Disparities in Colorectal Cancer Incidence among Asian and Pacific Islander Populations in Guam, Hawai’i, and the United States
Abstract
1. Introduction
2. Methods
3. Ethics Statement
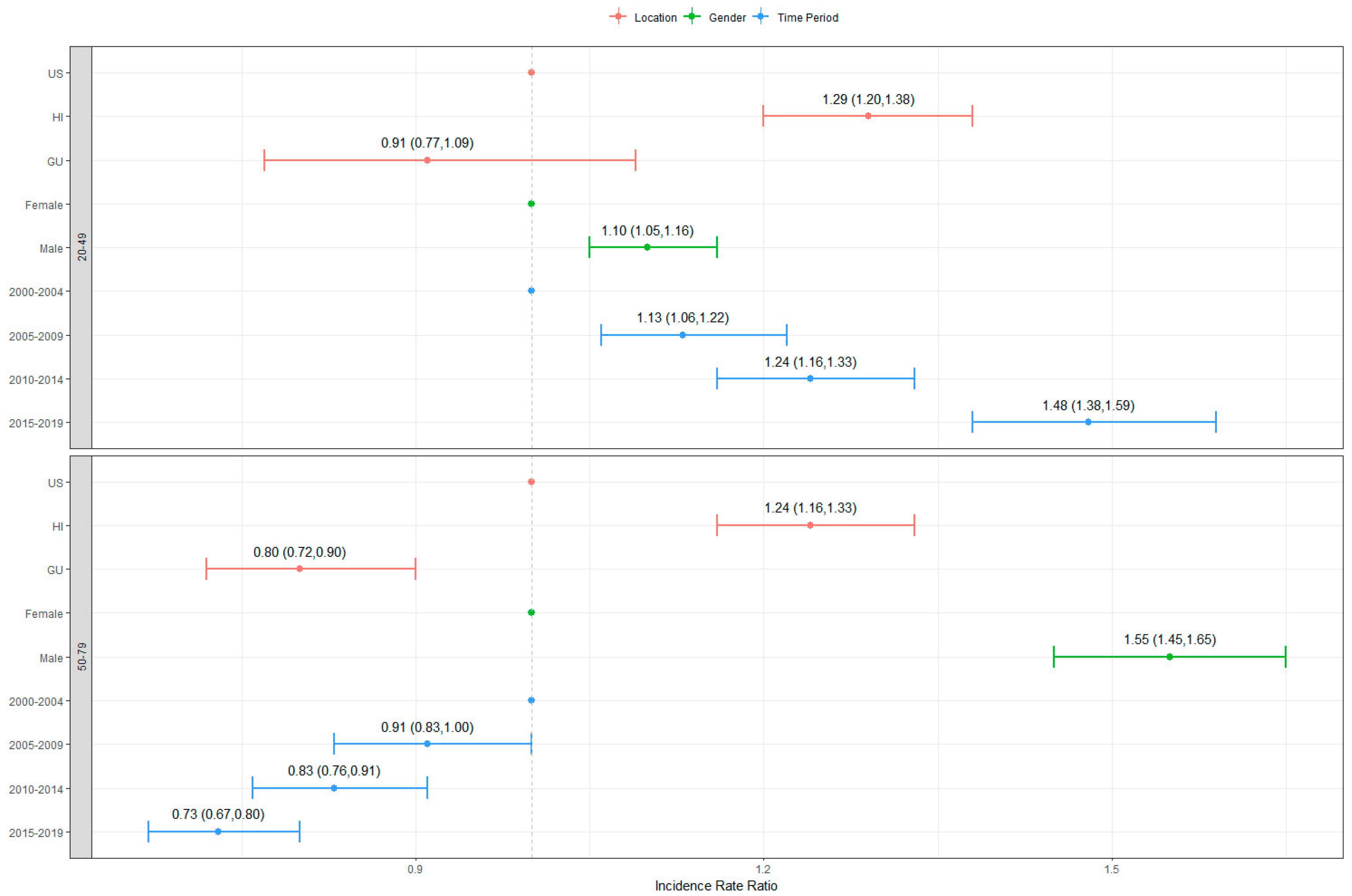
4. Results
5. Discussion
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer.Net. Colorectal Cancer: Statistics. 2023. Available online: https://www.cancer.net/cancer-types/colorectal-cancer/statistics (accessed on 1 May 2023).
- University of Guam Cancer Research Center. Guam Cancer Facts and Figures 2013–2017. Available online: https://www.uog.edu/_resources/files/research/gcr/reports/2013-2017GuamCancerFactsFigures.pdf. (accessed on 1 May 2023).
- University of Hawai’i Cancer Center. Hawai’i Cancer at a Glance 2014–2018. Available online: https://www.uhcancercenter.org/pdf/htr/Cancer%20at%20a%20Glance%202014-2018.pdf (accessed on 1 May 2023).
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Noone, A.M.; Gomez, S.L.; Scoppa, S.; Gibson, J.T.; Lichtensztajn, D.; Fish, K.; Wilkens, L.R.; Goodman, M.T.; Morris, C.; et al. Cancer incidence trends among native Hawaiians and other Pacific Islanders in the United States, 1990–2008. J. Natl. Cancer Inst. 2013, 105, 1086–1095. [Google Scholar] [CrossRef] [PubMed]
- Willingham, M.L., Jr.; Sy, A.; Taafaki, M.; Bodnar, R.; Diaz, T.P.; Somera, L.P.; Porte, C.L.; Ceria-Ulep, C.D.; Pingul, A.; Bissell, J.; et al. Utilizing Filipino key informants to guide community outreach for cancer prevention in Hawai’i. Public Health Nurs. 2023, 40, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, F.; Gaw, A. Mental health care of Filipino Americans. Psychiatr. Serv. 2007, 58, 810–815. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, A.E.; Bastani, R.; Vida, P.; Warda, U.S. Results of a randomized trial to increase breast and cervical cancer screening among Filipino American women. Prev. Med. 2003, 37, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Bock, S.; Henley, S.J.; O’Neil, M.E.; Singh, S.D.; Thompson, T.D.; Wu, M. Cancer Distribution Among Asian, Native Hawaiian, and Pacific Islander Subgroups—United States, 2015–2019. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Sauer, A.M.; Chen, M.S., Jr.; Kagawa-Singer, M.; Jemal, A.; Siegel, R.L. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA Cancer J. Clin. 2016, 66, 182–202. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zhang, J.; Deapen, D.; Stern, M.C.; Sipin, A.; Pandol, S.J.; Setiawan, V.W. Differences in Pancreatic Cancer Incidence Rates and Temporal Trends Across Asian Subpopulations in California (1988–2015). Pancreas 2019, 48, 931–933. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.G.; Karlitz, J.J.; Yen, T.; Lieu, C.H.; Boland, C.R. The rising tide of early-onset colorectal cancer: A comprehensive review of epidemiology, clinical features, biology, risk factors, prevention, and early detection. Lancet Gastroenterol. Hepatol. 2022, 7, 262–274. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services of Minority Health. Asian American Health. Available online: https://www.minorityhealth.hhs.gov/asian-american-health (accessed on 27 August 2023).
- Haddock, R.L.; Whippy, H.J.; Talon, R.J.; Montano, M.V. Ethnic disparities in cancer incidence among residents of Guam. Asian Pac. J. Cancer Prev. 2009, 10, 57–62. [Google Scholar] [PubMed]
- Central Intelligence Agency. The World Factbook—Guam. Available online: https://www.cia.gov/the-world-factbook/countries/guam/ (accessed on 29 April 2023).
- Hernandez, B.Y.; Bordallo, R.A.; Green, M.D.; Haddock, R.L. Cancer in Guam and Hawaii: A comparison of two U.S. Island populations. Cancer Epidemiol. 2017, 50, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.K.; Tsark, J.A.; Mokuau, N.K. Diet-related cancer in Native Hawaiians. Cancer 1996, 78, 1558–1563. [Google Scholar] [CrossRef]
- United States Census Bureau. QuickFacts: Hawaii Country, Hawaii. 2022. Available online: https://www.census.gov/quickfacts/hawaiicountyhawaii (accessed on 2 May 2023).
- Leon Guerrero, R.T.; Badowski, G.; Yamanaka, A.; Blas-Laguana, M.; Bordallo, R.; Buyum, A.; Wilkens, L.; Novotny, R. University of Hawai’i Cancer Center connection: The vital role of cancer registries in the recruitment of an understudied minority population into a breast cancer study: Breast Cancer Risk Model for the Pacific. Hawaii. J. Med. Public Health 2014, 73, 335–340. [Google Scholar] [PubMed]
- Ferlitsch, M.; Reinhart, K.; Pramhas, S.; Wiener, C.; Gal, O.; Bannert, C.; Hassler, M.; Kozbial, K.; Dunkler, D.; Trauner, M.; et al. Sex-specific prevalence of adenomas, advanced adenomas, and colorectal cancer in individuals undergoing screening colonoscopy. JAMA 2011, 306, 1352–1358. [Google Scholar] [CrossRef] [PubMed]
- Gopalani, S.V.; Soman, A.; Shapiro, J.A.; Miller, J.W.; Ortiz-Ortiz, K.J.; Castañeda-Avila, M.A.; Buenconsejo-Lum, L.E.; Fredericks, L.E.; Tortolero-Luna, G.; Saraiya, M. Breast, cervical, and colorectal cancer screening test use in the US territories of Guam, Puerto Rico, and the US Virgin Islands. Cancer Epidemiol. 2023, 84, 102371. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data. 2015. Available online: https://www.cdc.gov/brfss/brfssprevalence/ (accessed on 27 August 2023).
- Braun, K.L.; Fong, M.; Kaanoi, M.E.; Kamaka, M.L.; Gotay, C.C. Testing a culturally appropriate, theory-based intervention to improve colorectal cancer screening among Native Hawaiians. Prev. Med. 2005, 40, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Domingo, J.B.; Chen, J.J.; Braun, K.L. Colorectal Cancer Screening Compliance among Asian and Pacific Islander Americans. J. Immigr. Minor. Health 2018, 20, 584–593. [Google Scholar] [CrossRef] [PubMed]

| Time Period | Location | 20–49 Years (Early Onset) | 50–79 Years (Senior) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Total | Males | Females | Total | ||||||||
| CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | ||
| 2000–2004 | United States | 0.30 | (0.29, 0.31) | 0.26 | (0.25, 0.27) | 0.28 | (0.27, 0.29) | 5.90 | (5.81, 5.99) | 4.16 | (4.09, 4.22) | 4.95 | (4.90, 5.00) |
| Hawaii | 0.43 | (0.37, 0.49) | 0.33 | (0.28, 0.39) | 0.38 | (0.34, 0.42) | 6.80 | (6.42, 7.18) | 4.08 | (3.81, 4.34) | 5.32 | (5.10, 5.55) | |
| Guam | 0.24 | (0.11, 0.38) | 0.30 | (0.15, 0.46) | 0.27 | (0.17, 0.37) | 4.83 | (3.73, 5.93) | 2.51 | (1.75, 3.26) | 3.57 | (2.93, 4.21) | |
| 2005–2009 | United States | 0.33 | (0.32, 0.34) | 0.29 | (0.27, 0.30) | 0.31 | (0.30, 0.32) | 4.93 | (4.85, 5.00) | 3.62 | (3.56, 3.68) | 4.22 | (4.18, 4.217 |
| Hawaii | 0.55 | (0.47, 0.62) | 0.30 | (0.25, 0.36) | 0.43 | (0.38, 0.47) | 6.24 | (5.89, 6.60) | 3.90 | (3.64, 4.15) | 4.98 | (4.77, 5.19) | |
| Guam | 0.21 | (0.09, 0.33) | 0.28 | (0.14, 0.42) | 0.24 | (0.15, 0.34) | 3.51 | (2.68, 4.34) | 1.92 | (1.34, 2.49) | 2.69 | (2.19, 3.19) | |
| 2010–2014 | United States | 0.36 | (0.35, 0.37) | 0.32 | (0.31, 0.33) | 0.34 | (0.33, 0.35) | 4.01 | (3.95, 4.07) | 2.94 | (2.89, 2.99) | 3.44 | (3.40, 3.48) |
| Hawaii | 0.47 | (0.40, 0.54) | 0.44 | (0.37, 0.51) | 0.45 | (0.41, 0.50) | 6.15 | (5.79, 6.51) | 3.62 | (3.38, 3.86) | 4.77 | (4.56, 4.97) | |
| Guam | 0.21 | (0.10, 0.33) | 0.37 | (0.21, 0.53) | 0.29 | (0.19, 0.39) | 3.87 | (3.01, 4.73) | 1.98 | (1.40, 2.55) | 2.90 | (2.39, 3.41) | |
| 2015–2019 | United States | 0.42 | (0.40, 0.43) | 0.37 | (0.36, 0.38) | 0.39 | (0.38, 0.40) | 3.52 | (3.47, 3.57) | 2.55 | (2.51, 2.59) | 3.01 | (2.97, 3.04) |
| Hawaii | 0.47 | (0.41, 0.53) | 0.45 | (0.39, 0.51) | 0.46 | (0.41, 0.50) | 5.04 | (4.74, 5.34) | 2.68 | (2.51, 2.86) | 3.35 | (3.21, 3.49) | |
| Guam | 0.40 | (0.23, 0.57) | 0.44 | (0.25, 0.62) | 0.42 | (0.29, 0.54) | 3.75 | (2.86, 4.64) | 2.54 | (1.86, 3.22) | 3.11 | (2.56, 3.66) | |
| Time Period | Population | 20–49 Years (Early Onset) | 50–79 Years (Senior) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Total | Males | Females | Total | ||||||||
| CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | CIR | 95% CI | ||
| 2000–2004 | US Whites | 0.29 | (0.27, 0.30) | 0.24 | (0.23, 0.25) | 0.26 | (0.25, 0.27) | 5.88 | (5.78, 5.97) | 4.16 | (4.09, 4.24) | 4.95 | (4.89, 5.01) |
| US Filipino | 0.30 | (0.25, 0.34) | 0.24 | (0.21, 0.28) | 0.27 | (0.24, 0.30) | 4.76 | (4.44, 5.09) | 2.67 | (2.47, 2.88) | 3.53 | (3.35, 3.72) | |
| US Hawaiian | 0.40 | (0.28, 0.53) | 0.19 | (0.10, 0.27) | 0.29 | (0.22, 0.37) | 7.47 | (6.38, 8.57) | 3.91 | (3.26, 4.56) | 5.38 | (4.79, 5.97) | |
| HI Filipino | 0.43 | (0.28, 0.59) | 0.35 | (0.22, 0.49) | 0.39 | (0.29, 0.49) | 5.85 | (5.01, 6.70) | 3.00 | (2.43, 3.57) | 4.29 | (3.80, 4.79) | |
| HI Hawaiian | 0.46 | (0.31, 0.61) | 0.21 | (0.11, 0.31) | 0.34 | (0.25, 0.43) | 7.78 | (6.61, 8.95) | 3.47 | (2.82, 4.11) | 5.07 | (4.46, 5.68) | |
| GU Filipino | 0.20 | (0.00, 0.42) | 0.27 | (0.00, 0.54) | 0.23 | (0.06, 0.40) | 3.38 | (2.00, 4.76) | 2.24 | (1.09, 3.40) | 2.85 | (1.94, 3.76) | |
| GU CHamoru | 0.36 | (0.07, 0.65) | 0.33 | (0.06, 0.59) | 0.34 | (0.15, 0.53) | 5.37 | (3.40, 7.33) | 2.96 | (1.65, 4.27) | 3.94 | (2.85, 5.02) | |
| 2005–2009 | US Whites | 0.32 | (0.31, 0.33) | 0.28 | (0.26, 0.29) | 0.30 | (0.29, 0.31) | 4.86 | (4.78, 4.95) | 3.56 | (3.49, 3.62) | 4.17 | (4.12, 4.22) |
| US Filipino | 0.34 | (0.29, 0.39) | 0.25 | (0.21, 0.29) | 0.29 | (0.26, 0.32) | 4.52 | (4.22, 4.81) | 2.67 | (2.49, 2.85) | 3.41 | (3.25, 3.58) | |
| US Hawaiian | 0.47 | (0.34, 0.60) | 0.38 | (0.26, 0.49) | 0.42 | (0.34, 0.51) | 6.14 | (5.29, 6.99) | 3.46 | (2.93, 3.98) | 4.59 | (4.13, 5.06) | |
| HI Filipino | 0.58 | (0.42, 0.75) | 0.21 | (0.11, 0.31) | 0.39 | (0.29, 0.48) | 5.65 | (4.84, 6.46) | 3.00 | (2.50, 3.50) | 4.15 | (3.70, 4.60) | |
| HI Hawaiian | 0.50 | (0.35, 0.64) | 0.40 | (0.27, 0.53) | 0.45 | (0.35, 0.55) | 6.18 | (5.25, 7.11) | 3.16 | (2.62, 3.70) | 4.41 | (3.92, 4.9) | |
| GU Filipino | 0.00 | (0.00, 0.00) | 0.19 | (−0.03, 0.41) | 0.09 | (−0.01, 0.19) | 2.85 | (1.73, 3.98) | 1.11 | (0.38, 1.83) | 1.95 | (1.29, 2.61) | |
| GU CHamoru | 0.26 | (0.03, 0.49) | 0.57 | (0.23, 0.90) | 0.41 | (0.21, 0.62) | 4.96 | (3.22, 6.70) | 2.27 | (1.26, 3.28) | 3.47 | (2.52, 4.41) | |
| 2010–2014 | US Whites | 0.35 | (0.34, 0.37) | 0.32 | (0.30, 0.33) | 0.33 | (0.32, 0.34) | 3.84 | (3.78, 3.91) | 2.87 | (2.82, 2.93) | 3.33 | (3.29, 3.38) |
| US Filipino | 0.29 | (0.24, 0.33) | 0.25 | (0.22, 0.29) | 0.27 | (0.24, 0.30) | 4.02 | (3.76, 4.28) | 2.37 | (2.21, 2.53) | 3.03 | (2.89, 3.17) | |
| US Hawaiian | 0.43 | (0.32, 0.55) | 0.37 | (0.26, 0.48) | 0.40 | (0.32, 0.48) | 6.40 | (5.57, 7.22) | 2.88 | (2.46, 3.31) | 4.27 | (3.86, 4.69) | |
| HI Filipino | 0.51 | (0.36, 0.66) | 0.46 | (0.32, 0.60) | 0.48 | (0.38, 0.58) | 5.18 | (4.46, 5.90) | 3.48 | (2.98, 3.97) | 4.20 | (3.78, 4.62) | |
| HI Hawaiian | 0.42 | (0.29, 0.55) | 0.27 | (0.17, 0.37) | 0.35 | (0.26, 0.43) | 5.70 | (4.85, 6.55) | 2.39 | (1.98, 2.81) | 3.66 | (3.25, 4.06) | |
| GU Filipino | 0.10 | (−0.04, 0.24) | 0.13 | (−0.05, 0.32) | 0.12 | (0.00, 0.23) | 3.49 | (2.22, 4.76) | 1.27 | (0.50, 2.05) | 2.34 | (1.61, 3.07) | |
| GU CHamoru | 0.33 | (0.09, 0.58) | 0.58 | (0.24, 0.93) | 0.45 | (0.24, 0.66) | 4.77 | (3.16, 6.37) | 2.86 | (1.81, 3.92) | 3.73 | (2.81, 4.66) | |
| 2015–2019 | US Whites | 0.42 | (0.41, 0.44) | 0.37 | (0.36, 0.39) | 0.40 | (0.39, 0.41) | 3.38 | (3.33, 3.44) | 2.48 | (2.43, 2.53) | 2.91 | (2.88, 2.95) |
| US Filipino | 0.33 | (0.28, 0.37) | 0.26 | (0.22, 0.29) | 0.29 | (0.26, 0.32) | 4.24 | (3.97, 4.51) | 2.37 | (2.21, 2.53) | 3.11 | (2.96, 3.25) | |
| US Hawaiian | 0.57 | (0.45, 0.70) | 0.55 | (0.42, 0.68) | 0.56 | (0.47, 0.65) | 4.69 | (4.10, 5.28) | 3.06 | (2.65, 3.48) | 3.75 | (3.41, 4.10) | |
| HI Filipino | 0.36 | (0.23, 0.49) | 0.36 | (0.24, 0.48) | 0.36 | (0.27, 0.44) | 4.64 | (4.04, 5.25) | 2.52 | (2.14, 2.91) | 3.44 | (3.10, 3.78) | |
| HI Hawaiian | 0.54 | (0.40, 0.69) | 0.43 | (0.29, 0.56) | 0.49 | (0.39, 0.59) | 3.96 | (3.40, 4.52) | 3.14 | (2.62, 3.67) | 3.52 | (3.14, 3.90) | |
| GU Filipino | 0.35 | (0.07, 0.63) | 0.31 | (0.04, 0.59) | 0.33 | (0.13, 0.53) | 2.50 | (1.39, 3.60) | 1.53 | (0.71, 2.34) | 1.99 | (1.32, 2.67) | |
| GU CHamoru | 0.42 | (0.11, 0.73) | 0.54 | (0.19, 0.89) | 0.48 | (0.24, 0.71) | 4.69 | (3.26, 6.13) | 3.75 | (2.37, 5.14) | 4.49 | (3.39, 5.59) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.; Badowski, G.; Shvetsov, Y.B.; Dulana, L.; Teria, R.; Jin, S.B.; Aguon, C.; Bordallo, R.; Leon Guerrero, R.T. Disparities in Colorectal Cancer Incidence among Asian and Pacific Islander Populations in Guam, Hawai’i, and the United States. Int. J. Environ. Res. Public Health 2024, 21, 170. https://doi.org/10.3390/ijerph21020170
Choi J, Badowski G, Shvetsov YB, Dulana L, Teria R, Jin SB, Aguon C, Bordallo R, Leon Guerrero RT. Disparities in Colorectal Cancer Incidence among Asian and Pacific Islander Populations in Guam, Hawai’i, and the United States. International Journal of Environmental Research and Public Health. 2024; 21(2):170. https://doi.org/10.3390/ijerph21020170
Chicago/Turabian StyleChoi, JaeYong, Grazyna Badowski, Yurii B. Shvetsov, Louis Dulana, Rodney Teria, Su Bin Jin, Cabrini Aguon, Renata Bordallo, and Rachael T. Leon Guerrero. 2024. "Disparities in Colorectal Cancer Incidence among Asian and Pacific Islander Populations in Guam, Hawai’i, and the United States" International Journal of Environmental Research and Public Health 21, no. 2: 170. https://doi.org/10.3390/ijerph21020170
APA StyleChoi, J., Badowski, G., Shvetsov, Y. B., Dulana, L., Teria, R., Jin, S. B., Aguon, C., Bordallo, R., & Leon Guerrero, R. T. (2024). Disparities in Colorectal Cancer Incidence among Asian and Pacific Islander Populations in Guam, Hawai’i, and the United States. International Journal of Environmental Research and Public Health, 21(2), 170. https://doi.org/10.3390/ijerph21020170






