What Is the Impact of Unemployment as an Adverse Experience? Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: A Meta-Analysis
Abstract
1. Introduction
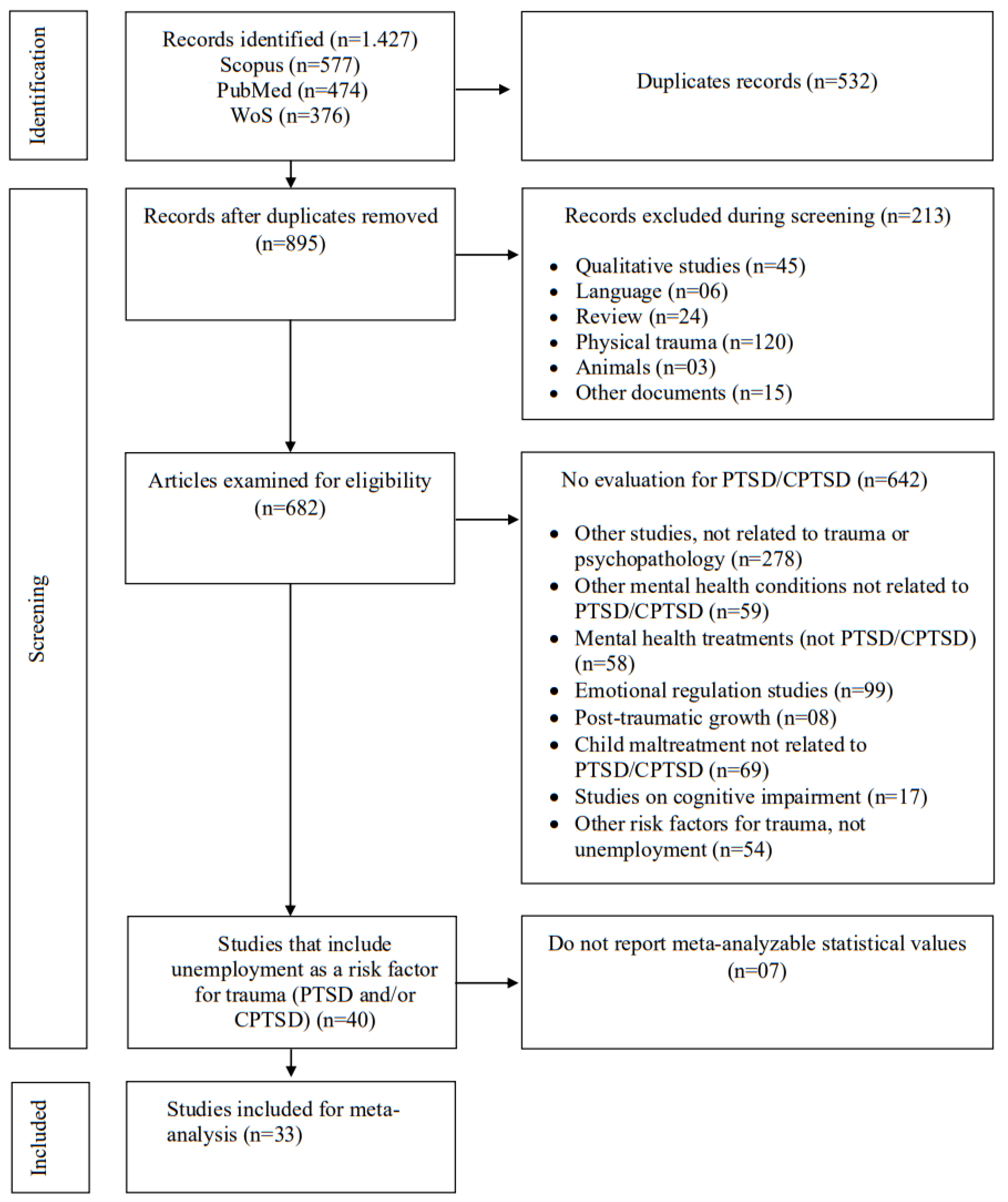
2. Search Strategy
3. Inclusion and Exclusion Criteria
4. Quality Assessment
5. Data Extraction
6. Statistical Analysis
7. Results
8. Quality Assessment
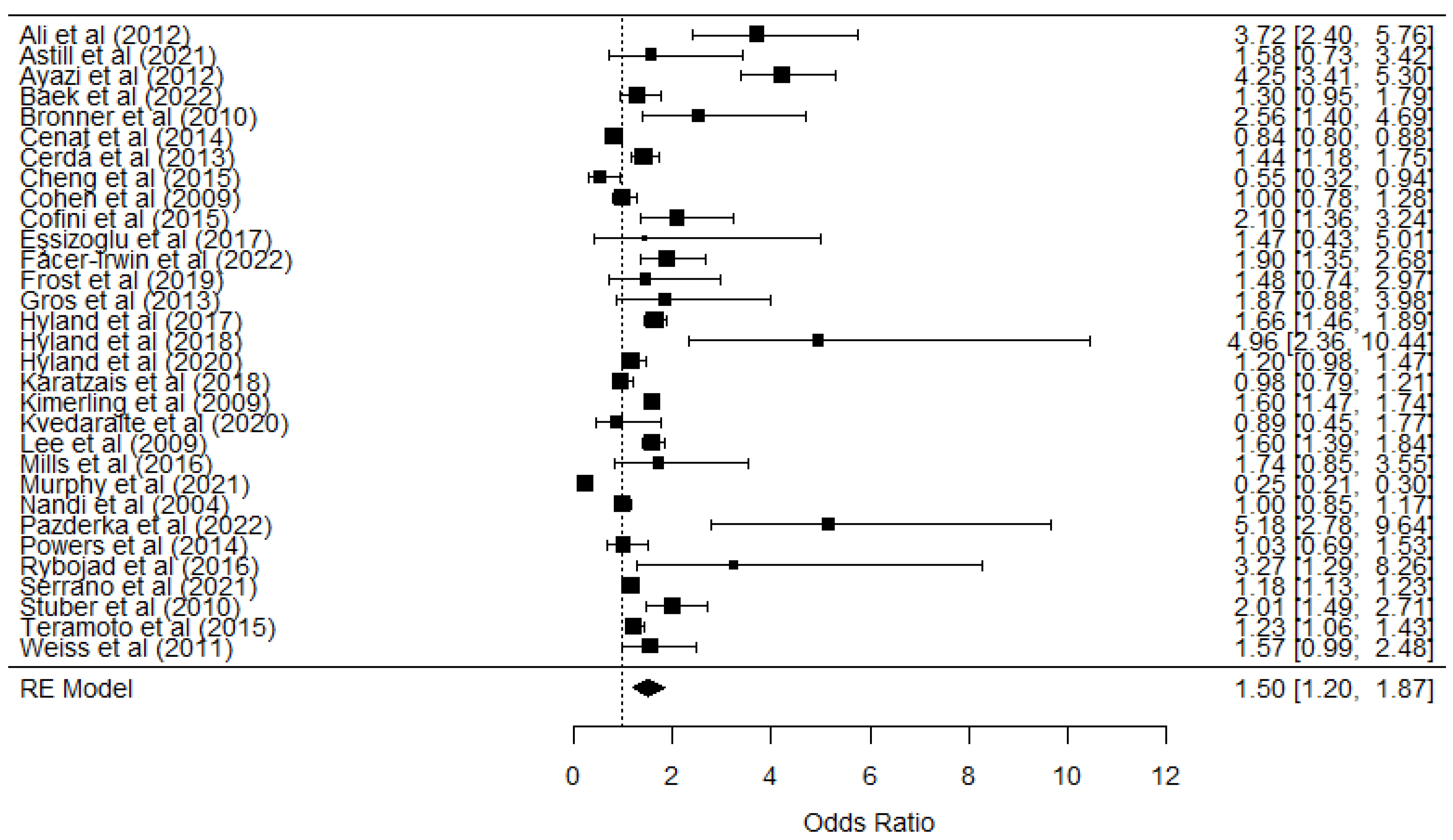
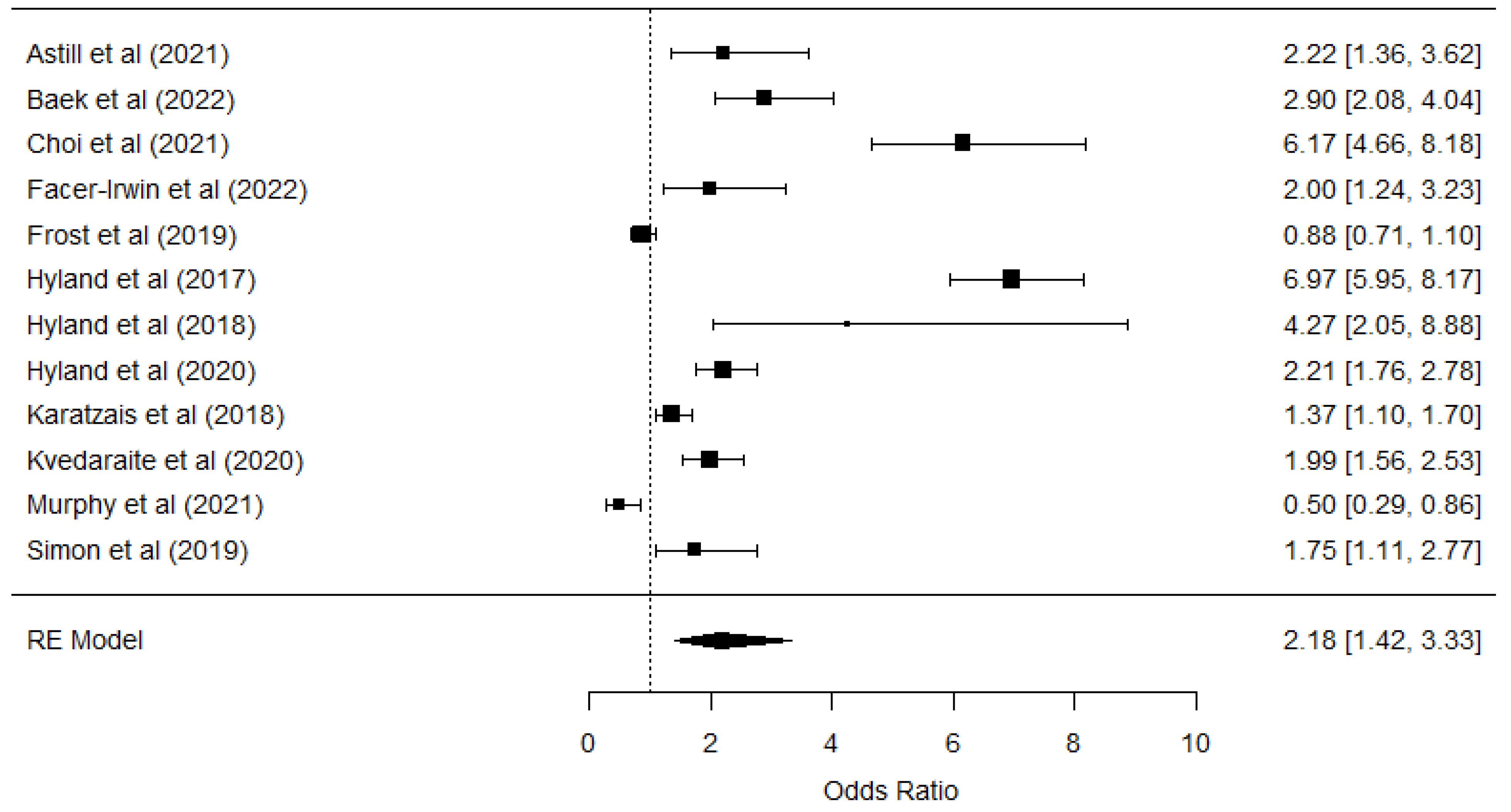
9. Meta-Analysis
10. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Arena, A.F.; Mobbs, S.; Sanatkar, S.; Williams, D.; Collins, D.; Harris, M.; Harvey, S.B.; Deady, M. Mental health and unemployment: A systematic review and meta-analysis of interventions to improve depression and anxiety outcomes. J. Affect. Disord. 2023, 335, 450–472. [Google Scholar] [CrossRef] [PubMed]
- Paul, K.I.; Batinic, B. The need for work: Jahoda’s latent functions of employment in a representative sample of the German population. J. Organ. Behav. 2010, 31, 45–64. [Google Scholar] [CrossRef]
- Nam, G.E.; Eum, M.-J.; Huh, Y.; Jung, J.H.; Choi, M.-J. The Association Between Employment Status and Mental Health in Young Adults: A Nationwide Population-Based Study in Korea. J. Affect. Disord. 2021, 295, 1184–1189. [Google Scholar] [CrossRef]
- Jebb, A.T.; Morrison, M.; Tay, L.; Diener, E. Subjective Well-Being Around the World: Trends and Predictors Across the Life Span. Psychol. Sci. 2020, 31, 293–305. [Google Scholar] [CrossRef]
- Bartelink, V.H.M.; Ya, K.Z.; Guldbrandsson, K.; Bremberg, S. Unemployment among young people and mental health: A systematic review. Scand. J. Public Health 2019, 48, 544–558. [Google Scholar] [CrossRef]
- World Bank. World Health Organization Global Health Expenditure Database. Available online: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS (accessed on 26 March 2025).
- Ahammer, A.; Packham, A. Effects of unemployment insurance duration on mental and physical health. J. Public Econ. 2023, 226, 104996. [Google Scholar] [CrossRef]
- Drydakis, N. The effect of unemployment on self-reported health and mental health in Greece from 2008 to 2013: A longitudinal study before and during the financial crisis. Soc. Sci. Med. 2015, 128, 43–51. [Google Scholar] [CrossRef]
- Gedikli, C.; Miraglia, M.; Connolly, S.; Bryan, M.; Watson, D. The relationship between unemployment and wellbeing: An updated meta-analysis of longitudinal evidence. Eur. J. Work Organ. Psychol. 2023, 32, 128–144. [Google Scholar] [CrossRef]
- Murphy, B.A. The Griffith Empathy Measure Does Not Validly Distinguish between Cognitive and Affective Empathy in Children. Aust. Psychol. 2019, 54, 159–164. [Google Scholar] [CrossRef]
- Stolove, C.A.; Galatzer-Levy, I.R.; Bonanno, G.A. Emergence of depression following job loss prospectively predicts lower rates of reemployment. Psychiatry Res. 2017, 253, 79–83. [Google Scholar] [CrossRef]
- Olesen, S.C.; Butterworth, P.; Leach, L.S.; Kelaher, M.; Pirkis, J. Mental health affects future employment as job loss affects mental health: Findings from a longitudinal population study. BMC Psychiatry 2013, 13, 144. [Google Scholar] [CrossRef] [PubMed]
- Nurmela, K.; Mattila, A.; Heikkinen, V.; Uitti, J.; Ylinen, A.; Virtanen, P. Identification of depression and screening for work disabilities among long-term unemployed people. Int. J. Environ. Res. Public Health 2018, 15, 909. [Google Scholar] [CrossRef] [PubMed]
- McKee-Ryan, F.; Song, Z.; Wanberg, C.R.; Kinicki, A.J. Psychological and physical well-being during unemployment: A meta-analytic study. J. Appl. Psychol. 2005, 90, 53–76. [Google Scholar] [CrossRef] [PubMed]
- Steed, L.B.; Swider, B.W.; Keem, S.; Liu, J.T. Leaving Work at Work: A Meta-Analysis on Employee Recovery from Work. J. Manag. 2021, 47, 867–897. [Google Scholar] [CrossRef]
- Dorahy, M.J.; Corry, M.; Shannon, M.; MacSherry, A.; Hamilton, G.; McRobert, G.; Elder, R.; Hanna, D. Complex PTSD, interpersonal trauma and relational consequences: Findings from a treatment-receiving Northern Irish sample. J. Affect. Disord. 2009, 112, 71–80. [Google Scholar] [CrossRef]
- Frost, R.; Vang, M.L.; Karatzias, T.; Hyland, P.; Shevlin, M. The distribution of psychosis, ICD-11 PTSD and complex PTSD symptoms among a trauma-exposed UK general population sample. Psychosis 2019, 11, 187–198. [Google Scholar] [CrossRef]
- Bruya, B.; Tang, Y.-Y. Is attention really effort? Revisiting Daniel Kahneman’s influential 1973 book attention and effort. Front. Psychol. 2018, 9, 1133. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Leiva-Bianchi, M.; Nvo-Fernandez, M.; Villacura-Herrera, C.; Miño-Reyes, V.; Varela, N.P. What are the predictive variables that increase the risk of developing a complex trauma? A meta-analysis. J. Affect. Disord. 2023, 343, 153–165. [Google Scholar] [CrossRef]
- Serrano, C.; Leiva-Bianchi, M.; Ahumada, F.; Araque-Pinilla, F. What is the association between post-traumatic stress disorder and unemployment after A disaster? Int. J. Occup. Med. Environ. Health 2021, 34, 755–766. [Google Scholar] [CrossRef]
- Wong, P.T.P. Existential positive psychology and integrative meaning therapy. Int. Rev. Psychiatry 2020, 32, 565–578. [Google Scholar] [CrossRef]
- Burgard, S.A.; Kalousova, L. Effects of the Great Recession: Health and Well-Being. Annu. Rev. Sociol. 2015, 41, 181–201. [Google Scholar] [CrossRef]
- Patel, R.; Spreng, R.N.; Shin, L.M.; Girard, T.A. Neurocircuitry models of posttraumatic stress disorder and beyond: A meta-analysis of functional neuroimaging studies. Neurosci. Biobehav. Rev. 2012, 9, 2130–2142. [Google Scholar]
- Patel, V.; Burns, J.K.; Dhingra, M.; Tarver, L.; Kohrt, B.A.; Lund, C. Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry 2018, 17, 76–89. [Google Scholar] [PubMed]
- Barbalat, G.; Franck, N. Ecological study of the association between mental illness with human development, income inequalities and unemployment across OECD countries. BMJ Open 2020, 10, e035055. [Google Scholar] [CrossRef]
- Johnson, S.L.; Wibbels, E.; Wilkinson, R. Economic inequality is related to cross-national prevalence of psychotic symptoms. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1799–1807. [Google Scholar] [CrossRef]
- Riumallo-Herl, C.; Basu, S.; Stuckler, D.; Courtin, E.; Avendano, M. Job loss, wealth and depression during the Great Recession in the USA and Europe. Int. J. Epidemiol. 2014, 43, 1508–1517. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Thelwall, M. Early Mendeley readers correlate with later citation counts. Scientometrics 2018, 115, 1231–1240. [Google Scholar] [CrossRef]
- Villacura-Herr, C.; Kenner, N. rESCMA: A brief summary on effect size conversion for meta-analysis. arXiv 2020. [Google Scholar] [CrossRef]
- Riley, R.D.; Higgins, J.P.T.; Deeks, J.J. Interpretation of random effects meta-analyses. BMJ 2011, 342, d549. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Viechtbauer, W.; Cheung, M.W.-L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 2010, 1, 112–125. [Google Scholar] [CrossRef]
- Solt, F. Measuring Income Inequality Across Countries and over Time: The Standardized World Income Inequality Database. Soc. Sci. Q. 2020, 101, 1183–1199. [Google Scholar] [CrossRef]
- Ferguson, C.J. An Effect Size Primer: A Guide for Clinicians and Researchers. Prof. Psychol. Res. Pract. 2009, 40, 532–538. [Google Scholar] [CrossRef]
- Sedgwick, P. Meta-analyses: What is heterogeneity? BMJ 2015, 350, h1435. [Google Scholar]
- Ali, M.; Farooq, N.; Bhatti, M.A.; Kuroiwa, C. Assessment of prevalence and determinants of posttraumatic stress disorder in survivors of earthquake in Pakistan using Davidson trauma scale. J. Affect. Disord. 2012, 136, 238–243. [Google Scholar] [CrossRef]
- Wright, L.A.; Roberts, N.P.; Lewis, C.; Simon, N.; Hyland, P.; Ho, G.W.; McElroy, E.; Bisson, J.I. High prevalence of somatisation in ICD-11 complex PTSD: A cross sectional cohort study. J. Psychosom. Res. 2021, 148, 110574. [Google Scholar] [CrossRef]
- Ayazi, T.; Lien, L.; Eide, A.H.; Ruom, M.M.; Hauff, E. What Are the Risk Factors for the Comorbidity of Posttraumatic Stress Disorder and Depression in a War-Affected Population? A Cross-Sectional Community Study in South Sudan. 2012. Available online: http://www.biomedcentral.com/1471-244X/12/175 (accessed on 27 March 2025).
- Baek, J.; Kim, K.-A.; Kim, H.; Kim, O.; Ko, M.; Kim, S.H.; Sohn, I.B.; Shin, B.K.; Jeon, W.T.; Chu, S.H. The validity of ICD-11 PTSD and complex PTSD in North Korean defectors using the International Trauma Questionnaire. Eur. J. Psychotraumatology 2022, 13, 2119012. [Google Scholar] [CrossRef]
- Bronner, M.B.; Peek, N.; Knoester, H.; Bos, A.P.; Last, B.F.; Grootenhuis, M.A. Course and predictors of posttraumatic stress disorder in parents after pediatric intensive care treatment of their child. J. Pediatr. Psychol. 2010, 35, 966–974. [Google Scholar] [CrossRef]
- Cénat, J.M.; Derivois, D. Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adults survivors of earthquake in Haiti after 30 months. J. Affect. Disord. 2014, 159, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Cerdá, M.; Paczkowski, M.; Galea, S.; Nemethy, K.; Péan, C.; Desvarieux, M. Psychopathology in the aftermath of the Haiti earthquake: A population-based study of posttraumatic stress disorder and major depression. Depress. Anxiety 2013, 30, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Ma, N.; Yang, L.; Agho, K.; Stevens, G.; Raphael, B.; Cui, L.; Liu, Y.; Yan, B.; Ma, H.; et al. Depression and posttraumatic stress disorder in temporary settlement residents 1 year after the sichuan earthquake. Asia Pac. J. Public Health 2015, 27, NP1962–NP1972. [Google Scholar] [CrossRef]
- Choi, H.; Lee, W.; Hyland, P. Factor structure and symptom classes of ICD-11 complex posttraumatic stress disorder in a South Korean general population sample with adverse childhood experiences. Child Abus. Negl. 2021, 114, 104982. [Google Scholar] [CrossRef]
- Cohen, M.H.; Fabri, M.; Cai, X.; Shi, Q.; Hoover, D.R.; Binagwaho, A.; Culhane, M.A.; Mukanyonga, H.; Karegeya, D.K.; Anastos, K. Prevalence and Predictors of Posttraumatic Stress Disorder and Depression in HIV-Infected and At-Risk Rwandan Women. J. Women’s Health 2009, 18, 1783–1791. [Google Scholar] [CrossRef]
- Cofini, V.; Carbonelli, A.; Cecilia, M.; Binkin, N.; di Orio, F. Post traumatic stress disorder and coping in a sample of adult survivors of the Italian earthquake. Psychiatry Res. 2015, 229, 353–358. [Google Scholar] [CrossRef]
- Eşsizoğlu, A.; Altınöz, A.E.; Sonkurt, H.O.; Kaya, M.C.; Köşger, F.; Kaptanoğlu, C. The risk factors of possible PTSD in individuals exposed to a suicide attack in Turkey. Psychiatry Res. 2017, 253, 274–280. [Google Scholar] [CrossRef]
- Facer-Irwin, E.; Karatzias, T.; Bird, A.; Blackwood, N.; MacManus, D. PTSD and complex PTSD in sentenced male prisoners in the UK: Prevalence, trauma antecedents, and psychiatric comorbidities. Psychol. Med. 2022, 52, 2794–2804. [Google Scholar] [CrossRef]
- Gros, D.F.; Price, M.; Yuen, E.K.; Acierno, R. Predictors of completion of exposure therapy in OEF/OIF veterans with posttraumatic stress disorder. Depress. Anxiety 2013, 30, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Hyland, P.; Murphy, J.; Shevlin, M.; Vallières, F.; McElroy, E.; Elklit, A.; Christoffersen, M.; Cloitre, M. Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 727–736. [Google Scholar] [CrossRef]
- Hyland, P.; Ceannt, R.; Daccache, F.; Daher, R.A.; Sleiman, J.; Gilmore, B.; Byrne, S.; Shevlin, M.; Murphy, J.; Vallières, F. Are posttraumatic stress disorder (PTSD) and complex-PTSD distinguishable within a treatment-seeking sample of Syrian refugees living in Lebanon? Glob. Ment. Health 2018, 5, e14. [Google Scholar] [CrossRef]
- Hyland, P.; Vallières, F.; Cloitre, M.; Ben-Ezra, M.; Karatzias, T.; Olff, M.; Murphy, J.; Shevlin, M. Trauma, PTSD, and complex PTSD in the Republic of Ireland: Prevalence, service use, comorbidity, and risk factors. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Karatzias, T.; Hyland, P.; Bradley, A.; Cloitre, M.; Roberts, N.P.; Bisson, J.I.; Shevlin, M. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: Findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress. Anxiety 2019, 36, 887–894. [Google Scholar] [CrossRef]
- Kimerling, R.; Alvarez, J.; Pavao, J.; Mack, K.P.; Smith, M.W.; Baumrind, N. Unemployment among women: Examining the relationship of physical and psychological intimate partner violence and posttraumatic stress disorder. J. Interpers. Violence 2009, 24, 450–463. [Google Scholar] [CrossRef]
- Kvedaraite, M.; Gelezelyte, O.; Kairyte, A.; Roberts, N.P.; Kazlauskas, E. Trauma exposure and factors associated with ICD-11 PTSD and complex PTSD in the Lithuanian general population. Int. J. Soc. Psychiatry 2022, 68, 1727–1736. [Google Scholar] [CrossRef]
- Lee, C.-S.; Chang, J.-C.; Liu, C.-Y.; Chang, C.-J.; Chen, T.H.H.; Chen, C.-H.; Cheng, A.T.A. Acculturation, psychiatric comorbidity and posttraumatic stress disorder in a Taiwanese aboriginal population. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 55–62. [Google Scholar] [CrossRef]
- Mills, K.L.; Barrett, E.L.; Merz, S.; Rosenfeld, J.; Ewer, P.L.; Sannibale, C.; Baker, A.L.; Hopwood, S.; Back, S.E.; Brady, K.T.; et al. Integrated exposure-based therapy for co-occurring post traumatic stress disorder (PTSD) and substance dependence: Predictors of change in PTSD symptom severity. J. Clin. Med. 2016, 5, 101. [Google Scholar] [CrossRef]
- Murphy, D.; Karatzias, T.; Busuttil, W.; Greenberg, N.; Shevlin, M. ICD-11 posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) in treatment seeking veterans: Risk factors and comorbidity. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1289–1298. [Google Scholar] [CrossRef]
- Nandi, A.; Galea, S.; Tracy, M.; Ahern, J.; Resnick, H.; Gershon, R.; Vlahov, D. Job loss, unemployment, work stress, job satisfaction, and the persistence of posttraumatic stress disorder one year after the september 11 attacks. J. Occup. Environ. Med. 2004, 46, 1057–1064. [Google Scholar] [CrossRef]
- Pazderka, H.; Shalaby, R.; Eboreime, E.; Mao, W.; Obuobi-Donkor, G.; Agyapong, B.; Oluwasina, F.; Adu, M.K.; Owusu, E.; Sapara, A.; et al. Isolation, Economic Precarity, and Previous Mental Health Issues as Predictors of PTSD Status in Females Living in Fort McMurray During COVID-19. Front. Psychiatry 2022, 13, 837713. [Google Scholar] [CrossRef]
- Powers, M.B.; Warren, A.M.; Rosenfield, D.; Roden-Foreman, K.; Bennett, M.; Reynolds, M.C.; Davis, M.L.; Foreman, M.L.; Petrey, L.B.; Smits, J.A. Predictors of PTSD symptoms in adults admitted to a Level I trauma center: A prospective analysis. J. Anxiety Disord. 2014, 28, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Rybojad, B.; Aftyka, A.; Baran, M.; Rzońca, P. Risk factors for posttraumatic stress disorder in Polish paramedics: A pilot study. J. Emerg. Med. 2016, 50, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Simon, N.; Roberts, N.P.; Lewis, C.E.; van Gelderen, M.J.; Bisson, J.I. Associations between perceived social support, posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD): Implications for treatment. Eur. J. Psychotraumatology 2019, 10, 1573129. [Google Scholar] [CrossRef]
- Stuber, M.L.; Meeske, K.A.; Krull, K.R.; Leisenring, W.; Stratton, K.; Kazak, A.E.; Huber, M.; Zebrack, B.; Uijtdehaage, S.H.; Mertens, A.C.; et al. Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics 2010, 125, e1124–e1134. [Google Scholar] [CrossRef]
- Teramoto, C.; Matsunaga, A.; Nagata, S. Cross-sectional study of social support and psychological distress among displaced earthquake survivors in Japan. Jpn. J. Nurs. Sci. 2015, 12, 320–329. [Google Scholar] [CrossRef]
- Weiss, T.; Skelton, K.; Phifer, J.; Jovanovic, T.; Gillespie, C.F.; Smith, A.; Umpierrez, G.; Bradley, B.; Ressler, K.J. Posttraumatic stress disorder is a risk factor for metabolic syndrome in an impoverished urban population. Gen. Hosp. Psychiatry 2011, 33, 135–142. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; Brewin, C.R.; Cloitre, M.; Downes, A.J.; Jumbe, S.; Karatzias, T.; Bisson, J.I.; Roberts, N.P. Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International Trauma Questionnaire. Acta Psychiatr. Scand. 2017, 136, 313–322. [Google Scholar] [CrossRef]
- Leiva-Bianchi, M.; Ahumada, F.; Araneda, A.; Botella, J. What is the Psychosocial Impact of Disasters? A Meta-Analysis. Issues Ment. Health Nurs. 2018, 39, 320–327. [Google Scholar] [CrossRef]
- Leiva-Bianchi, M.; Arellano, C.; Pardo, E.; Ahumada, F.; Amaya, I.; Antúnez, S.; Cáceres, C.; Salinas, M.; Serrano, C. Diseño y validación de una escala de impacto psicosocial de los desastres (SPSI-D). Rev. Sociol. 2019, 34, 21–42. [Google Scholar] [CrossRef]
- Krug, G.; Drasch, K.; Jungbauer-Gans, M. The social stigma of unemployment: Consequences of stigma consciousness on job search attitudes, behaviour and success. J. Labour Mark. Res. 2019, 53, 11. [Google Scholar] [CrossRef]
- Urbanos-Garrido, R.M.; Lopez-Valcarcel, B.G. The influence of the economic crisis on the association between unemployment and health: An empirical analysis for Spain. Eur. J. Health Econ. 2015, 16, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Miño-Reyes, V.; González-Cabeza, G.; Nvo-Fernández, M. Perspective Chapter: Silenced Voices—Childhood, Trauma, and Dissociation. In Post-Traumatic Stress Disorder—Latest Developments in Diagnosis, Causes, and Treatments; IntechOpen: London, UK, 2024. [Google Scholar] [CrossRef]
- Pickett, K.E.; Wilkinson, R.G. Income inequality and health: A causal review. Soc. Sci. Med. 2015, 128, 316–326. [Google Scholar] [PubMed]
- Frasquilho, D.; Matos, M.; Salonna, F.; Guerreiro, D.; Storti, C.S.; Gaspar, T.; Caldas-de-Almeida, J.M. Mental health outcomes in times of economic recession: A systematic literature review Health behavior, health promotion and society. BMC Public Health 2015, 16, 115. [Google Scholar] [CrossRef]
- Dokkedahl, S.B.; Vang, M.L.; Elklit, A. Does tonic immobility mediate the effects of psychological violence on PTSD and complex PTSD? Eur. J. Trauma Dissociation 2022, 6, 100297. [Google Scholar] [CrossRef]
- Lonergan, M. Cognitive behavioral therapy for PTSD: The role of complex PTSD on treatment outcome. J. Aggress. Maltreat. Trauma 2014, 23, 494–512. [Google Scholar]
- Caddick, N.; Smith, B.; Phoenix, C. Male combat veterans’ narratives of PTSD, masculinity, and health. Sociol. Health Illn. 2015, 1, 97–111. [Google Scholar]
- Kairyte, A.; Kvedaraite, M.; Kazlauskas, E.; Gelezelyte, O. Exploring the links between various traumatic experiences and ICD-11 PTSD and Complex PTSD: A cross-sectional study. Front. Psychol. 2022, 13, 896981. [Google Scholar] [CrossRef]
- Liberzon, I.; Sripada, C.S. The functional neuroanatomy of PTSD: A critical review. Prog. Brain. Res. 2008, 167, 151–169. [Google Scholar] [CrossRef]
- Korn, D.L. EMDR and the Treatment of Complex PTSD: A Review. J. EMDR Pract. Res. 2009, 3, 264–278. [Google Scholar] [CrossRef]
| Scopus | TITLE (“complex PTSD” OR “complex posttraumatic stress disorder” OR “CPTSD” OR “PTSD” OR “posttraumatic stress disorder”) AND TITLE (“risk factors” OR “predictors” OR “unemployment”). |
| Web of Sciences | TI = ((“complex PTSD” OR “complex posttraumatic stress disorder” OR “CPTSD” OR “PTSD” OR “posttraumatic stress disorder”) AND (“risk factors” OR “predictors” OR “unemployment”)) |
| PubMed | ((“complex PTSD”[Title] OR “complex posttraumatic stress disorder”[Title] OR “CPTSD”[Title] OR “PTSD”[Title] OR “posttraumatic stress disorder”[Title]) AND (“risk factors”[Title] OR “predictors”[Title] OR “unemployment”[Title])) |
| ID | Authors | Design | Sample Type | N | % Female | Age (M ± SD) | N Unemp | Identification of PTSD/CPTSD |
|---|---|---|---|---|---|---|---|---|
| 01 | Ali et al. (2012) [39] | Cross-sectional | Survivors | 300 | 39.3% | 37.8 ± 14.0 | 234 | Davidson Trauma Scale |
| 02 | Wright et al. (2021) [40] | Cross-sectional | General | 222 | - | 16 | 137 | International Trauma Questionnaire (ITQ) |
| 03 | Ayazi et al. (2012) [41] | Cross-sectional | General | 1200 | 44% | - | 111 | Harvard Trauma Questionnaire (HTQ) |
| 04 | Baek et al. (2022) [42] | Cross-sectional | Defectors | 503 | 84.5% | 46 ± 13.2 | - | International Trauma Questionnaire (ITQ) |
| 05 | Bronner et al. (2010) [43] | Longuitudinal | Clinical | 588 | 56.8% | 36.5 ± 7.0 | 150 | Self-Rating Scale for PTSD (SRS-PTSD) |
| 06 | Cénat et al. (2014) [44] | Cross-sectional | General | 1355 | 48.7% | 31.57 | 221 | Impact of Event Scale—Revised (IES-R) |
| 07 | Cerdá et al. (2013) [45] | Cross-sectional | General | 1315 | 71.1% | - | - | Lifetime Violent Traumatic Event Experience |
| 08 | Cheng et al. (2015) [46] | Cross-sectional | Survivors | 182 | 65.2% | - | 88 | Structured Clinical Interview for DSM-IV Axis I Disorders |
| 09 | Choi et al. (2021) [47] | Cross-sectional | General | 800 | - | - | - | International Trauma Questionnaire (ITQ) |
| 10 | Cohen et al. (2009) [48] | Cross-sectional | Clinical | 850 | 100% | 36.4 ± 8.3 | 637 | Harvard Trauma Questionnairem (HTQ) |
| 11 | Cofini er al. (2015) [49] | Cross-sectional | Survivors | 281 | 54% | 43 | 103 | Davidson Trauma Scale (DTS) |
| 12 | Eşsizoğlu et al. (2017) [50] | Cross-sectional | General | 93 | 34.4% | 28.28 ± 9.8 | 63 | Traumatic Stress Symptom Scale (TSSC) |
| 13 | Facer-Irwin et al. (2022) [51] | Cross-sectional | Imprisoned | 221 | 0% | 31.3 ± 9.0 | 116 | International Trauma Questionnaire (ITQ) |
| 14 | Frost et al. (2019) [17] | Cross-sectional | General | 1051 | 68.4% | 47.18 | - | Life Events Checklist (LEC) |
| 15 | Gros et al. (2013) [52] | Cross-sectional | Veterans | 92 | 6.5% | 33.2 ± 9.0 | 48 | Clinician Administered PTSD Scale |
| 16 | Hyland et al. (2017) [53] | Cross-sectional | General | 2591 | 54.6% | 24 | - | International Trauma Questionnaire (ITQ) |
| 17 | Hyland et al. (2018) [54] | Cross-sectional | Refugees | 110 | 51% | - | - | International Trauma Questionnaire (ITQ) |
| 18 | Hyland et al. (2021) [55] | Cross-sectional | General | 1020 | 51% | 43.1 ± 15.1 | - | International Trauma Questionnaire (ITQ) |
| 19 | Karatzias et al. (2019) [56] | Cross-sectional | General | 1051 | 68.4% | 47.18 ± 15 | - | International Trauma Questionnaire (ITQ) |
| 20 | Kimerling et al. (2009) [57] | Cross-sectional | General | 6698 | 100% | - | - | Harvard Trauma Questionnaire (HTQ) |
| 21 | Kvedaraite et al. (2022) [58] | Cross-sectional | General | 885 | 63.4% | 37.96 ± 14.67 | 205 | International Trauma Questionnaire (ITQ) |
| 22 | Lee et al. (2009) [59] | Cross-sectional | General | 196 | - | - | - | Schedules for Clinical Assessment in Neuropsychiatry |
| 23 | Mills et al. (2016) [60] | Longitudinal | Clinical | 103 | 60% | 33.4 ± 7.40 | 79 | Clinician-Administered PTSD Scale |
| 24 | Murphy et al. (2021) [61] | Cross-sectional | Veterans | 177 | 4.90% | - | 127 | International Trauma Questionnaire (ITQ) |
| 25 | Nandi et al. (2004) [62] | Longitudinal | General | 1939 | 54.3% | - | - | Structured Clinical Interview for DSM-IV Axis I Disorders |
| 26 | Pazderka et al. (2022) [63] | Cross-sectional | General | 159 | 100% | - | - | Lifetime Violent Traumatic Event Experience |
| 27 | Powers et al. (2014) [64] | Longitudinal | Clinical | 327 | 36% | 46 ± 18.00 | 141 | Primary Care Post-Traumatic Stress Disorder Screen |
| 28 | Rybojad et al. (2016) [65] | Cross-sectional | Paramedics | 100 | 14% | 33.6 ± 9.30 | - | Impact of Event Scale—Revised (IES-R) |
| 29 | Serrano et al. (2021) [21] | Cross-sectional | General | 26,213 | 68.7% | 49.5 ± 17.0 | - | Davidson Trauma Scale (DTS) |
| 30 | Simon et al. (2019) [66] | Cross-sectional | Clinical | 246 | 50% | 47.37 ± 12 | 235 | International Trauma Questionnaire (ITQ) |
| 31 | Stuber et al. (2010) [67] | Cross-sectional | Childhood | 6542 | 52.3% | 31.85 ± 7.5 | 1439 | Posttraumatic Stress Diagnostic Scale |
| 32 | Teramoto et al. (2015) [68] | Cross-sectional | General | 296 | 57.1% | 57.10 | - | Kessler Psychological Distress Scale |
| 33 | Weiss et al. (2011) [69] | Cross-sectional | Clinical | 245 | 69.6% | 43.7 ± 10.9 | - | Clinician Administered PTSD Scale |
| ID | Author | PTSD | CPTSD | Region | GINI | NPIB | Quality Score | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | Log | VarLog | OR | Log | VarLog | ||||||
| 01 | Ali et al. (2012) [39] | 3.72 | 1.31370 | 0.0497 | - | - | Pakistan | 29.6 | 1588 | 6.0 | |
| 02 | Wright et al. (2021) [40] | 1.58 | 0.45742 | 0.1555 | 2.22 | 0.79750 | 0.06235 | United Kingdom | 32.6 | 46,125 | 6.0 |
| 03 | Ayazi et al. (2012) [41] | 4.25 | 1.44690 | 0.0127 | - | - | - | South Sudan | 44.1 | 1071 | 7.0 |
| 04 | Baek et al. (2022) [42] | 1.30 | 0.26236 | 0.0263 | 2.90 | 1.06471 | 0.02847 | South Korea | 31.4 | 32,422 | 6.0 |
| 05 | Bronner et al. (2010) [43] | 2.56 | 0.94001 | 0.0951 | - | - | - | Netherlands | 26.0 | 57,025 | 10 |
| 06 | Cénat et al. (2014) [44] | 0.84 | −0.17435 | 0.0007 | - | - | - | Haiti | 41.1 | 1742 | 6.0 |
| 07 | Cerdá et al. (2013) [45] | 1.44 | 0.36464 | 0.0100 | - | - | - | Haiti | 41.1 | 1742 | 7.0 |
| 08 | Cheng et al. (2015) [46] | 0.55 | −0.59784 | 0.0746 | - | - | - | China | 37.1 | 12,720 | 7.0 |
| 09 | Choi et al. (2021) [47] | - | - | - | 6.17 | 1.81969 | 0.02061 | South Korea | 31.4 | 32,422 | 5.0 |
| 10 | Cohen et al. (2009) [48] | 1.00 | 0.00000 | 0.0154 | - | - | - | Rwanda | 43.7 | 966 | 7.0 |
| 11 | Cofini er al (2015) [49] | 2.10 | 0.74194 | 0.0489 | - | - | - | Italy | 35.2 | 34,776 | 8.0 |
| 12 | Eşsizoğlu et al. (2017) [50] | 1.47 | 0.38526 | 0.3908 | - | - | - | Turkey | 41.9 | 10,674 | 7.0 |
| 13 | Facer-Irwin et al. (2022) [51] | 1.90 | 0.64185 | 0.0309 | 2.00 | 0.69314 | 0.05981 | United Kingdom | 32.6 | 46,125 | 7.0 |
| 14 | Frost et al. (2019) [17] | 1.48 | 0.39204 | 0.1264 | 0.88 | −0.12783 | 0.01258 | United Kingdom | 32.6 | 46,125 | 5.0 |
| 15 | Gros et al. (2013) [52] | 1.87 | 0.62594 | 0.1489 | - | - | - | United States | 39.8 | 76,329 | 9.0 |
| 16 | Hyland et al. (2017) [53] | 1.66 | 0.50682 | 0.0045 | 6.99 | 1.94448 | 0.00654 | Denmark | 27.5 | 67,790 | 7.5 |
| 17 | Hyland et al. (2018) [54] | 4.96 | 1.60141 | 0.1442 | 4.27 | 1.46161 | 0.13962 | Lebanon | 31.8 | 4136 | 6.5 |
| 18 | Hyland et al. (2021) [55] | 1.20 | 0.18232 | 0.0110 | 2.21 | 0.79299 | 0.01353 | Ireland | 31.8 | 103,983 | 6.5 |
| 19 | Karatzias et al. (2019) [56] | 0.98 | −0.02020 | 0.0120 | 1.37 | 0.31481 | 0.01259 | United Kingdom | 32.6 | 46,125 | 8.0 |
| 20 | Kimerling et al. (2009) [57] | 1.60 | 0.47000 | 0.0019 | - | - | - | United States | 39.8 | 76,329 | 5.0 |
| 21 | Kvedaraite et al. (2022) [58] | 0.89 | −0.11653 | 0.1226 | 1.99 | 0.68813 | 0.01542 | Lithuanian | 36 | 25,064 | 7.0 |
| 22 | Lee et al. (2009) [61] [59] | 1.60 | 0.47000 | 0.0051 | - | - | - | Taiwan | 34.2 | 35,513 | 7.0 |
| 23 | Mills et al. (2016) [60] | 1.74 | 0.55389 | 0.1320 | - | - | - | Australia | 34.3 | 52,084 | 7.0 |
| 24 | Murphy et al. (2021) [61] | 0.25 | −1.38629 | 0.0085 | 0.50 | −0.69314 | 0.07749 | United Kingdom | 32.6 | 46,125 | 7.5 |
| 25 | Nandi et al. (2004) [62] | 1.00 | 0.00000 | 0.0067 | - | - | - | United States | 39.8 | 76,329 | 9.0 |
| 26 | Pazderka et al. (2022) [63] | 5.18 | 1.64481 | 0.1004 | - | - | - | Canada | 31.7 | 54,917 | 6.0 |
| 27 | Powers et al. (2014) [64] | 1.03 | 0.02956 | 0.0403 | - | - | - | United States | 39.8 | 76,329 | 7.0 |
| 28 | Rybojad et al. (2016) [65] | 3.27 | 1.18479 | 0.2235 | - | - | - | Poland | 28.8 | 18,688 | 7.0 |
| 29 | Serrano et al. (2021) [21] | 1.18 | 0.16551 | 0.0005 | - | - | - | Chile | 44.9 | 15,355 | 7.0 |
| 30 | Simon et al. (2019) [66] | - | - | - | 1.75 | 0.55961 | 0.05499 | United Kingdom | 32.6 | 46,125 | 8,0 |
| 31 | Stuber et al. (2010) [67] | 2.01 | 0.69813 | 0.0232 | - | - | - | United States | 39.8 | 76,329 | 6.0 |
| 32 | Teramoto et al. (2015) [68] | 1.23 | 0.20701 | 0.0061 | - | - | - | Japan | 32.9 | 33,950 | 6.5 |
| 33 | Weiss et al. (2011) [69] | 1.57 | 0.45108 | 0.0547 | - | - | - | United States | 39.8 | 76,329 | 5.0 |
| REM | Heterogeneity Tests | Publication Bias | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| k | n | logOR | OR | p | PIlower | PIupper | IClower | ICupper | Q | p | I2 | ZEgger | p | |
| PTSD | 31 | 56,905 | 0.3826 | 1.500 | 0.000 | 0.457 | 4.702 | 0.165 | 0.600 | 804.155 | 0.001 | 98.02% | 2.0813 | 0.037 |
| CPTSD | 12 | 8047 | 0.743 | 2.180 | 0.000 | 0.501 | 8.808 | 0.346 | 1.138 | 405.014 | 0.001 | 96.42% | −0.2670 | 0.789 |
| Heterogeneity Tests | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| k | Mod | Estimate | SE | p | IClower | ICupper | Q | p | I2 | |
| PTSD | 31 | GINI | −0.0242 | 0.0221 | 0.2733 | −0.0659 | 0.0224 | 799.9109 | 0.001 | 97.76% |
| NGDP | −0.0000 | 0.0000 | 0.4926 | −0.0000 | 0.0000 | 750.4517 | 0.001 | 97.83% | ||
| CPTSD | 12 | GINI | −0.2125 | 0.1014 | 0.0649 | −0.4113 | −0.0136 | 223.8095 | 0.001 | 94.94% |
| NGDP | −0.0000 | 0.0000 | 0.8294 | −0.0000 | 0.0000 | 345.4163 | 0.001 | 96.32% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nvo-Fernandez, M.; Miño-Reyes, V.; Serrano, C.; Acosta-Antognoni, H.; Salas, F.; Wiedeman, C.V.; Ahumada-Méndez, F.; Leiva-Bianchi, M. What Is the Impact of Unemployment as an Adverse Experience? Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: A Meta-Analysis. Int. J. Environ. Res. Public Health 2025, 22, 696. https://doi.org/10.3390/ijerph22050696
Nvo-Fernandez M, Miño-Reyes V, Serrano C, Acosta-Antognoni H, Salas F, Wiedeman CV, Ahumada-Méndez F, Leiva-Bianchi M. What Is the Impact of Unemployment as an Adverse Experience? Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2025; 22(5):696. https://doi.org/10.3390/ijerph22050696
Chicago/Turabian StyleNvo-Fernandez, Marcelo, Valentina Miño-Reyes, Carlos Serrano, Hedy Acosta-Antognoni, Fabiola Salas, Claudio Vásquez Wiedeman, Francisco Ahumada-Méndez, and Marcelo Leiva-Bianchi. 2025. "What Is the Impact of Unemployment as an Adverse Experience? Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: A Meta-Analysis" International Journal of Environmental Research and Public Health 22, no. 5: 696. https://doi.org/10.3390/ijerph22050696
APA StyleNvo-Fernandez, M., Miño-Reyes, V., Serrano, C., Acosta-Antognoni, H., Salas, F., Wiedeman, C. V., Ahumada-Méndez, F., & Leiva-Bianchi, M. (2025). What Is the Impact of Unemployment as an Adverse Experience? Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: A Meta-Analysis. International Journal of Environmental Research and Public Health, 22(5), 696. https://doi.org/10.3390/ijerph22050696








