptoms after an exposure to direct or witnessed threats, injuries, or violence: reexperiencing, avoidance of stimuli, negative alteration in cognition and mood, and marked alterations in arousal and reactivity, all related to the traumatic event. In this context, it has been described that the COVID-19 pandemic headed a 27.6% increase in depression cases and a 25.6% rise in anxiety in 2021 [9]. The Pan American Health Organization [10] also reported a 6.5% rise in mental health issues (8.9% in women and 3.2% in men) in Mexico between 2000 and 2019. The rate was 1716.4 YLD per 100,000 Mexicans in 2019 (1975.7 for women and 1438.2 for men). Our preliminary study during the pandemic indicated a prevalence of depression, anxiety, and PTSD symptoms among Mexican youth of 44.46%, 47.90%, and 29.47%, respectively [7].
Lastly, HAU is a pattern of psychoactive substance use that damages health. This damage may be physical or mental, and it is associated with social consequences, e.g., family or work problems [1]. Alcohol consumption is responsible for 2.6 million deaths each year globally. It is the leading factor for premature mortality and disability among those aged 20 to 39, accounting for 13% of the deaths in this age group [11]. In Mexico, alcohol use went up from 28% in 2011 to 33.6% in 2016 [National Report on Alcohol and Tobacco—Ramón de la Fuente Muñiz National Institute of Psychiatry [INPRFM], [12]). Our study showed that 20.20% of Mexican youth reported HAU during the pandemic [7].
The frequency of ShSTB, MDDS, perpetrating–suffering intimate–interpersonal violence, depression, anxiety, PTSD, and HAU between our Mexican population highlights the need to describe the relationship directionality between them, as well as the role of sex, for improving cost-effective preventive programs and mental health interventions. Clare et al. [13] have suggested that research should consider the common social determinants of violence and ShSTB, including early exposure to substance use and mental health issues. Perpetrating intimate violence, after suffering it, may explain the presence of the ShSTB. Comorbidity of suicide, self-harm, violence, mental health, and HAU may have an order of co-occurrence in life.
Perpetrating intimate violence and having ShSTB have common risky social determinants, including early exposure to adversity (such as witnessing or being a victim of intimate violence), substance use, and mental health problems [13]. Rooney et al. [14] even indicated that the experience of suffering and perpetrating violence may provide youth with the capability (such as fearlessness and physical means) to engage in suicidal behavior. They have particularly suggested that perpetration of violence may increase after being a victim of violence, and that such trajectory may increase the probability of suffering from ShSTB occurrence.
There is evidence to support the association between various psychosocial conditions (such as depression, hopelessness, social isolation, and adverse life events) and suicidal thoughts. Yu and Zhu [15] suggested that being the victim of intimate partner violence is associated with ShSTB. Aloyce et al. [16] also found that depression is a common health problem strongly associated with intimate partner violence perpetration in young men aged between 18 and 24 years. We previously explored the relationship between depression, anxiety, and related MDDS with ShSTB by sex in Mexican adults during the COVID-19 pandemic [4]. Our findings suggest that depression leads to ShSTB in three possible ways: through PShTB, PShTB affecting MDDS, and generalized anxiety affecting MDDS. Predisposing factors for ShSTB would appear to include depression, anxiety, and hopelessness. Nevertheless, Benatov et al. [17] reported that traditional bullying perpetration was prospectively associated with suicide attempts, whereas being the victim of bullying was cross-sectionally associated with suicide ideation and attempts.
Exposure to interpersonal violence is associated with suicide attempts and suicide among youth and young adults [18]. Among adults, those who perpetrate violence are more likely to report suicide attempts [19]. Research also examining non-suicidal and suicidal self-injury risk among victims of bullying (in other words, those who bully others and are bullied themselves) suggests that they are at greater risk for suicide than those who are only victims or perpetrators [20]. Wolford-Clevenger et al. [21] also found a high prevalence of non-fatal suicidal ideation among perpetrators of violence.
Kafka et al. [22] evaluated the nature of intimate violence prior to suicide, by sex, between 2010 and 2017 in North Carolina. They noted whether the person who died by suicide was described as a perpetrator of violence, a victim, or both (bilateral violence), recording the type of abuse, whether physical or emotional, verbal threats to harm/kill, illegal trespassing, sexual assault, or stalking, and abusive suicide-related threats in the two weeks prior to their death. They described 439 suicides in which 72.67% of male decedents had perpetrated non-fatal intimate violence compared to 51.22% of female decedents, who also reported perpetrating intimate violence. Findings suggested that intimate personal violence may be a precipitating factor in 6.1% of suicides in North Carolina. Over 80% of decedents had engaged in non-fatal intimate personal violence prior to their suicide, while intimate violence was more common for youth involved in the criminal legal system, who revealed suicidal intent and used a firearm or alcohol. A systematic review by Sesar et al. [23] identified nine studies examining the association between perpetrating intimate violence and non-fatal suicidal behaviors in community and clinical samples, concluding that suicide is an impulsive response to acute strain or conflict in an already abusive relationship.
Rooney et al. [14] examined the association between suffering, perpetrating, and attempting suicide in a national sample of American youth reporting suicide ideation in the past year, suggesting that those who both experience and perpetrate violence are at greater risk for engaging in suicide behaviors, with a cumulative effect. The authors worked with 821 participants who indicated that they had seriously thought about committing suicide in the past year—63.1% female, 64.7% white, and 12.1% hispanic. They used stepwise hierarchical regressions to examine the association between victimization and perpetrating violence and attempting suicide, reporting that 52.7% suffered some form of aggression, 30.8% perpetrated some form of violence, and 28% attempted suicide in the past year. In general, the authors concluded that victimization and the interaction between victimization and perpetrating violence were associated with the frequency of attempting suicide, over demographics, depression, and other non-violent externalizing behaviors.
While both being victim of and perpetrating violence are associated with suicidal behaviors generally, there is a need to research suicidal thoughts and behaviors among those who are both suffering and perpetrating violence [13]. Further research needs to confirm how perpetrating intimate violence is associated with single suicides unrelated to other violent deaths [17]. Additional research throughout a prospective longitudinal cohort study may help to describe the relationship between victimization and perpetration of violence and ShSTB over time. But mainly, we want to know: does perpetrating intimate violence, after suffering it, relate to the presence of the ShSTB, mental health problems, and HAU in life?
Prevalence of ShSTB, intimate violence, mental health symptoms, and HAU was high in Mexico during the pandemic. Previous independent studies also suggest an association between ShSTB and suffering–perpetrating intimate–interpersonal violence, mental health conditions, and HAU in Mexico [4,7]. A cohort longitudinal study will help to describe the relationship directionality between perpetrating and suffering intimate violence, ShSTB, mental health symptoms, and HAU among 18- to 20-year-old Mexican youths. In previous findings (e.g., [4,7,14] or [23]), we have proved directionality associations by screening for violence to ShSTB, mental health problems, and HAU. Thus, our hypotheses state that perpetrating intimate violence and suffering intimate violence are associated with ShSTB (Ha1 and Ha2), as well as depressive, anxious, and PTSD symptoms (Ha3, Ha4, and Ha5), and HAU (Ha6) in one evolving age group.
2. Methods
2.1. Participants and Procedure
We based our research on a longitudinal evolving group cohort study. Therefore, we analyze data from 2486 young Mexicans, comprising 1390 aged 18 in 2021 (55.91%), 654 aged 19 in 2022 (26.31%), and 442 aged 20 in 2023 (17.78%). As for proportions by sex, 50% were matched in every cohort. Thus, the evolution–age sample achievement accounted for 47% in 2022 and 32% in 2023 (see Table 1).

Table 1.
Proportions by Sex and Cohort Years.
Participants were invited to enroll voluntarily in a web-based application called My Health is also Mental (https://www.misalud.unam.mx (accessed on 31 December 2023), [4]), through the Health Ministry and the University Call for applications on their websites (announced by press conferences on the radio, television, and internet). Participants entered if they were interested in screening their mental health or seeking psychological care during the COVID-19 pandemic. Therefore, once they entered the application, they had to use their email addresses to register and complete an evaluation of their mental health status and receive free feedback and treatment if necessary.
We used the criteria for internet E-surveys, such as data protection, development, testing, contact mode, advertising the survey, compulsory/voluntary participation, completion rate, cookies used, IP check, log file analysis, registration, and atypical timestamp considerations [24]. Since the survey platform automatically eliminates respondents who fail to complete the survey, we can only obtain complete response rates. It means that we have a zero rate of respondents who did not complete the survey. Consequently, we are not able to describe Mexicans not interested in participating in the strategy.
The Ethics Committee of the Psychology Faculty of the National Autonomous University of Mexico (UNAM) approved the project (code FPSI/422/CEIP/157/2020. All participants signed the informed consent about findings being used for epidemiological research and the opportunity to refuse complying with the data requests and dropping out at any point in the study. The study did not offer any incentive; however, it provided psychoeducational material, and written feedback (e.g., with infographics about relaxation techniques). Feedback contained information about how to get remote psychological care from public health services, if needed. Lastly, we asymmetrically transformed personal information from the database with numbers and letters to protect them while holding it in the official university domain. Only authorized researchers could access information using security locks that protect data.
2.2. Instruments
The survey [4] includes a sociodemographic section and seven psychological tests (see Appendix A). The self-harm/suicide survey is a twenty-one question yes/no dichotomic response item scale classified on three blocks referring to symptoms now, in the past month, and in the past year from the mhGAP algorithm [1,4]: the ShSTB warning signs, the PShTB, and the MDDS scales. Subjects are considered at risk when they have at least one symptom in each scale. The three-factor model obtained an (186) = 19,643.19, p < 0.001; an RMSEA = 0.075 (0.074–0.076), a CFI = 0.984, a TLI = 0.982, and an α = 0.94.
The Life Events Checklist 5th edition (LEC-5; [25,26]) screens suffering–perpetrating intimate–interpersonal violence with 11 yes/no dichotomic response items relating to the past six months (see Appendix A). The suffering intimate violence scales obtained an (2) = 6.09, p < 0.048, an RMSEA = 0.017 (0.001–0.032), a CFI = 0.999, a TLI = 0.997, and an α = 0.76 (Morales-Chainé et al. [7]). The suffering interpersonal violence scales got an (13) = 343.57, p < 0.001, an RMSEA = 0.059 (0.053–0.064), a CFI = 0.949, a TLI = 0.917, and an α = 0.76. The perpetrating intimate model identified exact parameters, with an α = 0.68. The perpetrating interpersonal violence scales got an (2) = 94.634, p < 0.001, an RMSEA = 0.079 (0.066–0.093), a CFI = 0.952, a TLI = 0.855, and an α = 0.68. Participants were asked to choose the violent event that bothered them most at the time, and to answer the questions in part B of the Posttraumatic Check List (PCL-5).
The PCL-5 included 20 five-option-response items [27] about stressful symptoms in the past month (see Appendix A). We used the four-factor DMS-5-TR [8,26] structure [28]: reexperiencing, avoidance, negative alterations in cognition and mood (NACM), and hyperarousal. The four-factor structure got an (162) = 4535.593, p < 0.001, a CFI = 0.916, a TLI = 0.901, an RMSEA = 0.076 (0.074–0.078), an SRMR = 0.044, and an α = 0.93 [7]. PTSD is considered when the 2-response option or more is selected for at least one of the B-items, one of the C-items, two of the D-items, and two of the E-items, plus considering symptoms present for over a month.
The Major Depressive Episode (MDE) checklist is an 11-question five-option-response item scale covering the past twelve months from the DSM-5-TR [8] (see Appendix A). The scale obtained an (42) = 1210.25, p < 0.001, a CFI = 0.954, a TLI = 0.939, an RMSEA = 0.072 (0.069–0.076), an SRMR = 0.034, and an α = 0.89 [7]. The at-risk score is met when part 1, part 2, part 3, and criterion A and B guidelines are reached. The criterion for Part 1 is met when items one and two are answered with options 1 or 2. The criterion for Part 2 is met when five or more items are answered with options 1 or 2 from items 2 to 10 and Part 1. The criterion for Part 3 is met when question 3 is answered with response options 1 or 2. Criterion A is met when part 1 and part 2 or 3 are completed. Criterion B is met when question 11 is answered with response options 1, 2, or 3. Lastly, an MDE is identified when criteria A and B are met [8].
The Generalized Anxiety (GA) [29] is a five-question eleven-response-options item scale about symptoms in the past two weeks (see Appendix A). The scale obtained an (5) = 74.940, p < 0.001, a CFI = 0.998, a TLI = 0.995, an RMSEA = 0.043 (0.035–0.052), an SRMR = 0.005, and an α = 0.93 [7]. At risk GA resulted in a symptomatology average of 60%.
The WHO Alcohol, Smoking, and Substance Involvement Screening Test determines harmful use for ten groups of substances (e.g., HAU by screening use of alcoholic beverages [beer, wine, spirits], see Appendix A [30]). In the ASSIST, eight questions screen for HAU (e.g., failing to do what is expected because of the use of the drug in question); ASSIST also screens for injecting any drug (non-medical use only). The total ASSIST obtained an [8] = 163,646, p < 0.001, an RMSEA = 0.051, confidence interval of 0.045–0.058, an SRMR = 0.018, a CFI = 0.986, and a TLI = 0.973 [7]. The Cronbach α varied from 0.71 for the hallucinogen dimension, 0.77 for alcohol, to 0.96 for opioids [7]. We have calculated the score of the HAU as instructed by the WHO [30] [on page 32 of the ASSIST manual], adding the answers to questions two to seven. In the study, we just considered the alcohol scale.
2.3. Data Analysis
First, we ran the Confirmatory Factor Analysis CFA for each scale (with the maximum likelihood [ML] and the diagonally weighted least squares [DWLS] procedures [31,32]. We evaluated the overall fit of the models with the chi-square goodness of fit test: the Comparative Fit Index (CFI), the Tucker–Lewis Index (TLI), the Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR) [31,32]. We did not consider the SRMR index for categorical data [30]. We calculated Cronbach’s alpha reliability for each scale.
Secondly, we obtained scores for each scale and classified subjects who met the self-harm/suicide (ShSTB, MDDS), violence (LEC-5), PTSD (PCL-5), depression (MDE), anxiety (GA), and HAU (from the ASSIST) criteria for risk. We compared the distribution of participants regarding such criteria by sex and cohort year of the pandemic, performing chi-squared tests and considering p-values under 0.05 on distributions.
At the end, we evaluated the association directionality between suffering and perpetrating intimate and interpersonal violence, ShSTB, MDDS, mental health symptoms and HAU with the Structural Equation Modeling [SEM], with a mixture of continuous and categorical variables [31,32], based on the comparison with the chi-square curve. The chi-square test proves the hypothesized models fit the data, based on the good fitting data indexes (e.g., TLI), to be confident about the latent variable association directionality [32]. We also got models by sex and cohort year of the pandemic. For the analysis, we used the Lavaan statistical package 0.6–11, from the RSTUDIO® statistical software 2022.02.0 [33] and the SPSS Statistics 25 [34].
3. Results
3.1. Confirmatory Factorial Analyses and Cronbach’s Alpha
Appendix B shows the psychometric properties of all scales in the present study, as a replication of previous studies [4,7]. Thus, Appendix B shows the CFAs of the ShSTB, MDDS, LEC-5, MDE, GA, PCL-5, and ASSIST scales. Data fitting showed CFIs and TLIs > 0.90, RMSEAs < 0.08, and SRMRs < 0.06—the latter for continuous data for all scales. The reliability of the scales ranged from 0.38 for the Perpetrating Interpersonal Violence scale to 0.97 for the NACM from the PCL-5 and the MDE.
3.2. Self-Harm–Suicide, Violence, Depression, Anxiety, PTSD, and HAU for the Total Sample by Sex and Cohort Years
The distribution of participants at risk for ShSTB, MDDS, violence, depression, anxiety, PTSD, and HAU in the total sample by sex and cohort year are shown in Table 2. In the overall sample and according to the cutoff score in the corresponding scales, 38.10% of participants were at risk for ShSTB and 40% for MDDS; 37.70% of youths were at risk for suffering intimate violence, 58.70% for suffering interpersonal violence, 19.10% for perpetrating intimate violence, and 32.50% for perpetrating interpersonal violence. 71.00% of participants were at risk for depression, and 47.70% for anxiety, 43.10% were reexperiencing violence symptoms, 36.10% suffered from avoidance, 47.40% from NACM, and 46.90% from hyperarousal, while 47.10% of participants met the PTSD criterion. Finally, 18.20% of participants were at risk for HAU.

Table 2.
Distribution of Participants at Risk for Self-harm–suicide, Violence, Depression, Anxiety, PTSD Symptoms, and Harmful Alcohol Use for the Total Sample by Sex and Cohort.
Moreover, women at risk for ShSTB, MDDS, suffering–perpetrating intimate–interpersonal violence, and mental health symptoms were significantly higher than men (p < 0.001). The participants at risk for alcohol use were similar by sex. There were significant differences between the proportions of participants at risk in the three-year-cohort group for almost all variables except depression (p < 0.001). The trends would appear to have increased by the last cohort year of the pandemic: 20-year-olds in 2023. Depression symptoms remained stable across the three cohort years.
3.3. Structural Equation Modeling
Figure 1 shows the overall model. For the three years of the pandemic, the model includes the following paths: from perpetrating intimate violence (PIV) to ShSTB (βPIV, βShSTB = 0.137) and MDDS (βPIV, βMDDS = 0.084), from anxiety to ShSTB (βGA, βShSTB = 0.591) and MDDS (βGA, βMDDS = 0.634), and from suffering intimate violence (SIV) to reexperiencing, avoidance, negative alterations in cognitions and mood (NACM), hyperarousal (βSIV, βRex = 0.823, βSIV, βAvo = 0.830, βSIV, βNACM = 0.832, βSIV, βHyp = 0.829, respectively), to depression and anxiety (βSIV, βMDE = 0.180, and βSIV, βGA = 0.698, respectively), to HAU (βSIV, βAlc = 0.347), and perpetrating interpersonal and intimate violence (βSIV, βPIntV = 0.702, βSIV, βPIntPV = 0.665, respectively).
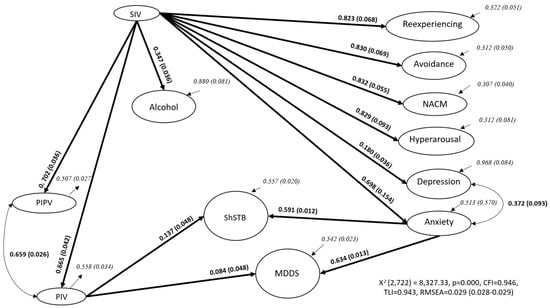
Figure 1.
Variables from SEM, path coefficients, and residual variances for the whole sample. Adapted with permission from Morales-Chainé et al. [4]. Note. ShSTB—current Self-harm and Suicide Thoughts and Behaviors; MDDS—Marked Distress, Dysfunction, and Somatization; SIV—Suffering Intimate Violence; PIV—Perpetrating Intimate Violence; PIPV—Perpetrating Interpersonal Violence; NACM—Negative Alterations in Cognitions and Mood.
SIV was indirectly associated with ShSTB and MDDS through PIV, meaning that it is associated with ShSTB and MDDS: SIV–PIV–ShSTB and SIV–PIV–MDDS, given that GA is also related to ShSTB and MDDS. The model fit the data from 195 iterations with 246 parameters (X2[2722] = 8327.33, p < 0.001). It yielded a CFI of 0.946, a TLI of 0.943, and an RMSEA of 0.029 [0.028–0.029]), using a mixture of continuous and categorical observed variables from the total sample. Appendix A shows factor loadings for the observed variables for each scale of the SEM. In all cases, factor loadings were greater than 0.300.
Table 3 shows the general pattern replicated for women and 20-year-old participants in 2023. For women and the oldest cohort, SIV + PIV and anxiety were therefore associated with ShSTB and MDDS symptoms, and SIV was strongly related to PTSD symptoms, anxiety, depression, HAU, PIPV, and PIV. For men, SIV + PIV and anxiety were related to ShSTB, but only anxiety was associated with MDDS symptoms. For men, SIV was also associated with mental health symptoms, HAU, and perpetrating interpersonal–intimate violence. For the two younger cohorts, anxiety was the variable related to ShSTB and MDDS symptoms. At the same time, SIV was associated with mental health symptoms, HAU, and perpetrating interpersonal–intimate violence. All models obtained CFIs and TLIs over 0.949, RMSEAs, and upper confidence intervals under 0.027.

Table 3.
Variables from SEMs with their path coefficients (β) and standard errors (e) by sex and cohort year.
The results suggest the scale’s dimensionality, perpetrating–suffering interpersonal–intimate violence, ShSTB, MDDS, mental health symptomatology, and HAU, among the cohort years during the pandemic, were all moderated by sex. We have evidence that perpetrating intimate violence and anxiety were related to ShSTB and MDDS (Ha1 and Ha4) for women, and in the last cohort year, SIV indirectly by PIV was also associated with ShSTB and MDDS (Ha2) for women and in the last cohort year. PIV and, indirectly, SIV were exclusively related to ShSTB for men (Ha1–Ha2). SIV was associated with PTSD symptoms (Ha5), depression (Ha3), anxiety (Ha4), HAU (Ha6), and perpetrating interpersonal–intimate violence for all participants.
4. Discussion
The present study describes the relationship directionality between perpetrating and suffering intimate violence, ShSTB, mental health symptoms, and HAU among 18- to 20-year-old Mexican youths through a longitudinal cohort study during the COVID-19 pandemic. Findings suggest an upward trend in self-harm–suicide, violence, mental health symptoms, and HAU in young Mexicans in 2021, 2022, and 2023. They mainly indicate that women and 20-year-old Mexicans who perpetrated intimate violence after suffering intimate violence and anxiety symptoms experienced self-harm–suicide warning signs and MDDS. Suffering intimate violence is also associated with PTSD, depression, anxiety symptoms, HAU, and perpetrating violence. These patterns varied for men and younger cohorts. In particular, men who also reported perpetrating intimate violence after suffering intimate violence and suffering anxiety symptoms experienced self-harm–suicide warning signs.
The proportions of young people perpetrating intimate violence were slightly higher than what our previous longitudinal cohort study suggested in 2024. We have seen asymmetries by sex for mental health conditions as well as patterns; except for depression, which remained high and stable during the pandemic for the entire sample [2,5,9]. HAU is a crucial condition associated with self-harm–suicide and violence. Findings indicated an increasing pattern among Mexican youth, reporting harm due to the use of this substance, and similar rates between men and women. Incidence of alcohol use was similar to what INPRFM [11] and our previous study indicated [7].
According to our hypothesis, findings thus suggest an associative pattern where perpetrating intimate violence, preceded by suffering intimate violence as well as anxiety symptoms, were associated with ShSTB and MDDS symptoms. However, the relationship was stronger in women and 20-year-old Mexicans. Among young Mexican men, the association between perpetrating intimate violence preceded by suffering violence and anxiety was exclusively associated with ShSTB warning signs. In addition, suffering intimate violence has been related to mental health symptoms such as depression, anxiety, and PTSD symptoms, as well as HAU. Our findings contribute to what Aloyce et al. [16] already suggested about depression related to intimate partner violence in youth, and to what Yu and Zhu [15] also proposed about intimate partner violence victimization related to ShSTB. Our findings indicate a central role played by the perpetrated intimate violence; once participants suffered from intimate violence, ShSTB warning signs and MDDS arose in women, and only ShSTB in men.
The central findings of PIV-SIV-GA associated with ShSTB and MDDS agree with previous ones reported by Benatov et al. [17] who also reported that perpetration was associated with suicide attempts, and being the victim of violence was related with suicide ideation and attempts. Our secondary proved hypothesis, in which SIV is associated with mental health and alcohol use, is also similar to what Kafka et al. [22] suggested about intimate violence being common in younger participants who also use alcohol and to our previous findings about SIV associated with depression, anxiety, PTSD symptoms, and HAU [7].
As Rooney et al. [14] suggested, in the current study, it appears we examined the association between perpetrating–suffering violence and self-harm–suicide thoughts and behaviors among Mexicans at the time of the evaluation. Nevertheless, instead of stepwise hierarchical regression, we used SEM analysis to examine these associations. Our model, therefore, suggested that the perpetration of violence was associated with ShSTB for the young Mexican people in our sample who experienced victimization, also supporting conclusions about the interaction between violent victimization and perpetration associated with ShSTB, even after accounting for sex, gender, mental health symptoms, and alcohol use.
Rooney et al. [14] suggested that separate processes contribute to suicide ideation and suicide attempts. They proposed that ideation-to-action frameworks could pinpoint the role of the acquired capability for suicide in the process of engaging in suicide behavior. They describe how painful or provocative experiences drive increases in pain tolerance and lack of fear of death, which contribute to the acquired capability for suicide. As all these authors have suggested, future studies should consider that being a victim of violence may be associated with increased pain tolerance. In contrast, violence perpetration may be associated with a decreased fear of death and an increased willingness to engage in self-directed violent acts. Morales-Chainé, Palafox, et al. [4] suggested distinguishing suffering from marked distress, dysfunction, somatization, and anxious depression from conditions where only the participants suffer from depression to prevent suicidal thoughts and behaviors. Moreover, current findings seem to suggest that previous experiences of suffering could interact with perpetrating intimate violence to explain reported ShSTB in both men and women and MDDS in women and 20-year-old participants.
It seems that being a victimi of intimate violence is followed by a traumatic stress response (such as reexperiencing, intrusive cognition, avoidance, or numbing) and that it may serve to habituate adolescents to pain, increasing their acquired capability and accounting for the association between victimization and suicide attempts [35]. Dewar et al. [36] also reported that perpetrators used non-fatal suicidal behaviors as a coping strategy to deal with overwhelming negative emotions, particularly in response to relationship stressors. Participants in our study reported this type of mental health symptom was associated with suffering intimate violence. It is, therefore, essential to continue exploring how mental health symptoms interact with perpetrating–suffering intimate violence to increase this proposed capability due to increased pain tolerance or a reduced fear of death in future research.
Meanwhile, Rooney et al. [14] have already suggested that repeated experiences of perpetration may result, for example, in decreased fear of death in the face of physical danger—signaling an increase in the acquired capability for suicide. A history of violent perpetration and victimization could indicate that the young participants in this study have an increased capability for self-harm–suicide thoughts and behaviors. However, it is essential to determine whether young Mexicans displaying an increase in marked distress, dysfunction, and somatization symptoms have greater pain tolerance or a reduced fear of death due to their acquired capability for perpetrating intimate violence after suffering intimate violence. There is a need to confirm these conditions and their relationship with the ShSTB warning signs in clinical studies and with men, women, and 20-year-old participants.
The Three-Step Theory (3ST; [37]) posits that ShSTB develops in the presence of everyday pain (such as emotional pain) connected with lack of hope in life. The second step is the development of severe ideation, when the pain becomes higher than the sense of connectedness. At the end, the theory emphasizes the capability for suicide as a component of the intent to die. The capability for suicide is characterized by the habituation to the fear of death aroused by suicide ideation. The exposure to factors associated with suicide behavior may facilitate the development of suicide capability and help us identify effective mechanisms for prevention and intervention on suicide behavior matters.
We were able to measure ShSTB, MDDS, perpetrating–suffering intimate–interpersonal violence, depression, anxiety, PTSD symptoms, and HAU in young Mexicans during the pandemic. ShSTB and MDDS symptoms were conceptualized in the mhGAP [1]. Perpetrating–suffering intimate–interpersonal violence was also conceptualized regarding what Oram et al. [38], Alexander and Johnson [39], Kourti et al. [40], Scott-Storey et al. [41], Weathers et al. [25], and Morales-Chainé et al. [7] suggested. Depression, anxiety, PTSD symptoms, and HAU were evaluated as recommended by the American Psychiatric Association [8], Goldberg et al. [29], Blevins et al. [28], and WHO [30], in that order.
Study findings suggest the relationship directionalities between ShSTB, MDDS, violence, mental health, and alcohol use for a group of young Mexicans during the pandemic. We have seen increased reports of self-harm, suicide risks, MDDS, perpetrating–suffering intimate–interpersonal violence, anxiety, PTSD symptoms, and alcohol use in youth aged from 18 in 2021 to 20 in 2023 at the end of the pandemic. Almost one in two youths suffered from ShSTB or MDDS symptoms. Findings showed that one in five women had perpetrated intimate violence. One in two women suffered intrafamilial violence as compared to one in three men [7]. Furthermore, 65.20% of the women suffered interpersonal violence as contrasting to 52.10 of men. ShSTB and MDDS, and suffering intimate and interpersonal violence, increased by the end of the pandemic among young people in our study.
Intimate violence precedes a significant proportion of ShSTB and MDDS, pointing to clear opportunities for intervention. It is essential to identify abusive partner-threatening suicide planning not only to ensure the safety of the victim of intimate personal violence but also to prevent the perpetrator’s suicidal behavior from emerging as a result of these social conditions. Considering trauma-informed approaches for intervention programs integrating suicide prevention efforts could increase the effectiveness of these programs while encouraging people who are perpetrating intimate personal violence to seek treatment [7]. Developing screening and early intervention for intimate personal violence and suicidal thoughts and behaviors mediated by sex could help prevent socially tough outcomes. We may provide training on assessment and early treatment of self-harm and suicide to those professionals that work with clients who suffer received or perpetrated violence.
5. Conclusions
Our study describes the relationship directionality between perpetrating and suffering intimate violence, ShSTB, mental health symptoms, and HAU among 18- to 20-year-old Mexican youths through a longitudinal cohort study during the COVID-19 pandemic. Findings suggest upward patterns in ShSTB, MDDS, violence, mental health symptoms, and harmful use of alcohol in very young Mexicans in 2021, 2022, and 2023. Nearly one in two youths suffered from ShSTB or MDDS symptoms. Furthermore, one in five women have perpetrated intimate violence, while one in two women suffered intimate violence in contrast to one in three men. Self-harm–suicide, marked distress, dysfunction, and somatization symptoms, and suffering intimate and interpersonal violence, increased by the end of the pandemic among young Mexicans. We noted asymmetries by sex for mental health conditions and growing patterns, except for depression, which remained high and stable during the pandemic, for our sample. Findings imply an increasing pattern among Mexican youth to report harm due to the use of this substance, with similar rates between young Mexican men and women.
Our study suggests an associative pattern where perpetrating intimate violence, preceded by suffering intimate violence combined with suffering anxiety symptoms were associated with ShSTB and MDDS. Nevertheless, the relationship was stronger in women and 20-year-old Mexicans. Among the young men in our sample, the relationship between perpetrating intimate violence preceded by suffering violence and anxiety was exclusively associated with ShSTB. Moreover, suffering from intimate violence has been related to mental health symptoms such as depression, anxiety, and PTSD symptoms, as well as HAU. Future research could explore whether young Mexicans displaying increased MDDS symptoms have increased pain tolerance or a reduced fear of death regarding their acquired capability for perpetrating intimate violence after suffering intimate violence. Confirming these conditions and their relationship with ShSTB in clinical studies and with men, women, and 20-year-old participants is essential.
Forthcoming research may consider mechanisms explaining how perpetrating–suffering violence is related to the capability for suicide behaviors and how MDDS symptoms increase tolerance of pain or reduce the fear of death. It may be helpful to study mechanisms to prevent in ShSTB and perpetrating–suffering intimate violence in Mexico. We need to adopt evidence-based interventions for self-harm and suicide while addressing perpetration of intimate violence at the primary care level, reducing the intervention gap to specialized care services in Mexico.
Intimate violence leads to a self-harm/suicide risk, emphasizing opportunities for prevention. We need to screen participants who warn about ShSTB for the safety of the victims of intimate personal violence and to prevent the perpetrator’s suicidal behavior. Conclusions in Mexican youth point to the need to design cost-effective perpetrating intimate violence interventions to prevent self-harm–suicide warning signs, marked distress, dysfunction, and somatization, distinguishing between sex and age, as well as to eliminate intimate violence and diminish mental health problems and HAU, as a public health policy for future pandemics. We need to design cost-effective intimate violence interventions to prevent ShSTB, MDDS, depression, anxiety, and HAU, integrating them into public health policy.
Limitations
This is a longitudinal cohort study based solely on youth clinical reports of ShSTB, MDDS, violence, mental health symptomatology, and HAU. It has limitations in regard to the survey platform automatically eliminating respondents who fail to complete the screening. Thus, we may consider that we only obtained response rates of clinical relevance, and it forces us to reflect on the bias entailed in working with young Mexican’s data who were really seeking psychological care. In this context, our conclusions’ extent exclusively to clinical samples highly motivated to receive psychoeducation or treatment and not from a representative sample of Mexican youths. To generalize our findings, we suggest collecting data from a randomized sample of young Mexicans who are not essentially seeking professional help. Nevertheless, our findings are an alert about how mental health professionals may be aware of violence, self-harm/suicide, mental health, and HAU relationship while screening several mental health risks in the primary care settings.
Another limitation is the one regarding the need to include a wide range of Mexicans while determining the policies and community programs that should be implemented in Mexico. Upcoming studies may consider obtaining sensitivity and specificity evaluation research on the validity of our scales. Confirming these psychometric assessment characteristics during the pandemic would help solve their possible limitations. This would prevent overestimation of symptoms and reports while replicating the models in future research.
Author Contributions
S.M.-C., G.B., R.R.-G., A.L.L.-F., and V.F.-R. contributed to the conceptualization, writing, data analysis, discussion, and data interpretation. All authors have read and agreed to the published version of the manuscript.
Funding
We are grateful to the National Autonomous University of Mexico (UNAM) for its support with the key DGAPA-IV300121, and for its support with the PASPA from DGAPA-UNAM program.
Institutional Review Board Statement
The protocol was approved with code FPSI/422/CEIP/157/2020 by the Institutional Review Board of Ethics Committee on Applied Research of the Psychology Faculty at the National Autonomous University of Mexico (UNAM).
Informed Consent Statement
Participants were told that findings would be used for epidemiological research and that they could refuse to comply with the data requests and drop out at any point in the study. Informed consent was obtained from all those involved in the study.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare that the research was conducted without commercial or financial relationships that could create a conflict of interest.
Appendix A

Table A1.
Factor loadings, standard errors (SE), and p-value (p) for the observed variables for each SEM variable.
Table A1.
Factor loadings, standard errors (SE), and p-value (p) for the observed variables for each SEM variable.
| Variables and Measuring Items | Loadings | SE | p< |
|---|---|---|---|
| ShSTB | |||
| Current extreme hopelessness | 0.903 | ||
| Extreme despair | 0.906 | 0.011 | 0.001 |
| Current thoughts of self-harm | 0.932 | 0.012 | 0.001 |
| Plans for self-harm | 0.882 | 0.015 | 0.001 |
| Acts of self-harm | 0.82 | 0.017 | 0.001 |
| Thoughts of suicide | 0.919 | 0.012 | 0.001 |
| Plans for suicide | 0.859 | 0.018 | 0.001 |
| Acts of suicide | 0.775 | 0.024 | 0.001 |
| Extreme lethargy without cause | 0.974 | 0.012 | 0.001 |
| Chronic pain without cause | 0.951 | 0.012 | 0.001 |
| MDDS | |||
| Current chronic pain with no apparent cause | 0.951 | ||
| Difficulty performing usual work | 0.982 | 0.009 | 0.001 |
| Difficulty performing usual schoolwork | 0.994 | 0.009 | 0.001 |
| Difficulty performing usual domestic activities | 0.962 | 0.009 | 0.001 |
| Difficulty performing usual social activities | 0.978 | 0.009 | 0.001 |
| Repeated self-medication for emotional distress | 0.621 | 0.033 | 0.001 |
| Marked distress | 0.941 | 0.01 | 0.001 |
| Repeated help-seeking | 0.692 | 0.022 | 0.001 |
| Suffering Interpersonal Violence | |||
| Have you been a victim of physical violence (been attacked, hit, slapped, kicked, beaten up)? | 0.967 | ||
| Have you been a victim of emotional violence (insults, humiliation, screaming, dismissing, being ignored, or similar experiences)? | 0.810 | 0.061 | 0.001 |
| Have you been a victim of sexual violence (unwanted touching, sexual act through force, or threat of harm to maintain unwanted sexual activity)? | 0.533 | 0.060 | 0.001 |
| Have you been a victim of sexual harassment (e.g., soliciting intimate/physical contact in exchange for academic or work achievements, experiencing continuous verbal-or-online threats)? | 0.515 | 0.050 | 0.001 |
| Have you been a victim of any of these violent situations: violent stealing, gun threats, kidnapping, extreme physical violence (complications or fractures), blackmailing? | 0.563 | 0.059 | 0.001 |
| Have any of your family experienced these violent situations: violent stealing, gun threats, kidnapping, extreme physical violence (complications or fractures), blackmailing, sexual abuse, homicide? | 0.501 | 0.046 | 0.001 |
| Have you witnessed any violent situation against others (e.g., kicking, threats, humiliations, etc.)? | 0.657 | 0.045 | 0.001 |
| Suffering Intimate Violence | |||
| Was this emotional abuse inflicted by a family member or your partner? | 0.846 | ||
| Was this sexual abuse inflicted by a family member or your partner? | 0.859 | 0.037 | 0.001 |
| Was the violence you observed inside your family (such as that inflicted by a father against their son, or by any person against your partner)? | 0.587 | 0.035 | 0.001 |
| Perpetrating Intimate Violence | |||
| Was this physical abuse inflicted on a family member? | 0.766 | ||
| Was this emotional abuse inflicted on a family member? | 0.882 | 0.074 | 0.001 |
| Perpetrating Interpersonal Violence | |||
| Have you perpetrated any physical violence (such as hitting, pushing, or pinching)? | 0.701 | ||
| Have you perpetrated any emotional violence (insults, humiliation, screaming, dismissing, or similar experiences)? | 0.919 | 0.072 | 0.001 |
| Have you perpetrated any sexual violence (unwanted touching, sexual act through force, or threat of harm to maintain unwanted sexual activity)? | 0.630 | 0.116 | 0.001 |
| Have you perpetrated any sexual harassment (such as soliciting intimate/physical contact in exchange for academic or work achievements, sexual insinuation to make others feel uncomfortable, repeated insinuations, despite the resistance of the other person, whether verbal or online)? | 0.472 | 0.121 | 0.001 |
| Depression | |||
| Sadness or depressed mood | 0.922 | ||
| Discouraged because of how things were going in your life | 0.871 | 0.026 | 0.001 |
| Loss of interest or pleasure | 0.922 | 0.032 | 0.001 |
| Feeling worthless or not good enough | 0.771 | 0.029 | 0.001 |
| Recurrent thoughts of death | 0.801 | 0.048 | 0.001 |
| Indecisiveness or diminished ability to concentrate | 0.888 | 0.038 | 0.001 |
| Significant weight loss when not dieting or weight gain | 0.866 | 0.042 | 0.001 |
| Insomnia or hypersomnia | 0.808 | 0.034 | 0.001 |
| Psychomotor agitation or retardation | 0.997 | 0.065 | 0.001 |
| Fatigue or loss of energy | 0.884 | 0.036 | 0.001 |
| Symptoms causing impairment in social, occupational, or other important areas of functioning | 0.822 | 0.032 | 0.001 |
| Anxiety | |||
| I have felt nervous or on edge | 0.826 | ||
| I have felt unable to control my worrying | 0.877 | 0.047 | 0.001 |
| I have felt so restless it was hard to keep still | 0.784 | 0.047 | 0.001 |
| I have had trouble relaxing | 0.870 | 0.048 | 0.001 |
| I have felt afraid something awful could happen | 0.731 | 0.050 | 0.001 |
| Reexperiencing | |||
| Repeated, disturbing, and unwanted memories of the stressful experience | 0.927 | ||
| Repeated, disturbing dreams of the stressful experience | 0.860 | 0.031 | 0.001 |
| Suddenly feeling or acting as if the stressful experience were actually happening again (as if you were actually back there reliving it) | 0.906 | 0.036 | 0.001 |
| Feeling very upset when something reminded you of the stressful experience | 0.934 | 0.024 | 0.001 |
| Having strong physical reactions when something reminded you of the stressful experience (such as heart pounding, trouble breathing, sweating) | 0.889 | 0.035 | 0.001 |
| Avoidance | |||
| Avoiding memories, thoughts, or feelings related to the stressful experience | 0.956 | ||
| Avoiding external reminders of the stressful experience (such as people, places, conversations, activities, objects, or situations) | 0.934 | 0.023 | 0.001 |
| NACM | |||
| Trouble remembering important parts of the stressful experience | 0.857 | ||
| Having strong negative beliefs about yourself, other people, or the world (for example, having thoughts such as I am bad, there is something seriously wrong with me, no-one can be trusted, the world is completely dangerous) | 0.925 | 0.062 | 0.001 |
| Blaming yourself or someone else for the stressful experience or what happened after it | 0.912 | 0.045 | 0.001 |
| Having strong negative feelings such as fear, horror, anger, guilt, or shame | 0.946 | 0.061 | 0.001 |
| Loss of interest in activities you used to enjoy | 0.909 | 0.058 | 0.001 |
| Feeling distant or cut off from other people | 0.923 | 0.055 | 0.001 |
| Trouble experiencing positive feelings (for example, being unable to feel happiness or have loving feelings for people close to you | 0.899 | 0.047 | 0.001 |
| Hyperarousal | |||
| Irritable behavior, angry outbursts, or acting aggressively | 0.913 | ||
| Taking too many risks or doing things that could cause you harm | 0.859 | 0.031 | 0.001 |
| Being “hyperalert” or watchful or on guard | 0.852 | 0.035 | 0.001 |
| Feeling jumpy or easily startled | 0.926 | 0.045 | 0.001 |
| Having difficulty concentrating | 0.903 | 0.055 | 0.001 |
| Trouble falling or staying asleep | 0.893 | 0.047 | 0.001 |
| Alcoholic beverages (beer, wine, spirits). In the past three months… | |||
| How often have you consumed alcoholic beverages (beer, wine, spirits)? | 0.594 | ||
| How often have you had a strong desire or urge to use alcoholic beverages (beer, wine, spirits)? | 0.828 | 0.197 | 0.001 |
| How often has your use of alcoholic beverages (beer, wine, spirits) led to health, social, legal, or financial problems? | 0.533 | 0.174 | 0.001 |
| How often have you failed to do what was normally expected of you because of your use of alcoholic beverages (beer, wine, spirits)? | 0.531 | 0.233 | 0.001 |
| Has a friend or relative or anyone else ever expressed concern about your use of alcoholic beverages (beer, wine, spirits)? | 0.523 | 0.116 | 0.001 |
| Have you ever tried to cut down on alcoholic beverages (beer, wine, spirits) but failed? | 0.499 | 0.160 | 0.001 |
Note. Adapted with permission from Morales-Chainé et al. [4]. ShSTB—Current Self-harm and Suicide Thoughts and Behaviors; MDDS—Marked Distress, Dysfunction, and Somatization; NACM—Negative Alterations in Cognitions and Mood.
Appendix B

Table A2.
Chi-square analysis, degrees of freedom, p-values, fit indices, and Cronbach’s alpha by scales for the total group of participants.
Table A2.
Chi-square analysis, degrees of freedom, p-values, fit indices, and Cronbach’s alpha by scales for the total group of participants.
| Scales | X2 | df | p≤ | RMSEA | Confidence Interval | SRMR | CFI | TLI | Cronbach’s Alpha |
|---|---|---|---|---|---|---|---|---|---|
| ShSTB | 447.803 | 33 | 0.001 | 0.071 | 0.065–0.077 | 0.991 | 0.988 | 0.90 | |
| PShTB | 0.000 | 0 | 0.001 | 0.000 | 0.000–0.000 | 1.000 | 1.000 | 0.84 | |
| MDDS | 65.216 | 20 | 0.001 | 0.030 | 0.022–0.038 | 1.000 | 1.000 | 0.90 | |
| Suicide | 2289.464 | 186 | 0.001 | 0.067 | 0.065–0.070 | 0.993 | 0.992 | 0.94 | |
| LEC-5 Suffering Intimate Violence | 0.776 | 2 | 0.678 | 0.000 | 0.000–0.030 | 1.000 | 1.000 | 0.54 | |
| LEC-5 Suffering Interpersonal Violence | 103.717 | 13 | 0.001 | 0.053 | 0.044–0.063 | 0.961 | 0.937 | 0.62 | |
| LEC-5 Perpetrating Intimate Violence | 0.000 | 0 | 0.001 | 0.000 | 0.000–0.000 | 1.000 | 1.000 | 0.41 | |
| LEC-5 Perpetrating Interpersonal Violence | 0.010 | 1 | 0.922 | 0.000 | 0.000–0.019 | 1.000 | 1.000 | 0.38 | |
| LEC-5 Violence | 1359.011 | 113 | 0.001 | 0.067 | 0.063–0.070 | 0.979 | 0.975 | 0.80 | |
| MDE Depression | 597.594 | 41 | 0.001 | 0.074 | 0.069–0.079 | 0.016 | 0.982 | 0.976 | 0.97 |
| GA Anxiety | 56.221 | 5 | 0.001 | 0.064 | 0.050–0.080 | 0.008 | 0.995 | 0.99 | 0.93 |
| PCL-5 Reexperiencing | 29.024 | 4 | 0.001 | 0.05 | 0.034–0.068 | 0.004 | 0.998 | 0.996 | 0.96 |
| PCL-5 NACM | 110.007 | 10 | 0.001 | 0.063 | 0.053–0.074 | 0.006 | 0.996 | 0.991 | 0.97 |
| PCL-5 Hyperarousal | 54.580 | 6 | 0.001 | 0.057 | 0.044–0.071 | 0.005 | 0.997 | 0.993 | 0.96 |
| PCL-5 PTSD | 2381.298 | 152 | 0.001 | 0.077 | 0.074–0.080 | 0.019 | 0.971 | 0.964 | 0.99 |
| ASSIST Once in Lifetime | 100.478 | 27 | 0.001 | 0.033 | 0.026–0.040 | 0.972 | 0.963 | 0.61 | |
| ASSIST Tobacco | 39.777 | 4 | 0.001 | 0.060 | 0.044–0.078 | 0.016 | 0.992 | 0.980 | 0.81 |
| ASSIST Alcohol | 61.401 | 8 | 0.001 | 0.052 | 0.040–0.064 | 0.020 | 0.985 | 0.972 | 0.77 |
| ASSIST Cannabis | 81.898 | 8 | 0.001 | 0.061 | 0.049–0.073 | 0.019 | 0.988 | 0.977 | 0.85 |
| ASSIST Cocaine | 64.227 | 5 | 0.001 | 0.069 | 0.055–0.085 | 0.019 | 0.994 | 0.982 | 0.88 |
| ASSIST Stimulants | 41.037 | 4 | 0.001 | 0.061 | 0.045–0.079 | 0.006 | 0.997 | 0.990 | 0.94 |
| ASSIST Inhalants | 22.186 | 6 | 0.001 | 0.033 | 0.019–0.048 | 0.011 | 0.998 | 0.994 | 0.83 |
| ASSIST Sedatives | 41.584 | 5 | 0.001 | 0.054 | 0.040–0.070 | 0.014 | 0.994 | 0.982 | 0.85 |
| ASSIST Hallucinogens | 53.113 | 7 | 0.001 | 0.051 | 0.039–0.065 | 0.018 | 0.990 | 0.979 | 0.81 |
| ASSIST Other | 38.811 | 5 | 0.001 | 0.052 | 0.038–0.068 | 0.016 | 0.995 | 0.985 | 0.85 |
Note. Adapted with permission from Morales-Chainé et al. [4]. ShSTB—Current Self-harm and Suicide Thoughts and Behaviors; PShTB—Previous Self-harm Thoughts and Behaviors; MDDS—Marked Distress, Dysfunction, and Somatization; LEC-5—Life Events Checklist, MDE—Major Depressive Episode, GA—Generalized Anxiety, PCL-5—Posttraumatic Checklist, NACM—Negative Alterations in Cognitions and Mood, PTSD—Post-traumatic Stress Disorder, ASSIST—Alcohol, Smoking, and Substance Involvement Screening Test. Categorical variables do not show SRMR as Li (2021) recommended [31].
References
- mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP)—Version 2.0; World Health Organization: Geneva, Switzerland, 2016.
- World Health Organization. Suicide. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 15 June 2025).
- Pan American Health Organization. Burden of Suicide; Level by Country. 2020. Available online: https://www.paho.org/en/enlace/burden-suicide (accessed on 15 June 2025).
- Morales-Chainé, S.; Palafox-Palafox, G.; Robles-García, R.; Arenas-Landgrave, P.; López-Montoya, A.; Félix-Romero, A.; Imaz-Gispert, M. Pathways of depressive symptoms to self-harm and suicide warning signs during COVID-19 pandemic: The role of anxiety and related distress, dysfunction, and somatization. J. Affect. Disord. 2024, 35, 476–484. [Google Scholar] [CrossRef]
- World Health Organization. Youth Violence. 2024. Available online: https://apps.who.int/violence-info/youth-violence/ (accessed on 15 June 2025).
- United Nations Office on Drugs and Crime. UNODC Research—Data Portal—Violent and Sexual Crime. 2022. Available online: https://dataunodc.un.org/dp-crime-violent-offences (accessed on 15 June 2025).
- Morales-Chainé, S.; Bacigalupe, G.; Robles-García, R.; López-Montoya, A.; Félix-Romero, V.; Imaz-Gispert, M.A. Interpersonal and intimate violence in Mexican youth: Drug use, depression, anxiety, and stress during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 6484. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Reviewed, 5th ed.; USA Psychiatry Association: Washington, DC, USA, 2022. [Google Scholar]
- World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact. 2022. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (accessed on 15 June 2025).
- Pan American Health Organization. The Burden of Mental Disorders in the Region of the Americas, 2000–2019. 2021. Available online: https://www.paho.org/en/enlace/burden-mental-disorders (accessed on 15 June 2025).
- World Health Organization. Alcohol. 2024. Available online: https://www.who.int/health-topics/alcohol#tab=tab_1 (accessed on 15 June 2025).
- National Institute of Psychiatry Ramón de la Fuente Muñiz. National Report of Alcohol and Tobacco. 2016–2017; Encuesta Nacional de Consumo de Drogas, Alcohol y Tabaco, ENCODAT 2016–2017|Comisión Nacional contra las Adicciones|Gobierno|gob.mx. Available online: www.gob.mx (accessed on 15 June 2025).
- Clare, C.A.; Velasquez, G.; Martorell, G.M.M.; Fernandez, D.; Dinh, J.; Montague, A. Risk factors for male perpetration of intimate partner violence: A review. Aggress. Violent Behav. 2021, 56, 101532. [Google Scholar] [CrossRef]
- Rooney, E.E.; Hill, R.M.; Oosterhoff, B.; Kaplow, J.B. Violent victimization and perpetration as distinct risk factors for adolescent suicide attempts. Child. Health Care 2019, 48, 10–427. [Google Scholar] [CrossRef]
- Yu, Z.; Zhu, X. The association between victimization experiences and suicidality: The mediating roles of sleep and depression. J. Affect. Discorder 2023, 329, 243–250. [Google Scholar] [CrossRef]
- Aloyce, D.; Stökkl, H.; Mosha, N.; Malibwa, S.; Hashim, R.; Ayieko, P.; Hapiga, S.; Mshana, G. The association between depression, suicidal thoughts and intimate partner violence perpetration among young men in Mwanza, Tanzania. J. Fam. Violence 2024, 1–13. [Google Scholar] [CrossRef]
- Benatov, J.; Brunstein, K.A.; Chen-Gal, S. Bullying perpetration and victimization associations to suicide behavior: A longitudinal study. Eur. Child Adolesc. Psychiatry 2022, 31, 1353–1360. [Google Scholar] [CrossRef]
- Berny, L.M.; Tanner-Smith, E.E. Interpersonal violence and suicide risk: Ecamining buffering effects of school and Community connectedness. Child. Youth Serv. Rev. 2024, 157, 107405. [Google Scholar] [CrossRef]
- Mueller-Williams, A.C.; Ilgen, M.A.; Hicks, B.M. Characteristics of people who report firearm suicidal ideation in the USA. BMJ J. 2024. ahead of print. [Google Scholar] [CrossRef]
- Serafini, G.; Aguglia, A.; Amerio, A.; Canepa, G.; Adavastro, G.; Conigliaro, C.; Nebbia, J.; Franchi, L.; Flouri, E.; Amore, M. The relationship between bullying victimization and perpetration and non-suicidal self-injury: A systematic review. Child Psychiatry Hum. Dev. 2023, 54, 154–175. [Google Scholar] [CrossRef]
- Wolford-Clevenger, C.; Brem, M.J.; Zapor, H.; Elmquist, J.; Stuart, G.L. Prevalence, severity, and correlates of suicidal ideation among men and women in batterer intervention programs. Partn. Abus. 2017, 8, 190–203. [Google Scholar] [CrossRef]
- Kafka, J.M.; Moracco, K.E.; Taheri, C.; Young, B.; Graham, L.M.; Macy, R.J.; Proescholdbell, S. Intimate partner violence victimization and perpetration as precursors to suicide. SSM-Popul. Health 2022, 18, 101079. [Google Scholar] [CrossRef]
- Sesar, K.; Dodaj, A.; Simi’c, N. Mental health of perpetrators of intimate partner violence. Ment. Health Rev. J. 2018, 23, 221–239. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of web surveys: The checklist for reporting results of internet W-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Life Events Checklist for DSM-5 (LEC.5)-Standard. [Measurement Instrument]. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/documents/LEC5_Extended_Self-report.PDF (accessed on 15 June 2025).
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5)—LEC-5 and Extended Criterion A [Measurement Instrument]. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 15 June 2025).
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD CheckList for DSM-5 (PCL-5)-Standard. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.PDF (accessed on 15 June 2025).
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Reed, G.M.; Robles, R.; Minhas, F.; Razzaque, B.; Fortés, S.; Mari, J.J.; Lam, T.P.; García, J.A.; Gask, L.; et al. Screening for anxiety, depression, and anxious depression in primary care: A field study for ICD-11 PHC. J. Affect. Disord. 2017, 213, 199–206. [Google Scholar] [CrossRef]
- World Health Organization. The Alcohol, Smoking and Substance Involvement Screening Test: Manual for Use in Primary Care. 2010. Available online: https://www.who.int/publications/i/item/978924159938-2 (accessed on 15 June 2025).
- Li, C. Statistical estimation of structural equation models with a mixture of continuous and categorical observed variables. Behav. Res. Methods 2021, 53, 2191–2213. [Google Scholar] [CrossRef]
- West, S.G.; Wu, W.; McNeish, D.; Savord, A. Model fit in structural equation modeling. In Handbook of Structural Equation Modeling; Hoyle, R.H., Ed.; Guilford Press: New York, NY, USA, 2023; pp. 184–205. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. 2018. Available online: https://www.R-project.org (accessed on 15 June 2025).
- IBM Corp. Released. IBM SPSS Statistics for Windows, Version 25.0; IBM Corp.: Armonk, NY, USA, 2017.
- King, C.D.; Joyce, V.W.; Nash, C.C.; Buonopane, R.J.; Black, J.M.; Zuromski, K.L.; Milner, A.J. Fear of sleep and sleep quality mediate the relationship between trauma exposure and suicide attempt in adolescents. J. Psychiatr. Res. 2021, 135, 243–247. [Google Scholar] [CrossRef]
- Dewar, C.; Heggs, D.A.; Davies, J. Exploring the relationship between domestic violence perpetration and suicidal behavior in male prisoners. Arch. Suicide Res. 2021, 26, 1831–1846. [Google Scholar] [CrossRef]
- Klonsky, E.D.; Pachkowski, M.C.; Shahnaz, A.; May, A.M. The three-step theory of suicide: Description, evidence, and some useful points of clarification. Prev. Med. 2021, 152 Pt 1, 106549. [Google Scholar] [CrossRef]
- Oram, S.; Fisher, H.L.; Minnis, H.; Seedat, S.; Walby, S.; Hegarty, K.; Rouf, K.; Angénieux, C.; Callard, F.; Chandra, P.S.; et al. The Lancet Psychiatry Commission on intimate partner violence and mental health: Advancing mental health services, research, and policy. Lancet Psychiatry 2022, 9, 487–524. [Google Scholar] [CrossRef]
- Alexander, E.F.; Johnson, M.D. On categorizing intimate partner violence: A systematic review of exploratory clustering and classification studies. J. Fam. Psychol. 2023, 37, 743–752. Available online: https://psycnet.apa.org/doi/10.1037/fam0001075 (accessed on 15 June 2025). [CrossRef]
- Kourti, A.; Stavridou, A.; Panagouli, E.; Psaltopoulou, T.; Spiliopoulou, C.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Domestic violence during the COVID-19 pandemic: A systematic review. Trauma Violence Abus. 2023, 24, 719–745. [Google Scholar] [CrossRef]
- Scott-Storey, K.; O’Donnell, S.; Ford-Gilboe, M.; Varcoe, C.; Wachen, N.; Malcolm, J.; Vincent, C. What about the men? A critical review of men’s experiences of intimate partner violence. Trauma Violence Abus. 2023, 24, 858–872. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).