Abstract
Background: Our study aimed to examine whether health anxiety, social support, and ways of coping relate to dissociation directly or only through the mediation of perceived stress, moderated by the time of measurement (lockdown). We investigated the effect of perceived stress on different forms (sub-scales) of dissociation. Methods: A cross-sectional survey was conducted by an online form at two points in time: the beginning and the later stage of the COVID-19 pandemic. Results: We received a total of 1711 responses. Perceived stress moderately correlated with dissociation in both international and Hungarian samples. Health anxiety showed a strong direct and indirect correlation with dissociation. Regarding social support, the support of family significantly decreased the dissociative experiences in the Hungarian sample mediated by perceived and direct stress. In the international sample, goal-oriented coping strategies strongly decreased all dissociation scales in the first measurement, through the mediation of perceived stress. As for the Hungarian sample, positive thinking was found to decrease dissociation by decreasing perceived stress. Conclusion: health anxiety, coping, and social support appeared to influence dissociation directly and through the mediation of perceived stress. Social support, mainly support of the family and problem-focused coping strategies may decrease the level of stress, this way decreasing dissociative behavior.
1. Introduction
On 11 March 2020, the WHO classified COVID-19 a pandemic [1]. To avoid rapid spread, governments and international organizations introduced various measures, including nationwide lockdowns in several countries, and Hungary was no exception [2].
The lockdown was ordered on 28 March 2020 and eventually—after a few extensions—it was lifted in the countryside on 4 May 2020 and in Budapest on 18 May 2020. Among the first cases, there was a large number of Hungarians and foreigners who came home from abroad, e.g., Iranian students. The Hungarian foreign minister said “a new wave of migrants heading towards Europe, presenting health and security risks, is possible due to the pandemic” [2]. Turbid statements such as this one could have caused the birth of, often subconscious, xenophobic tendencies, even in individuals who previously had no such inclinations.
After the initial phase and as vaccines were introduced and spread across the globe, the number of patients treated in hospitals and on ventilators also decreased [2]. At first, the vaccination program was made available only for essential workers and high-risk individuals, but after that, anyone who wanted to receive the vaccine had the opportunity due to Hungary’s sufficient supply of vaccines by then. The head of the prime minister’s office ranked Hungary as one of the safest countries and said “The Hungarian government is ready to mitigate the damage students suffered during the coronavirus epidemic due to the lack of classroom education” [2].
Since then, mental effects of the pandemic have become widely known, as a plethora of studies has been conducted and written about it. These effects include, to name just a few, increased psychological distress, anxiety, depression, and disturbed sleep [3,4,5,6].
Confinement and isolation were already known to have mental and health implications before COVID-19, such as worse cardiovascular and mental health outcomes [7]. Lockdowns and quarantines during the pandemic created more opportunities to examine mental health of people living under these conditions, and thus the number of studies also increased expeditiously. In the course of the pandemic, confinement and isolation were found to influence important aspects of everyday life, such as food supply, teaching, and travel; they have a significant effect on the appearance of depression and anxiety, and their effect on mental health can be extensive and long-lasting [8,9,10].
That is why we found it important to examine psychological and social constructs, such as social support, perceived stress, health anxiety, coping mechanisms, and dissociation, during COVID-19 and even more so during the lockdowns. The relationship between perceived stress and dissociation is well-documented in the scientific literature. The COVID-19 pandemic increased perceived stress. We aimed to study variables that are closely related to perceived stress, such as coping, health anxiety, and social support. Al-though studies have been conducted for these separately, and even some have been combined, there has not yet been a study that examined all of them together to the best of our knowledge. We are now trying to fill this gap with this study. Our main focus (dependent variable) was dissociation, because in traumatic situations dissociation is a significant phenomenon, and it may lead to severe consequences such as PTSD [11] and addictive behavior [12]. According to recent studies, the importance of dissociation in mental health is under-recognized [13].
We aimed to examine the following: how perceived stress is related to dissociation, and how health anxiety, social support, and ways of coping relate to dissociation directly and through the mediation of perceived stress, moderated by the time of measurement (lockdown). Researchers found that higher levels of the psychological constructs we examined (perceived stress, anxiety, exhaustion, and depression) can be detected at a higher degree in those participating in higher education [3,14,15,16,17].
Regarding dissociation, we followed in the footsteps of Janet, who was the first to study dissociation comprehensively and in detail and “claimed it as the crucial psychological process with which the organism reacts to overwhelming trauma and which results in the wide variety of symptoms” [18]. He believed that under normal circumstances, the awareness of feelings, emotions, thoughts, and actions connected to a certain event or experience is concentrated in one consciousness and can be controlled voluntarily. However, the memories of frightening or novel events and experiences that do not fit into existing cognitive schemas can detach from consciousness and go beyond the authority of voluntary control, and the details of the unintegrated experiences created in this way can emerge as pathological automatisms [18].
Almost a hundred years later, Janet’s thoughts were carried forward by Bernstein and Putnam, who created the questionnaire we also utilized, the Dissociative Experiences Scale (DES). According to their definition, “dissociation is a lack of the normal integration of thoughts, feelings, and experiences into the stream of consciousness and memory” [19].
Even later, Grabe et al., summarized this as “dissociation is considered to serve as a defense mechanism against intolerable, trauma-associated memories and feelings, and results from a disintegration of consciousness, memory, identity, and perception” [20].
Initially, Janet thought of all forms of dissociation as pathological. With all respect to him, over time his theories have been further scrutinized and it has been found that dissociation is a spectrum with adaptive and pathological forms [21,22,23].
Different authors have described that greater stress and traumatic experiences promote dissociation [24,25]. Moreover, in a large study including 6941 individuals from the general population, Černis et al. [13] explored, using network approaches, how dissociative experiences taking the form of a Felt Sense of Anomaly (FSA) relate to common mental health conditions and psychotic experiences and found that dissociation is connected to many mental health disorders and may influence a number of presentations, particularly psychotic experiences.
Certain studies have already addressed dissociation emerging during COVID-19. In a study conducted on the general population, authors found that women have a higher rate of traumatic distress and that the Internet-addicted subgroup experienced dissociative experiences more often [26]. In another study, authors found that hopelessness is associated with more dissociative experiences, which contribute to the strengthening of denial about COVID-19, which is a maladaptive defense against feelings of hopelessness [27]. In the study conducted in Italy with an online questionnaire during the lockdown, it was possible to prove the direct relationship between the pathological personality (subjects with previous psychopathological vulnerability) and the fear of COVID-19, and that although dissociation and emotion dysregulation were not involved in the relationship between the two as intervening mediators. However, they found that dissociation and emotion dysregulation play an important role in the relationship between pathological personality and PTSD [28]. A French study of medical staff found that, among others, levels of peritraumatic dissociation were lower for men compared to women [29].
In these studies, different aspects of dissociation (the questionnaire subscales, namely absorption, depersonalization, and amnesia) were not differentiated, rather a summated score was used—however, different dissociative experiences may be different in their adaptiveness in stressful situations.
Among many psychological consequences of the pandemic, our main focus was dissociation caused by perceived stress. Why did we focus on dissociation? First, COVID-19 significantly increased addictive behavior in society [12], and as addiction may be considered a dissociative behavior, dissociation has to do with addictions [26]. Second, dissociative experiences entail a higher risk of the appearance of dissociative disorders such as PTSD [11]. Stress promotes dissociation, and the relationship between stress and dissociation is well-documented in the related scientific literature [24,25], but perceived stress in the same pandemic situation may differ along various variables. We aimed to study this relationship during the COVID-19 pandemic and expanded the examination by protective factors (e.g., social support, adaptive coping), and risk factors (e.g., health anxiety, maladaptive coping) as these constructs may have a role in the level of perceived stress.
1.1. Perceived Stress
We used this term as Cohen, Kamarck, and Mermelstein defined it: a crucial psychological factor that refers to the degree to which events in a person’s life are perceived as stressful, unpredictable, and uncontrollable [11]. During the COVID-19 pandemic, a wide range of studies was conducted in the area of stress. A meta-analysis of studies examining the effects of the COVID-19 pandemic on mental health found that anxiety has increased in the average population compared to pre-pandemic times [5]. A review emphasizes increased stress and lists which factors may contribute to its development, highlighting uncertainty about the disease and social isolation [4]. Others have found significantly increased levels of distress in the general population [3], especially during the early stages of the pandemic [14]. Examining the impact of the lockdown, it was found among students that the value of perceived stress increased, while the quality of mental well-being and the extent of physical exercise decreased during lockdown [30].
High levels of perceived stress appear to elevate dissociative experiences. In a longitudinal study by De Wachter et al., stress levels of participants were reduced by information and psychological support. Their results support a one-directional causal relationship: a decrease in perceived stress leads to a decrease in dissociative phenomena [31].
1.2. Social Support
In their 1985 work, Cohen and Syme defined social support as the resources provided by other persons, and they stated that it can have both negative and positive effects on health and well-being. In their work, two models are presented: in one, a direct effect is outlined, in which social support enhances health and well-being regardless of the level of stress; the other model is the buffering hypothesis, in which “social support exerts its beneficial effects in the presence of stress by protecting people from the pathogenic effects of such stress by attenuating or preventing a stress response” [32]. Other authors believe that “neither type of support effect is found uniformly”. Support refers to the positive, potentially health-promoting, or stress-buffering aspects of relationships such as instrumental aid, emotional caring or concern, and information. In essence, supportive relationships directly provide something that people need to stay healthy or to adapt to stress [33].
Authors found that social support can not only play a role in avoiding negative symptoms but can also help with adequate adaptation after COVID-19 and can be an excellent tool in the fight against stress and trauma [34]. In recent literature, we can find evidence that perceived social support moderates the relationship between COVID-19-related anxiety and psychological health [35] and that it can provide a buffering effect on mental health against the negative impact caused by low resilience [36]. Lower levels of perceived social support were found to be significantly associated with elevated risk for depression and poorer sleep quality [37]. Resilience, coping behaviors, and social support were identified as protective factors against loneliness [38].
Several studies examined the interaction between social support and dissociation as well, though results are somewhat contradicting; e.g., Baranyi et al. [39] did not support a link between PTSD and unfavorable perception of supportive relationships, while Coronas et al. [40] found that perceived social deprivation was related to the diagnosis of PTSD 2 months after a motor vehicle accident among victims. In a study, even Dissociative Identity Disorder was found to be best predicted by the absence of social and familial support in combination with an abuse history [41].
1.3. Health Anxiety
According to its definition, health anxiety is the way individuals think and behave about their health and the way they experience their concerns and threats to their health. Health anxiety lies on a spectrum, and while it can have a signaling function to initiate appropriate behaviors, it also can reach overwhelming levels with detrimental consequences [42]. However, both extremes can cause harm. AT one extreme, when health anxiety is excessively low, the person ignores their body’s signals and seeks medical help too late or disregards important measures. At the other extreme, when the level of health anxiety is excessively high, the person can overburden the health care system or worry excessively about their health while they remain locked in their rooms, afraid of the contagion [43].
The previously mentioned review also highlights the role of health anxiety on mental health and states that the level of health anxiety may rise during the epidemic [4]. However, it may be interesting that according to a systematic review analyzing longitudinal studies, the level of anxiety only increased in the initial period compared to the times before COVID-19, and later this seemed to settle down [44]. Interestingly, in contrast to this review in which the scientists found that the increase in measures of anxiety and general mental health observed in March–April 2020 decreased from May–July 2020 (the increase in depression remained higher) [44], the review examining college students found that, compared to the early results, the level of anxiety and depression among the students increased [45].
1.4. Coping
The dimensions of coping were determined based on Lazarus’ transactional theory of stress. According to this, the definition of coping is how individuals cope with stress. According to Lazarus and Folkman, stress is a relationship between the environment and the person, which a person perceives as exceeding his abilities and threatening his well-being. Coping is nothing more than a variable cognitive and behavioral effort that the person uses to manage internal and/or external demands that exceed the person’s resources, and it does all this by reducing demands or strengthening personal resources to meet demands. Management can refer to the environment or the person, past or future, and can be instrumental or palliative. Two types of coping are distinguished, between which overlaps can be observed: problem-focused coping (changing the problematic environment-person relationship) and emotion-focused coping (regulating emotional distress) [46].
In one study, the majority of college students used problem-focused coping, e.g., they followed strict measures, read about COVID, and avoided public places, and only a few used emotional-focused coping, e.g., venting emotions or adopting a positive attitude [47]. In another Austrian study, active coping and social support were highlighted, which helped mental well-being [48]. Interestingly, in a study in which nurses and nurse students were examined, it was found that practicing nurses use problem-focused coping more than students, and this may be because there is a psychological typhoon eye effect which means that people are less affected at the epicenter of the events [49]. Also, in their study, male students were more prone to use emotion-focused coping. As an explanation, they suggest that women are less able to cope emotionally, as they are more emotional, so they can be swept away by their emotions [50]. Overall, it seems that problem-focused coping was found to be more effective and people used it more often. The main contradiction and interesting thing is that most people experienced the virus as unpredictable and uncontrollable, at least initially. Along with this, many people used problem-focused coping, despite the fact that researchers previously found that problem-focused coping can be used primarily in encounters appraised as changeable [51]. On the other hand, it seems certain that avoiding or denying things is not expedient, as those who try to cope in this way have experienced increased levels of anxiety and stress [52].
1.5. Gender
Female gender was identified as a risk factor for higher stress levels in several meta-analyses during the pandemic [3,6,15,53] and overall; it was found that the pandemic affected women more deeply mentally than men [54]. According to a Malaysian study, the female gender and being alone as factors were significantly associated with elevated anxiety values among students. Examining individual stressors, they found that financial issues, online education, and an uncertain future or academic career were at the top [55]. The feelings of the female students regarding the quarantine were more negative compared to their male counterparts, and Italian researchers also found differences similar to other nations when examining the students (increased nervousness, irritability, rumination) and concluded that the student population is more vulnerable [56].
In a narrative review, different sensitivity groups were also identified among women, and they found that the pandemic can amplify the inequalities between the sexes and that social support can be a key protective factor in women’s cases [57].
1.6. Lockdown
The lockdown posed a great challenge for the entire population; from the food supply and the loss of financial income, through the reduction of body exercise and travel, to gender relations and domestic violence, everything was affected and had its own mental health implications [8].
The effects of lockdown on mental health are now well known, e.g., it can significantly elevate the amount of perceived stress [10]. This is especially true for students. It can be challenging for international students to get housing, they cannot travel home in these difficult times, which can put a special financial burden on them, and those who manage to get home may be uncertain as to whether they will be able to continue their studies [58]. With the closure of universities, students have adopted new habits, often not by choice. Among them was that classes were attended online. These made personal meetings impossible, and therefore it made them less motivated to study harder, to learn and apply interpersonal and social skills, which also became unattainable in such an environment [59]. The lockdown and the COVID-19 epidemic itself significantly increased the level of student suicides compared to previous years, which draws our attention to serious problems [6,60]. Other studies examining the general population note that school closings, the transition to online education, and isolation from others can all have effects on mental health [8].
A meta-analysis regarding the lockdown found minimal but significant effect sizes for anxiety and depression concerning the lockdown, but at the same time, no significant results were obtained regarding social support, and gender was not found to be a significant moderating factor. According to their conclusion, the lockdown causes heterogeneous differences, which are not outstanding in their magnitude, and the majority of people are psychologically resilient to the lockdown [9].
1.7. Aims of the Study
The aim of this study is to investigate how coping, social support, health anxiety (independent or predictor variables) affect dissociation (dependent variable) overall and its subscales. We would like to examine if these variables have direct effects on dissociation as well, or if their effect can only be explained by mediation through the effect of perceived stress (as a mediator variable).
2. Materials and Methods
2.1. Study Design and Setting
When reporting survey design and sample selection, we consider the CHERRIES statement [61]. The survey was approved by the Hungarian Ethical Review Committee for Research in Psychology (see Patents). In our study, participants filled out an online questionnaire voluntarily. Google Forms was used to create the online survey. Data results of the questionnaire is protected by a password that is only known to the leader of the research. No personal data were collected that would allow the identification of subjects. Informed consent was included in the online questionnaire, on the first page, so as the estimated time of completion.
We conducted a cross-sectional survey at two points in time: the first round (Study 1) was conducted at the time of the nationwide lockdown during one of the most stressful periods of the COVID-19 pandemic in Hungary and when the virus was largely unknown; the second round took place after the lockdown (Study 2). Peace prevailed in the country, easing the strict measures, very low positive test ratio, few new cases, and minimal COVID-related deaths. We found that fewer people participated in the later survey, around the time the virus was tamed by knowledge, vaccines, and measurements. During the COVID-19 period, several longitudinal surveys were conducted, and it was a general problem to lose participants from the first round to the further runs [14].
2.2. Study Participants and Sampling
The target population of our study was the students at the second largest university in Hungary, the University of Debrecen from all study programs and study levels (undergraduate, graduate, and postgraduate). We used convenience sampling. The students were approached through social media platforms (Facebook®) as well as the official administration system at the university (Neptun system). Both domestic and international students were recruited to participate in our survey and the questionnaire was available in Hungarian and English languages. Regarding international students, English fluency is an entry requirement at the University of Debrecen and students have been doing their studies in English too. All participants should have been at least 18 years or older and enrolled in a study program at the University of Debrecen to be eligible for participation on a self-reported base. The questionnaires were administered on 20 April 2020 in the first round (Study 1). The second measurement started on 20 July 2021 (Study 2). Google Forms checked IP addresses, preventing double completion. Partly incomplete questionnaires were included, but the sample sizes of the particular statistics are different because only complete answers were analyzed.
Our sample is not representative, so non-response bias should be taken into account when drawing conclusions, though we do not presume major differences between respondents and non-respondents.
2.3. Survey Instruments
Our survey questionnaire has solicited anonymous responses using brief sociodemographic items and international scales, namely, the Perceived Stress Scale (PSS) [62,63,64], the Multidimensional Scale of Perceived Social Support (MSPSS) [65,66], the Short Health Anxiety Inventory (SHAI) [67,68], the Ways of Coping Questionnaire (WCQ) [69,70,71] and the Dissociative Experiences Scale (DES) [19,72,73]. The sociodemographic questions were about age, gender, and faculty/study program. Questions were not randomized, they followed the same order for every participant.
2.3.1. The Perceived Stress Scale (PSS)
To assess the stress encountered by the students, we used the Perceived Stress Scale (PSS) which was designed by Cohen et al. [62] and it asks about the stressful situations people went through in the preceding month. It contains 10 statements that respondents can answer on a 5-point (0–4) Likert scale [63]. Among the Hungarian university students, we used the Hungarian version of the PSS [64], which differs from the English version in that it contains 14 statements [64].
2.3.2. Multidimensional Scale of Perceived Social Support (MSPSS)
To measure the amount of social support the students felt they receive we used the Multidimensional Scale of Perceived Social Support (MSPSS). The 12 items are rated on a 7-point Likert scale in the English version [65] while the 10-item Hungarian version uses a 5-point Likert scale [66]. The higher score can be interpreted as a greater amount of available social support. Three subscales were identified, each addressing a different source of support: Family, Friends, and Significant Others [65,66].
2.3.3. Short Health Anxiety Inventory (SHAI)
The third scale we utilized was the Short Health Anxiety Inventory (SHAI), which has 18 items and two subscales. The first subscale comprises 14 items that examine to what degree the respondents were worried about their health, about a serious illness, and about their bodily sensations in the past six months and what their environment said, how much attention they paid to their health. The second subscale of SHAI comprises 4 items that try to evaluate the negative consequences of the illness if it occurs [67]. There are 4 statements for every item in an increasing frequency order (scored from 0 to 3) and one of the four statements must be chosen [74]. For the Hungarian students, the validated Hungarian version of the SHAI was used [68]. The scoring differs from the original version in that the four statements are scored from 1 to 4, but the statements themselves are the same [68].
2.3.4. Ways of Coping Questionnaire (WCQ)
To see what coping strategies the students employ to relieve stress, we used the 26-Item Ways of Coping Questionnaire (WCQ) which was based on the revised 66-Item version [69] and developed by Sørlie and Sexton [70]. The international students answered the validated English version of the 26-Item WCQ that examines how often the respondents used certain coping mechanisms in recently occurring stressful situations. The responses are scored on a 4-point Likert scale (from 0 = “does not apply and/or not used” to 3 = “used a great deal”). The WCQ distinguishes five different factors: Seeking support, Goal-oriented, Thinking it over, Wishful thinking, and Avoidance [70].
For the Hungarian students, we utilized the validated Hungarian 16-Item WCQ [71]. The authors identified four dimensions: Cognitive restructuring/Adaptation, Problem analysis, Stress reduction, and Helplessness/Passive coping [71].
2.3.5. The Dissociative Experiences Scale (DES)
This scale was developed by Carlson and Putnam to measure dissociative experiences. During the design of DES, the scale was defined as a continuum of dissociative experiences based on the number and frequency [19]. On this continuum, healthy people report rare and few dissociative experiences (i.e., when is rarely and few are the different dissociative experiences the person experiences, they can even be healthy experiences). According to Vanderlinden, the dissociative experiences that are considered to be healthy originate from the adaptive dissociative mechanisms which are absorption and loss of control [75]. As the scale moves towards the other endpoint, more and more individuals can be found who have clinical symptoms and report diverse and varied dissociative experiences [19]. The number and frequency of symptoms make it likely that the clinical condition will appear. The DES is a series of 28 statements of questions that describe dissociative symptoms in general and could initially be marked on a scale (DES-I) [19] how often a person feels the given symptom in a part of their everyday life, and using the updated version the same could be done on a 0% to 100% scale (DES-II) [74]. The average of the summation gives how many points the person has completed on DES. The higher it is the more likely the presence of dissociative symptoms. Some dissociative activity can also be measured among healthy people, which was found to be 4.38 points [19]. This value was found to be the highest in dissociative identity disorder (57.1), while it was found to be the second-highest in post-traumatic stress disorder, PTSD (31.3) [76]. The test has three subscales: amnestic dissociation; absorption and imagination; and depersonalization and derealization [72,73].
2.3.6. Data Analysis
We calculated the mean scores of the items for the aggregated measures of the Perceived Stress Scale, Short Health Anxiety Inventory, and Dissociative Experiences Scale. For the Multidimensional Scale of Perceived Social Support and the English version of the Ways of Coping Questionnaire, means were calculated for each subscale. In the case of the Hungarian version of WCQ, the authors of adaptation suggested investigating the factor structure of used data [71]. Since Cronbach’s alphas were unacceptable (below 0.5) for 3 subscales, we conducted exploratory factor analysis with the ‘Minimum residual’ extraction method and ‘oblimin’ rotation. Bartlett’s Test of Sphericity was significant with χ2 (120) = 332, p < 0.001, KMO Measure of Sampling Adequacy was 0.821 for the four-factor solution (Table 1).

Table 1.
Factor loadings for the Hungarian version of WCQ.
Factor 1 consisted of items connected to positive thinking, Factor 2 contained items connected to distancing coping, Item 2 in Factor 3 is connected to humor, while the last factor had items connected to taking up outer perspectives. Mean scores were computed according to the factors, except for humor coping, for which the single item was kept. Descriptive statistics and reliability measures can be seen in Table 2 and Table 3. Cronbach’s alpha measure of reliability had good or excellent values for most scales, acceptable values for wishful thinking and thinking it over coping in the international sample, positive coping in the Hungarian sample, questionable for outer perspective coping, and poor values for avoidant coping in the Hungarian sample.

Table 2.
Descriptive statistics for variables of international sample.

Table 3.
Descriptive statistics for variables of the Hungarian sample.
RStudio and IBM SPSS 27.0 were used to analyze the data. Mann-Whitney U-test was used to investigate the differences between the two measurements and between males and females. Spearman correlation was used for examining connections between variables.
We used conditional process modeling by Hayes (2018) to test the independent effects of health anxiety, social support and coping on dissociation, and the mediating role of perceived stress [77]. We also tested the moderating effect of measurement time, which was dummy coded and we used model 8. We used health anxiety, social support and coping scales as predictor variables, always one predictor at a time, other variables were set as covariates. Bootstrapping was used with 5000 samples and the same seed across models. We used the PROCESS syntax file provided on www.processmacro.org (accessed on 12 September 2022).
3. Results
We received a total of 1711 responses, but n = 29 respondents were excluded for not staying in Hungary during the lock-down period, and n = 2 respondents were excluded, because they answered only the first questions in the questionnaire. In the final sample, there were n = 483 (n = 347 in the first measurement, n = 136 in the second measurement) valid responses from international and n = 1197 (n = 950 in the first measurement, n = 247 in the second measurement) valid responses from Hungarian students. Of the international students, 58.3% were females, and 41.5% were males, with age M = 22.67 and SD = 4.344. Of the Hungarian students, 75% were females, and 25% are males, with age M = 24.98 and SD = 8.047. As the questionnaire was somewhat different in English and in Hungarian, we divided our sample and analyzed the two groups separately.
3.1. Descriptive and Correlational Analysis
In the international sample, gender differences were found regarding absorption (Uint_abs = 24.140, p < 0.05); females reported higher values (MDint_absf = 32.5; MDint_absm = 25). Amnesia and depersonalization showed statistically higher values in the second measurement (Uint_amn = 19.951, pint_amn < 0.05, MDint_amn1 = 5; MDint_amn2 = 10; Uint_dep = 20.351, pint_dep < 0.05, MDint_dep1 = 3.33; MDint_dep2 = 10). In the Hungarian sample, males had significantly higher values in amnesia (Uhun_amn = 120.173, phun_amn < 0.05, MDhun_amnf = 5; MDhun_amn = 7.5), and values of two measurements differed in depersonalization (Uhun_dep = 108.132, phun_dep < 0.05, MDhun_dep1 = 3.33; MDhun_dep2 = 6.67).
In Table 4 and Table 5, we can see that stress moderately correlated with dissociation in both international (r(483) = 0.436 p < 0.001) and Hungarian sample (r(1197) = 0.450, p < 0.001). Other variables had low to moderate correlation coefficients with dissociation. Goal-oriented coping (international sample), humor (Hungarian sample) and coping by taking up outer perspective did not have significant correlation coefficients with dissociation.

Table 4.
Correlation matrix for the international sample.

Table 5.
Correlation matrix for the Hungarian sample.
3.2. Moderated Mediation Analysis
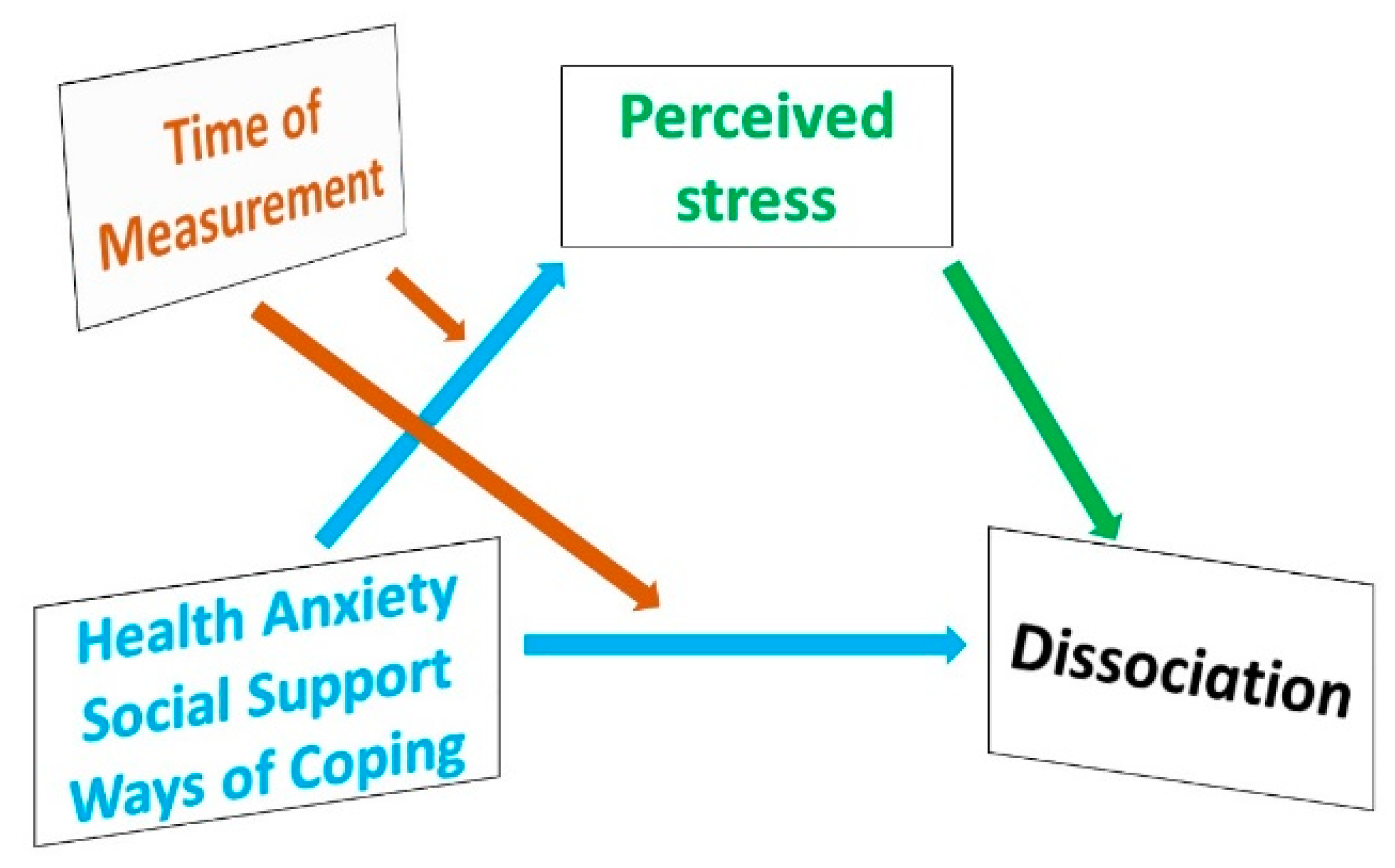
We aimed to examine whether health anxiety, social support and coping (predictor variables) have direct effects on dissociation (dependent variable), or if their effect can rather be explained by mediation through the effect of perceived stress (mediator variable). Time of measurement (in lockdown and after lockdown) may moderate this relationship (moderator variable). Perceived stress as a mediator variable in the model means we wanted to examine the predictor variables’ effect on dissociation through perceived stress. That is to say, we aimed to uncover whether health anxiety, social support and coping affect dissociation by increasing or decreasing perceived stress, or whether they have a direct effect on dissociation in their own right, independent from perceived stress. Our theoretical consideration is demonstrated in Figure 1. Time of measurement as a moderator variable means that time of measurement may moderate the relationship between perceived stress and dissociation and predictor variables and dissociation.
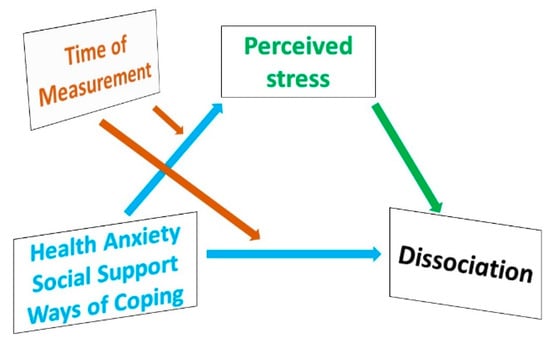
Figure 1.
Theoretical model of factors influencing dissociation.
The parameters and model fit measures for the Hayes process analysis are shown in Table 6 and Table 7.

Table 6.
Coefficients of the linear regression of the Hungarian sample.

Table 7.
Coefficients of the linear regression of the Hungarian sample.
Health anxiety had a positive direct and indirect effect on scale absorption, depersonalization, and the summated score of dissociation in both samples and both measurement times. Its effect on amnesia was positive and only indirect in the Hungarian sample, while in the international sample, it had a positive indirect effect in both measurement times, a positive direct effect in the second measurement time, and a positive tendential direct effect (p = 0.051) in the first measurement time.
Considering social support, support by others had no effect on dissociation in the international sample. In the Hungarian sample, there were negative direct effects on depersonalization and amnesia, but only in the second measurement for the latter one. Support by the family showed no effect in the international sample at all, while both direct and indirect negative effects can be seen on each scale regarding the Hungarian sample. There was no direct effect in the case of support by friends, but regarding the international sample it had negative indirect effects on absorption, and in the first measurement on amnesia. While in the Hungarian sample, negative effects can be seen on every scale in the second measurement.
Investigating the effects of coping in the international sample, wishful thinking had positive indirect effects on every scale, and positive direct effects on absorption and, in the first measurement, on depersonalization. Goal-oriented coping had negative indirect effects in the first measurement. Seeking for support had an effect only in the case of absorption and a direct effect in the first measurement. We found a negative indirect effect in the case of think over coping, and tendential positive direct effects of absorption and amnesia (pabs = 0.051, pamn = 0.054) but only in the first measurement. Avoiding seemed to have positive direct effects in every scale of dissociation in the first measurements.
In the Hungarian sample, humor had a negative indirect effect on each scale, and there was a tendential positive effect (p = 0.055) in the second measurement of amnesia. Positive thinking was found to have negative indirect effects, while having positive direct effects in the first measurement. There were positive direct and indirect effects on all the scales in the case of distancing. While the outer perspective did not show any significant effect.
The results of direct and indirect effects are summarized in Table 8 and Table 9. The index of moderated mediation was significant only for think over and goal-oriented coping in the international sample.

Table 8.
Coefficients of the linear regression of the Hungarian sample.

Table 9.
Coefficients of the linear regression of the International sample.
4. Discussion
Our study aimed to investigate how health anxiety, social support, and ways of coping contribute to dissociation directly and through the mediation of perceived stress, moderated by the time of measurement (lockdown). We investigated the effect of perceived stress on different forms (sub-scales) of dissociation.
Depersonalization showed significantly higher values in the second run regarding both Hungarian and international samples; amnesia was higher in the second round in the international sample. That is to say, maladaptive dissociative mechanisms occurred more often with time. Gender differences showed usually reported tendencies for females having higher scores than males [29,56].
Results showing that stress moderately correlated with dissociation in both the international and Hungarian samples are also consistent with the relevant literature [24,25]. Stress was found to relate to dissociation before [31], and also, adaptive forms of dissociation might be a way to cope with stressful situations, because in the context of trauma, it may serve as protection against overwhelming experiences [78]. According to our findings, prolonged stress was related to pathological dissociation (amnesia and depersonalization as well), while absorption as an adaptive coping strategy stayed on a high level over time during the pandemic.
Health anxiety correlated with perceived stress, consistent with previous research [79]. The general positive effect of health anxiety on overall dissociation and all its subscales is not surprising. This result indicates that there is a strong relationship between anxiety and dissociation, directly and through perceived stress as well. This result is consistent with previous research findings about health anxiety and dissociative experiences occurring at the same time [80]. This result emphasizes that reducing anxiety may have a double effect on controlling dissociative experiences: decreased anxiety itself may decrease dissociation directly and through stress reduction.
Results regarding social support were consistent with findings of recent publications reporting that social support moderates anxiety and stress caused by COVID-19 [35,38]. We found several differences between the Hungarian and International samples, as well as regarding measurement time. As to the Hungarian sample, support by the family was so important that it significantly decreased dissociative experiences directly and through decreasing perceived stress as well (considering all scales and both measures). Results reflected that international students were far from their families and in alliance with this we found no significant effects (the direct effect of social support from the family was not significantly decreasing for dissociation, and even slightly increased dissociation through perceived stress). Unlike the support of friends, that seemed to gain more importance for the international students. Again, satisfying social support was proved to relate to less dissociative experiences, consistent with some previous findings [40,41].
As to ways of coping, we found interesting and somewhat contradicting results. Regarding the international sample, the goal-oriented coping strategy had a strong decreasing effect on all dissociation scales in the first measurement, through the mediation of perceived stress. In this sample, wishful thinking proved to increase dissociative experiences overall, and in all its subscales through the mediation of perceived stress, and had a direct increasing effect on absorption and depersonalization. Wu et al [81] found the same adverse effect when examining the effects of COVID-specific wishful thinking of Chinese university students and found that the wishful thinking strategy increased anxiety and also prevented students from adaptive protective behaviors.
As to the Hungarian sample, positive thinking was found to decrease dissociation through decreasing perceived stress, while, just as wishful thinking in the international sample, it had a dissociation-increasing direct effect at the beginning of the pandemic. It may suggest that perceived stress had a strong enough overall effect on dissociation that even if positive thinking (or toxic positivity) may lead to dissociation, shifting from reality, it can still decrease stress and through this effect decreases dissociative experiences. Think over coping showed a similar tendency; it might directly lead to dissociation, but by decreasing stress, it seems to help decrease dissociative experiences. Humor as a strategy seems more confident in decreasing dissociation.
The avoiding coping strategy in the international sample was similar to the distancing coping strategy in the Hungarian sample and showed a similar increasing effect on dissociation directly and indirectly as well.
Our results are consistent with recent research findings [48,52], where problem-focused coping proved to be adaptive in stressful situations, and avoiding or denying things is not a useful strategy for they increase stress, and, in this way, dissociation. Further investigation of the interrelations of the variables is needed, a more complex model could be useful to help understand complicated correlations between the factors examined.
Dissociation can serve as an adaptive coping mechanism in unpredictable stressful situations, maladaptive ways of dissociation may increase the risk of the appearance of dissociative disorders.
Among other negative consequences of increasing dissociative behavior during the COVID-19 pandemic, recent studies report that increased addictive behaviors like alcohol consumption [82] and internet addiction [26] showed correlations with dissociative experiences. We think it is important to find possibilities to decrease the occurrence of dissociative experiences. According to our findings, there are several factors possibly contributing to (such as health anxiety and distancing coping strategy) or alleviating (such as social support) dissociation.
5. Conclusions
In respect of limitations, the generalizability of our results is restricted to the population of university students in Debrecen, which was appropriate for testing our model and for investigating the pattern of the interrelation of variables affecting dissociative experiences in the pandemic. On the other hand, other pandemic-related variables were controlled this way (e.g., area-specific factors like the number of cases). We have to take non-response errors into consideration though, that is to say, according to Biddle and Sollis [83], the characteristics (and so answers) of those who do not participate in a particular round of data collection may be different from those who do respond. Although considering the content of the questionnaires, we don’t presume major differences in the psychological contrasts, and the study field and study level of the students represented the whole spectrum of the university, this possibility should still be considered. A further methodological limitation of the study may be that perceived stress is assessed over one month, while health anxiety is assessed over six months.
Several studies have recently reported on the effects of stress on dissociative experiences, mainly in relation to the COVID-19 pandemic [26,27,28,29]. Our results are consistent with these findings, and unlike previous reports, we investigated the effect of perceived stress on the three mechanisms of dissociation with regard to other independent variables with conditional process modeling. Health anxiety, coping and social support appeared to influence dissociation directly and through the mediation of perceived stress. Social support, mainly support from the family and problem-focused coping strategies may decrease the level of stress, this way decreasing dissociative behavior.
When designing interventions and policies for a situation like the COVID-19 pandemic, these specific results should be taken into account.
Author Contributions
All authors (L.R.K., V.R., S.G., Á.H.-N., A.S.-N., M.S.-A. and K.H.-N.) contributed in Methodology, Data curation, Writing—original draft, and Writing—review & editing; Supervision: K.H.-N. and L.R.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Hungarian Ethical Review Committee for Research in Psychology (Reference number: 2020-45, date of approval: 22 April 2020) for studies involving humans.
Informed Consent Statement
Written informed consent has been obtained from the participating students to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical reasons.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Coronavirus Disease (COVID-19) Outbreak Situation. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 15 December 2022).
- About Hungary. Hungary—COVID-19. Available online: http://abouthungary.hu/coronavirus/ (accessed on 15 December 2022).
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Aknin, L.B.; De Neve, J.E.; Dunn, E.W.; Fancourt, D.E.; Goldberg, E.; Helliwell, J.F.; Jones, S.P.; Karam, E.; Layard, R.; Lyubomirsky, S.; et al. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. Perspect. Psychol. Sci. 2022, 17, 915–936. [Google Scholar] [CrossRef]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef]
- Onyeaka, H.; Anumudu, C.K.; Al-Sharify, Z.T.; Egele-Godswill, E.; Mbaegbu, P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci. Prog. 2021, 104, 368504211019854. [Google Scholar] [CrossRef]
- Prati, G.; Mancini, A.D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021, 51, 201–211. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Birmes, P.; Brunet, A.; Benoit, M.; Defer, S.; Hatton, L.; Sztulman, H.; Schmitt, L. Validation of the Peritraumatic Dissociative Experiences Questionnaire self-report version in two samples of French-speaking individuals exposed to trauma. Eur. Psychiatry 2005, 20, 145–151. [Google Scholar] [CrossRef]
- Daglis, T. The Increase in Addiction during COVID-19. Encyclopedia 2021, 1, 1257–1266. [Google Scholar] [CrossRef]
- Černis, E.; Evans, R.; Ehlers, A.; Freeman, D. Dissociation in relation to other mental health conditions: An exploration using network analysis. J. Psychiatr Res. 2021, 136, 460–467. [Google Scholar] [CrossRef]
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schmidt, M.V.; de Quervain, D.; van Amelsvoort, T.; Bisson, J.I.; Cryan, J.F.; Howes, O.D.; Pinto, L.; et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. Eur. Neuropsychopharmacol. 2022, 55, 22–83. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Wen, W.; Zhang, H.; Ni, J.; Jiang, J.; Cheng, Y.; Zhou, M.; Ye, L.; Feng, Z.; Ge, Z.; et al. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: A systematic review and meta-analysis. J. Am. Coll. Health 2021, 1, 1–8. [Google Scholar] [CrossRef]
- Elharake, J.A.; Akbar, F.; Malik, A.A.; Gilliam, W.; Omer, S.B. Mental Health Impact of COVID-19 among Children and College Students: A Systematic Review. Child Psychiatry Hum. Dev. 2022, 11, 1–13. [Google Scholar] [CrossRef]
- Van der Kolk, B.A.; van der Hart, O. Pierre Janet and the breakdown of adaptation in psychological trauma. Am. J. Psychiatry 1989, 146, 1530–1540. [Google Scholar] [CrossRef]
- Bernstein, E.M.; Putnam, F.W. Development, reliability, and validity of a dissociation scale. J. Nerv. Ment. Dis. 1986, 174, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Grabe, H.J.; Rainermann, S.; Spitzer, C.; Gänsicke, M.; Freyberger, H.J. The relationship between dimensions of alexithymia and dissociation. Psychother. Psychosom. 2000, 69, 128–131. [Google Scholar] [CrossRef]
- Waller, N.; Putnam, F.W.; Carlson, E.B. Types of dissociation and dissociative types: A taxometric analysis of dissociative experiences. Psychol. Methods 1996, 1, 300–321. [Google Scholar] [CrossRef]
- Spitzer, C.; Barnow, S.; Freyberger, H.J.; Grabe, H.J. Recent developments in the theory of dissociation. World Psychiatry 2006, 5, 82–86. [Google Scholar]
- Lynn, C.D. Adaptive and Maladaptive Dissociation: An Epidemiological and Anthropological Comparison and Proposition for an Expanded Dissociation Model. Anthropol. Conscious 2005, 16, 16–49. [Google Scholar] [CrossRef]
- Van der Kolk, B.A.; Fisler, R. Dissociation and the fragmentary nature of traumatic memories: Overview and exploratory study. J. Trauma. Stress 1995, 8, 505–525. [Google Scholar] [CrossRef] [PubMed]
- Schauer, M.; Elbert, T. Dissociation following traumatic stress: Etiology and treatment. J. Psychol. 2010, 218, 109–127. [Google Scholar] [CrossRef]
- La Rosa, V.L.; Gori, A.; Faraci, P.; Vicario, C.M.; Craparo, G. Traumatic Distress, Alexithymia, Dissociation, and Risk of Addiction During the First Wave of COVID-19 in Italy: Results from a Cross-sectional Online Survey on a Non-clinical Adult Sample. Int. J. Ment. Health Addict. 2022, 20, 3128–3144. [Google Scholar] [CrossRef]
- Chiara, C.; Giorgio, V.; Claudio, B.; Virginia, C.; Antonio, D.C.; Carlo, L. Escaping the Reality of the Pandemic: The Role of Hopelessness and Dissociation in COVID-19 Denialism. JPM 2022, 12, 1302. [Google Scholar] [CrossRef]
- Velotti, P.; Civilla, C.; Rogier, G.; Beomonte Zobel, S. A Fear of COVID-19 and PTSD Symptoms in Pathological Personality: The Mediating Effect of Dissociation and Emotion Dysregulation. Front. Psychiatry 2021, 23, 590021. [Google Scholar] [CrossRef]
- Azoulay, E.; Cariou, A.; Bruneel, F.; Demoule, A.; Kouatchet, A.; Reuter, D.; Souppart, V.; Combes, A.; Klouche, K.; Argaud, L.; et al. Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study. Am. J. Respir. Crit. Care Med. 2020, 202, 1388–1398. [Google Scholar] [CrossRef] [PubMed]
- Savage, M.J.; James, R.; Magistro, D.; Donaldson, J.; Healy, L.C.; Nevill, M.; Hennis, P.J. Mental health and movement behaviour during the COVID-19 pandemic in UK university students: Prospective cohort study. MENPA 2020, 19, 100357. [Google Scholar]
- De Wachter, D.; Lange, A.; Vanderlinden, J.; Pouw, J.; Strubbe, E. The influence of current stress on dissociative experiences: An exploratory study in a non-clinical population. J. Trauma Dissociation 2006, 7, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Syme, S.L. Social Support and Health, 1st ed.; Academic Press: San Fransisco, CA, USA, 1985; pp. 3–22. [Google Scholar]
- House, J.S.; Umberson, D.; Landis, K.R. Structures and processes of social support. Annu. Rev. Sociol. 1988, 14, 293–318. [Google Scholar] [CrossRef]
- Saltzman, L.Y.; Hansel, T.C.; Bordnick, P.S. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol. Trauma 2020, 12, S55–S57. [Google Scholar] [CrossRef] [PubMed]
- Szkody, E.; Stearns, M.; Stanhope, L.; McKinney, C. Stress-Buffering Role of Social Support during COVID-19. Fam. Process 2021, 60, 1002–1015. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Luo, S.; Mu, W.; Li, Y.; Ye, L.; Zheng, X.; Xu, B.; Ding, Y.; Ling, P.; Zhou, M.; et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 16. [Google Scholar] [CrossRef] [PubMed]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, A.; Tohme, P.; Abi-Habib, R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef]
- Labrague, L.J.; De Los Santos, J.A.A.; Falguera, C.C. Social and emotional loneliness among college students during the COVID-19 pandemic: The predictive role of coping behaviors, social support, and personal resilience. Perspect. Psychiatr. Care 2021, 57, 1578–1584. [Google Scholar] [CrossRef]
- Baranyi, A.; Leithgöb, O.; Kreiner, B.; Tanzer, K.; Ehrlich, G.; Hofer, H.P.; Rothenhäusler, H.B. Relationship between posttraumatic stress disorder, quality of life, social support, and affective and dissociative status in severely injured accident victims 12 months after trauma. Psychosomatics 2010, 51, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Coronas, R.; García-Parés, G.; Viladrich, C.; Santos, J.M.; Menchón, J.M. Clinical and sociodemographic variables associated with the onset of posttraumatic stress disorder in road traffic accidents. Depress. Anxiety 2008, 25, E16–E23. [Google Scholar] [CrossRef] [PubMed]
- Korol, S. Familial and social support as protective factors against the development of dissociative identity disorder. J. Trauma Dissociation 2008, 9, 249–267. [Google Scholar] [CrossRef]
- Abramowitz, J.S.; Braddock, A. Hypochondriasis and Health Anxiety, 1st ed.; Hogrefe Publishing: Cambridge, UK, 2011; pp. 1–9. [Google Scholar]
- Asmundson, G.J.G.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 102211. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef]
- Li, Y.; Wang, A.; Wu, Y.; Han, N.; Huang, H. Impact of the COVID-19 Pandemic on the Mental Health of College Students: A Systematic Review and Meta-Analysis. Front. Psychol. 2021, 12, 669119. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.; Folkman, S. Stress, Appraisal, and Coping, 1st ed.; Springer Publishing: New York, NY, USA, 1984; pp. 1–60. [Google Scholar]
- Erick, T.B. Knowledge, Attitudes, Anxiety, and Coping Strategies of Students during COVID-19 Pandemic. J. Loss Trauma 2020, 25, 635–642. [Google Scholar] [CrossRef]
- Budimir, S.; Probst, T.; Pieh, C. Coping strategies and mental health during COVID-19 lockdown. J. Ment. Health 2021, 30, 156–163. [Google Scholar] [CrossRef]
- Li, S.; Liu, H.; Bai, X.W. The “psychological eye of typhoon” effect in wenchuan “5.12” earthquake. Sci. Technol. Rev. 2009, 27, 87–89. [Google Scholar]
- Huang, L.; Lei, W.; Xu, F.; Liu, H.; Yu, L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: A comparative study. PLoS ONE 2020, 15, e0237303. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Transactional theory and research on emotions and coping. EJP 1987, 1, 141–169. [Google Scholar] [CrossRef]
- Kar, N.; Kar, B.; Kar, S. Stress and coping during COVID-19 pandemic: Result of an online survey. Psychiatry Res. 2021, 295, 113598. [Google Scholar] [CrossRef]
- Pashazadeh Kan, F.; Raoofi, S.; Rafiei, S.; Khani, S.; Hosseinifard, H.; Tajik, F.; Raoofi, N.; Ahmadi, S.; Aghalou, S.; Torabi, F.; et al. A systematic review of the prevalence of anxiety among the general population during the COVID-19 pandemic. J. Affect. Disord. 2021, 293, 391–398. [Google Scholar] [CrossRef]
- Thibaut, F.; van Wijngaarden-Cremers, P.J.M. Women’s Mental Health in the Time of COVID-19 Pandemic. Front. Glob. Womens Health 2020, 1, 588372. [Google Scholar] [CrossRef]
- Sundarasen, S.; Chinna, K.; Kamaludin, K.; Nurunnabi, M.; Baloch, G.M.; Khoshaim, H.B.; Hossain, S.F.A.; Sukayt, A. Psychological Impact of COVID-19 and Lockdown among University Students in Malaysia: Implications and Policy Recommendations. Int. J. Environ. Res. Public Health 2020, 17, 6206. [Google Scholar] [CrossRef] [PubMed]
- Commodari, E.; La Rosa, V.L.; Carnemolla, G.; Parisi, J. The psychological impact of the lockdown on Italian university students during the first wave of COVID-19 pandemic: Psychological experiences, health risk perceptions, distance learning, and future perspectives. MJCP 2021, 9, 1–19. [Google Scholar]
- Almeida, M.; Shrestha, A.D.; Stojanac, D.; Miller, L.J. The impact of the COVID-19 pandemic on women’s mental health. Arch. Womens Ment. Health 2020, 23, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Sahu, P. Closure of Universities Due to Coronavirus Disease 2019 (COVID-19): Impact on Education and Mental Health of Students and Academic Staff. Cureus 2020, 12, e7541. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, K.; Vishwakarma, D.K.; Singh, N. COVID-19 and its impact on education, social life and mental health of students: A survey. Child. Youth Serv. Rev. 2021, 121, 105866. [Google Scholar] [CrossRef] [PubMed]
- Kaparounaki, C.K.; Patsali, M.E.; Mousa, D.V.; Papadopoulou, E.V.K.; Papadopoulou, K.K.K.; Fountoulakis, K.N. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020, 290, 113111. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Spacapan, S.; Oskamp, S. The Social Psychology of Health, 1st ed.; SAGE Publications: Thousand Oaks, CA, USA, 1988; pp. 31–67. [Google Scholar]
- Stauder, A.; Thege, B.K. Az Észlelt Stressz Kérdőív (PSS) Magyar Verziójának Jellemzői. Mentálhig Pszichoszomatika 2006, 7, 203–216. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Papp-Zipernovszky, O.; Kékesi, M.Z.; Jámbori, S. A Multidimenzionális Észlelt Társas Támogatás Kérdőív magyar nyelvű validálása. Mentálhig Pszichoszomatika 2017, 18, 230–262. [Google Scholar] [CrossRef]
- Salkovskis, P.M.; Rimes, K.A.; Warwick, H.M.C. The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol. Med. 2002, 32, 843. [Google Scholar] [CrossRef] [PubMed]
- Köteles, F.; Simor, P.; Bárdos, G. Validation and psychometric evaluation of the Hungarian version of the Short Health Anxiety Inventory (SHAI). Mentálhigiéné Pszichoszomatika 2011, 12, 191–213. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J. Pers. Soc. Psychol. 1985, 48, 150–170. [Google Scholar] [CrossRef] [PubMed]
- Sørlie, T.; Sexton, H.C. The factor structure of “The Ways of Coping Questionnaire” and the process of coping in surgical patients. Pers. Individ. Differ. 2001, 30, 961–975. [Google Scholar] [CrossRef]
- Rózsa, S.; Purebl, G.; Susánszky, É.; Kő, N.; Szádóczky, E.; Réthelyi, J.; Danis, I.; Skrabski, Á.; Kopp, M. Dimensions of coping: Hungarian adaptation of the Ways of Coping Questionnaire. Mentálhigiéné Pszichoszomatika 2008, 9, 217–241. [Google Scholar] [CrossRef]
- Carlson, E.B.; Putnam, F.W. Dissociation: An update on the Dissociative Experience Scale. Univ. Oregon. Sch. Bank 1993, 6, 16–27. [Google Scholar]
- Perczel-Forintos, D.; Ajtay, G.; Barna, C.; Kiss, Z.; Komlósi, S. Kérdőívek, Becslőskálák a Klinikai Pszichológiában, 3rd ed.; Semmelweis Kiadó: Budapest, Hungary, 2018; p. 230. [Google Scholar]
- Alberts, N.M.; Hadjistavropoulos, H.D.; Jones, S.L.; Sharpe, D. The Short Health Anxiety Inventory: A systematic review and meta-analysis. J. Anxiety Disord. 2013, 27, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Vanderlinden, J.; Van Dyck, R.; Vandereycken, W.; Vertommen, H. The Dissociation Questionnaire (Dis-G): Development, reliability and validity of a new self-reporting Dissociation Questionnaire. Acta Psychiatr. Belg. 1994, 94, 53–54. [Google Scholar]
- Chu, J.A. Rebuilding Shattered Lives: Treating Complex PTSD and Dissociative Disorders, 2nd ed.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Andrew, F.H. Introduction to Mediation, Moderation, and Conditional Process Analysis, 2nd ed.; The Guilford Press: New York, NY, USA, 2018; p. 588. [Google Scholar]
- Paul, F.D.; John, A.O. Dissociation and the Dissociative Disorders: DSM-V and Beyond, 1st ed.; Routledge: Oxfordshire, UK, 2009; pp. 145–154. [Google Scholar]
- Asmundson, G.J.; Abramowitz, J.S.; Richter, A.A.; Whedon, M. Health anxiety: Current perspectives and future directions. Curr. Psychiatry Rep. 2010, 12, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Ray, S.; Ray, R.; Singh, N.; Paul, I. Dissociative experiences and health anxiety in panic disorder. Indian J. Psychiatry 2021, 63, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zheng, Y.; Xiong, S.; Zhang, W.; Guo, S. The Effect of Perceived Threat Avoidability of COVID-19 on Coping Strategies and Psychic Anxiety Among Chinese College Students in the Early Stage of COVID-19 Pandemic. Front. Psychiatry 2022, 3, 854698. [Google Scholar] [CrossRef]
- Rodriguez, L.M.; Litt, D.M.; Stewart, S.H. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict. Behav. 2020, 110, 106532. [Google Scholar] [CrossRef] [PubMed]
- Biddle, N.; Sollis, K. Determinants of Participation in a Longitudinal Survey during the COVID-19 Pandemic: The Case of a Low-Infection Country; Bristol University Press: Bristol, UK, 2021. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).