Abstract
Child undernutrition persists in Cambodia despite recent progress. As Cambodia undergoes a shift in dietary consumption that coincides with economic, demographic, and epidemiologic changes, there is risk of ultra-processed foods and sugar-sweetened beverages displacing nutrient-dense foods during the critical period of infant growth in the first 24 months. The aim of this study was to assess the introduction and intake of foods of low nutritional value and sugar-sweetened beverages and their association with undernutrition among children 24 months of age in rural and semi-urban Cambodia. Cross-sectional analyses of a 24-h dietary recall from a sample (n = 377) of 24-month-olds found that the majority of infants had been introduced to packaged salty snacks and sweets by 12 months of age and to sugar-sweetened beverages by 15 months. By 24 months of age, 78% of children had consumed foods of low nutritional value and 57% consumed a sugar-sweetened beverage on the previous day. Multivariate logistic regression analyses demonstrated that infant intake of a flavored sugary drink on the previous day was associated with over two times the odds of both stunting and wasting, and consumption of packaged sweets on the previous day was associated with over two times the odds of wasting, but no association was found with stunting. These findings underscore the need to improve educational and policy interventions to support healthy feeding practices for infants and young children.
1. Introduction
Globally, 22% of children under the age of five suffer from stunting (low height-for-age) and 6.7% from wasting (low weight-for-height), with higher proportions in low-income countries [1]. Child undernutrition continues to represent a significant global public health problem that contributes to an estimated 45% of child deaths and has significant adverse implications for children’s physical, cognitive, and behavioral development during childhood and later in life [2].
Cambodia, a rapidly developing lower-middle income country, has made considerable improvements in child nutrition over the past two decades [3]. However, approximately 22% of children under the age of five years are still stunted and 10% are still wasted [3]. Furthermore, infant and young child feeding practices (IYCF) in Cambodia are inadequate. Among children 6–23 months, only 42% met the minimum acceptable diet according to the World Health Organization (WHO) IYCF guidelines [3,4]. Since the first 1000 days from conception through age two are a critical period to reduce stunting, improving IYCF practices during this time is essential [5]. Specifically, the WHO recommends exclusive breastfeeding in the first 6 months of life and introduction of nutritionally adequate complementary foods from 6–23 months [4].
Like many low- and middle-income countries, Cambodia’s rapid economic growth has been accompanied by a transition away from traditional dietary patterns towards westernized diets, including ultra-processed foods with added sugars, fats, and refined carbohydrates and sugar-sweetened beverages (SSBs) [6]. Rising consumption of these unhealthy foods and beverages by Cambodian children has been documented in the most recent Cambodia Demographic and Health Survey, which found that among children 6–23 months, 21% consumed unhealthy foods, 28% consumed sweet beverages, and 29% consumed no vegetables or fruits on the previous day [3]. High consumption of unhealthy snack foods and beverages has been associated with lower nutrient intake and stunting among children in LMICs [7,8]. One explanation for this is that unhealthy foods and beverages may displace nutrient-dense foods that are critical during the first two years of life [7,9]. Other studies have demonstrated that increased consumption of ultra-processed foods has been associated with a higher prevalence of overweight/obesity and cardiometabolic comorbidities among children [10] and that high SSB consumption is associated with an increased risk for type 2 diabetes [11]. Given the persistence of undernutrition in Cambodia and rising rates of child obesity throughout Asia [12], consumption of unhealthy foods and sugar-sweetened beverages may have important implications for the concurrent development of undernutrition and obesity in Cambodia [13,14,15].
There is a need for further investigation of the health impacts of infants’ consumption of foods of low nutritional value, such as ultra-processed foods and sugar-sweetened beverages, particularly in rural and semi-urban Cambodia, where the majority of these infants reside. While there is a growing body of nutrition research in Cambodia, few studies have explicitly examined the introduction and frequency of consumption of different categories of low nutritional value foods and beverages and the association with malnutrition [16]. The aim of this study was to assess the consumption of foods of low nutritional value and sugar-sweetened beverages, as well as the association of intake of these foods and beverages with undernutrition among children 24 months of age in rural and semi-urban Cambodia.
2. Materials and Methods
This is a cross-sectional, secondary analysis of data collected through Cambodia SMILE, a pilot study that aimed to determine the effectiveness of a community-based health promotion program to reduce dental caries in children from infancy to 24 months of age. It included an intervention arm that received an oral health intervention (fluoride application, oral health education) and a control arm [17]. The protocol was approved by the National Ethics Committee for Health Research (NECHR #0306) under the Ministry of Health in Cambodia.
Cambodia SMILE recruited child-caregiver dyads from community health centers in rural and semi-urban districts of Kampong Speu Province. Rural and semi-urban districts were selected as this is where the majority of infant-aged children live; additionally, as the study was conducted in conjunction with the Ministry of Health and Cambodian government, the study districts were selected by these government stakeholders. Data were collected from 2015 to 2017 by trained primary healthcare providers at child ages of 9, 12, 15, 18, and 24 months using research examination forms (Supplementary File S1). After informed consent was obtained, caregivers were interviewed in the Khmer language by trained native-speaking interviewers. Basic sociodemographic data including parent occupation, income (reported in Cambodian riels then converted to United States dollars (USD)), parent age, parent education, and household characteristics were collected. At each study visit, caregivers were asked if they had introduced various foods and beverages, and if so, the age (in months) at which the child was first exposed to the following list: dietary staples (rice, meat, vegetables, fruit, egg); foods of low nutritional value (FLNV) (packaged salty snacks, such as crackers; packaged sweets, such as candy and cookies; and Khmer sweet cake—a traditional Cambodian rice cake that is typically made of glutinous rice flour dough and palm sugar); low- or no-sugar added beverages (water, breastmilk, bottled milk formula); and SSBs (flavored sugary drinks without nutrient content which included fruit juices, sodas, and syrups; and sugar-sweetened drinks with some nutrient content, including sweetened condensed milk, sweetened soy milk, and sweetened rice water). Caregivers also reported the frequency of consumption by the child on the previous day of selected foods at specific time points (morning, middle of the day, afternoon, evening, and night); the methodology was comparable to a food frequency questionnaire isolated to the last 24 h. The food list for the questionnaire was adapted from a prior study by Turton et al. [18] focused on foods and beverages associated with the development of dental caries among children including those most commonly consumed. A “packaged food” variable was created by combining packaged salty snacks and packaged sweets. The study population for this secondary analysis consists of a sub-sample of 377 children and their caregivers and uses data collected at the 24-month follow-up only.
Trained researchers assessed each child’s length/height and weight at the 24-month visit, including recumbent length in children under 2 years of age or unable to stand up and height of children aged 2 years and older; weight was measured with a calibrated precise scale. Children were measured twice and the mean value was used according to WHO guidelines [19]. The following anthropometrics were calculated according to WHO Child Growth Standards [19]: length/height-for-age z-score/height-for-age z-score (LAZ/HAZ), weight-for-age z-score (WAZ), BMI-for-age z-score (BAZ), and weight-for-height z-score (WHZ). Child malnutrition status was categorized as stunted (LAZ/HAZ < −2 SD below median), wasted (WHZ < −2 SD below median), and underweight (WAZ < −2 SD below median).
The control and intervention data from the original Cambodia SMILE study were merged to increase the sample size for the secondary analysis. A sensitivity analysis was conducted to confirm the robustness of the findings by analyzing the original control and intervention groups separately using the same multivariate models (Supplementary Tables S1 and S2). Cases with relevant missing data were excluded from the logistic regressions.
Data were entered into, cleaned, and analyzed in STATA 15 SE. Tables for the sensitivity analysis and figures were created in R (version 4.3.0). Descriptive analyses assessed the sociodemographic and nutritional characteristics of the study population, as well as the introduction and previous-day consumption of the selected foods and beverages. Bivariate associations of FLNV and SSB—based on any consumption (binary) as well as increasing levels of consumption (ordinal)—were examined. Within the SSB category, only the subcategory of flavored sugary drinks met our criteria for inclusion in multivariate analysis (i.e., bivariate p-value < 0.20). We then performed staged multivariable models. An initial multivariable model examined the associations of stunting and wasting with sociodemographic variables, with p < 0.20 resulting in a final base model including child sex, household income, and maternal occupation, as well as a variable indicating subject intervention in the original Cambodia SMILE study. Statistical significance was considered for p-values < 0.05.
3. Results
3.1. Sociodemographic and Nutritional Status Characteristics
Children had a mean age of 22.7 months, with approximately equal representation of sexes (Table 1). Most families were low-income, with a monthly household income less than $250 (average GDP per capita in Cambodia for the period of data collection—2015–2017—was $1284 [20]). Most parents had a primary school level of education or less, and rural and semi-urban households were nearly equally represented.

Table 1.
Sociodemographic, health, and nutritional status characteristics of study population.
Many children experienced undernutrition, with 43% of the infants being stunted, 16% being wasted, and 27% being underweight.
3.2. First Introduction of Foods and Beverages
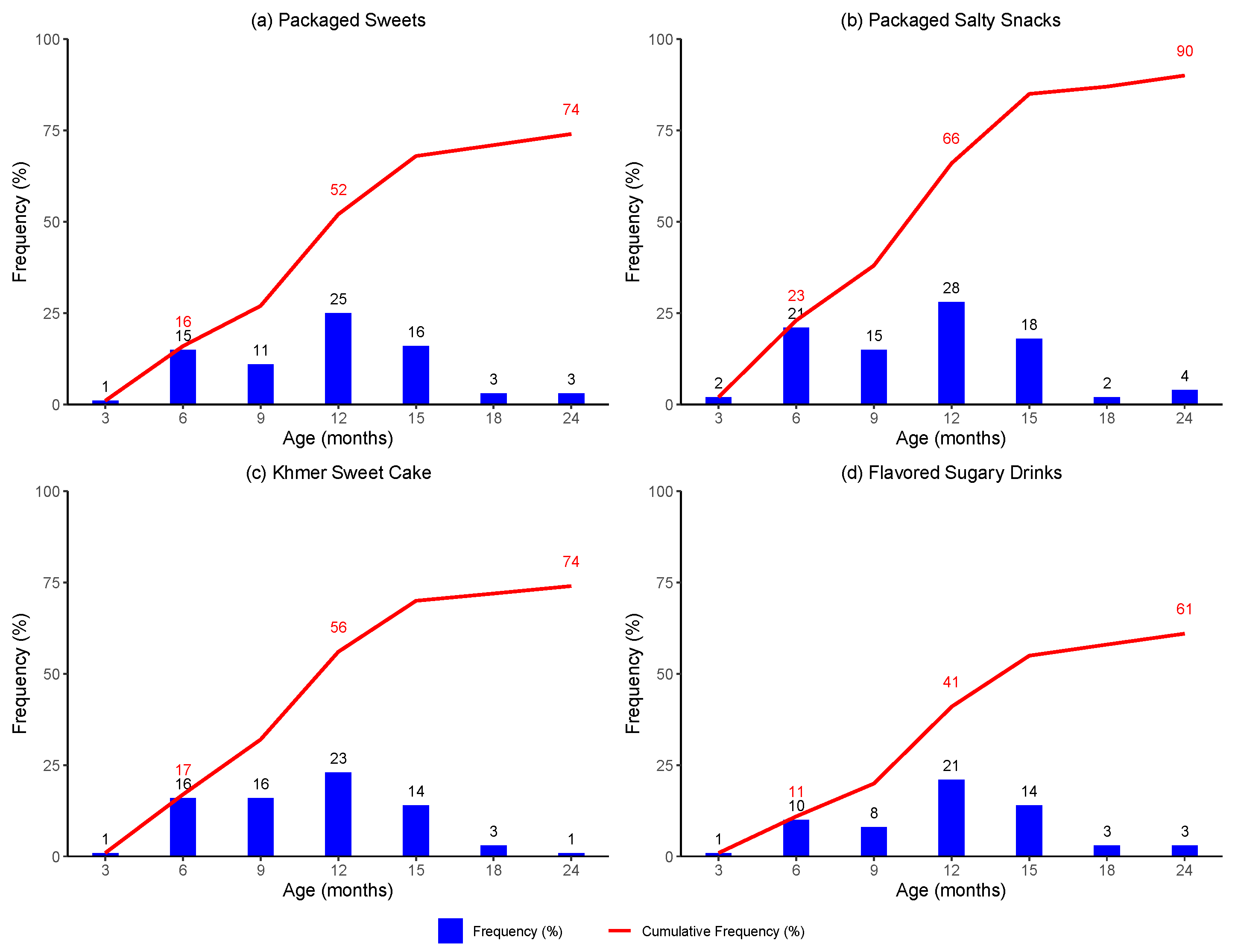
By 3 months of age, very few children had been introduced to the specified foods and beverages, except milk formula and water (Figure 1). Roughly a quarter of caregivers reported introducing their child to milk formula and slightly less than one-third reported introducing their child to water.
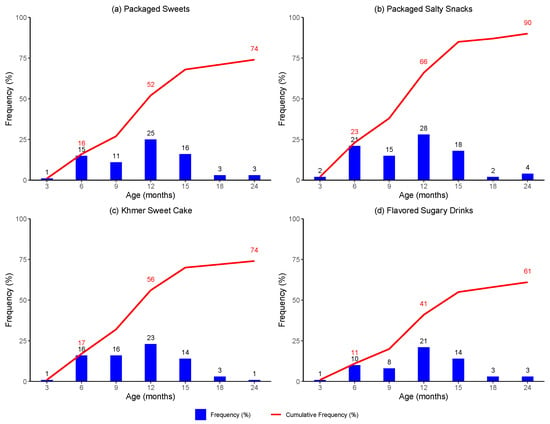
Figure 1.
Introduction to selected food and beverage products by age in months.
By 6 months of age, a larger proportion of infants had been introduced to a wider variety of foods and beverages. A substantial proportion of infants (11–23%) had been introduced to foods of low nutritional value, including packaged sweets, packaged salty snacks, and Khmer sweet cake, and to flavored sugary drinks.
By 12 months of age, a greater proportion of children had been introduced to all selected foods and beverages. Over half of children had been introduced to packaged sweets and Khmer sweet cake and two-thirds had been introduced to packaged salty snacks. Likewise, nearly half of children had been introduced to flavored sugary drinks.
By 24 months of age, the majority of children had been introduced to FLNV and SSB. Three-quarters of children had been introduced to packaged sweets and Khmer sweet cake, while almost all had been introduced to packaged salty snacks. Finally, almost two-thirds of children had been introduced to flavored sugary drinks.
3.3. Frequency of Reported Food and Beverage Intake at 24 Months
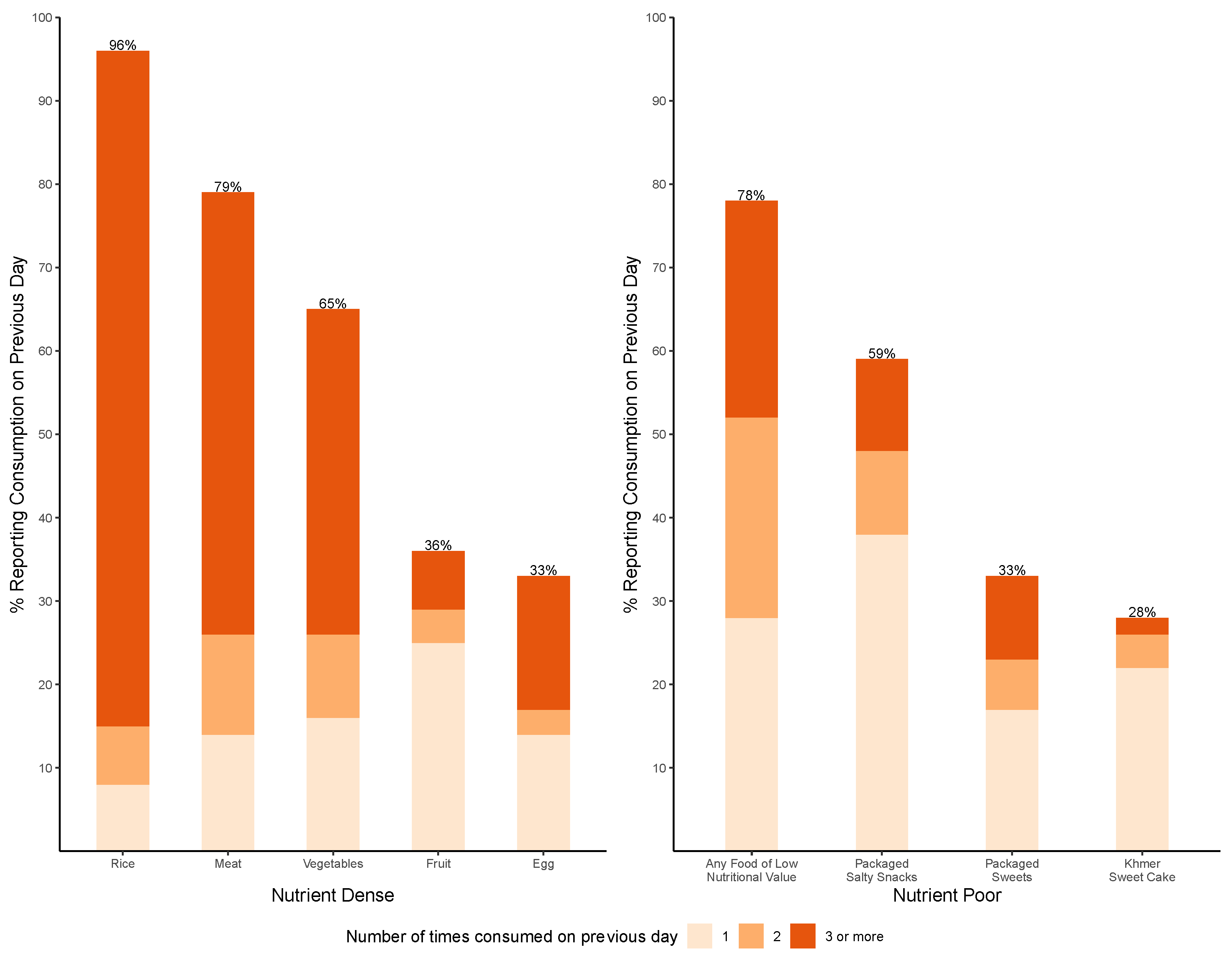
At 24 months of age, reported consumption of selected foods on the previous day shows that most children had consumed rice or rice porridge (96%), meat (79%), and vegetables (65%) (Figure 2). In addition, over three-quarters (78%) of children had consumed at least one FLNV, making it the third most frequently consumed food category; and over one-quarter had consumed an FLNV three or more times on the previous day. The most commonly consumed FLNV were packaged salty snacks (59%), followed by packaged sweets (33%) and Khmer sweet cake (28%).
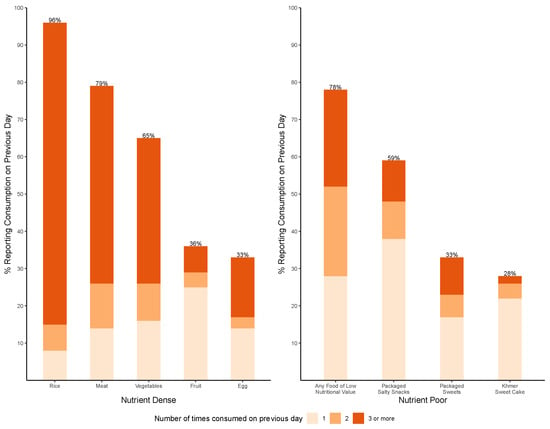
Figure 2.
Frequency of consumption of reported foods on previous day at 24 months of age.
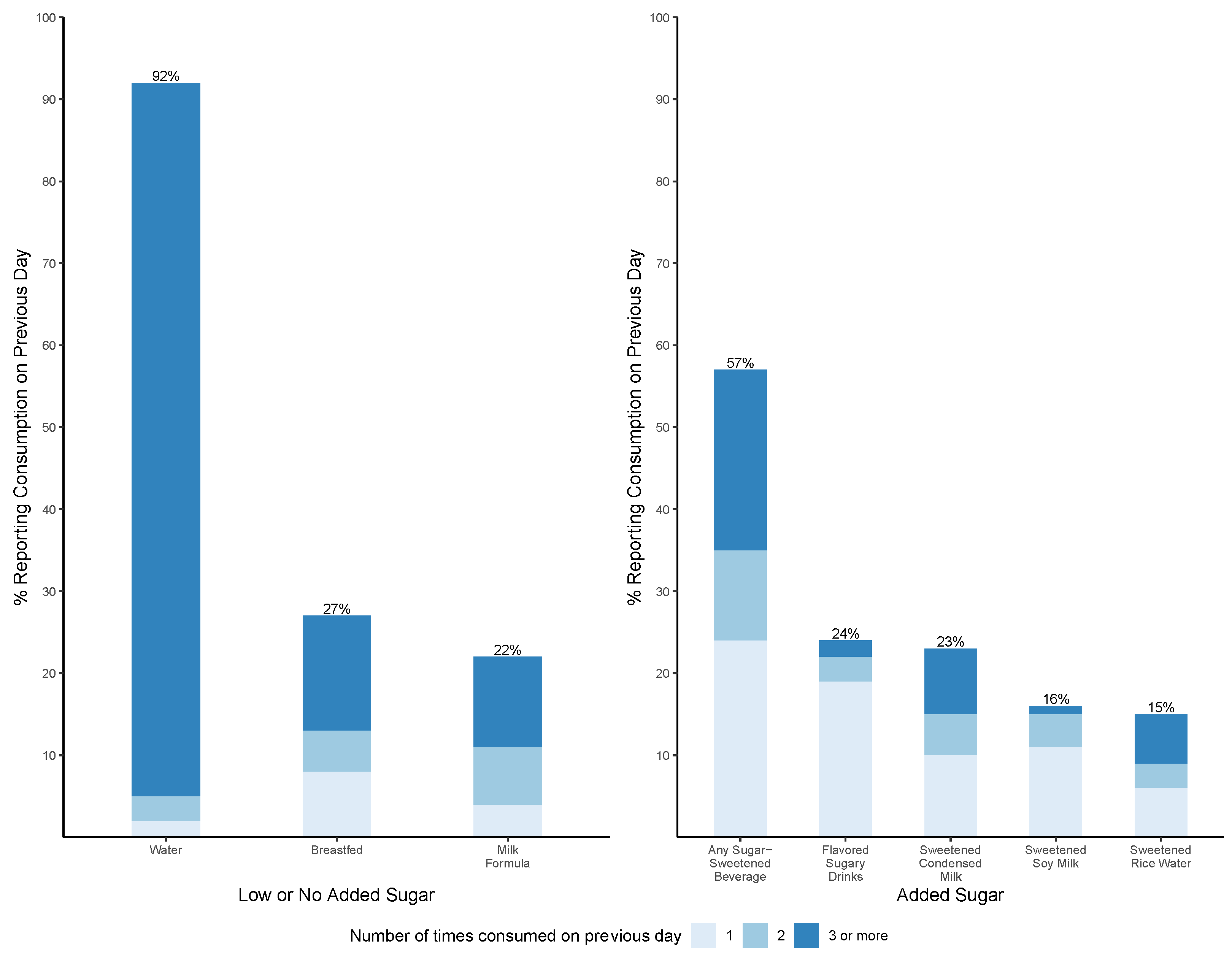
At 24 months of age, reported consumption of selected beverages on the previous day shows that the majority (92%) drank water, and approximately one-quarter were breastfed (27%) and given milk formula (22%) (Figure 3). Furthermore, over half (57%) of children had consumed at least one SSB, and one-fifth had consumed an SSB three or more times on the previous day. The most commonly consumed SSBs were flavored sugary drinks (24%) and sweetened condensed milk (23%).
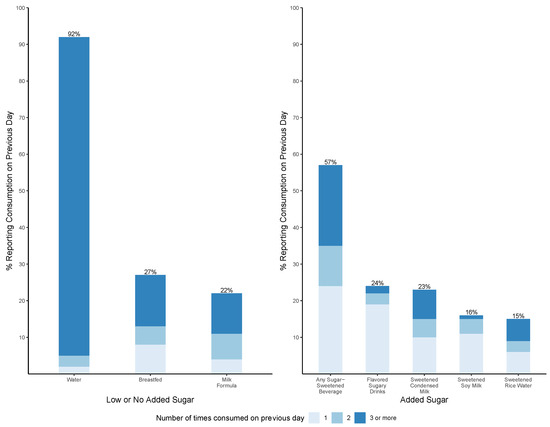
Figure 3.
Frequency of consumption of reported beverages on previous day at 24 months of age.
3.4. Association between Food and Beverage Intake and Stunting at 24 Months of Age
At 24 months, consumption of a flavored sugary drink on the previous day was significantly associated with higher odds of stunting in the adjusted model (OR 2.02; 95% CI [1.18, 3.43]) (Table 2). This association was driven by the control group after sensitivity analysis (Supplementary Table S1). There was a trend towards decreased odds of stunting with increased levels of consumption of any FLNV or any packaged salty snacks on the previous day. This trend appears to be primarily driven by the intervention subgroup in which consumption of higher levels of FLNV or packaged salty snacks was significantly associated with decreased odds of stunting (Supplementary Table S1).

Table 2.
Association between flavored sugary drinks and foods of low nutritional value consumed on previous day and stunting at 24 months †.
3.5. Association between Food and Beverage Intake and Wasting at 24 Months of Age
At 24 months, consumption of a flavored sugary drink on the previous day was significantly associated with greater odds of wasting in adjusted models (OR 2.21; 95% CI [1.20, 4.08]) (Table 3). Higher odds of wasting was associated with consumption of two FLNV on the previous day (i.e., Khmer sweet cake, packaged salty snack, or packaged sweet) compared to no FLNV consumption on the previous day (OR 2.64; 95% CI [1.10, 6.33]). This finding appeared to be primarily driven by the intervention subgroup (Supplementary Table S2). In addition, higher odds of wasting was associated with consumption of one packaged sweet on the previous day compared to no consumption of packaged sweets on the previous day (OR 2.22; 95% CI [1.11, 4.44]). The directionality of these relationships observed in the overall cohort were maintained in the sensitivity analysis (Supplementary Table S2).

Table 3.
Association between flavored sugary drinks and foods of low nutritional value consumed on the previous day and wasting at 24 months †.
4. Discussion
In this study sample from rural and semi-urban Cambodia, a substantial proportion of children had been introduced to sugar-sweetened beverages and/or ultra-processed snacks in the first 6 months of life, contrary to WHO IYCF guidelines [4]. Cumulative introduction to these unhealthy foods and beverages increased steadily with age. The majority of children had been introduced to packaged salty snacks and packaged sweets by 12 months and to sugar-sweetened beverages by 15 months. By 24 months, three-quarters of children consumed foods of low nutritional value on the previous day. Compared to nutrient-dense foods, foods of low nutritional value at this age were consumed at higher frequency than vegetables and fruits and almost equal frequency to meat. Additionally, at 24 months, one-half of children consumed a sugar-sweetened beverage on the previous day.
Multivariate logistic regression analysis demonstrated that prior-day child intake of a flavored sugary drink was significantly associated with over two times the odds of both stunting and wasting, and prior-day consumption of one packaged sweet was associated with over two times the odds of wasting. The association between increased odds of stunting and prior day consumption of a flavored sugary drink was largely driven by the control subgroup (Supplementary Table S1). This may be due to a social desirability bias resulting in under reporting of flavored sugary drink intake among the intervention subgroup participants who received education on the relationship between sugar intake and dental caries.
This study also found a trend towards decreased stunting with increased number of FLNV and any packaged salty snack consumed on the prior day. This protective association may be related to the specific types and quantity of packaged salty snacks consumed, which our study did not examine in detail. We hypothesize that perhaps children who ate more packaged salty snacks—that had been purchased—were from families with higher income, which might have afforded access to more nutritious foods for the mothers during pregnancy as well as their young children; and therefore, this association may be confounded by income in a way that we were unable to demonstrate in this study. Prior studies in India have demonstrated similar findings with lower rates of stunting and wasting with higher rates of junk food consumption (Athavale et al., 2020) [21]. Sensitivity analysis demonstrated that this trend was largely driven by the intervention subgroup and, moreover, that within the intervention subgroup the opposite directionality was seen with the consumption of these foods and increased odds of wasting. Since stunting is a measure of chronic malnutrition and wasting is a measure of acute malnutrition, this opposing directionality may reflect recency differences in terms of when children were consuming these foods that this study was not designed to capture.
The infant and young child feeding practices in this sample are contrary to the World Health Organization and UNICEF recommendations to exclusively breastfeed infants for the first 6 months, and from 6–23 months to introduce nutritionally adequate complementary solid foods including daily fruits and vegetables and to avoid ultra-processed foods and sugar-sweetened drinks [4]. Our finding that most children frequently consumed foods of low nutritional value and sugary drinks indicates that these unhealthy products have become a staple of infant diets in rural and semi-urban Cambodia. These findings are consistent with previous studies in Cambodia and other low- and middle-income countries [14,22,23,24]. Data collection for this study was performed between 2015–2017, yet remains consistent with more recent analysis from Hinnouho et al. [25] demonstrating high rates of commercial food consumption among infants and with the most recent Cambodia Demographic and Health Survey [3].
Though the prevalence of undernutrition among infants and children has declined significantly in Cambodia since the time of data collection for this study (2015–2017), Cambodia continues to have unacceptably high rates of stunting and wasting [3]. At 24 months of age, the association between prior-day consumption of sugar-sweetened beverages with significantly increased odds of stunting and wasting is likely explained by evidence that non-nutritious diets reported at 24 months reflect a longstanding pattern of non-nutritious diets at earlier infant ages [25]; and, over the first 2 years of life, the cumulative impact of sugary drinks and non-nutritious snack foods displacing nutrient-dense foods and beverages can lead to stunting and wasting [26,27]. Factors that contribute to this displacement include the increasing marketing and availability of low-cost and convenient processed foods and beverages and the subsequent development of taste preferences for these food products among young children [21,28,29,30,31,32]. Children with high sugar intake have been found to consume less protein, total fat, and key vitamins compared to those with low sugar intake [33]. Other studies have found that high consumption of ultra-processed foods and sugar-sweetened beverages corresponded to low dietary diversity [34], which in turn has been associated with stunting [35,36], and greater dietary diversity has been associated with higher HAZ scores [37,38].
The association between high sugar intake and undernutrition may also be mediated by dental caries. Early and frequent consumption of sugary drinks and snacks is known to cause dental caries [39], and dental caries have been shown to be associated with increased risk of stunting and wasting in low- and middle-income countries, including Cambodia [40,41,42,43]. The hypothesized mechanisms include chronic oral infection/inflammation, oral pain, difficulty eating and sleeping, and disruption of the hypothalamic–pituitary–adrenal axis [44,45,46].
In all, these findings of unhealthy children’s diets and associations with stunting and wasting are particularly concerning as similar dietary shifts throughout Asia have contributed to a double burden of malnutrition—with undernutrition persisting alongside obesity at the individual, household, and population level—placing children at risk of poor growth and development as well as non-communicable diseases (NCDs) such as diabetes and cardiovascular disease [47,48,49,50,51]. Displacement of nutrient-dense foods due to excessive intake of saturated fats and consumption of foods high in added sugars may play a role in measures of overnutrition [52] as well as undernutrition. It is therefore critical to develop effective measures to improve infant diets, including programs for caregiver and child education on healthy food and beverage choices, as well as policies to limit the sale of sugary drinks and ultra-processed food products, and to provide families with better access to affordable nutrient-rich food and beverage options.
Limitations of this study include purposive sampling and small sample size, which limits the generalizability of the findings, and its cross-sectional design, which precludes the ability to make causal inferences. Survey responses may be affected by recall and social desirability bias. While sensitivity analysis confirmed the directionality of the observed associations, the potential for unmeasured confounding remains. Additionally, the dietary questionnaire was not developed according to WHO Infant and Young Child Feeding (IYCF) guidelines, nor was it validated against other previously validated dietary survey instruments [53,54], limiting further detailed nutritional analysis. The strengths of this study include its contribution to the literature regarding the introduction and frequency of consumption of packaged foods and sugar-sweetened beverages in addition to nutrient-dense foods in children’s diets and the significant associations between consumption of sugary beverages and foods of low nutritional value with increased odds of stunting and wasting. Future studies should explore other variables such as food and beverage composition and portion size using a culturally appropriate validated survey instrument and maternal health characteristics such as BMI, tobacco use, and intergenerational malnutrition resulting from famine during the Khmer Rouge era. In addition, mediation analysis could be utilized to capture more nuanced effects of diet—especially the unique role of sugar—on anthropometric measures, particularly stunting, and to elucidate mediating mechanisms such as nutrient displacement and dental caries.
5. Conclusions
This study found that children in rural and semi-urban Cambodia were introduced to foods of low nutritional value and sugar-sweetened beverages at very young ages, and these products have become a routine part of the infant and young child diet, in contrast to IYCF guidelines. Furthermore, consumption of these products was significantly associated with over two-fold odds of stunting and wasting. While more detailed investigation of the consumption of specific products remains to be conducted, more effective educational and policy interventions are needed to promote healthy IYCF practices and reduce consumption of sugary beverages and commercially packaged foods of low nutritional value.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph21020169/s1, File S1: Survey Instrument and Examination Form; Table S1: Association between flavored sugary drinks and foods of low nutritional value and stunting at 24 months stratified by original Cambodia SMILE study group assignment; Table S2: Association between flavored sugary drinks and foods of low nutritional value and wasting at 24 months stratified by original Cambodia SMILE study group assignment.
Author Contributions
All authors made significant contributions to the conception or design of the work or to the acquisition, analysis, or interpretation of data. Conceptualization, A.B. and K.S.-G.; methodology, A.B. and K.M.; software, A.B.; validation, A.B. and B.T.; formal analysis, A.B.; investigation, A.B., B.T. and K.S.-G.; resources, A.B. and B.T.; data curation, A.B.; writing—original draft preparation, A.B.; writing—review and editing, A.B., M.T., K.S.-G., B.T., L.F. and K.M.; visualization, A.B. and M.T.; supervision, K.S.-G. and B.T.; project administration, B.T.; funding acquisition, A.B. and B.T. All authors have read and agreed to the published version of the manuscript.
Funding
Data collection for this study was funded by the Cambodia SMILE study, including One-2-One Cambodia and Ivoclar Vivadent. Analysis was funded by the UC Berkeley-UCSF Joint Medical Program Research Grant and the Schoeneman Grant.
Institutional Review Board Statement
The protocol was approved by the National Ethics Committee for Health Research (NECHR #0306) under the Ministry of Health in Cambodia. The protocol for the secondary data analysis of de-identified data was reviewed by the University of California, Berkeley, Office for Protection of Human Subjects and considered “not human subjects research”.
Informed Consent Statement
The original Cambodia SMILE study obtained informed consent from all caregivers involved in the study.
Data Availability Statement
The data presented in this study are available upon reasonable request to the corresponding author. The data are not publicly available due to privacy concerns for participants.
Acknowledgments
This study was supported by the UC Berkeley-UCSF Joint Medical Program Research Grant and the Schoeneman Grant in addition to funding which made the Cambodia SMILE study possible, including from One-2-One Cambodia and Ivoclar Vivadent. The authors declare no conflicts of interest. We would like to thank the participants and research team, with particular mention of Sieng Chanthyda, Cham Roeun, Heng Chanlay, Sok Phirak, Loy Sreylan, and Horn RithVitou, in making this research possible. We also thank Ndola Prata for continued advising and statistical guidance.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- United Nations Children’s Fund (UNICEF); World Health Organization; International Bank for Reconstruction and Development/The World Bank. Levels and Trends of Child Malnutrition: Key Findings of the 2021 Edition of the Joint Child Malnutrition Estimates. Available online: https://www.who.int/publications/i/item/9789240073791 (accessed on 16 June 2023).
- World Health Organization. Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 19 June 2023).
- National Institute of Statistics (NIS) [Cambodia]; Ministry of Health (MoH) [Cambodia]; ICF. Cambodia Demographic and Health Survey 2021–2022 Final Report. Available online: https://dhsprogram.com/publications/publication-FR377-DHS-Final-Reports.cfm (accessed on 16 June 2023).
- World Health Organization; United Nations Children’s Fund (UNICEF). Indicators for Assessing Infant and Young Child Feeding Practices. Available online: https://www.who.int/publications/i/item/9789240018389 (accessed on 16 June 2023).
- Victora, C.G.; de Onis, M.; Hallal, P.C.; Blössner, M.; Shrimpton, R. Worldwide timing of growth faltering: Revisiting implications for interventions. Pediatrics 2010, 125, 473–480. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Pries, A.M.; Rehman, A.M.; Filteau, S.; Sharma, N.; Upadhyay, A.; Ferguson, E.L. Unhealthy Snack Food and Beverage Consumption Is Associated with Lower Dietary Adequacy and Length-for-Age z-Scores among 12-23-Month-Olds in Kathmandu Valley, Nepal. J. Nutr. 2019, 149, 1843–1851. [Google Scholar] [CrossRef] [PubMed]
- Zahid, N.; Khadka, N.; Ganguly, M.; Varimezova, T.; Turton, B.; Spero, L.; Sokal-Gutierrez, K. Associations between Child Snack and Beverage Consumption, Severe Dental Caries, and Malnutrition in Nepal. Int. J. Environ. Res. Public Health 2020, 17, 7911. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Giovannucci, E.L. Ultra-processed foods and health: A comprehensive review. Crit. Rev. Food Sci. Nutr. 2022, 63, 10836–10848. [Google Scholar] [CrossRef] [PubMed]
- Petridi, E.; Karatzi, K.; Magriplis, E.; Charidemou, E.; Philippou, E.; Zampelas, A. The impact of ultra-processed foods on obesity and cardiometabolic comorbidities in children and adolescents: A systematic review. Nutr. Rev. 2023, 7, nuad095. [Google Scholar] [CrossRef] [PubMed]
- Veit, M.; van Asten, R.; Olie, A.; Prinz, P. The role of dietary sugars, overweight, and obesity in type 2 diabetes mellitus: A narrative review. Eur. J. Clin. Nutr. 2022, 76, 1497–1501. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.; Brinsden, H.; Neveux, M. World Obesity Atlas 2022. Available online: https://www.worldobesityday.org/assets/downloads/World_Obesity_Atlas_2022_WEB.pdf (accessed on 9 July 2023).
- Popkin, B.M. The nutrition transition and obesity in the developing world. J. Nutr. 2001, 131, 871–873. [Google Scholar] [CrossRef]
- Pries, A.M.; Huffman, S.L.; Champeny, M.; Adhikary, I.; Benjamin, M.; Coly, A.N.; Diop, E.H.I.; Mengkheang, K.; Sy, N.Y.; Dhungel, S.; et al. Consumption of commercially produced snack foods and sugar-sweetened beverages during the complementary feeding period in four African and Asian urban contexts. Matern. Child Nutr. 2017, 13 (Suppl. S2), e12412. [Google Scholar] [CrossRef]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Windus, J.L.; Burrows, T.L.; Duncanson, K.; Collins, C.E.; Rollo, M.E. Scoping review of nutrition intervention and dietary assessment studies in Khmer populations living in Cambodia. J. Hum. Nutr. Diet. 2021, 34, 953–968. [Google Scholar] [CrossRef] [PubMed]
- Turton, B.; Durward, C.; Crombie, F.; Sokal-Gutierrez, K.; Soeurn, S.; Manton, D.J. Evaluation of a community-based early childhood caries (ECC) intervention in Cambodia. Community Dent. Oral Epidemiol. 2021, 49, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Turton, B.; Durward, C.; Manton, D.; Bach, K.; Yos, C. Socio-behavioural risk factors for early childhood caries (ECC) in Cambodian preschool children: A pilot study. Eur. Arch. Paediatr. Dent. 2016, 17, 97–105. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Available online: https://www.who.int/publications/i/item/924154693X (accessed on 24 July 2023).
- The World Bank. GDP per Capita (Constant 2015 US$)-Cambodia. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.KD?locations=KH (accessed on 10 November 2023).
- Athavale, P.; Khadka, N.; Roy, S.; Mukherjee, P.; Chandra Mohan, D.; Turton, B.B.; Sokal-Gutierrez, K. Early Childhood Junk Food Consumption, Severe Dental Caries, and Undernutrition: A Mixed-Methods Study from Mumbai, India. Int. J. Environ. Res. Public Health 2020, 17, 8629. [Google Scholar] [CrossRef] [PubMed]
- Huffman, S.L.; Piwoz, E.G.; Vosti, S.A.; Dewey, K.G. Babies, soft drinks and snacks: A concern in low- and middle-income countries? Matern. Child Nutr. 2014, 10, 562–574. [Google Scholar] [CrossRef]
- Pries, A.M.; Huffman, S.L.; Mengkheang, K.; Kroeun, H.; Champeny, M.; Roberts, M.; Zehner, E. High use of commercial food products among infants and young children and promotions for these products in Cambodia. Matern. Child Nutr. 2016, 12, 52–63. [Google Scholar] [CrossRef]
- Pries, A.M.; Filteau, S.; Ferguson, E.L. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: A systematic review. Matern. Child Nutr. 2019, 15 (Suppl. S4), e12729. [Google Scholar] [CrossRef]
- Hinnouho, G.M.; Ferguson, E.L.; MacDougall, A.; Kroeun, H.; Sophonneary, P.; Chea, M.; Pries, A.M. High consumption of unhealthy commercial foods and beverages tracks across the complementary feeding period in rural/peri-urban Cambodia. Matern. Child Nutr. 2023, 19, e13485. [Google Scholar] [CrossRef]
- Pan American Health Organization. Guiding Principles for Complementary Feeding of the Breastfed Child. Available online: https://www.who.int/publications/i/item/9275124604 (accessed on 16 June 2023).
- Contreras, M.; Zelaya Blandón, E.; Persson, L.Å.; Ekström, E.C. Consumption of highly processed snacks, sugar-sweetened beverages and child feeding practices in a rural area of Nicaragua. Matern. Child Nutr. 2016, 12, 164–176. [Google Scholar] [CrossRef]
- Mennella, J.A. Ontogeny of taste preferences: Basic biology and implications for health. Am. J. Clin. Nutr. 2014, 99, 704S–711S. [Google Scholar] [CrossRef]
- Puspikawati, S.I.; Dewi, D.M.S.K.; Astutik, E.; Kusuma, D.; Melaniani, S.; Sebayang, S.K. Density of outdoor food and beverage advertising around gathering place for children and adolescent in East Java, Indonesia. Public Health Nutr. 2021, 24, 1066–1078. [Google Scholar] [CrossRef] [PubMed]
- Mazarello Paes, V.; Hesketh, K.; O’Malley, C.; Moore, H.; Summerbell, C.; Griffin, S.; van Sluijs, E.M.; Ong, K.K.; Lakshman, R. Determinants of sugar-sweetened beverage consumption in young children: A systematic review. Obes. Rev. 2015, 16, 903–913. [Google Scholar] [CrossRef] [PubMed]
- De Cosmi, V.; Scaglioni, S.; Agostoni, C. Early Taste Experiences and Later Food Choices. Nutrients 2017, 9, 107. [Google Scholar] [CrossRef]
- Sharma, N.; Ferguson, E.L.; Upadhyay, A.; Zehner, E.; Filteau, S.; Pries, A.M. Perceptions of commercial snack food and beverages for infant and young child feeding: A mixed-methods study among caregivers in Kathmandu Valley, Nepal. Matern. Child Nutr. 2019, 15 (Suppl. S4), e12711. [Google Scholar] [CrossRef]
- Ruottinen, S.; Niinikoski, H.; Lagström, H.; Rönnemaa, T.; Hakanen, M.; Viikari, J.; Jokinen, E.; Simell, O. High sucrose intake is associated with poor quality of diet and growth between 13 months and 9 years of age: The special Turku Coronary Risk Factor Intervention Project. Pediatrics 2008, 121, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Marrón-Ponce, J.A.; Sánchez-Pimienta, T.G.; Rodríguez-Ramírez, S.; Batis, C.; Cediel, G. Ultra-processed foods consumption reduces dietary diversity and micronutrient intake in the Mexican population. J. Hum. Nutr. Diet. 2023, 36, 241–251. [Google Scholar] [CrossRef]
- Motbainor, A.; Worku, A.; Kumie, A. Stunting Is Associated with Food Diversity while Wasting with Food Insecurity among Underfive Children in East and West Gojjam Zones of Amhara Region, Ethiopia. PLoS ONE 2015, 10, e0133542. [Google Scholar] [CrossRef]
- Molani Gol, R.; Kheirouri, S.; Alizadeh, M. Association of Dietary Diversity With Growth Outcomes in Infants and Children Aged Under 5 Years: A Systematic Review. J. Nutr. Educ. Behav. 2022, 54, 65–83. [Google Scholar] [CrossRef]
- Darapheak, C.; Takano, T.; Kizuki, M.; Nakamura, K.; Seino, K. Consumption of animal source foods and dietary diversity reduce stunting in children in Cambodia. Int. Arch. Med. 2013, 6, 29. [Google Scholar] [CrossRef]
- Sié, A.; Tapsoba, C.; Dah, C.; Ouermi, L.; Zabre, P.; Bärnighausen, T.; Arzika, A.M.; Lebas, E.; Snyder, B.M.; Moe, C.; et al. Dietary diversity and nutritional status among children in rural Burkina Faso. Int. Health 2018, 10, 157–162. [Google Scholar] [CrossRef]
- Valenzuela, M.J.; Waterhouse, B.; Aggarwal, V.R.; Bloor, K.; Doran, T. Effect of sugar-sweetened beverages on oral health: A systematic review and meta-analysis. Eur. J. Public Health 2021, 31, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Dimaisip-Nabuab, J.; Duijster, D.; Benzian, H.; Heinrich-Weltzien, R.; Homsavath, A.; Monse, B.; Sithan, H.; Stauf, N.; Susilawati, S.; Kromeyer-Hauschild, K. Nutritional status, dental caries and tooth eruption in children: A longitudinal study in Cambodia, Indonesia and Lao PDR. BMC Pediatr. 2018, 18, 300. [Google Scholar] [CrossRef]
- Renggli, E.P.; Turton, B.; Sokal-Gutierrez, K.; Hondru, G.; Chher, T.; Hak, S.; Poirot, E.; Laillou, A. Stunting Malnutrition Associated with Severe Tooth Decay in Cambodian Toddlers. Nutrients 2021, 13, 290. [Google Scholar] [CrossRef]
- Turton, B.; Chher, T.; Hak, S.; Sokal-Gutierrez, K.; Lopez Peralta, D.; Laillou, A.; Singh, A. Associations between dental caries and ponderal growth in children: A Cambodian study. J. Glob. Health 2022, 12, 04046. [Google Scholar] [CrossRef]
- Turton, B.; Sullivan, S.; Chher, T.; Hak, S.; Sokal-Gutierrez, K.; Wieringa, F.; Singh, A. Caries Incidence Is Associated with Wasting among Cambodian Children. J. Dent. Res. 2023, 102, 157–163. [Google Scholar] [CrossRef]
- Alkarimi, H.A.; Watt, R.G.; Pikhart, H.; Sheiham, A.; Tsakos, G. Dental caries and growth in school-age children. Pediatrics 2014, 133, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Lui, D.T.; Wahab, R.M.A.; Kuppusamy, E.; Hamzaid, N.H.; Hassan, M.R.; Yazid, F. Association of early childhood caries and nutritional status: A scoping review. J. Clin. Pediatr. Dent. 2023, 47, 11–25. [Google Scholar] [CrossRef]
- Da Silveira, A.C.; Leite, Á.J.M.; Cabral, P.C.; de Oliveira, A.C.; de Oliveira, K.A.; de Lira, P.I.C. Toxic stress, health and nutrition among Brazilian children in shelters. BMC Pediatr. 2021, 21, 112. [Google Scholar] [CrossRef] [PubMed]
- Rachmi, C.N.; Agho, K.E.; Li, M.; Baur, L.A. Stunting coexisting with overweight in 2·0–4·9-year-old Indonesian children: Prevalence, trends and associated risk factors from repeated cross-sectional surveys. Public Health Nutr. 2016, 19, 2698–2707. [Google Scholar] [CrossRef]
- Greffeuille, V.; Sophonneary, P.; Laillou, A.; Gauthier, L.; Hong, R.; Hong, R.; Poirot, E.; Dijkhuizen, M.; Wieringa, F.; Berger, J. Persistent Inequalities in Child Undernutrition in Cambodia from 2000 until Today. Nutrients 2016, 8, 297. [Google Scholar] [CrossRef]
- World Health Organization. The Double Burden of Malnutrition: Policy Brief. Available online: https://www.who.int/publications/i/item/WHO-NMH-NHD-17.3 (accessed on 24 July 2023).
- Horiuchi, Y.; Kusama, K.; Kanha, S.; Yoshiike, N.; FIDR research team. Urban-Rural Differences in Nutritional Status and Dietary Intakes of School-Aged Children in Cambodia. Nutrients 2018, 11, 14. [Google Scholar] [CrossRef]
- Biswas, T.; Townsend, N.; Magalhaes, R.J.S.; Hasan, M.; Mamun, A. Patterns and determinants of the double burden of malnutrition at the household level in South and Southeast Asia. Eur. J. Clin. Nutr. 2021, 75, 385–391. [Google Scholar] [CrossRef]
- Jimenez-Cruz, A.; Bacardi-Gascon, M.; Pichardo-Osuna, A.; Mandujano-Trujillo, Z.; Castillo-Ruiz, O. Infant and toddlers’ feeding practices and obesity amongst low-income families in Mexico. Asia Pac. J. Clin. Nutr. 2010, 19, 316–323. [Google Scholar] [PubMed]
- Saravia, L.; González-Zapata, L.I.; Rendo-Urteaga, T.; Ramos, J.; Collese, T.S.; Bove, I.; Delgado, C.; Tello, F.; Iglesia, I.; Gonçalves Sousa, E.D.; et al. Development of a Food Frequency Questionnaire for Assessing Dietary Intake in Children and Adolescents in South America. Obesity 2018, 26 (Suppl. S1), S31–S40. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Moreno-Franco, B.; Ordovás, J.M.; León, M.; Casasnovas, J.A.; Peñalvo, J.L. Design and development of an instrument to measure overall lifestyle habits for epidemiological research: The Mediterranean Lifestyle (MEDLIFE) index. Public Health Nutr. 2015, 18, 959–967. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).