Identifying Predictors of Utilization of Skilled Birth Attendance in Uganda Through Interpretable Machine Learning
Abstract
1. Introduction
2. Related Literature
3. Methodology
3.1. Data Source
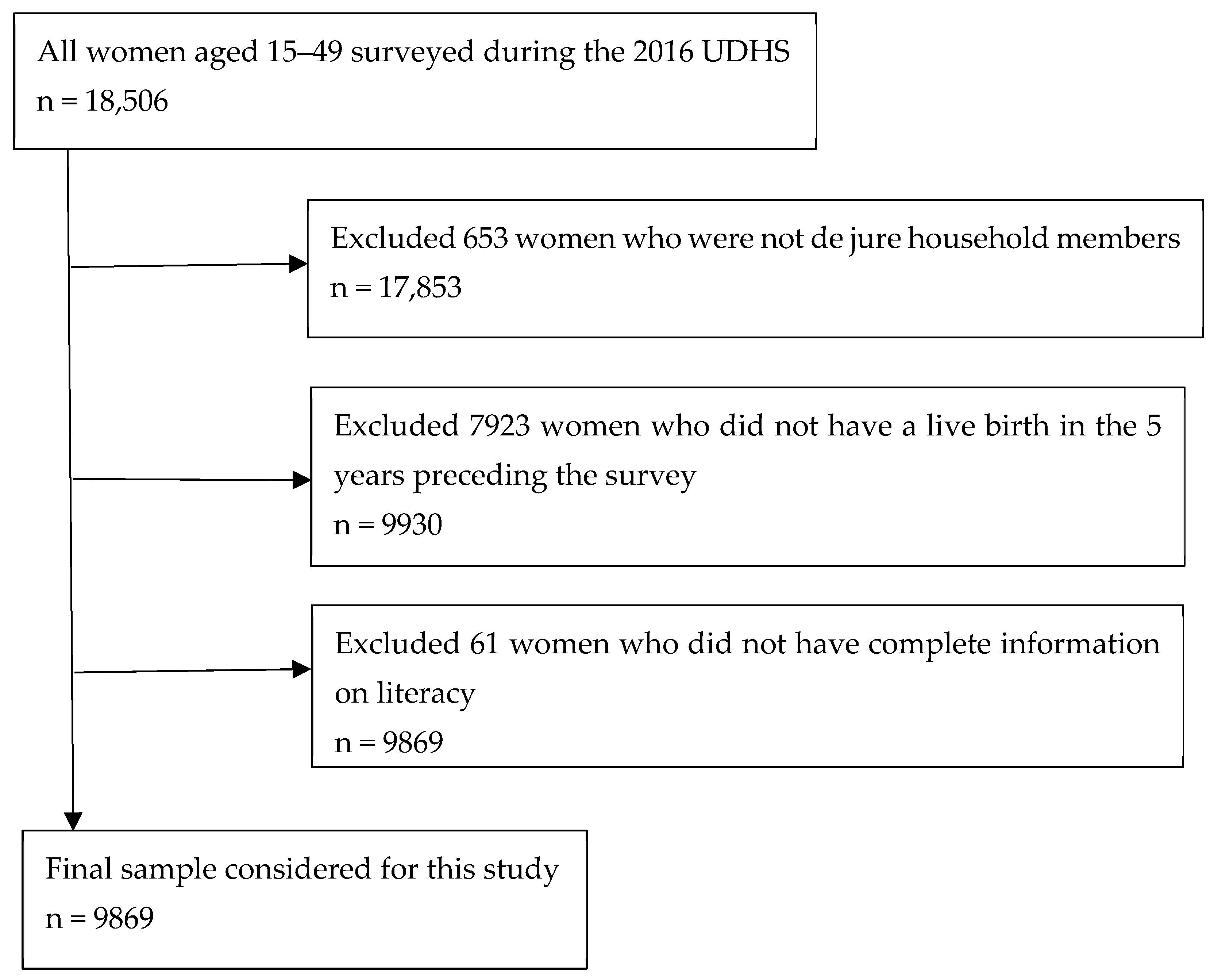
3.2. Study Population
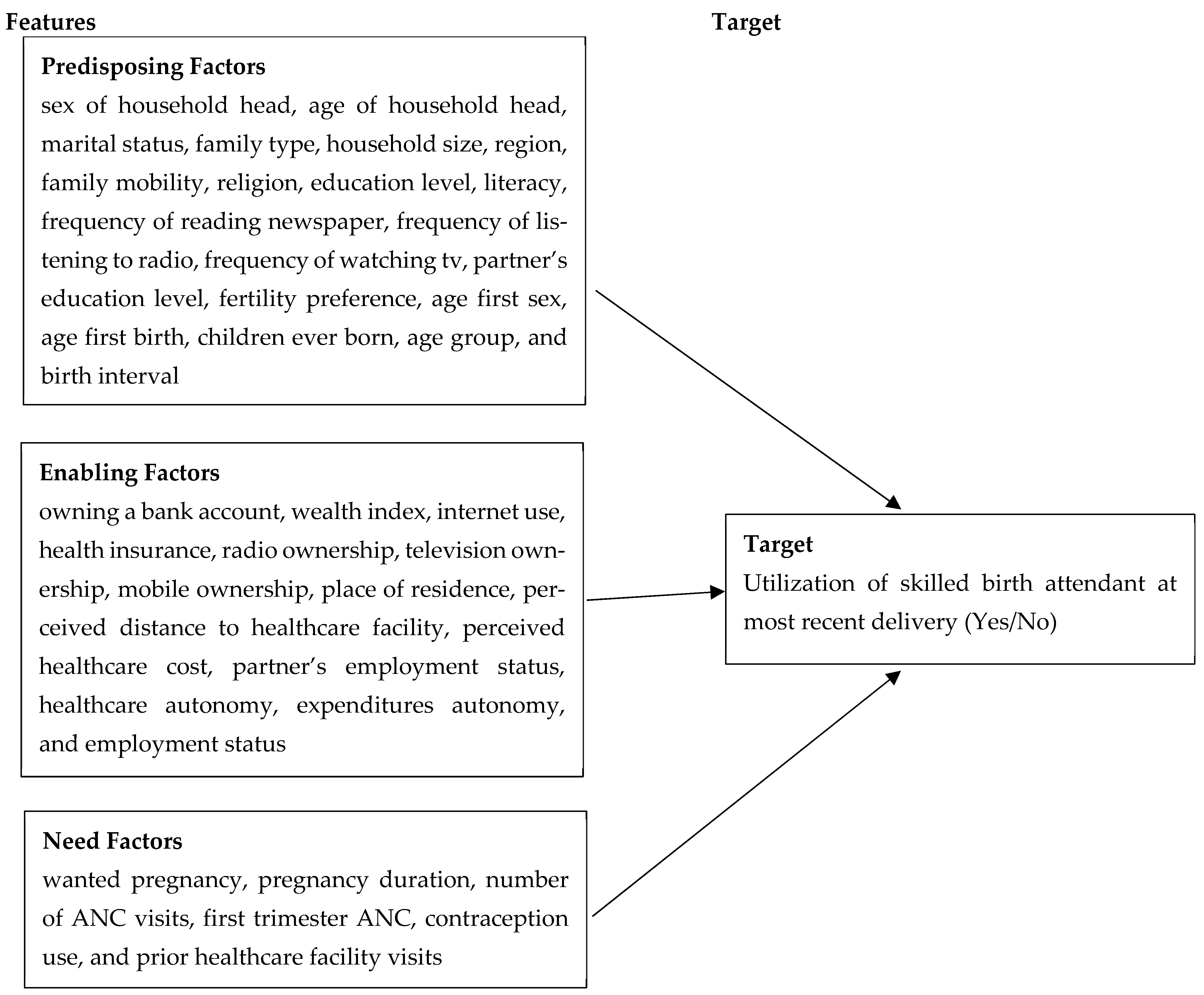
3.3. Study Variables
- (i)
- Predisposing factors: These capture socio-demographic and cultural characteristics that influence an individual’s likelihood to use health services. Variables included: sex of household head, age of household head, marital status, family type, household size, region, family mobility, religion, education level, literacy, frequency of reading newspaper, frequency of listening to radio, frequency of watching tv, partner’s education level, fertility preference, age first sex, age first birth, children ever born, age group, and birth interval.
- (ii)
- Enabling factors: These are the economic or logistic resources or conditions that facilitate or hinder access to healthcare. Variables included: owning a bank account, wealth index, internet use, health insurance, radio ownership, television ownership, mobile ownership, place of residence, perceived distance to healthcare facility, perceived healthcare cost, partner’s employment status, healthcare autonomy, expenditures autonomy, and employment status.
- (iii)
- Need factors: These are the individual’s perception of their health status and their perceived need for healthcare. Variables included: wanted pregnancy, pregnancy duration, number of ANC visits, first trimester ANC, contraception use, and prior healthcare facility visits.
- (i)
- Sex → Marriage → Birth (SMB);
- (ii)
- Marriage → Sex → Birth (MSB);
- (iii)
- Sex → Birth → Marriage (SBM);
- (iv)
- Sex → Birth → No Marriage (SBNoM).
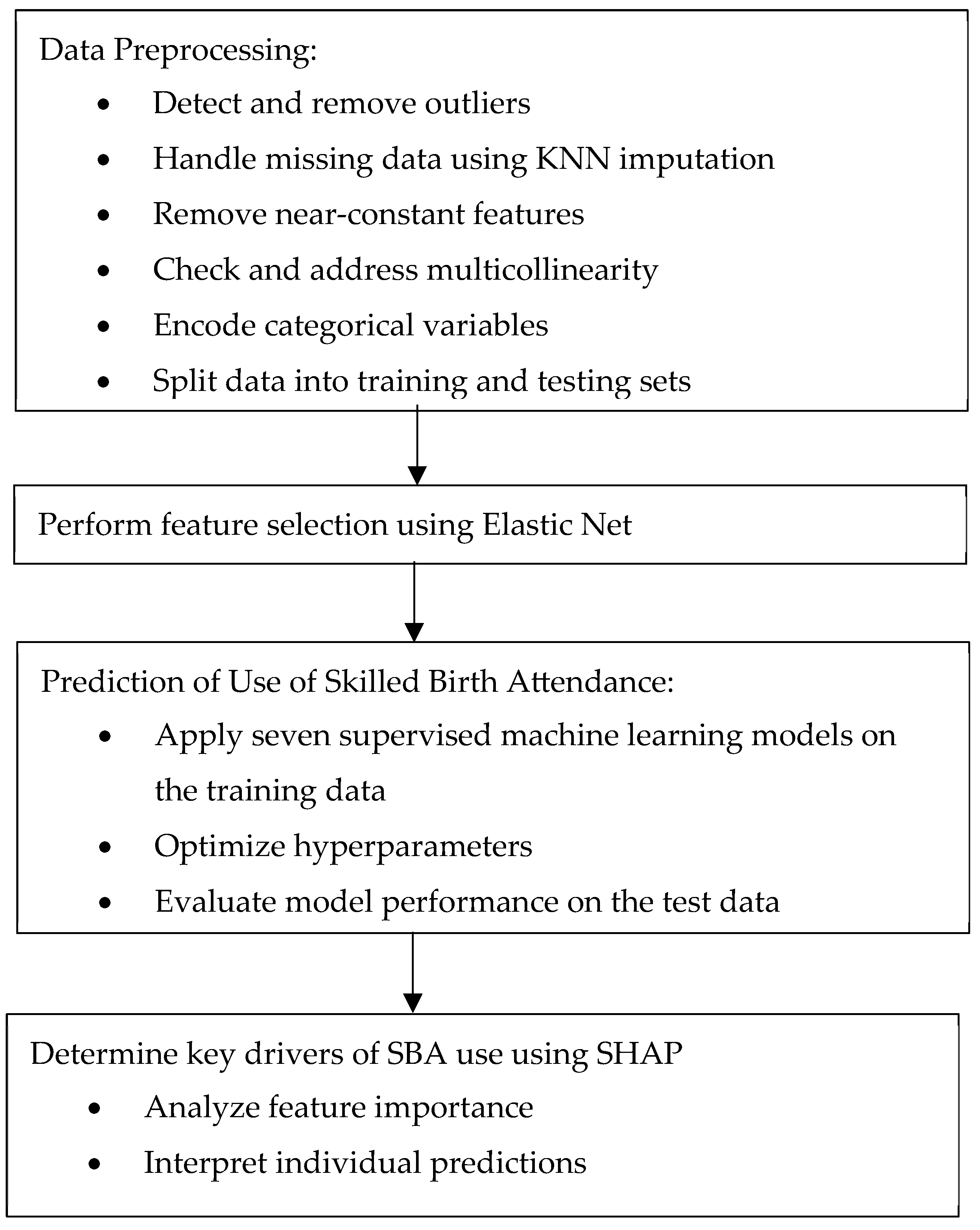
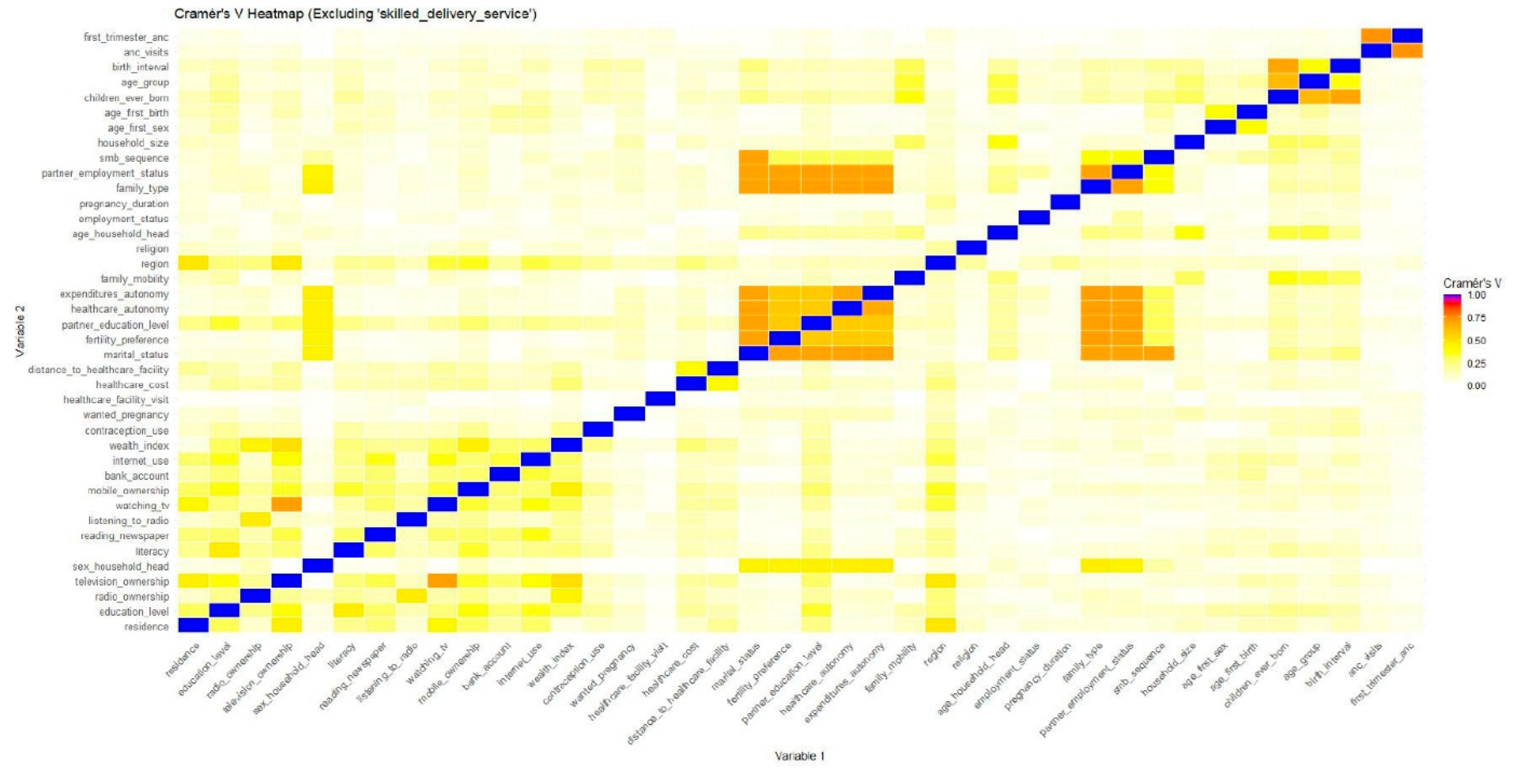
3.4. Data Preprocessing
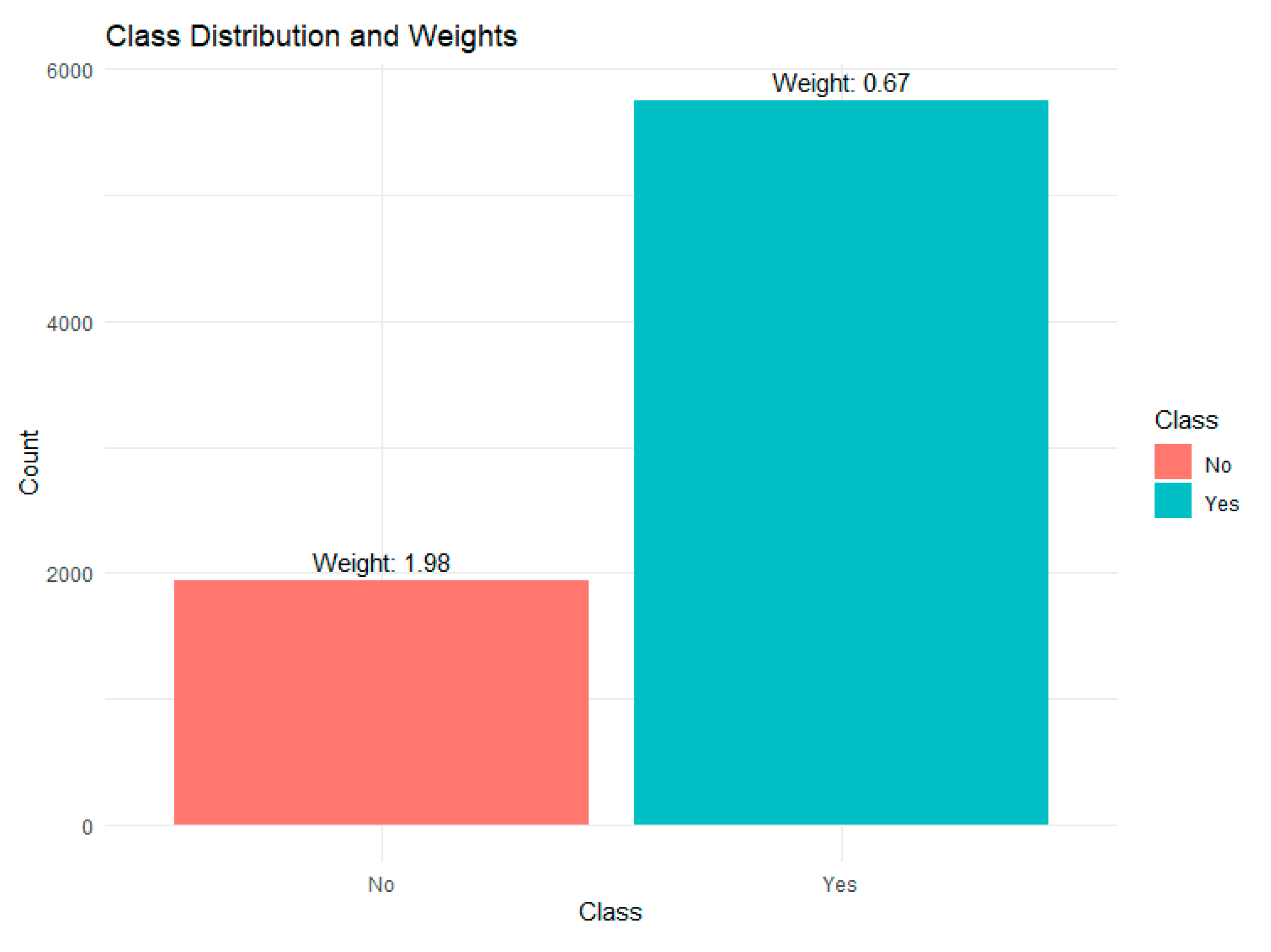
3.5. Data Splitting and Handling Class Imbalance
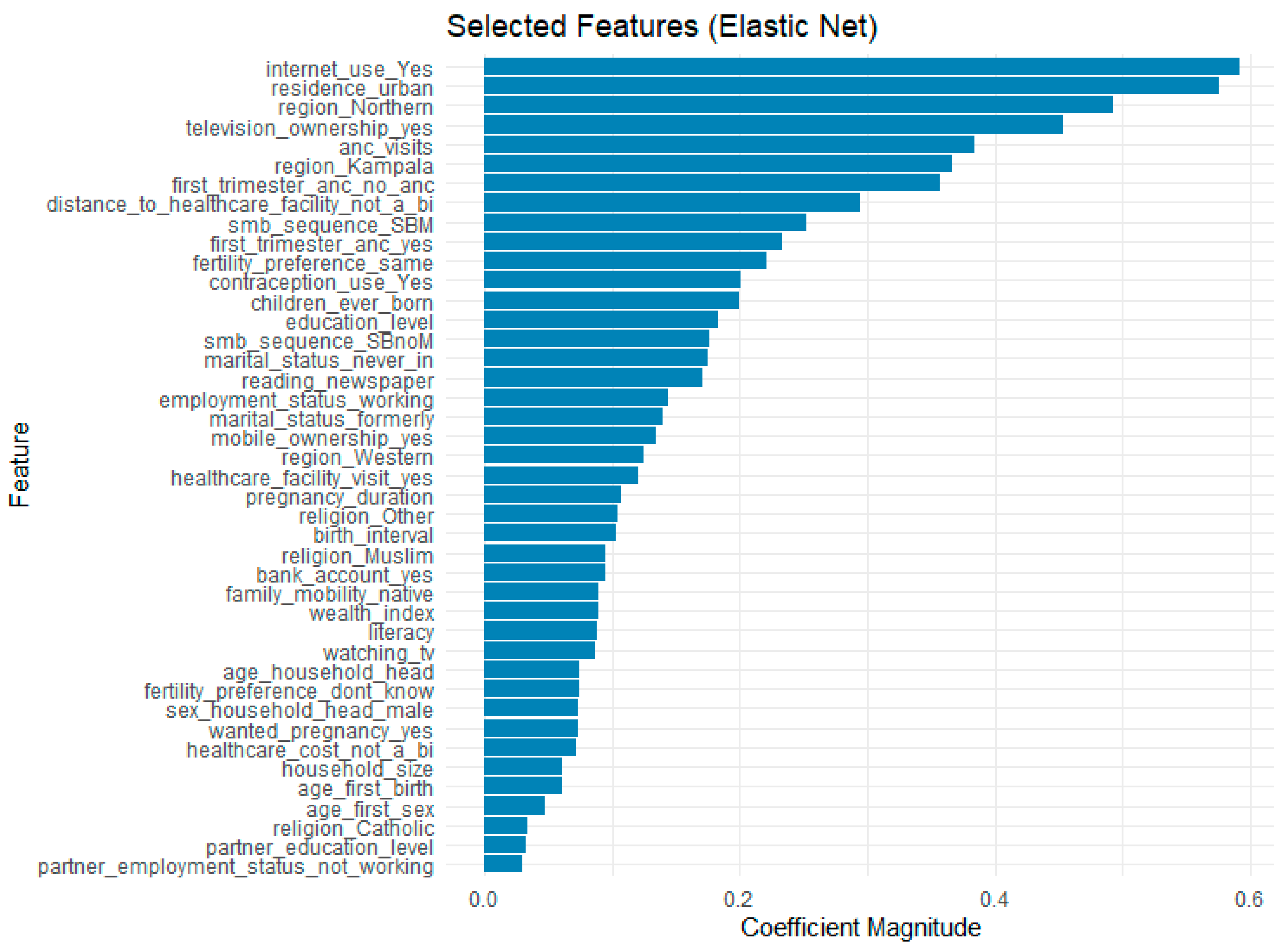
3.6. Feature Selection
3.7. Model Training
3.8. Hyperparameter Tuning
3.9. Model Evaluation
- Accuracy: the proportion of correct predictions made by the model out of all predictions.
- 2.
- Area Under the ROC Curve (AUC): measures how well the model can distinguish between different classes; i.e., it measures how well the model separates users from non-users of SBA. It is a score ranging from 0 to 1, where 1 means perfect distinction and 0.5 means no distinction.
- 3.
- Recall: measures how well the model identifies positive cases. In this case, it gives the proportion of SBA cases correctly identified by the model.
- 4.
- Precision: the proportion of true positive results out of all the positive results predicted by the model. It measures how many of the women predicted by the model as using SBA were correctly classified. In other words, it is the proportion of true SBA cases out of all cases the model predicted as SBA.
- 5.
- F1-Score: combines precision and recall into a single score. It is useful for evaluating models trained on imbalanced data.
3.10. Enhancing Model Interpretability with SHAP
4. Results
4.1. Data Characteristics and Preprocessing Results
4.2. Socio-Demographic and Economic Characteristics of the Study Population
4.3. Maternal Obstetric Characteristics of the Study Population
4.4. Feature Selection
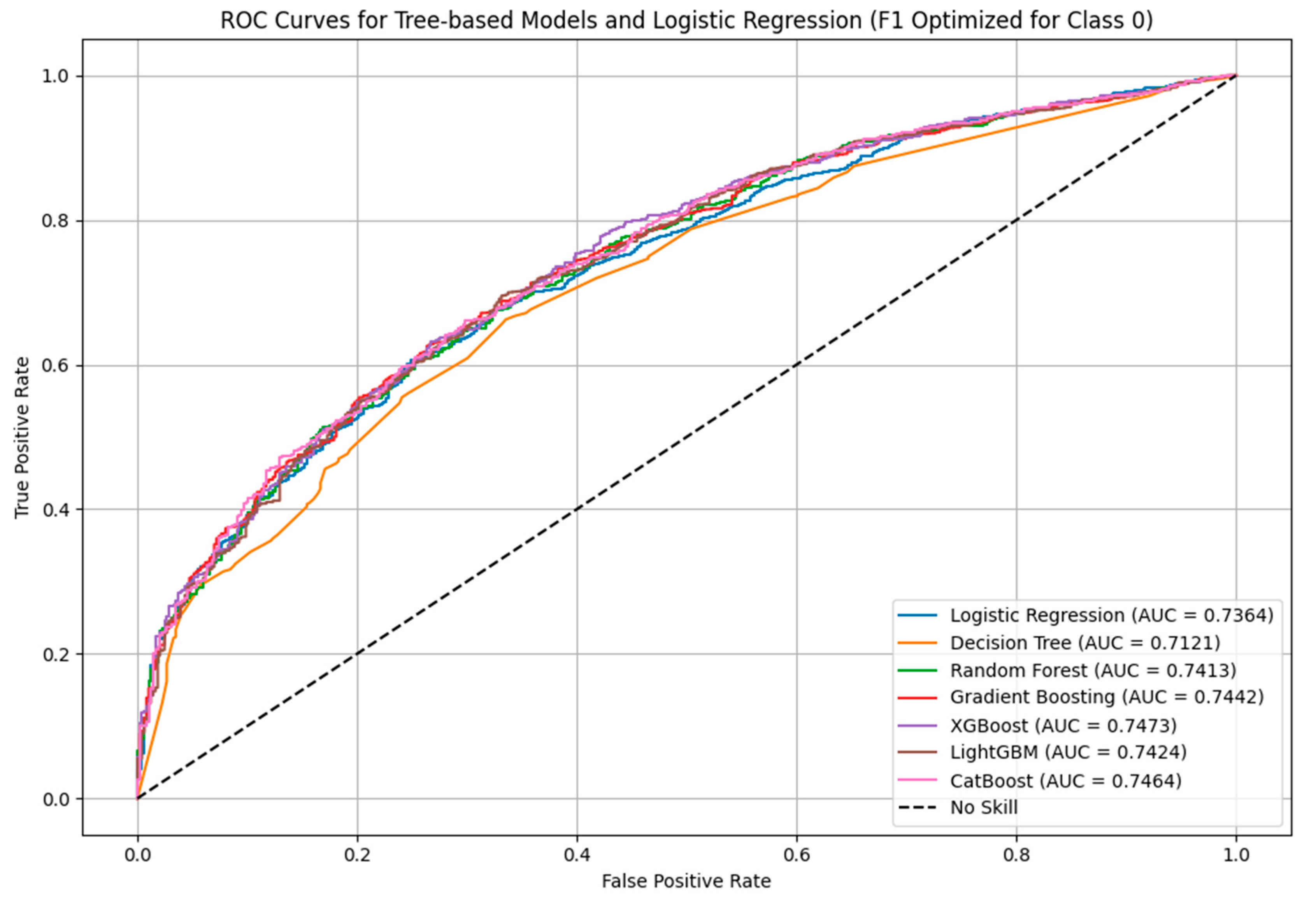
4.5. Prediction of Use of Skilled Birth Attendance
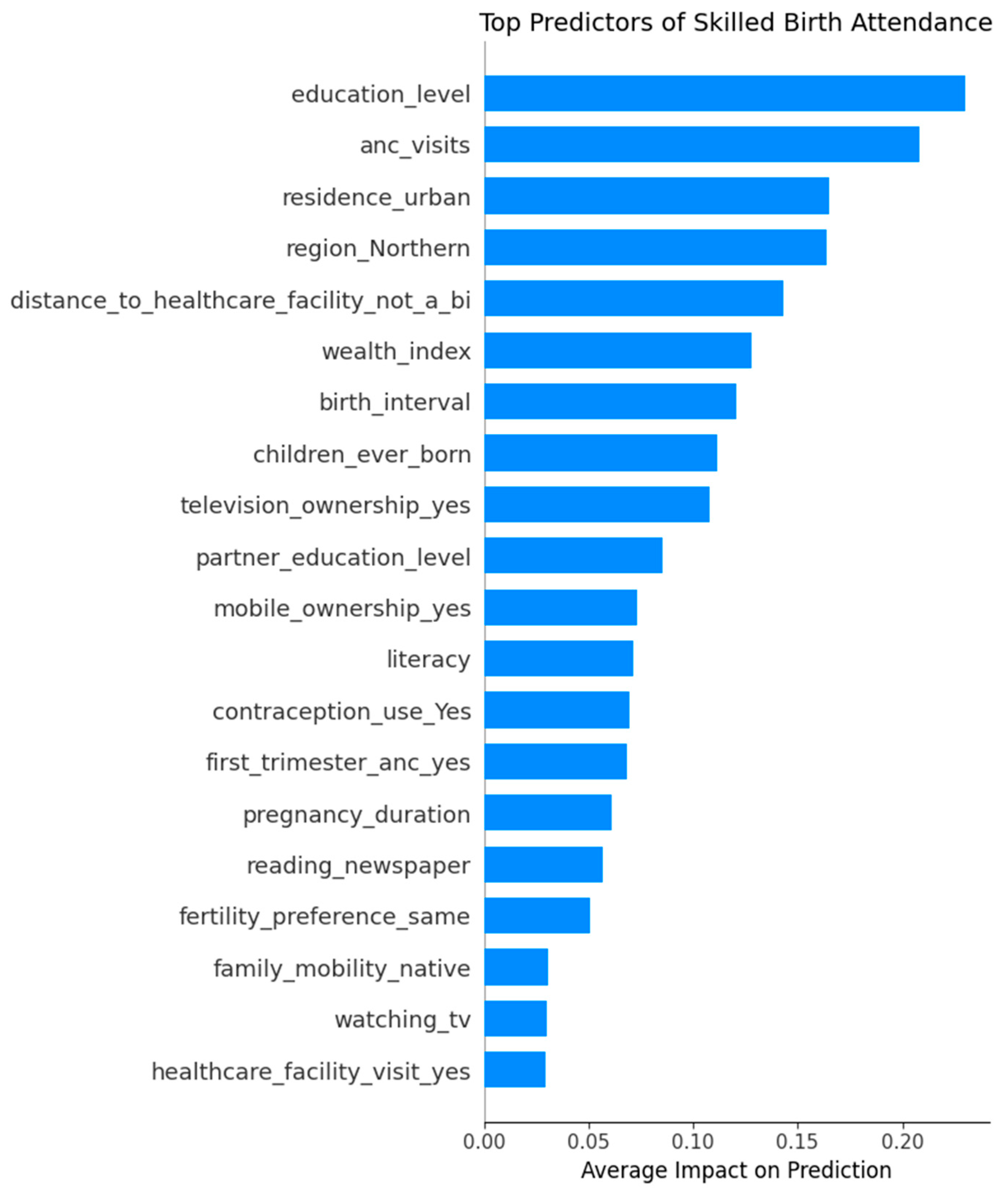
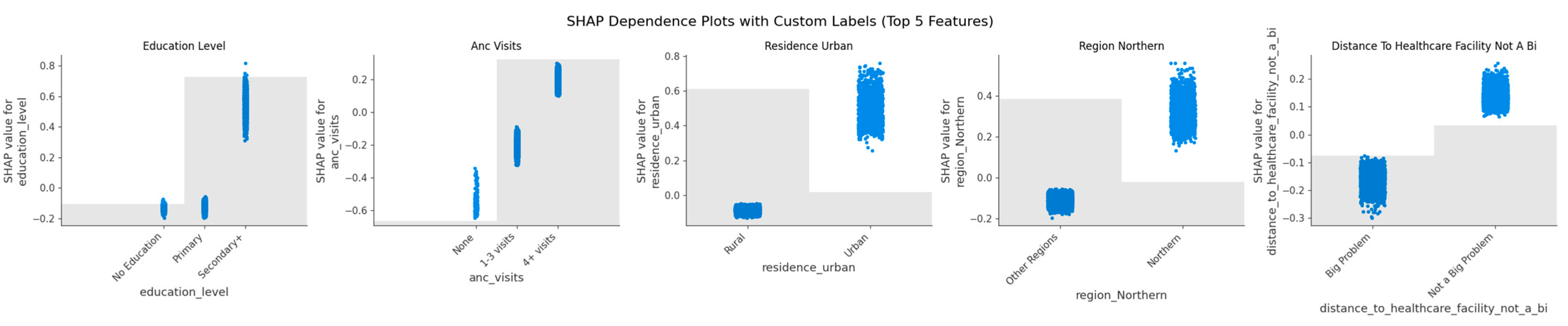
4.6. Key Drivers of SBA Use: SHAP Explanations
- Education level is the most important factor. Women with higher education are much more likely to use skilled delivery services.
- ANC visits also play a big role. Women who attended more antenatal care visits, especially 4 or more, have higher chances of using skilled birth attendants.
- Urban residence is linked to higher use of services.
- Region (Northern) has positive SHAP values, meaning women from the Northern region are more likely to use skilled delivery services, according to the model.
- Distance to health facilities is another important factor. Women who said distance was a big problem were less likely to use skilled care.
- Wealth index shows that wealthier women are more likely to use skilled services.
- Longer birth intervals are linked to higher chances of use of SBA.
- Number of children ever born shows that first-time mothers or those with fewer children are more likely to seek skilled delivery services.
- Television ownership and other media exposure like mobile ownership help improve use of services.
- Partner’s education also matters; women with more educated partners were more likely to use skilled care.
- Education level: Women with secondary or higher education strongly increase the likelihood of SBA use compared to those with no or only primary education.
- ANC visits: More antenatal visits, especially 4 or more, increase SBA use, while no visits reduce it.
- Residence (urban): Living in urban areas shifts predictions toward SBA, while rural areas shift predictions away.
- Region (Northern): Being from the Northern region increases the likelihood of SBA use compared to other regions.
- Distance to healthcare facility: Women who perceive distance as a big problem are less likely to use SBA, while those who report no distance problem are more likely to access skilled delivery.
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kibria, G.M.A.; Burrowes, V.; Choudhury, A.; Sharmeen, A.; Ghosh, S.; Mahmud, A.; Kc, A. Determinants of Early Neonatal Mortality in Afghanistan: An Analysis of the Demographic and Health Survey 2015. Glob. Health 2018, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Pattinson, R.C.; Vannevel, V.; Barnard, D.; Baloyi, S.; Gebhardt, G.S.; le Roux, K.; Moran, N.; Moodley, J. Failure to Perform Assisted Deliveries Is Resulting in an Increased Neonatal and Maternal Morbidity and Mortality: An Expert Opinion. South Afr. Med. J. 2018, 108, 75–78. [Google Scholar] [CrossRef]
- Tekelab, T.; Chojenta, C.; Smith, R.; Loxton, D. The Impact of Antenatal Care on Neonatal Mortality in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. PLoS ONE 2019, 14, e0222566. [Google Scholar] [CrossRef] [PubMed]
- WHO. Births Attended by Skilled Health Personnel; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Musarandega, R.; Nyakura, M.; Machekano, R.; Pattinson, R.; Munjanja, S.P. Causes of Maternal Mortality in Sub-Saharan Africa: A Systematic Review of Studies Published from 2015 to 2020. J. Glob. Health 2021, 11, 04048. [Google Scholar] [CrossRef]
- Adegoke, A.; van den Broek, N. Skilled Birth Attendance-Lessons Learnt. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 33–40. [Google Scholar] [CrossRef]
- Dantas, J.A.R.; Singh, D.; Lample, M. Factors Affecting Utilization of Health Facilities for Labour and Childbirth: A Case Study from Rural Uganda. BMC Pregnancy Childbirth 2020, 20, 39. [Google Scholar] [CrossRef]
- Sserwanja, Q.; Mukunya, D.; Musaba, M.W.; Kawuki, J.; Kitutu, F.E. Factors Associated with Health Facility Utilization during Childbirth among 15 to 49-Year-Old Women in Uganda: Evidence from the Uganda Demographic Health Survey 2016. BMC Health Serv. Res. 2021, 21, 1160. [Google Scholar] [CrossRef]
- Tesema, G.A.; Tessema, Z.T. Pooled Prevalence and Associated Factors of Health Facility Delivery in East Africa: Mixed-Effect Logistic Regression Analysis. PLoS ONE 2021, 16, e0250447. [Google Scholar] [CrossRef]
- Doctor, H.V.; Nkhana-Salimu, S.; Abdulsalam-Anibilowo, M. Health Facility Delivery in Sub-Saharan Africa: Successes, Challenges, and Implications for the 2030 Development Agenda. BMC Public Health 2018, 18, 765. [Google Scholar] [CrossRef]
- Ministry of Finance, Planning and Economic Development. Millennium Development Goals Report for Uganda 2010; Special Theme: Accelerating Progress towards Improving Maternal Health; Ministry of Finance, Planning and Economic Development: Kampala, Uganda, 2010. [Google Scholar]
- Munabi-Babigumira, S.; Nabudere, H.; Asiimwe, D.; Fretheim, A.; Sandberg, K. Implementing the Skilled Birth Attendance Strategy in Uganda: A Policy Analysis. BMC Health Serv. Res. 2019, 19, 655. [Google Scholar] [CrossRef]
- UBOS; ICF International. Uganda Demographic and Health Survey 2016; The DHS Program ICF: Rockville, MD, USA; UBOS: Kampala, Uganda, 2018. [Google Scholar]
- Rajula, H.S.R.; Verlato, G.; Manchia, M.; Antonucci, N.; Fanos, V. Comparison of Conventional Statistical Methods with Machine Learning in Medicine: Diagnosis, Drug Development, and Treatment. Medicina 2020, 56, 455. [Google Scholar] [CrossRef]
- Bzdok, D.; Krzywinski, M.; Altman, N. Machine Learning: A Primer. Nat. Methods 2017, 14, 1119–1120. [Google Scholar] [CrossRef]
- Kawakatsu, Y.; Sugishita, T.; Oruenjo, K.; Wakhule, S.; Kibosia, K.; Were, E.; Honda, S. Determinants of Health Facility Utilization for Childbirth in Rural Western Kenya: Cross-Sectional Study. BMC Pregnancy Childbirth 2014, 14, 265. [Google Scholar] [CrossRef]
- Moshi, F.V.; Mbotwa, C.H. Determinants for Choice of Home Birth over Health Facility Birth among Women of Reproductive Age in Tanzania: An Analysis of Data from the 2015-16 Tanzania Demographic and Health Survey and Malaria Indicator Survey. BMC Pregnancy Childbirth 2020, 20, 561. [Google Scholar] [CrossRef]
- Fekadu, G.A.; Kassa, G.M.; Berhe, A.K.; Muche, A.A.; Katiso, N.A. The Effect of Antenatal Care on Use of Institutional Delivery Service and Postnatal Care in Ethiopia: A Systematic Review and Meta-Analysis. BMC Health Serv. Res. 2018, 18, 577. [Google Scholar] [CrossRef]
- Mwebesa, E.; Kagaayi, J.; Ssebagereka, A.; Nakafeero, M.; Ssenkusu, J.M.; Guwatudde, D.; Tumwesigye, N.M. Effect of Four or More Antenatal Care Visits on Facility Delivery and Early Postnatal Care Services Utilization in Uganda: A Propensity Score Matched Analysis. BMC Pregnancy Childbirth 2022, 22, 7. [Google Scholar] [CrossRef]
- Gabrysch, S.; Campbell, O.M. Still Too Far to Walk: Literature Review of the Determinants of Delivery Service Use. BMC Pregnancy Childbirth 2009, 9, 34. [Google Scholar] [CrossRef]
- Bain, L.E.; Aboagye, R.G.; Dowou, R.K.; Kongnyuy, E.J.; Memiah, P.; Amu, H. Prevalence and Determinants of Maternal Healthcare Utilisation among Young Women in Sub-Saharan Africa: Cross-Sectional Analyses of Demographic and Health Survey Data. BMC Public Health 2022, 22, 647. [Google Scholar] [CrossRef]
- Nesbitt, R.C.; Lohela, T.J.; Soremekun, S.; Vesel, L.; Manu, A.; Okyere, E.; Grundy, C.; Amenga-Etego, S.; Owusu-Agyei, S.; Kirkwood, B.R.; et al. The Influence of Distance and Quality of Care on Place of Delivery in Rural Ghana. Sci. Rep. 2016, 6, 30291. [Google Scholar] [CrossRef]
- Reynolds, H.W.; Luseno, W.K.; Speizer, I.S. The Measurement of Condom Use in Four Countries in East and Southern Africa. AIDS Behav. 2012, 16, 1044–1053. [Google Scholar] [CrossRef]
- Atusiimire, L.B.; Waiswa, P.; Atuyambe, L.; Nankabirwa, V.; Okuga, M. Determinants of Facility Based–Deliveries among Urban Slum Dwellers of Kampala, Uganda. PLoS ONE 2019, 14, e0214995. [Google Scholar] [CrossRef] [PubMed]
- Ayele, G.S.; Melku, A.T.; Belda, S.S. Utilization of Skilled Birth Attendant at Birth and Associated Factors among Women Who Gave Birth in the Last 24 Months Preceding the Survey in Gura Dhamole Woreda, Bale Zone, Southeast Ethiopia. BMC Public Health 2019, 19, 1501. [Google Scholar] [CrossRef] [PubMed]
- Budu, E.; Chattu, V.K.; Ahinkorah, B.O.; Seidu, A.-A.; Mohammed, A.; Tetteh, J.K.; Arthur-Holmes, F.; Adu, C.; Yaya, S. Early Age at First Childbirth and Skilled Birth Attendance during Delivery among Young Women in Sub-Saharan Africa. BMC Pregnancy Childbirth 2021, 21, 834. [Google Scholar] [CrossRef]
- Solanke, B.L.; Rahman, S.A. Multilevel Analysis of Factors Associated with Assistance during Delivery in Rural Nigeria: Implications for Reducing Rural-Urban Inequity in Skilled Care at Delivery. BMC Pregnancy Childbirth 2018, 18, 438. [Google Scholar] [CrossRef]
- Bessmertny, I.A.; Enkomaryam, B.C.; Mamuye, A.L. Determining the Critical Factors of Antenatal Care Follow-Up Using Two-Phase Machine Learning. In Proceedings of the 2024 XXVII International Conference on Soft Computing and Measurements (SCM), Saint Petersburg, Russia, 22–24 May 2024; pp. 316–319. [Google Scholar]
- Fredriksson, A.; Fulcher, I.R.; Russell, A.L.; Li, T.; Tsai, Y.-T.; Seif, S.S.; Mpembeni, R.N.; Hedt-Gauthier, B. Machine Learning for Maternal Health: Predicting Delivery Location in a Community Health Worker Program in Zanzibar. Front. Digit. Health 2022, 4, 855236. [Google Scholar] [CrossRef]
- Tesfaye, B.; Atique, S.; Azim, T.; Kebede, M.M. Predicting Skilled Delivery Service Use in Ethiopia: Dual Application of Logistic Regression and Machine Learning Algorithms. BMC Med. Inf. Decis. Mak. 2019, 19, 209. [Google Scholar] [CrossRef]
- Yehuala, T.Z.; Agimas, M.C.; Derseh, N.M.; Wubante, S.M.; Fente, B.M.; Yismaw, G.A.; Tesfie, T.K. Machine Learning Algorithms to Predict Healthcare-Seeking Behaviors of Mothers for Acute Respiratory Infections and Their Determinants among Children under Five in Sub-Saharan Africa. Front. Public Health 2024, 12, 1362392. [Google Scholar] [CrossRef]
- Ngusie, H.S.; Tesfa, G.A.; Taddese, A.A.; Enyew, E.B.; Alene, T.D.; Abebe, G.K.; Walle, A.D.; Zemariam, A.B. Predicting Place of Delivery Choice among Childbearing Women in East Africa: A Comparative Analysis of Advanced Machine Learning Techniques. Front. Public Health 2024, 12, 1439320. [Google Scholar] [CrossRef]
- Taye, E.A.; Woubet, E.Y.; Hailie, G.Y.; Arage, F.G.; Zerihun, T.E.; Zegeye, A.T.; Zeleke, T.C.; Kassaw, A.T. Application of the Random Forest Algorithm to Predict Skilled Birth Attendance and Identify Determinants among Reproductive-Age Women in 27 Sub-Saharan African Countries; Machine Learning Analysis. BMC Public Health 2025, 25, 901. [Google Scholar] [CrossRef]
- Andersen, R. Revisiting the Behavioral Model and Access to Medical Care: Does It Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Batista, G.E.A.P.A.; Monard, M.C. An Analysis of Four Missing Data Treatment Methods for Supervised Learning. Appl. Artif. Intell. 2003, 17, 519–533. [Google Scholar] [CrossRef]
- Memon, S.M.; Wamala, R.; Kabano, I.H. A Comparison of Imputation Methods for Categorical Data. Inform. Med. Unlocked 2023, 42, 101382. [Google Scholar] [CrossRef]
- Kuhn, M.; Johnson, K. Applied Predictive Modeling; Springer: New York, NY, USA, 2013; ISBN 978-1-4614-6848-6. [Google Scholar]
- Araf, I.; Idri, A.; Chairi, I. Cost-Sensitive Learning for Imbalanced Medical Data: A Review. Artif. Intell. Rev. 2024, 57, 80. [Google Scholar] [CrossRef]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic Minority over-Sampling Technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- He, H.; Bai, Y.; Garcia, E.A.; Li, S. ADASYN: Adaptive Synthetic Sampling Approach for Imbalanced Learning. In Proceedings of the 2008 IEEE International Joint Conference on Neural Networks (IEEE World Congress on Computational Intelligence), Hong Kong, China, 1–8 June 2008; pp. 1322–1328. [Google Scholar]
- Zou, H.; Hastie, T. Regularization and Variable Selection Via the Elastic Net. J. R. Stat. Soc. Ser. B Stat. Methodol. 2005, 67, 301–320. [Google Scholar] [CrossRef]
- Quinlan, J.R. C4. 5: Programs for Machine Learning; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy Function Approximation: A Gradient Boosting Machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. Xgboost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.-Y. Lightgbm: A Highly Efficient Gradient Boosting Decision Tree. In Proceedings of the Advances in Neural Information Processing Systems (NIPS 2017), Long Beach, CA, USA, 4–9 December 2017; Volume 30. [Google Scholar]
- Prokhorenkova, L.; Gusev, G.; Vorobev, A.; Dorogush, A.V.; Gulin, A. CatBoost: Unbiased Boosting with Categorical Features. In Proceedings of the Advances in Neural Information Processing Systems (NIPS 2018), Montréal, QC, Canada, 3–8 December 2018; Volume 31. [Google Scholar]
- Snoek, J.; Larochelle, H.; Adams, R.P. Practical Bayesian Optimization of Machine Learning Algorithms. In Proceedings of the Advances in Neural Information Processing Systems (NIPS 2012), Lake Tahoe, NV, USA, 3–6 December 2012; Volume 25. [Google Scholar]
- Salmi, M.; Atif, D.; Oliva, D.; Abraham, A.; Ventura, S. Handling Imbalanced Medical Datasets: Review of a Decade of Research. Artif. Intell. Rev. 2024, 57, 273. [Google Scholar] [CrossRef]
- Kumar, V.; Lalotra, G.S.; Sasikala, P.; Rajput, D.S.; Kaluri, R.; Lakshmanna, K.; Shorfuzzaman, M.; Alsufyani, A.; Uddin, M. Addressing Binary Classification over Class Imbalanced Clinical Datasets Using Computationally Intelligent Techniques. Healthcare 2022, 10, 1293. [Google Scholar] [CrossRef]
- Ghanem, M.; Ghaith, A.K.; El-Hajj, V.G.; Bhandarkar, A.; de Giorgio, A.; Elmi-Terander, A.; Bydon, M. Limitations in Evaluating Machine Learning Models for Imbalanced Binary Outcome Classification in Spine Surgery: A Systematic Review. Brain Sci. 2023, 13, 1723. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.-I. A Unified Approach to Interpreting Model Predictions. In Proceedings of the Advances in Neural Information Processing Systems (NIPS 2017), Long Beach, CA, USA, 4–9 December 2017; Volume 30. [Google Scholar]
- Dormann, C.F.; Elith, J.; Bacher, S.; Buchmann, C.; Carl, G.; Carré, G.; Marquéz, J.R.G.; Gruber, B.; Lafourcade, B.; Leitão, P.J.; et al. Collinearity: A Review of Methods to Deal with It and a Simulation Study Evaluating Their Performance. Ecography 2013, 36, 27–46. [Google Scholar] [CrossRef]
- He, H.; Garcia, E.A. Learning from Imbalanced Data. IEEE Trans. Knowl. Data Eng. 2009, 21, 1263–1284. [Google Scholar] [CrossRef]
- Johnson, J.M.; Khoshgoftaar, T.M. Survey on Deep Learning with Class Imbalance. J. Big Data 2019, 6, 27. [Google Scholar] [CrossRef]
- Walle, A.D.; Kebede, S.D.; Adem, J.B.; Mamo, D.N. Machine-Learning Algorithm to Predict Home Delivery after Antenatal Care Visit among Reproductive Age Women in East Africa. Front. Glob. Womens Health 2025, 6, 1461475. [Google Scholar] [CrossRef]
- Mlandu, C.; Matsena-Zingoni, Z.; Musenge, E. Predicting the Drop out from the Maternal, Newborn and Child Healthcare Continuum in Three East African Community Countries: Application of Machine Learning Models. BMC Med. Inform. Decis. Mak. 2023, 23, 191. [Google Scholar] [CrossRef]
- WHO. Intrapartum Care for a Positive Childbirth Experience; WHO Recommendations; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Babalola, S.; Fatusi, A. Determinants of Use of Maternal Health Services in Nigeria—Looking beyond Individual and Household Factors. BMC Pregnancy Childbirth 2009, 9, 43. [Google Scholar] [CrossRef]
- Namasivayam, A.; González, P.A.; Delgado, R.C.; Chi, P.C. The Effect of Armed Conflict on the Utilization of Maternal Health Services in Uganda: A Population-Based Study. PLoS Currents 2017, 9, ecurrents-dis. [Google Scholar] [CrossRef]

| Variable | Category | SBA Yes (74.73%) | SBA No (25.27%) | Total |
|---|---|---|---|---|
| Family Mobility | Native | 4201 (71.36%) | 1686 (28.64%) | 5887 |
| Internal Immigrant | 2981 (80.05%) | 743 (19.95%) | 3724 | |
| Residence | Rural | 5467 (70.82%) | 2253 (29.18%) | 7720 |
| Urban | 1715 (90.69%) | 176 (9.31%) | 1891 | |
| Region | Central | 1216 (78.91%) | 325 (21.09%) | 1541 |
| Kampala | 467 (96.09%) | 19 (3.91%) | 486 | |
| Northern | 1876 (76.95%) | 562 (23.05%) | 2438 | |
| Western | 1760 (70.26%) | 745 (29.74%) | 2505 | |
| Eastern | 1863 (70.54%) | 778 (29.46%) | 2641 | |
| Religion | Anglican | 2214 (73.87%) | 783 (26.13%) | 2997 |
| Catholic | 2929 (74.26%) | 1015 (25.74%) | 3944 | |
| Muslim | 966 (81.24%) | 223 (18.76%) | 1189 | |
| Other | 1073 (72.45%) | 408 (27.55%) | 1481 | |
| Literacy | None | 2542 (66.32%) | 1291 (33.68%) | 3833 |
| Partial | 886 (71.74%) | 349 (28.26%) | 1235 | |
| Complete | 3754 (82.63%) | 789 (17.37%) | 4543 | |
| Education Level | No Education | 789 (64.99%) | 425 (35.01%) | 1214 |
| Primary | 4147 (70.24%) | 1757 (29.76%) | 5904 | |
| Secondary | 2246 (90.09%) | 247 (9.91%) | 2493 | |
| Wealth Index | Poorest | 1608 (68.14%) | 752 (31.86%) | 2360 |
| Poorer | 1410 (69.7%) | 613 (30.3%) | 2023 | |
| Middle | 1372 (73.37%) | 498 (26.63%) | 1870 | |
| Richer | 1424 (79.51%) | 367 (20.49%) | 1791 | |
| Richest | 1368 (87.30%) | 199 (12.7%) | 1567 | |
| Age Group | 15–19 | 1235 (80.56%) | 298 (19.44%) | 1533 |
| 20–24 | 2136 (77.7%) | 613 (22.3%) | 2749 | |
| 25–29 | 1764 (75.51%) | 572 (24.49%) | 2336 | |
| 30–34 | 1088 (70.93%) | 446 (29.07%) | 1534 | |
| 35–39 | 684 (66.93%) | 338 (33.07%) | 1022 | |
| 40++ | 275 (62.93%) | 162 (37.07%) | 437 | |
| Employment Status | Not Working | 1206 (78.62%) | 328 (21.38%) | 1534 |
| Working | 5976 (73.99%) | 2101 (26.01%) | 8077 | |
| Marital Status | Currently in Union | 5910 (74.16%) | 2059 (25.84%) | 7969 |
| Formerly in Union | 819 (72.93%) | 304 (27.07%) | 1123 | |
| Never In Union | 453 (87.28%) | 66 (12.72%) | 519 | |
| SMB Sequence | MSB | 2987 (72.59%) | 1128 (27.41%) | 4115 |
| SBM | 1191 (78.30%) | 330 (21.70%) | 1521 | |
| SMB | 2551 (73.81%) | 905 (26.19%) | 3456 | |
| SBnoM | 453 (87.28%) | 66 (12.72%) | 519 | |
| Family Type | Monogamous | 4468 (74.77%) | 1508 (25.23%) | 5976 |
| Polygamous | 1442 (72.35%) | 551 (27.65%) | 1993 | |
| Not In Union | 1272 (77.47%) | 370 (22.53%) | 1642 | |
| Household Size | 1–4 | 2555 (78.62%) | 695 (21.38%) | 3250 |
| 5–8 | 3554 (72.63%) | 1339 (27.37%) | 4893 | |
| >8 | 1073 (73.09%) | 395 (26.91%) | 1468 | |
| Sex Household Head | Female | 1906 (76.15%) | 597 (23.85%) | 2503 |
| Male | 5276 (74.23%) | 1832 (25.77%) | 7108 | |
| Age of Household Head | <25 | 738 (75.93%) | 234 (24.07%) | 972 |
| 25–29 | 1333 (77.05%) | 397 (22.95%) | 1730 | |
| 30–49 | 3990 (73.06%) | 1471 (26.94%) | 5461 | |
| 50++ | 1121 (77.42%) | 327 (22.58%) | 1448 | |
| Radio Ownership | No | 2977 (70.51%) | 1245 (29.49%) | 4222 |
| Yes | 4205 (78.03%) | 1184 (21.97%) | 5389 | |
| Television Ownership | No | 5933 (71.65%) | 2347 (28.35%) | 8280 |
| Yes | 1249 (93.84%) | 82 (6.16%) | 1331 | |
| Mobile Ownership | No | 3895 (68.84%) | 1763 (31.16%) | 5658 |
| Yes | 3287 (83.15%) | 666 (16.85%) | 3953 | |
| Bank Account Ownership | No | 6262 (73.27%) | 2285 (26.73%) | 8547 |
| Yes | 920 (86.47%) | 144 (13.53%) | 1064 | |
| Internet Use | No | 6708 (73.52%) | 2416 (26.48%) | 9124 |
| Yes | 474 (97.33%) | 13 (2.67%) | 487 | |
| Reading Newspaper | At Least Once a Week | 536 (92.89%) | 41 (7.11%) | 577 |
| Less Than Once a Week | 852 (86.23%) | 136 (13.77%) | 988 | |
| Not At All | 5794 (72.01%) | 2252 (27.99%) | 8046 | |
| Listening To Radio | At Least Once a Week | 4213 (77.4%) | 1230 (22.6%) | 5443 |
| Less Than Once a Week | 1170 (77.02%) | 349 (22.98%) | 1519 | |
| Not At All | 1799 (67.91%) | 850 (32.09%) | 2649 | |
| Watching Tv | At Least Once a Week | 1303 (91.25%) | 125 (8.75%) | 1428 |
| Less Than Once a Week | 741 (79.25%) | 194 (20.75%) | 935 | |
| Not At All | 5138 (70.89%) | 2110 (29.11%) | 7248 | |
| Health Insurance | No | 7089 (74.56%) | 2419 (25.44%) | 9508 |
| Yes | 93 (90.29%) | 10 (9.71%) | 103 | |
| Partner Education Level | No Education | 436 (68.55%) | 200 (31.45%) | 636 |
| Primary | 3001 (67.94%) | 1416 (32.06%) | 4417 | |
| Secondary | 2473 (84.81%) | 443 (15.19%) | 2916 | |
| Not In Union | 1272 (77.47%) | 370 (22.53%) | 1642 | |
| Partner Employment Status | Not Working | 194 (68.55%) | 89 (31.45%) | 283 |
| Working | 5716 (74.37%) | 1970 (25.63%) | 7686 | |
| Not In Union | 1272 (77.47%) | 370 (22.53%) | 1642 | |
| Healthcare Facility Visit in the Past Year | No | 1415 (71.11%) | 575 (28.89%) | 1990 |
| Yes | 5767 (75.67%) | 1854 (24.33%) | 7621 | |
| Healthcare Cost | Big Problem | 3337 (70.64%) | 1387 (29.36%) | 4724 |
| Not A Big Problem | 3845 (78.68%) | 1042 (21.32%) | 4887 | |
| Distance To Healthcare Facility | Big Problem | 2704 (67.67%) | 1292 (32.33%) | 3996 |
| Not A Big Problem | 4478 (79.75%) | 1137 (20.25%) | 5615 | |
| Healthcare Decision-Making | Husband/Partner Alone | 1581 (73.36%) | 574 (26.64%) | 2155 |
| Respondent Alone | 1697 (73.78%) | 603 (26.22%) | 2300 | |
| Respondent And Husband/Partner | 2632 (74.9%) | 882 (25.1%) | 3514 | |
| Not In Union | 1272 (77.47%) | 370 (22.53%) | 1642 | |
| Expenditures Decision-Making | Husband/Partner Alone | 2086 (73.17%) | 765 (26.83%) | 2851 |
| Respondent Alone | 883 (72.32%) | 338 (27.68%) | 1221 | |
| Respondent And Husband/Partner | 2941 (75.47%) | 956 (24.53%) | 3897 | |
| Not In Union | 1272 (77.47%) | 370 (22.53%) | 1642 |
| Variable | Category | SBA Yes (74.73%) | SBA No (25.27%) | Total |
|---|---|---|---|---|
| Contraception Use | No | 1968 (68.76%) | 894 (31.24%) | 2862 |
| Yes | 5214 (77.26%) | 1535 (22.74%) | 6749 | |
| Wanted Pregnancy | No | 3118 (72.56%) | 1179 (27.44%) | 4297 |
| Yes | 4064 (76.48%) | 1250 (23.52%) | 5314 | |
| Wanting Same Number of Children as Husband/Partner | No | 2542 (72.94%) | 943 (27.06%) | 3485 |
| Yes | 2267 (78.01%) | 639 (21.99%) | 2906 | |
| Don’t Know | 1101 (69.77%) | 477 (30.23%) | 1578 | |
| Not In Union | 1272 (77.47%) | 370 (22.53%) | 1642 | |
| Children Ever Born | 1 | 1595 (86.73%) | 244 (13.27%) | 1839 |
| 2–4 | 3332 (76.76%) | 1009 (23.24%) | 4341 | |
| 5++ | 2255 (65.72%) | 1176 (34.28%) | 3431 | |
| Birth Interval (Years) | <2 | 1203 (70.43%) | 505 (29.57%) | 1708 |
| 2–3 | 2048 (67.55%) | 984 (32.45%) | 3032 | |
| >3 | 2335 (77.04%) | 696 (22.96%) | 3031 | |
| First Birth | 1596 (86.74%) | 244 (13.26%) | 1840 | |
| Age at First Sex | Early | 1211 (67.84%) | 574 (32.16%) | 1785 |
| Moderate | 3579 (74.04%) | 1255 (25.96%) | 4834 | |
| Late | 2392 (79.95%) | 600 (20.05%) | 2992 | |
| Age at First Birth | <18 | 2611 (70.85%) | 1074 (29.15%) | 3685 |
| 18–24 | 4202 (76.65%) | 1280 (23.35%) | 5482 | |
| >25 | 369 (83.11%) | 75 (16.89%) | 444 | |
| Number of ANC Visits | None | 119 (45.08%) | 145 (54.92%) | 264 |
| 1–3 | 2431 (67.40%) | 1176 (32.60%) | 3607 | |
| 4++ | 4632 (80.70%) | 1108 (19.30%) | 5740 | |
| First Trimester ANC | No | 4737 (73.07%) | 1746 (26.93%) | 6483 |
| Yes | 2281 (81.23%) | 527 (18.77%) | 2808 | |
| No ANC | 164 (51.25%) | 156 (48.75%) | 320 | |
| Pregnancy Duration (Months) | <9 | 1117 (79.62%) | 286 (20.38%) | 1403 |
| 9 | 5464 (73.82%) | 1938 (26.18%) | 7402 | |
| >9 | 601 (74.57%) | 205 (25.43%) | 806 | |
| Place of Delivery | Health facility | 6971 (98.24) | 125 (1.76) | 7096 |
| Not at health facility | 211 (8.39) | 2304 (91.61) | 2515 |
| Method | Precision | Recall | F1-Score | Accuracy | AUC |
|---|---|---|---|---|---|
| Logistic Regression | 0.39 | 0.76 | 0.51 | 0.64 | 0.7364 |
| Random Forest | 0.40 | 0.71 | 0.51 | 0.66 | 0.7413 |
| Gradient Boosting | 0.40 | 0.74 | 0.52 | 0.65 | 0.7442 |
| XGBoost | 0.40 | 0.73 | 0.52 | 0.66 | 0.7473 |
| LightGBM | 0.43 | 0.67 | 0.52 | 0.69 | 0.7424 |
| Decision Tree | 0.40 | 0.66 | 0.50 | 0.66 | 0.7121 |
| CatBoost | 0.41 | 0.70 | 0.52 | 0.67 | 0.7464 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Memon, S.M.Z.; Wamala, R.; Kabano, I.H. Identifying Predictors of Utilization of Skilled Birth Attendance in Uganda Through Interpretable Machine Learning. Int. J. Environ. Res. Public Health 2025, 22, 1691. https://doi.org/10.3390/ijerph22111691
Memon SMZ, Wamala R, Kabano IH. Identifying Predictors of Utilization of Skilled Birth Attendance in Uganda Through Interpretable Machine Learning. International Journal of Environmental Research and Public Health. 2025; 22(11):1691. https://doi.org/10.3390/ijerph22111691
Chicago/Turabian StyleMemon, Shaheen M. Z., Robert Wamala, and Ignace H. Kabano. 2025. "Identifying Predictors of Utilization of Skilled Birth Attendance in Uganda Through Interpretable Machine Learning" International Journal of Environmental Research and Public Health 22, no. 11: 1691. https://doi.org/10.3390/ijerph22111691
APA StyleMemon, S. M. Z., Wamala, R., & Kabano, I. H. (2025). Identifying Predictors of Utilization of Skilled Birth Attendance in Uganda Through Interpretable Machine Learning. International Journal of Environmental Research and Public Health, 22(11), 1691. https://doi.org/10.3390/ijerph22111691







