A Pilot Randomized Controlled Trial of Extracorporeal Vaginal Peflex Weights for Enhancing Pelvic Floor Function and Relieving Stress Urinary Incontinence
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Subjects
2.3. Ethical Considerations
2.4. Procedures and Data Collection
2.5. Allocation
2.6. Interventions
2.7. Intervention Protocol
2.8. Statistical Analysis
3. Results
3.1. Power Analysis
3.2. Primary Outcome Measures: Intra-Group Comparison
3.3. Secondary Outcome Measures: Intra-Group Comparison
3.4. Primary and Secondary Outcome Measures: Inter-Group Comparison
4. Discussion
4.1. Intragroup Comparison
4.2. Comparison Between the Groups
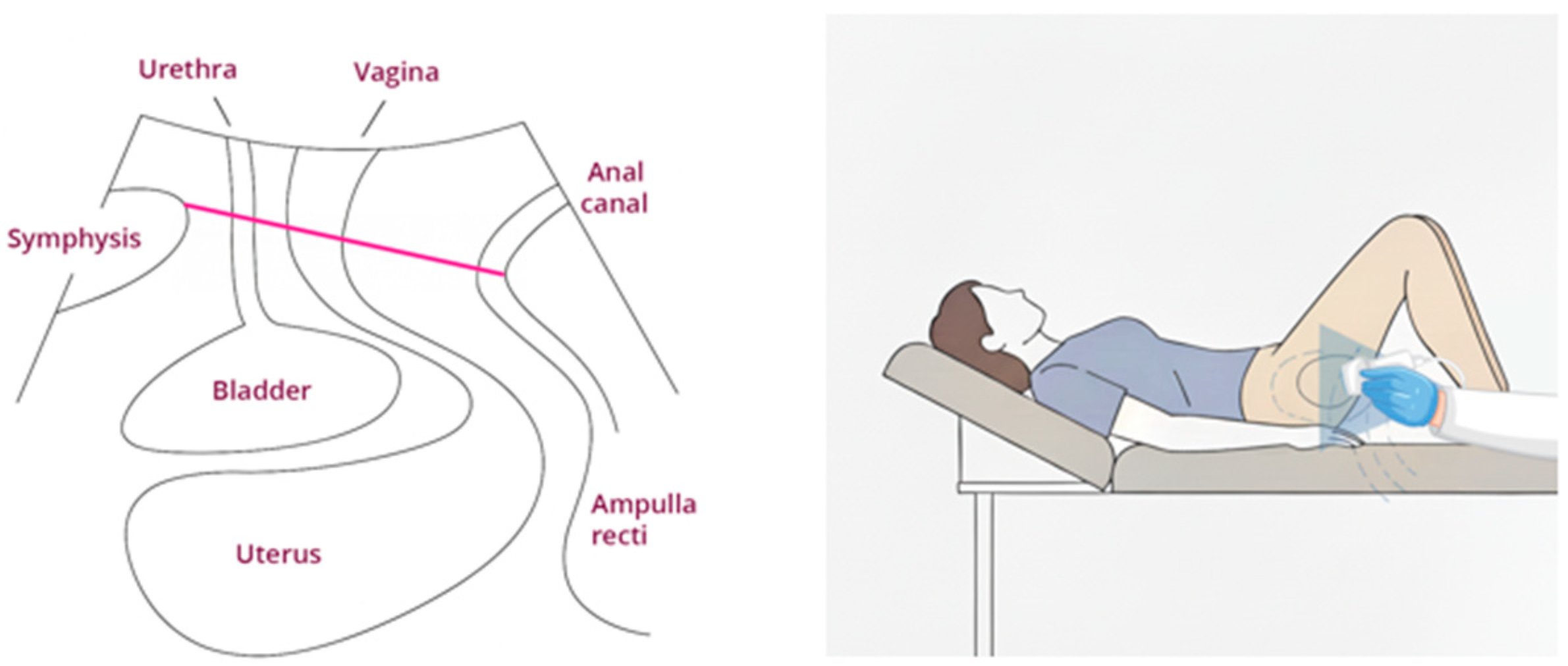
- The Peflex weights, as opposed to vaginal weights, are not inserted into the vagina but hung on a tampon string; the Peflex weights are pulled to the ground by gravity, unlike the vaginal cone that lies in a transverse position and is therefore retained in the vagina [36].
- The Peflex has a spring that allows for a slight vibrating movement that stimulates the PFM’s proprioception, which stimulates the muscle to contract; it is known that neural deficits may lead to SUI [37]. There is evidence that whole-body vibration training increases the strength of the PFM in women with SUI [38] and that proprioceptive input influences muscle activity timing, posture, coordination, and balance [39].
- The Peflex allows for visual biofeedback by practicing in front of a mirror and sensory biofeedback by pulling the Peflex down. The Peflex enables adjustments in the levels of training difficulty, such as altering the size of a tampon (the smaller the tampon, the more complex the training), adding more weights, and modifying the body’s training position (sitting, standing, squatting, etc.). The training can be more functional when carried out on a full bladder. It is recommended that training be conducted during the activity in which the patient reports SUI dysfunction, such as while singing.
- All the above induce sensorimotor adaptation, promoting pelvic floor reaction and enhancing motor learning. Motor learning encompasses repeated practice with successful outcomes, visual feedback that allows one to observe the weight being lifted upward, and practicing pelvic floor contractions with varying weights and positions [40].
- Relaxation is essential in muscle training. Muscle relaxation enables the muscles to recover between contractions, facilitating optimal strength development [41]. Reaching this state of relaxation is recommended by holding and lifting the Peflex weights.
4.3. Possible Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vaughan, C.P.; Markland, A.D. Urinary incontinence in women. Ann. Intern. Med. 2020, 172, ITC17–ITC32. [Google Scholar] [CrossRef]
- Haylen, B.T.; de Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int. Urogynecol. J. 2010, 21, 5–26. [Google Scholar] [CrossRef] [PubMed]
- Abufaraj, M.; Xu, T.; Cao, C.; Siyam, A.; Isleem, U.; Massad, A.; Soria, F.; Shariat, S.F.; Sutcliffe, S.; Yang, L. Prevalence and trends in urinary incontinence among women in the United States, 2005–2018. Am. J. Obstet. Gynecol. 2021, 225, e1–e166. [Google Scholar] [CrossRef] [PubMed]
- Elia, D.; Gambiacciani, M.; Ayoubi, J.-M.; Berreni, N.; Bohbot, J.M.; Descamps, P.; Druckmann, R.; Geoffrion, H.; Haab, F.; Heiss, N.; et al. Female urine incontinence: Vaginal erbium laser (VEL) effectiveness and safety. Horm. Mol. Biol. Clin. Investig. 2020, 41, 20200012. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M. Stress incontinence in women. N. Engl. J. Med. 2021, 384, 2428–2436. [Google Scholar] [CrossRef]
- Barakat, R.; Pelaez, M.; Montejo, R.; Luaces, M.; Zakynthinaki, M. Exercise during pregnancy improves maternal health perception: A randomized controlled trial. Am. J. Obstet. Gynecol. 2011, 204, e1–e7. [Google Scholar] [CrossRef]
- Tähtinen, R.M.; Cartwright, R.; Tsui, J.F.; Aaltonen, R.L.; Aoki, Y.; Cárdenas, J.L.; El Dib, R.; Joronen, K.M.; Al Juaid, S.; Kalantan, S.; et al. Long-term Impact of Mode of Delivery on Stress Urinary Incontinence and Urgency Urinary Incontinence: A Systematic Review and Meta-analysis. Eur. Urol. 2016, 70, 148–158. [Google Scholar] [CrossRef]
- Subak, L.L.; Richter, H.E.; Hunskaar, S. Obesity and urinary incontinence: Epidemiology and clinical research update. J. Urol. 2009, 182, S2–S7. [Google Scholar] [CrossRef]
- Abrams, P.; Andersson, K.; Apostolidis, A.; Birder, L.; Bliss, D.; Brubaker, L.; Cardozo, L.; Castro-Diaz, D.; O’COnnell, P.; Cottenden, A.; et al. 6th international consultation on incontinence. Recommendations of the international scientific committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol. Urodyn. 2018, 37, 2271–2272. [Google Scholar] [CrossRef]
- Hay-Smith, E.J.C.; Dumoulin, C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2006, 10, CD005654. [Google Scholar] [CrossRef]
- García-Sánchez, E.; Ávila-Gandía, V.; López-Román, J.; Martínez-Rodríguez, A.; Rubio-Arias, J.Á. What Pelvic Floor Muscle Training Load is Optimal in Minimizing Urine Loss in Women with Stress Urinary Incontinence? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4358. [Google Scholar] [CrossRef]
- Felicíssimo, M.F.; Carneiro, M.M.; Saleme, C.S.; Pinto, R.Z.; da Fonseca, A.M.R.M.; da Silva-Filho, A.L. Intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: A randomized comparative trial. Int. Urogynecol. J. 2010, 21, 835–840. [Google Scholar] [CrossRef]
- Bertotto, A.; Schvartzman, R.; Uchôa, S.; Wender, M.C.O. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2017, 36, 2142–2147. [Google Scholar] [CrossRef] [PubMed]
- Herderschee, R.; Hay-Smith, E.C.J.; Herbison, G.P.; Roovers, J.P.; Heineman, M.J. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women: Shortened version of a Cochrane systematic review. Neurourol. Urodyn. 2013, 32, 325–329. [Google Scholar] [CrossRef]
- Nunes, E.F.C.; Sampaio, L.M.M.; Biasotto-Gonzalez, D.A.; Nagano, R.C.D.R.; Lucareli, P.R.G.; Politti, F. Biofeedback for pelvic floor muscle training in women with stress urinary incontinence: A systematic review with meta-analysis. Physiotherapy 2019, 105, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Kondo, A. Clinical value of vaginal cones for the management of female stress incontinence. Int. Urogynecol. J. Pelvic Floor. Dysfunct. 1997, 8, 314–317. [Google Scholar] [CrossRef]
- Castro, R.A.; Arruda, R.M.; Zanetti, M.R.D.; Santos, P.D.; Sartori, M.G.F.; Girão, M.J.B.C. Single-blind, randomized, controlled trial of pelvic floor muscle training, electrical stimulation, vaginal cones, and no active treatment in the management of stress urinary incontinence. Clinics 2008, 63, 465–472. [Google Scholar] [CrossRef]
- Golmakani, N.; Khadem, N.; Arabipoor, A.; Kerigh, B.F.; Esmaily, H. Behavioral Intervention Program versus Vaginal Cones on Stress Urinary Incontinence and Related Quality of Life: A Randomized Clinical Trial. Oman Med. J. 2014, 29, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Sahin, N.; Yesil, H.; Gorcan, B. The effect of pelvic floor exercises performed with EMG biofeedback or a vaginal cone on incontinence severity, pelvic floor muscle strength, and quality of life in women with stress urinary incontinence: A randomized, 6-month follow-up study. Int. Urogynecol. J. 2022, 33, 2773–2779. [Google Scholar] [CrossRef]
- da Silva, J.B.; de Godoi Fernandes, J.G.; Caracciolo, B.R.; Zanello, S.C.; de Oliveira Sato, T.; Driusso, P. Reliability of the PERFECT scheme assessed by unidigital and bidigital vaginal palpation. Int. Urogynecol. J. 2021, 32, 3199–3207. [Google Scholar] [CrossRef]
- Ahlund, S.; Nordgren, B.; Wilander, E.-L.; Wiklund, I.; Fridén, C. Is home-based pelvic floor muscle training effective in treatment of urinary incontinence after birth in primiparous women? A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2013, 92, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, M.; Kitta, T.; Takahashi, Y.; Chiba, H.; Higuchi, M.; Togo, M.; Shinohara, N. Reliability of manometry for assessing pelvic floor muscle function in healthy men. Neurourol. Urodyn. 2020, 39, 1464–1471. [Google Scholar] [CrossRef]
- Bele, A.; Qureshi, M. Impact of Electrotherapy or Muscle Training on Quality of Life in Urinary Incontinence of Male Geriatric Population-A Protocol. J. Clin. Diagn. 2021, 15, YK01–YK03. [Google Scholar] [CrossRef]
- Tosun, O.C.; Mutlu, E.K.; Ergenoglu, A.; Yeniel, A.; Tosun, G.; Malkoc, M.; Askar, N.; Itil, I. Does pelvic floor muscle training abolish symptoms of urinary incontinence? A randomized controlled trial. Clin. Rehabil. 2015, 29, 525–537. [Google Scholar] [CrossRef]
- Rahmani, N.; Mohseni-Bandpei, M.A. Application of perineometer in the assessment of pelvic floor muscle strength and endurance: A reliability study. J. Bodyw. Mov. Ther. 2011, 15, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Alves, F.K.; Riccetto, C.; Adami, D.B.; Marques, J.; Pereira, L.C.; Palma, P.; Botelho, S. A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial. Maturitas 2015, 81, 300–305. [Google Scholar] [CrossRef]
- Avery, K.; Donovan, J.; Peters, T.J.; Shaw, C.; Gotoh, M.; Abrams, P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol. Urodyn. 2004, 23, 322–330. [Google Scholar] [CrossRef]
- Volløyhaug, I.; Mørkved, S.; Salvesen, Ø.; Salvesen, K.Å. Assessment of pelvic floor muscle contraction with palpation, perineometry and transperineal ultrasound: A cross-sectional study. Ultrasound Obstet. Gynecol. 2016, 47, 768–773. [Google Scholar] [CrossRef]
- Nyhus, M.Ø.; Oversand, S.H.; Salvesen, Ø.; Salvesen, K.Å.; Mathew, S.; Volløyhaug, I. Ultrasound assessment of pelvic floor muscle contraction: Reliability and development of an ultrasound-based contraction scale. Ultrasound Obstet. Gynecol. 2020, 55, 125–131. [Google Scholar] [CrossRef]
- Frawley, H.; Shelly, B.; Morin, M.; Bernard, S.; Bø, K.; Digesu, G.A.; Dickinson, T.; Goonewardene, S.; McClurg, D.; Rahnama’I, M.S.; et al. An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol. Urodyn. 2021, 40, 1217–1260. [Google Scholar] [CrossRef] [PubMed]
- Jagadeeswari, J.; KalaBarathi, S. Effectiveness of vaginal cone therapy on urinary incontinence among women in saveetha medical college hospital, Thandalam, Chennai. Asian J. Pharm. Clin. Res. 2019, 12, 133–136. [Google Scholar] [CrossRef]
- Bø, K.; Talseth, T.; Holme, I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 1999, 318, 487–493. [Google Scholar] [CrossRef]
- Pereira, V.S.; de Melo, M.V.; Correia, G.N.; Driusso, P. Vaginal cone for postmenopausal women with stress urinary incontinence: Randomized, controlled trial. Climacteric 2012, 15, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.T.; Yoon, H.; Kim, Y.H. A randomized prospective study comparing new vaginal cone and FES-Biofeedback. Yonsei Med. J. 2004, 45, 879–884. [Google Scholar] [CrossRef]
- Arvonen, T.; Fianu-Jonasson, A.; Tyni-Lenné, R. Effectiveness of two conservative modes of physical therapy in women with urinary stress incontinence. Neurourol. Urodyn. 2001, 20, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Hahn, I.; Milsom, I.; Ohlsson, B.L.; Ekelund, P.; Uhlemann, C.; Fall, M. Comparative assessment of pelvic floor function using vaginal cones, vaginal digital palpation and vaginal pressure measurements. Gynecol. Obstet. Investig. 1996, 41, 269–274. [Google Scholar] [CrossRef]
- Cervigni, M.; Gambacciani, M. Female urinary stress incontinence. Climacteric 2015, 18 (Suppl. 1), 30–36. [Google Scholar] [CrossRef]
- Farzinmehr, A.; Moezy, A.; Koohpayehzadeh, J.; Kashanian, M. A Comparative study of whole body vibration training and pelvic floor muscle training on women’s stress urinary incontinence: Three- month follow-up. J. Family Reprod. Health 2015, 9, 147–154. [Google Scholar] [PubMed]
- Franco, P.G.; Santos, K.B.; Rodacki, A.L.F. Joint positioning sense, perceived force level and two-point discrimination tests of young and active elderly adults. Braz. J. Phys. Ther. 2015, 19, 304–310. [Google Scholar] [CrossRef]
- Leech, K.A.; Roemmich, R.T.; Gordon, J.; Reisman, D.S.; Cherry-Allen, K.M. Updates in motor learning: Implications for physical therapist practice and education. Phys. Ther. 2022, 102, pzab250. [Google Scholar] [CrossRef]
- Cho, S.T.; Kim, K.H. Pelvic floor muscle exercise and training for coping with urinary incontinence. J. Exerc. Rehabil. 2021, 17, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Rocca Rossetti, S. Functional anatomy of pelvic floor. Arch. Ital. Urol. Androl. 2016, 88, 28–37. [Google Scholar] [CrossRef] [PubMed]

| Demographic Data | Peflex Group (N = 14) | Control Group (N = 14) | p-Value |
|---|---|---|---|
| Age (years) | 0.645 ^^ | ||
| Mean ± SD | 40.93 ± 5.60 | 39.50 ± 7.39 | |
| BMI (kg/m2) | 0.713 ^^ | ||
| Mean ± SD | 23.11 ± 2.86 | 23.91 ± 3.26 | |
| Number of deliveries | 0.266 ^^ | ||
| Mean ± SD | 2.36 ± 1.39 | 2.00 ± 0.43 | |
| Median (Q1, Q3) | 2.00 (1.00, 6.00) | 1.50 (1.00, 7.00) | |
| Newborn weight (grams) | 0.679 ^^ | ||
| Mean ± SD | 3272.86 ± 366.76 | 3286.86 ± 741.62 | |
| Number of pregnancies | 0.538 ^^ | ||
| Mean ± SD | 3.14 ± 2.24 | 2.57 ± 1.95 | |
| Median (Q1, Q3) | 2.00 (1.00, 7.00) | 2.00 (1.00, 8.00) | |
| Instrumental birth | ~1.000 ^ | ||
| Yes | 2 (14%) | 3 (21%) | |
| No | 12 (86%) | 11 (79%) | |
| Cesarean delivery | 0.481 ^ | ||
| Yes | 2 (14%) | 0 (0%) | |
| No | 8 (86%) | 14 (100%) | |
| Obstetric rupture | ~1.000 ^ | ||
| Yes | 8 (57%) | 9 (64%) | |
| No | 6 (43%) | 5 (36%) | |
| Episiotomy | ~1.000 ^ | ||
| Yes | 6 (42%) | 6 (42%) | |
| No | 8 (58%) | 8 (58%) | |
| Weekly sports activity (hours) | 0.303 ^^ | ||
| Mean ± SD | 2.00 ± 1.24 | 1.43 ± 1.45 |
| Outcome Measures | Peflex Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Pre-Treatment Mean ± SD | Post-Treatment Mean ± SD | p-Value | Pre-Treatment Mean ± SD | Post-Treatment Mean ± SD | p-Value | |
| Total ICIQ-UI-SF score | 10.07 ± 2.64 | 5.50 ± 3.44 | 0.002 ** | 12.29 ± 3.10 | 7.36 ± 3.27 | 0.002 ** |
| Amount of incontinence | 2.71 ± 0.99 | 1.57 ± 0.85 | 0.004 ** | 2.57± 1.22 | 2.00 ± 0.00 | 0.102 |
| Frequency of incontinence | 1.86 ± 0.86 | 0.86 ±0.53 | 0.005 ** | 2.21 ± 1.05 | 1.29 ± 0.83 | 0.025 ** |
| Daily Life Interference (NRS) | 5.64± 1.65 | 3.07 ± 2.53 | 0.005 ** | 7.50 ± 2.21 | 4.07 ± 2.64 | 0.003 ** |
| Outcomes Measures | Peflex Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Pre-Treatment Mean ± SD | Post-Treatment Mean ± SD | p-Value | Pre-Treatment Mean ± SD | Post-Treatment Mean ± SD | p-Value | |
| Perineometer pressure (cmH2O) | 12.79 ± 12.56 | 17.77 ± 14.49 | 0.001 ** | 11.07 ± 7.19 | 13.43 ± 7.36 | 0.019 ** |
| Power (1–5) | 2.5 ± 1.09 | 3.57 ± 0.85 | 0.027 ** | 2.64 ± 0.84 | 3.07 ± 0.83 | 0.034 ** |
| Endurance (seconds) | 8.07 ± 2.59 | 9.86 ± 0.53 | 0.001 ** | 5.79 ± 2.83 | 8.79 ± 1.67 | 0.003 ** |
| Repetitions (N) | 3.79 ± 1.85 | 8.14 ± 1.83 | 0.004 ** | 4.79 ± 2.42 | 6.64 ± 2.44 | 0.005 ** |
| Fast contractions (N) | 5.71 ± 2.40 | 8.93 ± 1.86 | 0.004 ** | 6.36 ± 2.44 | 8.21 ± 2.04 | 0.029 ** |
| US levator hiatus. Proportional change in contraction (mm) | 7.64 ± 5.18 | 10.71 ± 5.61 | 0.048 ** | 8.26 ± 7.34 | 7.08 ± 5.90 | 0.331 |
| Outcomes Measures | Peflex Group Mean ± SD | Control Group Mean ± SD | p-Value |
|---|---|---|---|
| Relative Delta Total ICIQ-UI-SF score (%) | 41.55 ± 31.43 | −44.80± 35.91 | 0.660 |
| Delta Frequency incontinence (%) | −9.09 ± 7.13 | −8.44 ± 11.53 | 0.883 |
| Delta Amount of incontinence (%) | −10.38 ± 9.33 | −5.19 ± 11.11 | 0.096 |
| Delta Daily Life Interference (%) | −23.37 ± 20.39 | −31.16 ± 26.13 | 0.471 |
| Delta Perineometer (%) | 37.01 ± 2993 | 21.42 ± 28.66 | 0.179 |
| Delta Power (%) | 9.09 ± 5.04 | 3.89 ± 5.87 | 0.015 ** |
| Delta Endurance (%) | 16.23 ± 23.43 | 27.27 ± 19.20 | 0.121 |
| Delta Repetitions (%) | 39.61 ± 21.27 | 17.20 ± 15.96 | 0.007 ** |
| Delta Fast contractions (%) | 29.22 ± 24.23 | 16.88 ± 26.40 | 0.286 |
| Delta Levator hiatus Proportional change in contraction (%) | 3.06 ± 5.52 | −1.17 ± 3.54 | 0.022 ** |
| Satisfaction with treatment (NRS) | 8.64 ± 1.50 | 7.50 ± 1.51 | 0.054 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bar Chen, A.; Fligelman, T.; Kalichman, L. A Pilot Randomized Controlled Trial of Extracorporeal Vaginal Peflex Weights for Enhancing Pelvic Floor Function and Relieving Stress Urinary Incontinence. Int. J. Environ. Res. Public Health 2025, 22, 1703. https://doi.org/10.3390/ijerph22111703
Bar Chen A, Fligelman T, Kalichman L. A Pilot Randomized Controlled Trial of Extracorporeal Vaginal Peflex Weights for Enhancing Pelvic Floor Function and Relieving Stress Urinary Incontinence. International Journal of Environmental Research and Public Health. 2025; 22(11):1703. https://doi.org/10.3390/ijerph22111703
Chicago/Turabian StyleBar Chen, Avital, Tal Fligelman, and Leonid Kalichman. 2025. "A Pilot Randomized Controlled Trial of Extracorporeal Vaginal Peflex Weights for Enhancing Pelvic Floor Function and Relieving Stress Urinary Incontinence" International Journal of Environmental Research and Public Health 22, no. 11: 1703. https://doi.org/10.3390/ijerph22111703
APA StyleBar Chen, A., Fligelman, T., & Kalichman, L. (2025). A Pilot Randomized Controlled Trial of Extracorporeal Vaginal Peflex Weights for Enhancing Pelvic Floor Function and Relieving Stress Urinary Incontinence. International Journal of Environmental Research and Public Health, 22(11), 1703. https://doi.org/10.3390/ijerph22111703







