Musculoskeletal Fitness for Identifying Low Physical Function in Older Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Musculoskeletal Fitness
2.3. Physical Functioning
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Factsheet—Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 12 January 2022).
- Boss, G.R.; Seegmiller, J.E. Age-related physiological changes and their clinical significance. West. J. Med. 1981, 135, 434–440. [Google Scholar] [PubMed]
- Nilwik, R.; Snijders, T.; Leenders, M.; Groen, B.B.; van Kranenburg, J.; Verdijk, L.B.; van Loon, L.J. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp. Gerontol. 2013, 48, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Brunner, F.; Schmid, A.; Sheikhzadeh, A.; Nordin, M.; Yoon, J.; Frankel, V. Effects of aging on Type II muscle fibers: A systematic review of the literature. J. Aging Phys. Act. 2007, 15, 336–348. [Google Scholar] [CrossRef] [PubMed]
- Lally, F.; Crome, P. Understanding frailty. Postgrad. Med. J. 2007, 83, 16–20. [Google Scholar] [CrossRef]
- Cawthon, P.M.; Visser, M.; Arai, H.; Ávila-Funes, J.A.; Barazzoni, R.; Bhasin, S.; Cruz-Jentoft, A.J. Defining terms commonly used in sarcopenia research: A glossary proposed by the Global Leadership in Sarcopenia (GLIS) Steering Committee. Eur. Geriatr. Med. 2022, 13, 1239–1244. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Zamboni, M. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Patrizio, E.; Calvani, R.; Marzetti, E.; Cesari, M. Physical Functional Assessment in Older Adults. J. Frailty Aging 2021, 10, 141–149. [Google Scholar] [CrossRef]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker for Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef]
- McGrath, R.P.; Kraemer, W.J.; Snih, S.A.; Peterson, M.D. Handgrip Strength and Health in Aging Adults. Sports Med. 2018, 48, 1993–2000. [Google Scholar] [CrossRef]
- Buckner, S.L.; Dankel, S.J.; Bell, Z.W.; Abe, T.; Loenneke, J.P. The Association of Handgrip Strength and Mortality: What Does It Tell Us and What Can We Do with It? Rejuvenation Res. 2019, 22, 230–234. [Google Scholar] [CrossRef]
- Grgic, J.; Garofolini, A.; Orazem, J.; Sabol, F.; Schoenfeld, B.J.; Pedisic, Z. Effects of Resistance Training on Muscle Size and Strength in Very Elderly Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sports Med. 2020, 50, 1983–1999. [Google Scholar] [CrossRef]
- Hetherington-Rauth, M.; Magalhães, J.P.; Alcazar, J.; Rosa, G.B.; Correia, I.R.; Ara, I.; Sardinha, L.B. Relative sit-to-stand muscle power predicts an older adult’s physical independence at age 90 beyond that of relative handgrip strength, physical activity and sedentary time: A cross-sectional analysis. Am. J. Phys. Med. Rehabil. 2022, 101, 995–1000. [Google Scholar] [CrossRef]
- Reid, K.F.; Fielding, R.A. Skeletal muscle power: A critical determinant of physical functioning in older adults. Exerc. Sport Sci. Rev. 2012, 40, 4–12. [Google Scholar] [CrossRef]
- Zymbal, V.; Carrasco, L.; Sañudo, B.; Luís, D.; Baptista, F. Mediating effect of muscle power on the relationship of physical activity with physical fitness and physical function in older women. Exp. Gerontol. 2022, 158, 111660. [Google Scholar] [CrossRef]
- Baltasar-Fernandez, I.; Alcazar, J.; Losa-Reyna, J.; Soto-Paniagua, H.; Alegre, L.M.; Takai, Y.; Ara, I. Comparison of available equations to estimate sit-to-stand muscle power and their association with gait speed and frailty in older people: Practical applications for the 5-rep sit-to-stand test. Exp. Gerontol. 2021, 156, 111619. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E. Measuring functional fitness of older adults. J. Act. Aging March 2002, 24–30. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Ngueleu, A.M.; Barthod, C.; Best, K.L.; Routhier, F.; Otis, M.; Batcho, C.S. Criterion validity of ActiGraph monitoring devices for step counting and distance measurement in adults and older adults: A systematic review. J. Neuroeng. Rehabil. 2022, 19, 112. [Google Scholar] [CrossRef]
- Buehring, B.; Krueger, D.; Fidler, E.; Gangnon, R.; Heiderscheit, B.; Binkley, N. Reproducibility of jumping mechanography and traditional measures of physical and muscle function in older adults. Osteoporos. Int. 2015, 26, 819–825. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Blair, S.N. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [PubMed]
- McLeod, M.; Breen, L.; Hamilton, D.L.; Philp, A. Live strong and prosper: The importance of skeletal muscle strength for healthy ageing. Biogerontology 2016, 17, 497–510. [Google Scholar] [CrossRef]
- Wang, D.X.M.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef] [PubMed]
- Meskers, C.G.M.; Reijnierse, E.M.; Numans, S.T.; Kruizinga, R.C.; Pierik, V.D.; Van Ancum, J.M.; Maier, A.B. Association of Handgrip Strength and Muscle Mass with Dependency in (Instrumental) Activities of Daily Living in Hospitalized Older Adults —The EMPOWER Study. J. Nutr. Health Aging 2019, 23, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Bahat, G.; Kilic, C.; Eris, S.; Karan, M.A. Power Versus Sarcopenia: Associations with Functionality and Physical Performance Measures. J. Nutr. Health Aging 2021, 25, 13–17. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; McBurnie, M.A. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Runge, M.; Rittweger, J.; Russo, C.R.; Schiessl, H.; Felsenberg, D. Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross-section, chair-rising test and jumping power. Clin. Physiol. Funct. Imaging 2004, 24, 335–340. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Rodrigues, B.; Gonçalves, I.O.; Asano, R.Y.; Uchida, M.C.; Marzetti, E. The physical capabilities underlying timed “Up and Go” test are time-dependent in community-dwelling older women. Exp. Gerontol. 2018, 104, 138–146. [Google Scholar] [CrossRef]
- Chen, T.; Chou, L.S. Effects of Muscle Strength and Balance Control on Sit-to-Walk and Turn Durations in the Timed Up and Go Test. Arch. Phys. Med. Rehabil. 2017, 98, 2471–2476. [Google Scholar] [CrossRef]
- Tsubaki, A.; Kubo, M.; Kobayashi, R.; Jigami, H.; Sugawara, K.; Takahashi, H.E. Maximum Power during Vertical Jump and Isometric Knee Extension Torque Alter Mobility Performance: A Cross-Sectional Study of Healthy Individuals. PM R. 2016, 8, 19–27. [Google Scholar] [CrossRef]
- Strotmeyer, E.S.; Winger, M.E.; Cauley, J.A.; Boudreau, R.M.; Cusick, D.; Collins, R.F.; Osteoporotic Fractures in Men (MrOS) Research Group. Normative Values of Muscle Power using Force Plate Jump Tests in Men Aged 77-101 Years: The Osteoporotic Fractures in Men (MrOS) Study. J. Nutr. Health Aging 2018, 22, 1167–1175. [Google Scholar] [CrossRef]
- Rose, D.; Jones, C.; Lucchese, N. Predicting the Probability of Falls in Community-Residing Older Adults Using the 8-Foot Up and-Go: A New Measure of Functional Mobility. J. Aging Phys. Act. 2002, 10, 4. [Google Scholar] [CrossRef]
- Ramsey, K.A.; Rojer, A.G.M.; D’Andrea, L.; Otten, R.H.; Heymans, M.W.; Trappenburg, M.C.; Maier, A.B. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 67, 101266. [Google Scholar] [CrossRef]
- Lopez, P.; Rech, A.; Petropoulou, M.; Newton, R.U.; Taaffe, D.R.; Galvão, D.A.; Turella, D.J.P.; Freitas, S.R.; Radaelli, R. Does high-velocity resistance exercise elicit greater physical function benefits than traditional resistance exercise in older adults? A systematic review and network meta-analysis of 79 trials. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2022, Glac230. [Google Scholar] [CrossRef]
| Mean (SD) | Standard Deviation | |
|---|---|---|
| Age, y | 73.62 | 8.23 |
| Body Mass, kg | 66.25 | 12.33 |
| Body Height, cm | 151.59 | 6.25 |
| BMI, kg/m2 | 19.87 | 3.05 |
| CPF Score (pts) | 19.97 | 4.49 |
| TUG (s) | 6.30 | 1.86 |
| Daily Steps (n) | 6364 | 2726 |
| Handgrip, kg | 21.7 | 21.7 |
| Rel. Handgrip, Kg/Kg | 0.33 | 0.74 |
| VJ Power, W | 1150 | 340 |
| Rel VJ Power, W/Kg | 17.64 | 4.53 |
| VJ Force, N | 1280 | 290 |
| Rel VJ Force, N/Kg | 19.46 | 3.14 |
| Low CPF (%) | 10.6 | - |
| Low TUG (%) | 13.6 | - |
| Low Daily Steps (%) | 21.2 | - |
| Variables | CPF | TUG | Daily Mobility |
|---|---|---|---|
| Handgrip Strength | 0.433 ** | −0.441 ** | 0.186 |
| Rel Handgrip strength | 0.503 ** | −0.292 * | 0.252 |
| Jump Power | 0.490 ** | −0.469 ** | 0.384 ** |
| Rel Jump Power | 0.575 ** | −0.371 ** | 0.460 ** |
| Jump Force | 0.062 | −0.189 | 0.390 |
| Rel Jump Force | 0.160 | −0.01 | 0.136 |
| Cutoff | Percentile | AUC (95% CI) | p-Value | Se | Sp | Odds Ratio (95% CI) a | |
|---|---|---|---|---|---|---|---|
| Rel. Handgrip (kg/kg) | |||||||
| Low Physical Function | - | 0.65 (0.43, 0.86) | 0.208 | - | - | - | |
| Low Gait Speed/Agility | - | 0.65 (0.44, 0.87) | 0.142 | - | - | - | |
| Low Daily Mobility | - | 0.64 (0.46, 0.82) | 0.115 | - | - | - | |
| Handgrip (kg) | |||||||
| Low Physical Function | - | 0.59 (0.38, 0.80) | 0.429 | - | - | - | |
| Low Gait Speed/Agility | 19.5 | 32 | 0.75 (0.57, 0.92) | 0.019 | 55.6 | 71.9 | 0.801 (0.670, 0.959) |
| Low Daily Mobility | - | 0.54 (0.36, 0.71) | 0.697 | - | - | - | |
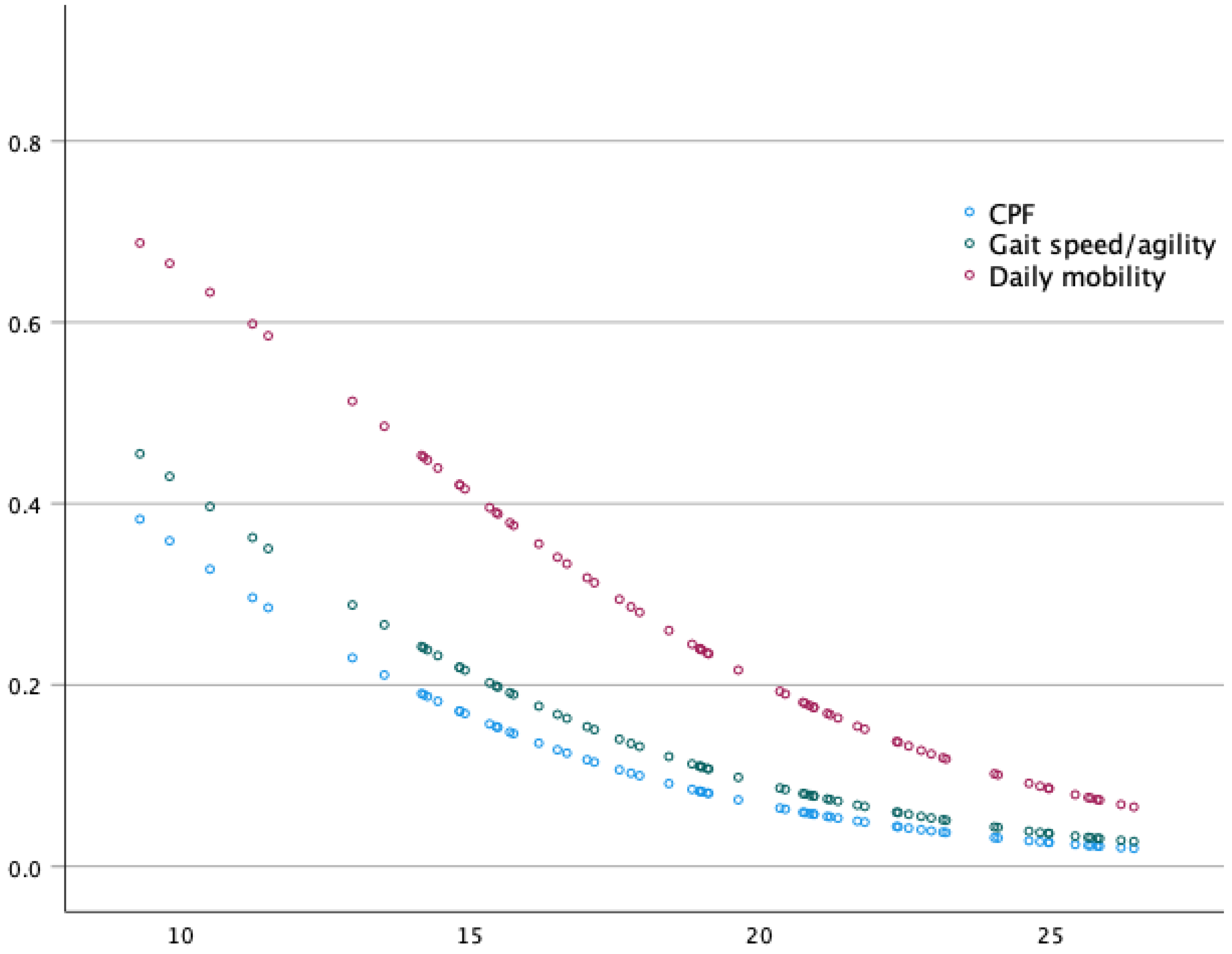
| Rel Jump Power (W/kg) | |||||||
| Low Physical Function | 13.9 | 24 | 0.79 (0.64, 0.94) | 0.013 | 71.4 | 81.4 | 0.790 (0.644, 0.969) |
| Low Gait Speed/Agility | 15.2 | 35 | 0.74 (0.56, 0.92) | 0.023 | 66.7 | 70.2 | 0.814 (0.682, 0.972) |
| Low Daily Mobility | 17.1 | 44 | 0.73 (0.59, 0.87) | 0.011 | 64.3 | 65.1 | 0.838 (0.721, 0.974) |
| Jump Power (W) | |||||||
| Low Physical Function | 1011 | 32 | 0.73 (0.54, 0.93) | 0.044 | 71.4 | 72.9 | 0.997 (0.994, 1.00) |
| Low Gait Speed/Agility | 800 | 18 | 0.78 (0.59, 0.96) | 0.008 | 66.7 | 89.5 | 0.995 (0.992, 0.999) |
| Low Daily Mobility | - | 0.63 (0.47, 0.79) | 0.148 | - | - | - | |
| Rel Jump Force (N/kg) | |||||||
| Low Physical Function | - | 0.55 (0.32,0.77) | 0.700 | - | - | - | |
| Low Gait Speed/Agility | - | 0.41 (0.25,0.57) | 0.385 | - | - | - | |
| Low Daily Mobility | - | 0.52 (0.36,0.68) | 0.824 | - | - | - | |
| Jump Force (N) | |||||||
| Low Physical Function | - | 0.52 (0.29,0.74) | 0.892 | - | - | - | |
| Low Gait Speed/Agility | - | 0.60 (0.32,0.75) | 0.327 | - | - | - | |
| Low Daily Mobility | - | 0.44 (0.27,0.60) | 0.493 | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abreu, F.; Zymbal, V.; Baptista, F. Musculoskeletal Fitness for Identifying Low Physical Function in Older Women. Int. J. Environ. Res. Public Health 2023, 20, 5485. https://doi.org/10.3390/ijerph20085485
Abreu F, Zymbal V, Baptista F. Musculoskeletal Fitness for Identifying Low Physical Function in Older Women. International Journal of Environmental Research and Public Health. 2023; 20(8):5485. https://doi.org/10.3390/ijerph20085485
Chicago/Turabian StyleAbreu, Frederico, Vera Zymbal, and Fátima Baptista. 2023. "Musculoskeletal Fitness for Identifying Low Physical Function in Older Women" International Journal of Environmental Research and Public Health 20, no. 8: 5485. https://doi.org/10.3390/ijerph20085485
APA StyleAbreu, F., Zymbal, V., & Baptista, F. (2023). Musculoskeletal Fitness for Identifying Low Physical Function in Older Women. International Journal of Environmental Research and Public Health, 20(8), 5485. https://doi.org/10.3390/ijerph20085485





