A Meta-Analysis and Systematic Review of Community-Based Intimate Partner Violence Interventions in India
Abstract
1. Introduction
2. Materials and Methods
2.1. Identifying Relevant Studies
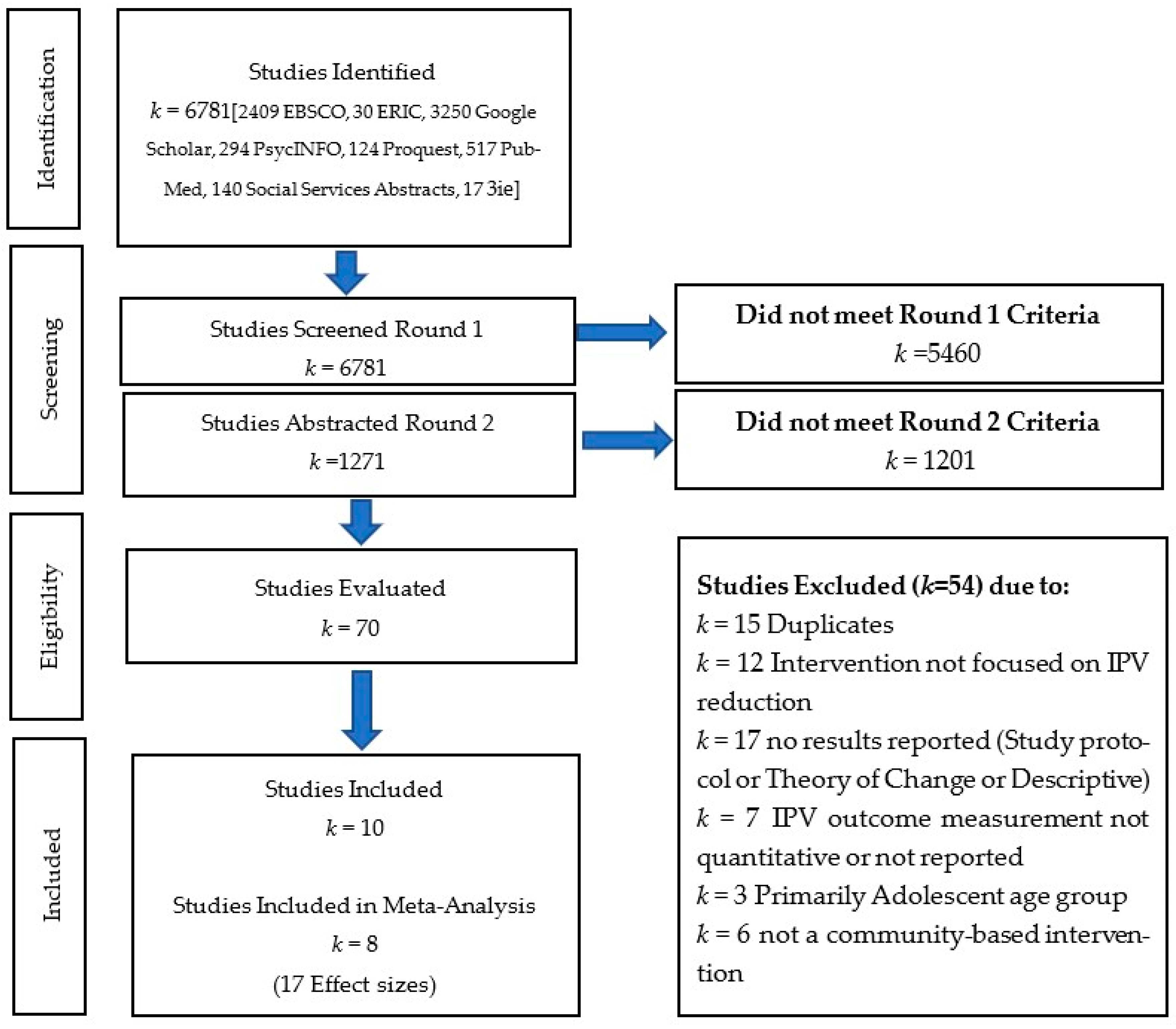
2.2. Study Selection
2.3. Search Results
2.4. Data Extraction
2.5. Data Analysis Plan
3. Results
3.1. Narrative Synthesis
3.1.1. Couple-Based Interventions
3.1.2. Individually Focused Interventions with Women
3.1.3. Multi-Level Interventions
3.2. Outcomes of Community-Based IPV Interventions
4. Discussion
Implications for Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Violence against Women Prevalence Estimates, 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence against Women. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/violence-against-women (accessed on 14 October 2022).
- Kalokhe, A.; del Rio, C.; Dunkle, K.; Stephenson, R.; Metheny, N.; Paranjape, A.; Sahay, S. Domestic Violence against Women in India: A Systematic Review of a Decade of Quantitative Studies. Glob. Public Health 2017, 12, 498–513. [Google Scholar] [CrossRef]
- Garg, P.; Das, M.; Goyal, L.D.; Verma, M. Trends and Correlates of Intimate Partner Violence Experienced by Ever-Married Women of India: Results from National Family Health Survey Round III and IV. BMC Public Health 2021, 21, 2012. [Google Scholar] [CrossRef] [PubMed]
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), 2019–2021; International Institute for Population Sciences (IIPS): Mumbai, India, 2021; Volume 1, Available online: http://rchiips.org/nfhs/NFHS-5Reports/NFHS-5_INDIA_REPORT.pdf (accessed on 25 October 2022).
- CDC. Fast Facts: Preventing Intimate Partner Violence; Center for Disease Control and Prevention: Atlanta, GA, USA, 2022. Available online: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/fastfact.html (accessed on 14 October 2022).
- Patra, P.; Prakash, J.; Patra, B.; Khanna, P. Intimate Partner Violence: Wounds Are Deeper. Indian J Psychiatry 2018, 60, 494. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, A.; Szoeke, C. The Effect of Intimate Partner Violence on the Physical Health and Health-Related Behaviors of Women: A Systematic Review of the Literature. Trauma Violence Abuse 2022, 23, 1157–1172. [Google Scholar] [CrossRef]
- Al-Modallal, H. Effect of Intimate Partner Violence on Health of Women of Palestinian Origin. Int. Nurs. Rev. 2016, 63, 259–266. [Google Scholar] [CrossRef]
- Karakurt, G.; Patel, V.; Whiting, K.; Koyutürk, M. Mining Electronic Health Records Data: Domestic Violence and Adverse Health Effects. J. Fam. Viol. 2017, 32, 79–87. [Google Scholar] [CrossRef]
- Decker, M.R.; Miller, E.; McCauley, H.L.; Tancredi, D.J.; Anderson, H.; Levenson, R.R.; Silverman, J.G. Recent Partner Violence and Sexual and Drug-Related STI/HIV Risk among Adolescent and Young Adult Women Attending Family Planning Clinics. Sex. Transm. Infect. 2014, 90, 145–149. [Google Scholar] [CrossRef]
- Taft, A.J.; Powell, R.L.; Watson, L.F. The Impact of Violence against Women on Reproductive Health and Child Mortality in Timor-Leste. Aust. N. Z. J. Public Health 2015, 39, 177–181. [Google Scholar] [CrossRef]
- Weiss, H.A.; Patel, V.; West, B.; Peeling, R.W.; Kirkwood, B.R.; Mabey, D. Spousal Sexual Violence and Poverty Are Risk Factors for Sexually Transmitted Infections in Women: A Longitudinal Study of Women in Goa, India. Sex. Transm. Infect. 2008, 84, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Kouyoumdjian, F.G.; Calzavara, L.M.; Bondy, S.J.; O’Campo, P.; Serwadda, D.; Nalugoda, F.; Kagaayi, J.; Kigozi, G.; Wawer, M.; Gray, R. Intimate Partner Violence Is Associated with Incident HIV Infection in Women in Uganda. AIDS 2013, 27, 1331–1338. [Google Scholar] [CrossRef]
- Lacey, K.K.; Mouzon, D.M. Severe Physical Intimate Partner Violence and the Mental and Physical Health of U.S. Caribbean Black Women. J. Women’s Health 2016, 25, 920–929. [Google Scholar] [CrossRef] [PubMed]
- Bacchus, L.J.; Ranganathan, M.; Watts, C.; Devries, K. Recent Intimate Partner Violence against Women and Health: A Systematic Review and Meta-Analysis of Cohort Studies. BMJ Open 2018, 8, e019995. [Google Scholar] [CrossRef] [PubMed]
- Chandra, P.S.; Satyanarayana, V.A.; Carey, M.P. Women Reporting Intimate Partner Violence in India: Associations with PTSD and Depressive Symptoms. Arch. Womens Ment. Health 2009, 12, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Kamimura, A.; Ganta, V.; Myers, K.; Thomas, T. Intimate Partner Violence and Physical and Mental Health among Women Utilizing Community Health Services in Gujarat, India. BMC Women’s Health 2014, 14, 127. [Google Scholar] [CrossRef] [PubMed]
- Bramhankar, M.; Reshmi, R.S. Spousal Violence against Women and Its Consequences on Pregnancy Outcomes and Reproductive Health of Women in India. BMC Women’s Health 2021, 21, 382. [Google Scholar] [CrossRef]
- Dhar, D.; McDougal, L.; Hay, K.; Atmavilas, Y.; Silverman, J.; Triplett, D.; Raj, A. Associations between Intimate Partner Violence and Reproductive and Maternal Health Outcomes in Bihar, India: A Cross-Sectional Study. Reprod. Health 2018, 15, 109. [Google Scholar] [CrossRef]
- Dietrich, D.M.; Schuett, J.M. Culture of Honor and Attitudes Toward Intimate Partner Violence in Latinos. SAGE Open 2013, 3, 215824401348968. [Google Scholar] [CrossRef]
- Yoshioka, M.R.; Choi, D.Y. Culture and Interpersonal Violence Research: Paradigm Shift to Create a Full Continuum of Domestic Violence Services. J. Interpers. Violence 2005, 20, 513–519. [Google Scholar] [CrossRef]
- Zark, L.; Satyen, L. Cross-Cultural Differences in Student Attitudes Toward Intimate Partner Violence: A Systematic Review. Trauma Violence Abuse 2022, 23, 1007–1022. [Google Scholar] [CrossRef]
- Chaurasia, H.; Debnath, P.; Srivastava, S.; Purkayastha, N. Is Socioeconomic Inequality Boosting Intimate Partner Violence in India? An Overview of the National Family Health Survey, 2005–2006 and 2015–2016. Glob. Soc. Welf. 2021, 8, 263–277. [Google Scholar] [CrossRef]
- Jin, X.; Doukas, A.; Beiting, M.; Viksman, A. Factors Contributing to Intimate Partner Violence among Men in Kerala, India. J. Fam. Viol. 2014, 29, 643–652. [Google Scholar] [CrossRef]
- Ler, P.; Sivakami, M.; Monárrez-Espino, J. Prevalence and Factors Associated with Intimate Partner Violence Among Young Women Aged 15 to 24 Years in India: A Social-Ecological Approach. J. Interpers. Violence 2020, 35, 4083–4116. [Google Scholar] [CrossRef]
- Ram, A.; Victor, C.; Christy, H.; Hembrom, S.; Cherian, A.; Mohan, V. Domestic Violence and Its Determinants among 15–49-Year-Old Women in a Rural Block in South India. Indian J. Community Med. 2019, 44, 362. [Google Scholar] [CrossRef]
- Sabri, B.; Renner, L.M.; Stockman, J.K.; Mittal, M.; Decker, M.R. Risk Factors for Severe Intimate Partner Violence and Violence-Related Injuries Among Women in India. Women Health 2014, 54, 281–300. [Google Scholar] [CrossRef]
- Dalal, K.; Lindqvist, K. A National Study of the Prevalence and Correlates of Domestic Violence among Women in India. Asia Pac. J. Public Health 2012, 24, 265–277. [Google Scholar] [CrossRef]
- Jeyaseelan, L.; Kumar, S.; Neelakantan, N.; Peedicayil, A.; Pillai, R.; Duvvury, N. Physical Spousal Violence against Women in India: Some Risk Factors. J. Biosoc. Sci. 2007, 39, 657–670. [Google Scholar] [CrossRef]
- Satheesan, S.C.; Satyaranayana, V.A. Quality of Marital Relationship, Partner Violence, Psychological Distress, and Resilience in Women with Primary Infertility. Int. J. Community Med. Public Health 2018, 5, 734–739. [Google Scholar] [CrossRef]
- Nongrum, R.; Thomas, E.; Lionel, J.; Jacob, K.S. Domestic Violence as a Risk Factor for Maternal Depression and Neonatal Outcomes: A Hospital-Based Cohort Study. Indian J. Psychol. Med. 2014, 36, 179–181. [Google Scholar] [CrossRef]
- Kalokhe, A.S.; Stephenson, R.; Kelley, M.E.; Dunkle, K.L.; Paranjape, A.; Solas, V.; Karve, L.; del Rio, C.; Sahay, S. The Development and Validation of the Indian Family Violence and Control Scale. PLoS ONE 2016, 11, e0148120. [Google Scholar] [CrossRef]
- Kaur, R.; Garg, S. Domestic Violence Against Women: A Qualitative Study in a Rural Community. Asia Pac. J. Public Health 2010, 22, 242–251. [Google Scholar] [CrossRef]
- Raj, A.; Sabarwal, S.; Decker, M.R.; Nair, S.; Jethva, M.; Krishnan, S.; Donta, B.; Saggurti, N.; Silverman, J.G. Abuse from In-Laws during Pregnancy and Post-Partum: Qualitative and Quantitative Findings from Low-Income Mothers of Infants in Mumbai, India. Matern. Child Health J. 2011, 15, 700–712. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothenstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Balaji, M.; Andrews, T.; Andrew, G.; Patel, V. The Acceptability, Feasibility, and Effectiveness of a Population-Based Intervention to Promote Youth Health: An Exploratory Study in Goa, India. J. Adolesc. Health 2011, 48, 453–460. [Google Scholar] [CrossRef]
- Cottler, L.B.; Satyanarayana, V.A.; O’Leary, C.C.; Vaddiparti, K.; Benegal, V.; Chandra, P.S. Feasibility and Effectiveness of HIV Prevention Among Wives of Heavy Drinkers in Bangalore, India. AIDS Behav. 2010, 14 (Suppl. 1), S168–S176. [Google Scholar] [CrossRef]
- Hartmann, M.; Datta, S.; Browne, E.N.; Appiah, P.; Banay, R.; Caetano, V.; Floreak, R.; Spring, H.; Sreevasthsa, A.; Thomas, S.; et al. A Combined Behavioral Economics and Cognitive Behavioral Therapy Intervention to Reduce Alcohol Use and Intimate Partner Violence Among Couples in Bengaluru, India: Results of a Pilot Study. J. Interpers. Violence 2021, 36, NP12456–NP12480. [Google Scholar] [CrossRef]
- Javalkar, P.; Platt, L.; Prakash, R.; Beattie, T.S.; Collumbien, M.; Gafos, M.; Ramanaik, S.; Davey, C.; Jewkes, R.; Watts, C.; et al. Effectiveness of a Multilevel Intervention to Reduce Violence and Increase Condom Use in Intimate Partnerships among Female Sex Workers: Cluster Randomised Controlled Trial in Karnataka, India. BMJ Glob. Health 2019, 4, e001546. [Google Scholar] [CrossRef]
- Kalokhe, A.S.; Iyer, S.; Gadhe, K.; Katendra, T.; Kolhe, A.; Rahane, G.; Stephenson, R.; Sahay, S. A Couples-Based Intervention (Ghya Bharari Ekatra) for the Primary Prevention of Intimate Partner Violence in India: Pilot Feasibility and Acceptability Study. JMIR Res 2021, 5, e26130. [Google Scholar] [CrossRef]
- Nair, N.; Daruwalla, N.; Osrin, D.; Rath, S.; Gagrai, S.; Sahu, R.; Pradhan, H.; De, M.; Ambavkar, G.; Das, N.; et al. Community Mobilisation to Prevent Violence against Women and Girls in Eastern India through Participatory Learning and Action with Women’s Groups Facilitated by Accredited Social Health Activists: A before-and-after Pilot Study. BMC Int. Health Hum. Rights 2020, 20, 6. [Google Scholar] [CrossRef]
- Nieder, C.; Bosch, J.F.; Nockemann, A.P.; Kärtner, J. Evaluation of RISE: A Sexual Violence Prevention Program for Female College Students in India. J. Interpers. Violence 2022, 37, NP5538–NP5565. [Google Scholar] [CrossRef]
- Reza-Paul, S.; Lorway, R.; O’Brien, N.; Lazarus, L.; Jain, J.; Bhagya, M.; Fathima Mary, P.; Venukumar, K.T.; Raviprakash, K.N.; Baer, J.; et al. Sex Worker-Led Structural Interventions in India: A Case Study on Addressing Violence in HIV Prevention through the Ashodaya Samithi Collective in Mysore. Indian J. Med. Res. 2012, 135, 98–106. [Google Scholar] [CrossRef]
- Saggurti, N.; Nair, S.; Silverman, J.G.; Naik, D.D.; Battala, M.; Dasgupta, A.; Balaiah, D.; Raj, A. Impact of the RHANI Wives Intervention on Marital Conflict and Sexual Coercion. Int. J. Gynaecol. Obs. 2014, 126, 18–22. [Google Scholar] [CrossRef]
- Schensul, S.L.; Saggurti, N.; Burleson, J.A.; Singh, R. Community-Level HIV/STI Interventions and Their Impact on Alcohol Use in Urban Poor Populations in India. AIDS Behav. 2010, 14, 158–167. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis; Version 3 [Computer Software]; Biostat: Brandon, FL, USA, 2014. [Google Scholar]
- Cumming, G. Understanding the New Statistics: Effect Sizes, Confidence Intervals, and Meta-Analysis; Routledge: New York, NY, USA, 2011. [Google Scholar]
- Rosenthal, R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979, 86, 638–641. [Google Scholar] [CrossRef]
| Table One: Evaluations of Community-Based IPV Interventions in India | |||||||
|---|---|---|---|---|---|---|---|
| Study | Condition of Intervention | Intervention Description | Study Design | Duration | Sample | Age of Participants | Primary Outcome |
| Interventions with Couples | |||||||
| Hartmann et al. 2021 [39] | Interventions with couples | Study with 3 arms: control, 4 weekly cognitive behavioral counseling sessions with couples, and 4 weekly cognitive behavioral counseling sessions with couples plus incentive to not drink | 3-arm randomized controlled trial | 1 month | 60 couples from a large city, 20 per arm | Men 27–52 and women 18–42 years of age | Female-reported IPV victimization and breath alcohol concentration among participants (both partners) |
| Kalokhe et al. 2021 [41] | Interventions with couples | Assign peer educators to groups of 3–5 couples to address relationship quality, resilience, communication, conflict negotiation, self-esteem, sexual health and communication, and norms around IPV. | Quasi-experimental | 6 weeks | 40 newly married couples residing in slum communities surrounding a major city, 20 per arm | Men averaging 26.4 and women averaging 21.6 years of age | Female-reported IPV victimization (psychological abuse); female mental health |
| Interventions with Women | |||||||
| Cottler et al. 2010 [38] | Interventions with women | Women’s groups—Body Wise Intervention—focused on sexual health and behavior | Pre/post evaluation | 2 months | 100 married women whose husbands reported heavy drinking during a community-wide household survey | 18–50 years of age | Female-reported IPV victimization (emotional, sexual, and physical abuse) |
| Neider et al. 2022 [43] | Interventions with women | Classroom-based training | Quasi- experimental | 10 h of training over 5 weeks | 254 female university students | 17–22 years of age | Female-reported sexual victimization; knowledge and attitudes of gender, healthy relationships and communication, sexual health, and bystander intention |
| Saggurti et al. 2014 [45] | Interventions with women | Intervention including 4 individual sessions and 2 women’s groups sessions; problem solving sessions with a counselor | 2-arm cluster randomized controlled trial | 6–9 weeks | 220 married women from a low-income community with a history of IPV or male partner heavy drinking | 18–40 years of age | Female-reported IPV victimization (physical and sexual abuse); marital conflict; and marital sexual coercion |
| Multi-Level Interventions | |||||||
| Balaji et al. 2011 [37] | Multi-level intervention (women, men, sex workers, and youth groups) | Peer educators conduct group sessions; street plays; teacher training program; and a health information campaign at household and community levels | Quasi-experimental | 18-month-long intervention | Young adults in 2 urban and 2 rural communities in a state | Young adults 16–24 years of age | Male- and female-reported IPV victimization (physical and sexual abuse), depression, and substance use |
| Javalkar et al. 2019 [40] | Multi-level intervention (women, men, sex workers, and youth groups) | Sex worker group meetings; peer educator counseling with sex workers; village plays; training of male champions; couples events for sex workers and their IP’s; and a crisis management team | Cluster randomized controlled trial | 27 months | 547 sex workers from 47 villages in 1 district | Women averaging 34.5 years of age | Female-reported IPV victimization (physical and sexual abuse), acceptance of IPV |
| Nair et al. 2020 [42] | Multi-level intervention (women, men, and youth groups) | Community mobilization through participatory learning and action—meetings with women’s groups followed by community gatherings | Pre/post evaluation | 16 months | 679 women at baseline and 861 women at endline from 39 women’s groups across 22 villages in one district | Age range of women not provided | Female-reported IPV victimization (emotional violence from husbands) |
| Reza-Paul et al. 2012 [44] | Multi-level intervention (women, men, sex workers, and youth groups) | Sex worker-led structural intervention to address root causes of violence against sex workers at the community level: addressed isolation, access to health services, intimidation, harassment, extortion, and rape from men and police, and assault by boyfriends; set up safe spaces, rapid violence response, improved workplace security, increased access to health care/condoms/STI testing, and increased community acceptance | Time-series and incident monitoring | 5 years | Sex workers in one community | 18 years or older; age range not provided | Female-reported IPV victimization (physical, sexual, emotional/psychological, and verbal) by boyfriends, clients, police, pimps/agents |
| Schensul et al. 2010 [46] | Multi-level intervention (men and community) | Men’s group meetings with referrals for individual counseling; community-wide health information campaign (street dramas, poster and banner presentations, film showings, and distribution of health communication materials) | Quasi- experimental | 3 years | Married men from three communities outside a major Indian city that are daily wage workers, petty traders, and small business owners | 21–40 years of age | Male-reported perpetration of violence (physical and verbal) towards spouse; drinking behavior, gender equity attitudes, and extramarital sex |
| Outcome Variable | k | OR | 95% CI | Fail-Safe n |
|---|---|---|---|---|
| IPV Victimization (all types) | 8 | 0.61 *** | [0.48, 0.79] | 151 |
| Physical IPV Victimization | 2 | 0.50 ** | [0.31, 0.80] | -- |
| Psychological IPV Victimization | 2 | 0.42 ** | [0.24, 0.75] | -- |
| Sexual IPV Victimization | 3 | 0.58 | [0.27, 1.25] | -- |
| Approval of IPV | 2 | 0.63 ** | [0.44, 0.89] | -- |
| Intervention Type | Statistically Significant Reduction in Any Type of IPV—Physical, Sexual, Emotional, Verbal? | Reduction in Other IPV-Related Outcomes? | Notable Effects Reported |
|---|---|---|---|
| Couples | Yes, 1 of 2 [39] | Yes, 2 of 2 | Statistically significant 10-point drop in violence score among couples experiencing IPV [39]; improvement in female participant mental health in 4–6-week intervention [41]. |
| Women’s | Yes, 1 of 3 [38] | Yes, 3 of 3 | Significant reduction in marital conflict and sexual coercion in 6–9-week intervention with an individual plus group component [45]. |
| Multi-Level | Yes, 3 of 5 [37,42,44] | Yes, 5 of 5 | Odds of experiencing emotional and physical violence by family other than husband decreased by more than 45% [42]); significant decrease in sexual abuse [72.2% (urban)] and depression [60% (rural) and 38.8% (urban)] among participants 16–24 years of age. [37]. |
| Key Findings |
|---|
|
|
|
|
|
| Future Research Questions |
|---|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mittal, M.; Paden McCormick, A.; Palit, M.; Trabold, N.; Spencer, C. A Meta-Analysis and Systematic Review of Community-Based Intimate Partner Violence Interventions in India. Int. J. Environ. Res. Public Health 2023, 20, 5277. https://doi.org/10.3390/ijerph20075277
Mittal M, Paden McCormick A, Palit M, Trabold N, Spencer C. A Meta-Analysis and Systematic Review of Community-Based Intimate Partner Violence Interventions in India. International Journal of Environmental Research and Public Health. 2023; 20(7):5277. https://doi.org/10.3390/ijerph20075277
Chicago/Turabian StyleMittal, Mona, Anna Paden McCormick, Manjushree Palit, Nicole Trabold, and Chelsea Spencer. 2023. "A Meta-Analysis and Systematic Review of Community-Based Intimate Partner Violence Interventions in India" International Journal of Environmental Research and Public Health 20, no. 7: 5277. https://doi.org/10.3390/ijerph20075277
APA StyleMittal, M., Paden McCormick, A., Palit, M., Trabold, N., & Spencer, C. (2023). A Meta-Analysis and Systematic Review of Community-Based Intimate Partner Violence Interventions in India. International Journal of Environmental Research and Public Health, 20(7), 5277. https://doi.org/10.3390/ijerph20075277






