The Contribution of Environmental Science to Mental Health Research: A Scoping Review
Abstract
1. Introduction
2. Review Aim, Objectives and Research Questions (Step 1)
- What is the current contribution of environmental science to mental health research? This includes consideration of the pathways by which the environment impacts mental health and wellbeing, including conditions of cognitive development and decline, and how environmental science has been leveraged to understand these pathways or impacts;
- What are the current research designs and methodological approaches being used in environmental science and mental health research?
- How does the relationship between environmental science and mental health research relate to existing evidence linking mental health and wellbeing to demographic, social, economic, and genetic determinants?
- What are the evidence gaps and opportunities for the contribution of environmental science to mental health research?
3. Methods
3.1. Overview
3.2. Identification of Relevant Studies (Step 2)
3.2.1. Protocol
3.2.2. Inclusion/Exclusion Criteria
3.2.3. Information Sources and Search Strategy
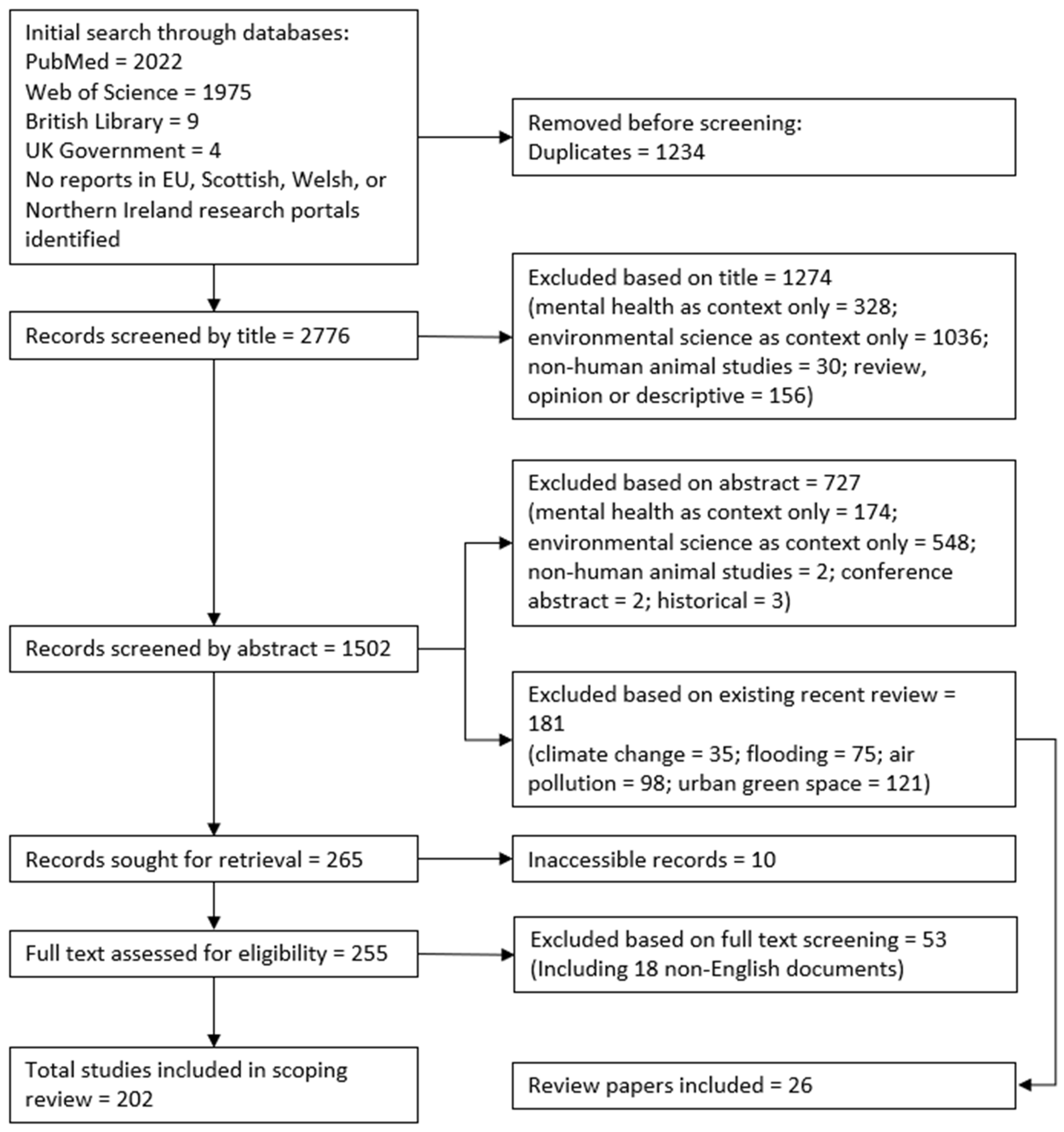
3.3. Study Selection (Step 3)
Review Papers
3.4. Data Charting and Synthesis (Step 4)
Reviews
4. Results (Step 5) Including Expert Consultations (Step 6)
4.1. Search Results
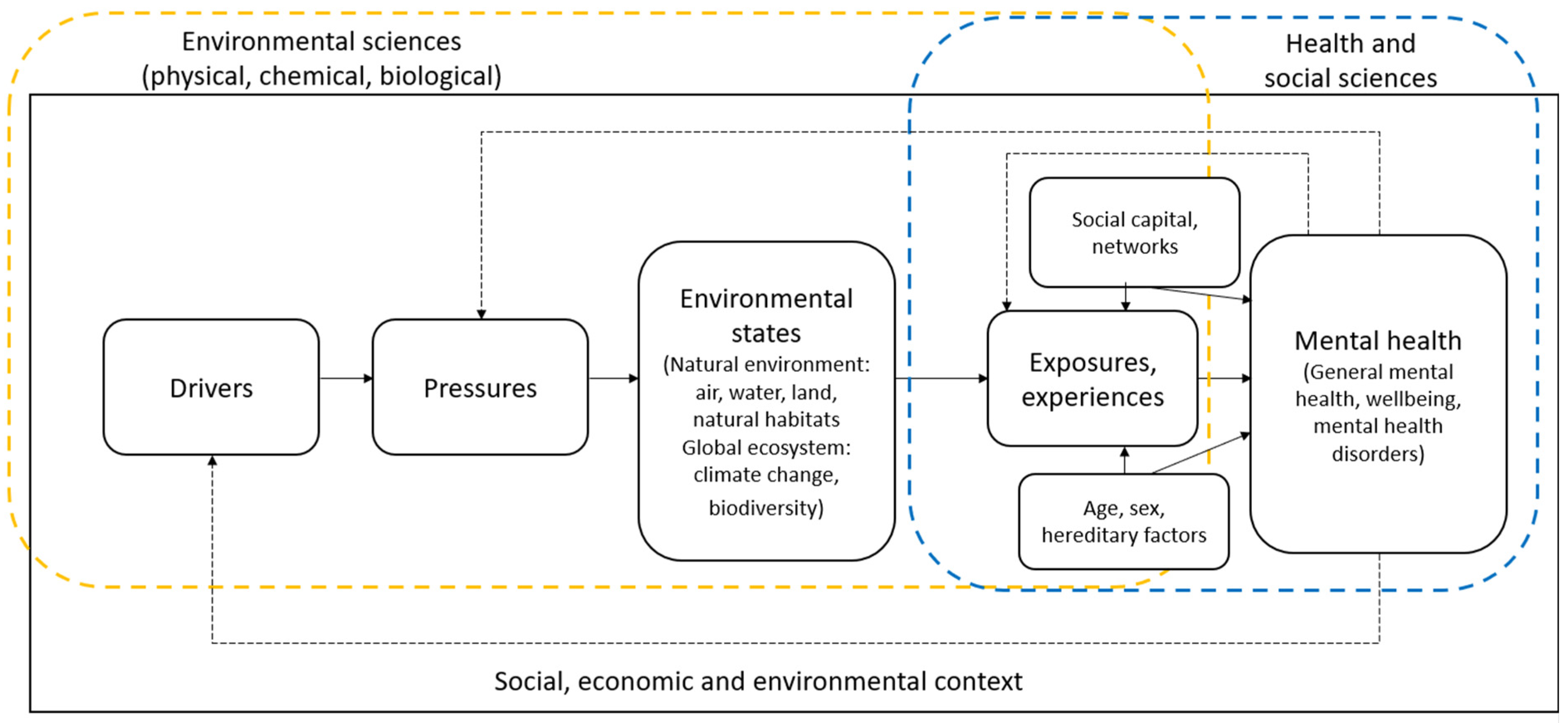
4.2. What Is the Current Contribution of Environmental Science to Mental Health Research?
4.2.1. Evidence from Reviews (Climate Change, Flooding, Air Pollution, Urban Green Space)
4.3. What Are the Current Research Designs and Methodological Approaches Being Used in Environmental Science-Mental Health Research?
- Noise monitoring was carried out using static noise monitors at the neighbourhood scale [69,71,72,73,74,78,110,111,112,113], recording peak and off-peak noise at varied locations to map noise across the study sites. Participants in one study carried portable noise sensors, enabling an individual noise map to be created [42].
- Pollutant studies used standard procedures, including for water [114,115,116], air [117], and chemical pollutants (e.g., arsenic, nitrate, uranium). Similar methods were used to measure oil spill characteristics to quantify the extent of exposure, including hazardous material, volume, surface area of the spill, magnitude, and dispersant volume [118]. Only studies of chemical pollutants used biomarkers indicative of exposure level, analysing parent compounds and their metabolites in hair and urine, to provide an estimate of the biological dose [53,114,119,120,121,122].
4.3.1. Evidence from Reviews (Climate Change, Flooding, Air Pollution, Urban Green Space)
4.4. How Does the Relationship between Environmental Science and Mental Health Research Relate to Existing Evidence Linking Mental Health and Wellbeing to Demographic, Social, Economic, and Genetic Determinants?
4.4.1. Evidence from Review Studies (Climate Change, Flooding, Air Pollution, Urban Green Space)
5. Discussion
5.1. What Is the Current Contribution of Environmental Science to Mental Health Research?
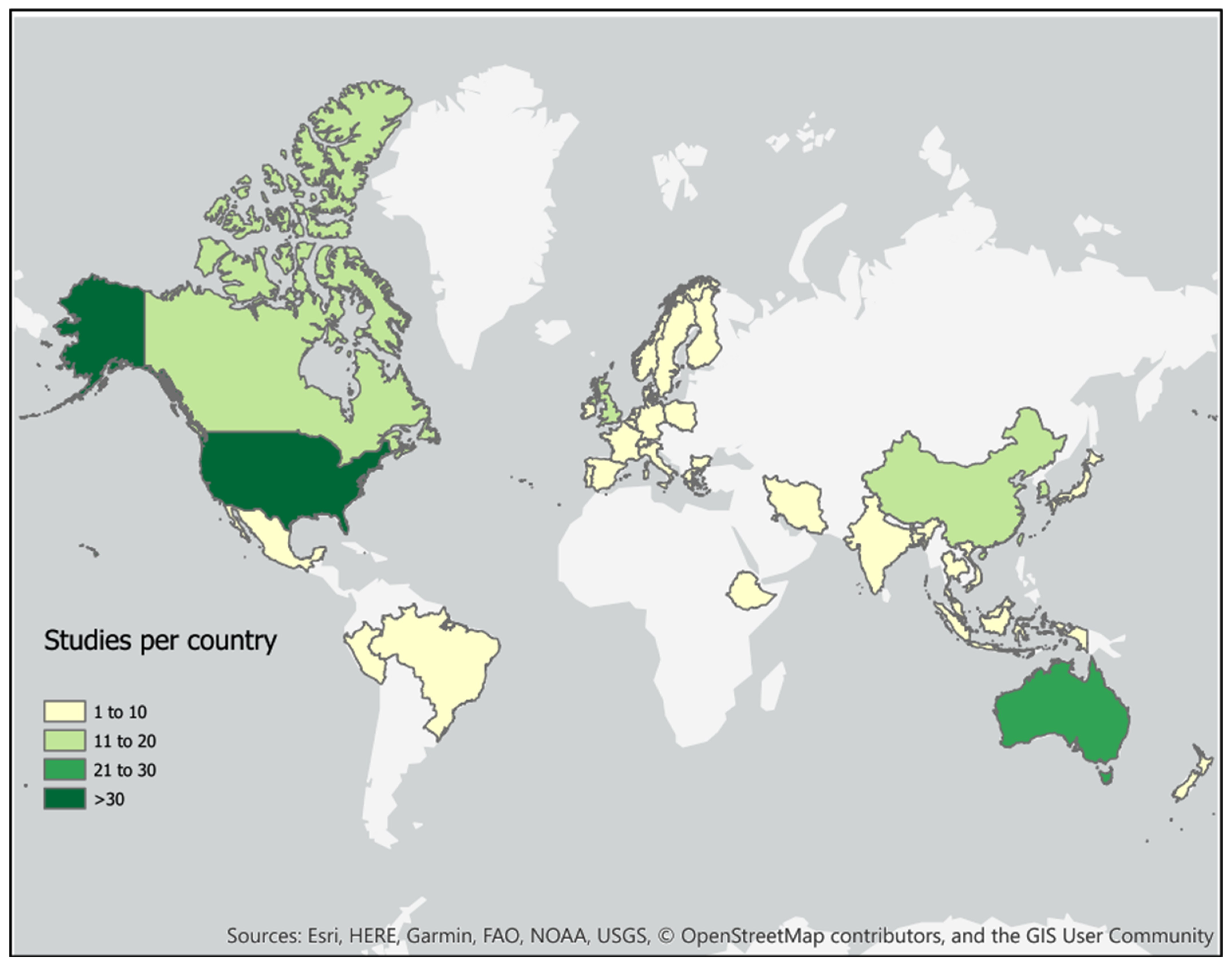
5.1.1. Future Research Focus: Expand Geographical Scope
5.1.2. Future Research Focus: Increase Range of Environmental Science Areas
5.2. What Are the Current Research Designs and Methodological Approaches Being Used in Environmental Science-Mental Health Research?
5.2.1. Future Research Focus: Greater Application of Experimental Research Design Principles
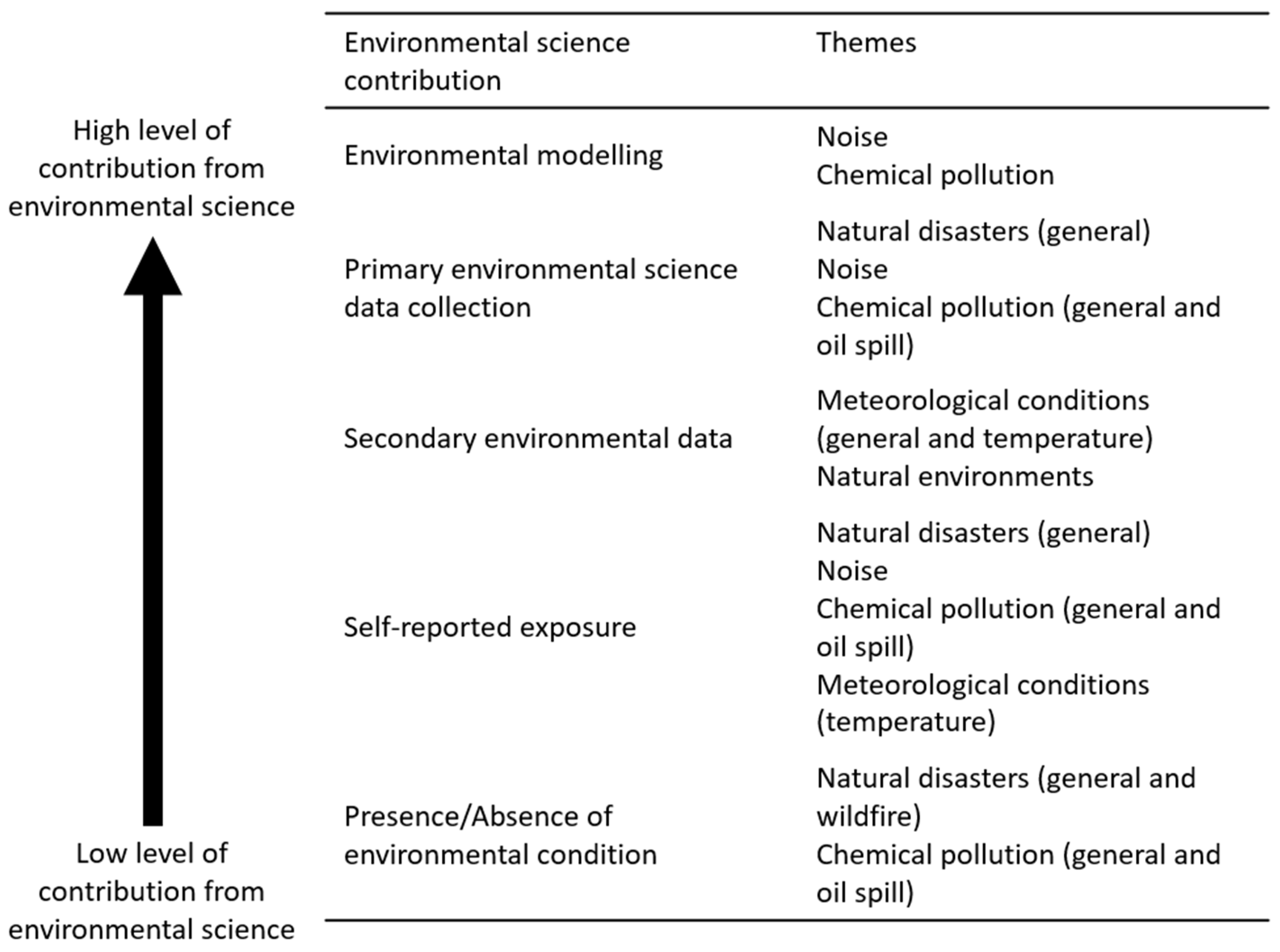
5.2.2. Future Research Focus: Draw on Environmental Science to Include Better Measures of Exposure
5.2.3. Future Research Focus: Inclusion and Development of Mixed and Qualitative Methods
5.2.4. Future Research Focus: Longitudinal Analysis
5.3. How Does the Relationship between Environmental Science and Mental Health Research Relate to Existing Evidence Linking Mental Health and Wellbeing to Demographic, Social, Economic, and Genetic Determinants?
5.3.1. Future Research Focus: Integration of Multiple Conceptual Models
5.3.2. Future Research Focus: Consideration of Socio-Economic (Political) Systems
5.4. What Are the Evidence Gaps and Opportunities for the Contribution of Environmental Science to Mental Health Research?
5.4.1. Future Research Focus: Considering ‘Good’ Mental Health
5.4.2. Future Research Focus: Exploring Variation between and within Communities
5.4.3. Future Research Focus: Review of Mediating Pathways
6. Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bache, I.; Reardon, L.; Anand, P. Wellbeing as a Wicked Problem: Navigating the Arguments for the Role of Government. J. Happiness Stud. 2015, 17, 893–912. [Google Scholar] [CrossRef]
- Rehm, J.; Shield, K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019, 21, 10. [Google Scholar] [CrossRef]
- World Health Organization. Green and Blue Spaces and Mental Health: New Evidence and Perspectives for Action. Copenhagen, WHO Regional Office for Europe. 2021. Available online: https://www.euro.who.int/en/publications/abstracts/green-and-blue-spaces-and-mental-health-new-evidence-and-perspectives-for-action-2021 (accessed on 27 July 2021).
- Jain, M.; Sharma, G.D.; Mahendru, M. Can I Sustain My Happiness? A Review, Critique and Research Agenda for Economics of Happiness. Sustainability 2019, 11, 6375. [Google Scholar] [CrossRef]
- Collins, P.Y.; Patel, V.; Joestl, S.S.; March, D.; Insel, T.R.; Daar, A.S.; Bordin, I.A.; Costello, E.J.; Durkin, M.; Fairburn, C.G.; et al. Grand challenges in global mental health. Nature 2011, 475, 27–30. [Google Scholar] [CrossRef]
- Patel, V.; Saxena, S.; Lund, C.; Thornicroft, G.; Baingana, F.; Bolton, P.; Chisholm, D.; Collins, P.Y.; Cooper, J.L.; Eaton, J.; et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018, 392, 1553–1598. [Google Scholar] [CrossRef]
- Massazza, A.; Teyton, A.; Charlson, F.; Benmarhnia, T.; Augustinavicius, J.L. Quantitative methods for climate change and mental health research: Current trends and future directions. Lancet Planet. Health 2022, 6, e613–e627. [Google Scholar] [CrossRef]
- Hayes, K.; Poland, B. Addressing Mental Health in a Changing Climate: Incorporating Mental Health Indicators into Climate Change and Health Vulnerability and Adaptation Assessments. Int. J. Environ. Res. Public Health 2018, 15, 1806. [Google Scholar] [CrossRef]
- Veenema, T.; Thornton, C.; Lavin, R.P.; Bender, A.K.; Seal, S.; Corley, A. Climate Change-Related Water Disasters’ Impact on Population Health. J. Nurs. Sch. 2017, 49, 625–634. [Google Scholar] [CrossRef]
- Braithwaite, I.; Zhang, S.; Kirkbride, J.B.; Osborn, D.P.; Hayes, J.F. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: A systematic review and meta-analysis. Environ. Health Perspect. 2019, 127, 126002. [Google Scholar] [CrossRef]
- Collins, R.M.; Spake, R.; Brown, K.A.; Ogutu, B.O.; Smith, D.; Eigenbrod, F. A systematic map of research exploring the effect of greenspace on mental health. Landsc. Urban Plan. 2020, 201, 103823. [Google Scholar] [CrossRef]
- Kabisch, N. The Influence of socio-economic and socio-demographic factors in the association between urban green space and health. In Biodiversity and Health in the Face of Climate Change; Marselle, M., Stadler, J., Korn, H., Irvine, K., Bonn, A., Eds.; Springer: Cham, Germany, 2019; pp. 91–119. [Google Scholar] [CrossRef]
- Kondo, M.C.; Fluehr, J.M.; McKeon, T.; Branas, C.C. Urban Green Space and Its Impact on Human Health. Int. J. Environ. Res. Public Health 2018, 15, 445. [Google Scholar] [CrossRef] [PubMed]
- Marselle, M.R.; Hartig, T.; Cox, D.T.; de Bell, S.; Knapp, S.; Lindley, S.; Triguero-Mas, M.; Böhning-Gaese, K.; Braubach, M.; Cook, P.A.; et al. Pathways linking biodiversity to human health: A conceptual framework. Environ. Int. 2021, 150, 106420. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, S.; Davinson, N. The impact of nature-based interventions on public health: A review using pathways, mechanisms and behaviour change techniques from environmental social science and health behaviour change. J. Br. Acad. 2021, 9, 33–61. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organization Constitution. In Proceedings of the International Health Conference, New York, NY, USA, 19–22 July 1946.
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Personal. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. On Happiness and Human Potentials: A Review of Research on Hedonic and Eudaimonic Well-Being. Annu. Rev. Psychol. 2001, 52, 141–166. [Google Scholar] [CrossRef]
- Keyes, C.L.M.; Annas, J. Feeling good and functioning well: Distinctive concepts in ancient philosophy and contemporary science. J. Posit. Psychol. 2009, 4, 197–201. [Google Scholar] [CrossRef]
- Dasgupta, P.; Weale, M. On measuring the quality of life. World Dev. 1992, 20, 119–131. [Google Scholar] [CrossRef]
- Kim-Prieto, C.; Diener, E.; Tamir, M.; Scollon, C.; Diener, M. Integrating The Diverse Definitions of Happiness: A Time-Sequential Framework of Subjective Well-Being. J. Happiness Stud. 2005, 6, 261–300. [Google Scholar] [CrossRef]
- Natural Environment Research Council. 2021. Available online: https://nerc.ukri.org/research (accessed on 27 July 2021).
- Engel, G.L. The Need for a New Medical Model: A Challenge for Biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Futures Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Barton, H.; Grant, M. A health map for the local human habitat. Perspect. Public Health 2006, 126, 252–253. [Google Scholar] [CrossRef]
- Pineo, H. Towards healthy urbanism: Inclusive, equitable and sustainable (THRIVES)—An urban design and planning framework from theory to praxis. Cities Health 2020, 6, 974–992. [Google Scholar] [CrossRef]
- Corvalán, C.; Briggs, D.J.; Kjellstrom, T. Development of environmental health indicators. In Linkage Methods for Environment and Health Analysis: General Guidelines; Briggs, D., Corvalán, C., Nurminen, M., Eds.; UNEP, USEPA and WHO: Geneva, Switzerland, 1996. [Google Scholar]
- Morris, G.P.; Beck, S.A.; Hanlon, P.; Robertson, R. Getting strategic about the environment and health. Public Health 2006, 120, 889–903. [Google Scholar] [CrossRef] [PubMed]
- Reis, S.; Morris, G.; Fleming, L.E.; Beck, S.; Taylor, T.; White, M.; Depledge, M.H.; Steinle, S.; Sabel, C.E.; Cowie, H.; et al. Integrating health and environmental impact analysis. Public Health 2015, 129, 1383–1389. [Google Scholar] [CrossRef]
- Garrity, C.; Stevens, A.; Gartlehner, G.; King, V.; Kamel, C. Cochrane Rapid Review Methods Group to play a leading role in guiding the production of informed high-quality, timely research evidence syntheses. Syst. Rev. 2016, 5, 184. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Dias, M.; Tufanaru, C.; Porritt, K.; Stern, C.; Jordan, Z.; Aromataris, E.; Pearson, A. The “quality” of JBI qualitative research synthesis: A methodological investigation into the adherence of meta-aggregative systematic reviews to reporting standards and methodological guidance. JBI Evid. Synth. 2021, 19, 1119–1139. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Westphaln, K.; Regoeczi, W.; Masotya, M.; Vasquez-Westphaln, B.; Lounsbury, K.; McDavid, L.; Lee, H.; Johnson, J.; Ronis, S. From Arskey and O’Malley and Beyond: Customizations to enhance a team-based, mixed method approach to scoping review methodology. Methods X 2021, 8, 101375. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Huutoniemi, K.; Klein, J.T.; Bruun, H.; Hukkinen, J. Analyzing interdisciplinarity: Typology and indicators. Res. Policy 2010, 39, 79–88. [Google Scholar] [CrossRef]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 5th ed.; 10th revision; World Health Organization: Geneva, Switzerland, 2015; Available online: https://icd.who.int/browse10/2019/en#/V (accessed on 27 July 2021).
- Staupe-Delgado, R. Progress, traditions and future directions in research on disasters involving slow-onset hazards. Disaster Prev. Manag. 2019, 28, 623–635. [Google Scholar] [CrossRef]
- Ma, J.; Li, C.; Kwan, M.-P.; Kou, L.; Chai, Y. Assessing personal noise exposure and its relationship with mental health in Beijing based on individuals’ space-time behavior. Environ. Int. 2020, 139, 105737. [Google Scholar] [CrossRef]
- Dreger, S.; Meyer, N.; Fromme, H.; Bolte, G. Environmental noise and incident mental health problems: A prospective cohort study among school children in Germany. Environ. Res. 2015, 143, 49–54. [Google Scholar] [CrossRef]
- Hammersen, F.; Niemann, H.; Hoebel, J. Environmental Noise Annoyance and Mental Health in Adults: Findings from the Cross-Sectional German Health Update (GEDA) Study 2012. Int. J. Environ. Res. Public Health 2016, 13, 954. [Google Scholar] [CrossRef]
- Jensen, H.A.R.; Rasmussen, B.; Ekholm, O. Neighbour and traffic noise annoyance: A nationwide study of associated mental health and perceived stress. Eur. J. Public Health 2018, 28, 1050–1055. [Google Scholar] [CrossRef]
- Nitschke, M.; Tucker, G.; Simon, D.L.; Hansen, A.L.; Pisaniello, D.L. The link between noise perception and quality of life in South Australia. Noise Health 2014, 16, 137–142. [Google Scholar] [CrossRef]
- Beutel, M.E.; Jünger, C.; Klein, E.M.; Wild, P.; Lackner, K.; Blettner, M.; Binder, H.; Michal, M.; Wiltink, J.; Brähler, E.; et al. Noise annoyance is associated with depression and anxiety in the general population-the contribution of aircraft noise. PLoS ONE 2016, 11, e0155357. [Google Scholar] [CrossRef]
- Beutel, M.E.; Brähler, E.; Ernst, M.; Klein, E.; Reiner, I.; Wiltink, J.; Michal, M.; Wild, P.S.; Schulz, A.; Münzel, T.; et al. Noise annoyance predicts symptoms of depression, anxiety and sleep disturbance 5 years later. Findings from the Gutenberg Health Study. Eur. J. Public Health 2020, 30, 516–521. [Google Scholar] [CrossRef]
- Yoon, J.H.; Won, J.U.; Lee, W.; Jung, P.K.; Roh, J. Occupational noise annoyance linked to depressive symptoms and suicidal ideation: A result from nationwide survey of Korea. PLoS ONE 2014, 9, e105321. [Google Scholar] [CrossRef] [PubMed]
- Stough, L.M.; North, C.S. The association of adverse mental health effects with repeated exposure to disasters. Ann. Clin. Psychiatry 2018, 30, 17–24. [Google Scholar]
- Chen, J.; Chen, S.; Landry, P.F. Migration, environmental hazards, and health outcomes in China. Soc. Sci. Med. 2013, 80, 85–95. [Google Scholar] [CrossRef]
- Kruger, D.J.; Cupal, S.; Franzen, S.P.; Kodjebacheva, G.; Bailey, E.S.; Key, K.D.; Kaufman, M.M. Toxic trauma: Household water quality experiences predict posttraumatic stress disorder symptoms during the Flint, Michigan, water crisis. J. Community Psychol. 2017, 45, 957–962. [Google Scholar] [CrossRef]
- Gaspar, F.W.; Harley, K.G.; Kogut, K.; Chevrier, J.; Mora, A.M.; Sjödin, A.; Eskenazi, B. Prenatal DDT and DDE exposure and child IQ in the CHAMACOS cohort. Environ. Int. 2015, 85, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Ayer, L.; Engel, C.; Parker, A.; Seelam, R.; Ramchand, R. Behavioral health of Gulf Coast residents 6 years after the Deepwater Horizon Oil Spill: The role of trauma history. Disaster Med. Public Health Prep. 2019, 13, 497–503. [Google Scholar] [CrossRef]
- Rung, A.L.; Gaston, S.; Oral, E.; Robinson, W.T.; Fontham, E.; Harrington, D.J.; Trapido, E.; Peters, E.S. Depression, Mental Distress, and Domestic Conflict among Louisiana Women Exposed to the Deepwater Horizon Oil Spill in the WaTCH Study. Environ. Health Perspect. 2016, 124, 1429–1435. [Google Scholar] [CrossRef]
- Johnson, E.J.; Boodram, C.-A.S. Health, well-being and quality of life of community members displaced after an industrial disaster in Trinidad. J. Public Health 2016, 25, 69–74. [Google Scholar] [CrossRef]
- Aiena, B.J.; Buchanan, E.M.; Smith, C.V.; Schulenberg, S.E. Meaning, resilience, and traumatic stress after the Deepwater Horizon oil spill: A study of Mississippi coastal residents seeking mental health services. J. Clin. Psychol. 2016, 72, 1264–1278. [Google Scholar] [CrossRef]
- Tawatsupa, B.; Yiengprugsawan, V.; Kjellstrom, T.; Seubsman, S.A.; Sleigh, A.; Thai Cohort Study Team. Heat stress, health and well-being: Findings from a large national cohort of Thai adults. BMJ Open 2012, 2, 001396. [Google Scholar] [CrossRef] [PubMed]
- Beecher, M.E.; Eggett, D.; Erekson, D.; Rees, L.B.; Bingham, J.; Klundt, J.; Bailey, R.J.; Ripplinger, C.; Kirchhoefer, J.; Gibson, R.; et al. Sunshine on my shoulders: Weather, pollution, and emotional distress. J. Affect. Disord. 2016, 205, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.Y.; Lam, H.C.Y.; So, S.H.W.; Goggins, W.B.; Ho, J.Y.; Liu, S.; Chung, P.P.W. Association between Ambient Temperatures and Mental Disorder Hospitalizations in a Subtropical City: A Time-Series Study of Hong Kong Special Administrative Region. Int. J. Environ. Res. Public Health 2018, 15, 754. [Google Scholar] [CrossRef]
- Ha, H.; Shao, W. A spatial epidemiology case study of mentally unhealthy days (MUDs): Air pollution, community resilience, and sunlight perspectives. Int. J. Environ. Health Res. 2019, 31, 491–506. [Google Scholar] [CrossRef]
- Alcock, I.; White, M.; Lovell, R.; Higgins, S.; Osborne, N.; Husk, K.; Wheeler, B. What accounts for ‘England’s green and pleasant land’? A panel data analysis of mental health and land cover types in rural England. Landsc. Urban Plan. 2015, 142, 38–46. [Google Scholar] [CrossRef]
- Garrett, J.K.; Clitherow, T.J.; White, M.P.; Wheeler, B.W.; Fleming, L.E. Coastal proximity and mental health among urban adults in England: The moderating effect of household income. Health Place 2019, 59, 102200. [Google Scholar] [CrossRef]
- White, M.P.; Alcock, I.; Wheeler, B.W.; Depledge, M.H. Coastal proximity, health and well-being: Results from a longitudinal panel survey. Health Place 2013, 23, 97–103. [Google Scholar] [CrossRef]
- Friel, S.; Berry, H.; Dinh, H.; O’Brien, L.; Walls, H.L. The impact of drought on the association between food security and mental health in a nationally representative Australian sample. BMC Public Health 2014, 14, 1102. [Google Scholar] [CrossRef]
- Hanigan, I.C.; Schirmer, J.; Niyonsenga, T. Drought and Distress in Southeastern Australia. EcoHealth 2018, 15, 642–655. [Google Scholar] [CrossRef]
- O’Brien, L.; Berry, H.; Coleman, C.; Hanigan, I. Drought as a mental health exposure. Environ. Res. 2014, 131, 181–187. [Google Scholar] [CrossRef]
- Yazd, S.D.; Wheeler, S.A.; Zuo, A. Understanding the impacts of water scarcity and socio-economic demographics on farmer mental health in the Murray-Darling Basin. Ecol. Econ. 2020, 169, 106564. [Google Scholar] [CrossRef]
- Al-Mutairi, N.Z.; Al-Attar, M.A.; Al-Rukaibi, F.S. Traffic-generated noise pollution: Exposure of road users and populations in Metropolitan Kuwait. Environ. Monit. Assess. 2011, 183, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Crombie, R.; Clark, C.; Stansfeld, S.A. Environmental noise exposure, early biological risk and mental health in nine to ten year old children: A cross-sectional field study. Environ. Health 2011, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Kageyama, T.; Yano, T.; Kuwano, S.; Sueoka, S.; Tachibana, H. Exposure-response relationship of wind turbine noise with self-reported symptoms of sleep and health problems: A nationwide socioacoustic survey in Japan. Noise Health 2016, 18, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Schreckenberg, D.; Griefahn, B.; Meis, M. The associations between noise sensitivity, reported physical and mental health, perceived environmental quality, and noise annoyance. Noise Health 2010, 12, 7–16. [Google Scholar] [CrossRef]
- Sygna, K.; Aasvang, G.M.; Aamodt, G.; Oftedal, B.; Krog, N.H. Road traffic noise, sleep and mental health. Environ. Res. 2014, 131, 17–24. [Google Scholar] [CrossRef]
- Wright, D.M.; Newell, K.; Maguire, A.; O’Reilly, D. Aircraft noise and self-assessed mental health around a regional urban airport: A population based record linkage study. Environ. Health 2018, 17, 74. [Google Scholar] [CrossRef]
- Stickley, A.; Ng, C.F.S.; Konishi, S.; Koyanagi, A.; Watanabe, C. Airborne pollen and suicide mortality in Tokyo, 2001–2011. Environ. Res. 2017, 155, 134–140. [Google Scholar] [CrossRef]
- Eze, I.C.; Foraster, M.; Schaffner, E.; Vienneau, D.; Pieren, R.; Imboden, M.; Wunderli, J.-M.; Cajochen, C.; Brink, M.; Röösli, M.; et al. Incidence of depression in relation to transportation noise exposure and noise annoyance in the SAPALDIA study. Environ. Int. 2020, 144, 106014. [Google Scholar] [CrossRef]
- Generaal, E.; Hoogendijk, E.O.; Stam, M.; Henke, C.E.; Rutters, F.; Oosterman, M.; Huisman, M.; Kramer, S.E.; Elders, P.J.M.; Timmermans, E.J.; et al. Neighbourhood characteristics and prevalence and severity of depression: Pooled analysis of eight Dutch cohort studies. Br. J. Psychiatry 2019, 215, 468–475. [Google Scholar] [CrossRef]
- He, S.; Smargiassi, A.; Low, N.; Bilodeau-Bertrand, M.; Ayoub, A.; Auger, N. Residential noise exposure and the longitudinal risk of hospitalization for depression after pregnancy: Postpartum and beyond. Environ. Res. 2019, 170, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Hill, E.; Billington, R.; Krageloh, C. Noise sensitivity and diminished health: Testing moderators and mediators of the relationship. Noise Health 2014, 16, 47. [Google Scholar] [CrossRef] [PubMed]
- Okokon, E.O.; Yli-Tuomi, T.; Turunen, A.W.; Tiittanen, P.; Juutilainen, J.; Lanki, T. Traffic noise, noise annoyance and psychotropic medication use. Environ. Int. 2018, 119, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Aschengrau, A.; Janulewicz, P.A.; White, R.F.; Vieira, V.M.; Gallagher, L.; Getz, K.; Webster, T.F.; Ozonoff, D. Long-term Neurotoxic Effects of Early-life Exposure to Tetrachloroethylene-contaminated Drinking Water. Ann. Glob. Health 2016, 82, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Gauvain, M.; Richert, R. Cognitive Development. In Encyclopaedia of Mental Health, 2nd ed.; Friedman, H.S., Ed.; Academic Press: Cambridge, MA, USA, 2015. [Google Scholar]
- Berry, H.L.; Hogan, A.; Owen, J.; Rickwood, D.; Fragar, L. Climate Change and Farmers’ Mental Health: Risks and Responses. Asia Pac. J. Public Health 2011, 23, 119S–132S. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.Y.; Ho, J.Y.; Hung, H.H.Y.; Liu, S.; Lam, H.C.Y. Health impact of climate change in cities of middle-income countries: The case of China. Br. Med. Bull. 2019, 130, 5–24. [Google Scholar] [CrossRef]
- van den Bosch, M.; Meyer-Lindenberg, A. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence. Annu. Rev. Public Health 2019, 40, 239–259. [Google Scholar] [CrossRef]
- Hayes, K.; Berry, P.; Ebi, K.L. Factors Influencing the Mental Health Consequences of Climate Change in Canada. Int. J. Environ. Res. Public Health 2019, 16, 1583. [Google Scholar] [CrossRef]
- Kinay, P.; Morse, A.P.; Villanueva, E.V.; Morrissey, K.; Staddon, P.L. Direct and indirect health impacts of climate change on the vulnerable elderly population in East China. Environ. Rev. 2019, 27, 295–303. [Google Scholar] [CrossRef]
- Jaakkola, J.J.K.; Juntunen, S.; Näkkäläjärvi, K. The Holistic Effects of Climate Change on the Culture, Well-Being, and Health of the Saami, the Only Indigenous People in the European Union. Curr. Environ. Health Rep. 2018, 5, 401–417. [Google Scholar] [CrossRef] [PubMed]
- Patz, J.A.; Frumkin, H.; Holloway, T.; Vimont, D.J.; Haines, A. Climate change: Challenges and opportunities for global health. JAMA 2014, 312, 1565–1580. [Google Scholar] [CrossRef] [PubMed]
- Dannenberg, A.L.; Frumkin, H.; Hess, J.J.; Ebi, K.L. Managed retreat as a strategy for climate change adaptation in small communities: Public health implications. Clim. Chang. 2019, 153, 1–14. [Google Scholar] [CrossRef]
- Yusa, A.; Berry, P.; Cheng, J.J.; Ogden, N.; Bonsal, B.; Stewart, R.; Waldick, R. Climate Change, Drought and Human Health in Canada. Int. J. Environ. Res. Public Health 2015, 12, 8359–8412. [Google Scholar] [CrossRef]
- Garcia, D.M.; Sheehan, M.C. Extreme Weather-driven Disasters and Children’s Health. Int. J. Health Serv. 2015, 46, 79–105. [Google Scholar] [CrossRef]
- Burton, H.; Rabito, F.; Danielson, L.; Takaro, T.K. Health effects of flooding in Canada: A 2015 review and description of gaps in research. Can. Water Resour. J. Rev. Can. Des Ressour. Hydr. 2015, 41, 238–249. [Google Scholar] [CrossRef]
- Du, W.; FitzGerald, G.J.; Clark, M.; Hou, X.-Y. Health Impacts of Floods. Prehospital Disaster Med. 2010, 25, 265–272. [Google Scholar] [CrossRef]
- Mousavi, A.; Ardalan, A.; Takian, A.; Ostadtaghizadeh, A.; Naddafi, K.; Bavani, A.M. Climate change and health in Iran: A narrative review. J. Environ. Health Sci. Eng. 2020, 18, 367–378. [Google Scholar] [CrossRef]
- Schulte, P.; Bhattacharya, A.; Butler, C.; Chun, H.; Jacklitsch, B.; Jacobs, T.; Kiefer, M.; Lincoln, J.; Pendergrass, S.; Shire, J.; et al. Advancing the framework for considering the effects of climate change on worker safety and health. J. Occup. Environ. Hyg. 2016, 13, 847–865. [Google Scholar] [CrossRef]
- Verner, G.; Schütte, S.; Knop, J.; Sankoh, O.; Sauerborn, R. Health in climate change research from 1990 to 2014: Positive trend, but still underperforming. Glob. Health Action 2016, 9, 30723. [Google Scholar] [CrossRef]
- Stanke, C.; Murray, V.; Amlôt, R.; Nurse, J.; Williams, R. The effects of flooding on mental health: Outcomes and recommendations from a review of the literature. PLoS Curr. 2012, 4, e4f9f1fa9c3cae. [Google Scholar] [CrossRef] [PubMed]
- Tzivian, L.; Winkler, A.; Dlugaj, M.; Schikowski, T.; Vossoughi, M.; Fuks, K.; Weinmayr, G.; Hoffmann, B. Effect of long-term outdoor air pollution and noise on cognitive and psychological functions in adults. Int. J. Hyg. Environ. Health 2015, 218, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bos, I.; De Boever, P.; Panis, L.I.; Meeusen, R. Physical Activity, Air Pollution and the Brain. Sport. Med. 2014, 44, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, G.; Danti, S.; Carlesi, C.; Borin, G. Danger in the Air: Air Pollution and Cognitive Dysfunction. Am. J. Alzheimer’s Dis. Other Dement. 2018, 33, 333–341. [Google Scholar] [CrossRef]
- de Pardo Bert, P.; Mercader, E.M.H.; Pujol, J.; Sunyer, J.; Mortamais, M. The Effects of Air Pollution on the Brain: A Review of Studies Interfacing Environmental Epidemiology and Neuroimaging. Curr. Environ. Health Rep. 2018, 5, 351–364. [Google Scholar] [CrossRef]
- Buoli, M.; Grassi, S.; Caldiroli, A.; Carnevali, G.S.; Mucci, F.; Iodice, S.; Cantone, L.; Pergoli, L.; Bollati, V. Is there a link between air pollution and mental disorders? Environ. Int. 2018, 118, 154–168. [Google Scholar] [CrossRef]
- Gladkikh, T.M.; Gould, R.K.; Coleman, K.J. Cultural ecosystem services and the well-being of refugee communities. Ecosyst. Serv. 2019, 40, 101036. [Google Scholar] [CrossRef]
- Hankey, S.; Marshall, J.D. Urban Form, Air Pollution, and Health. Curr. Environ. Health Rep. 2017, 4, 491–503. [Google Scholar] [CrossRef]
- O’Brien, L. Carrying out Physical Activity as Part of the Active Forests Programme in England: What Encourages, Supports and Sustains Activity?—A Qualitative Study. Int. J. Environ. Res. Public Health 2019, 16, 5118. [Google Scholar] [CrossRef]
- Lee, H.J.; Son, Y.-H.; Kim, S.; Lee, D.K. Healing experiences of middle-aged women through an urban forest therapy program. Urban For. Urban Green. 2019, 38, 383–391. [Google Scholar] [CrossRef]
- Powers, J.R.; Dobson, A.J.; Berry, H.L.; Graves, A.M.; Hanigan, I.C.; Loxton, D. Lack of association between drought and mental health in a cohort of 45-61 year old rural Australian women. Aust. New Zealand J. Public Health 2015, 39, 518–523. [Google Scholar] [CrossRef]
- Yazd, S.D.; Wheeler, S.A.; Zuo, A. Exploring the drivers of irrigator mental health in the Murray–Darling Basin, Australia. Sustainability 2019, 11, 6097. [Google Scholar] [CrossRef]
- Dzhambov, A.; Tilov, B.; Markevych, I.; Dimitrova, D. Residential road traffic noise and general mental health in youth: The role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Environ. Int. 2017, 109, 1–9. [Google Scholar] [CrossRef]
- Dzhambov, A.M.; Markevych, I.; Tilov, B.; Arabadzhiev, Z.; Stoyanov, D.; Gatseva, P.; Dimitrova, D.D. Pathways linking residential noise and air pollution to mental ill-health in young adults. Environ. Res. 2018, 166, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Dzhambov, A.M.; Markevych, I.; Tilov, B.G.; Dimitrova, D.D. Residential greenspace might modify the effect of road traffic noise exposure on general mental health in students. Urban For. Urban Green. 2018, 34, 233–239. [Google Scholar] [CrossRef]
- Roswall, N.; Høgh, V.; Envold-Bidstrup, P.; Raaschou-Nielsen, O.; Ketzel, M.; Overvad, K.; Olsen, A.; Sørensen, M. Residential Exposure to Traffic Noise and Health-Related Quality of Life—A Population-Based Study. PLoS ONE 2015, 10, e0120199. [Google Scholar] [CrossRef] [PubMed]
- Norra, C.; Ngoc, D.T.M.; Trang, P.T.K.; Lan, V.T.M.; Viet, P.H.; Norra, S.; Kunert, H.J. Mental health burden and neuropsychiatric deficits of chronic arsenic exposure: First results of the Vietnamese field study. In Understanding the Geological and Medical Interface of Arsenic; Ng., J.C., Noller, B.N., Naidu, R., Bundschuh, J., Bhattacharya, P., Eds.; Taylor and Francis Group: London, UK, 2012; pp. 168–170. [Google Scholar]
- Manczak, E.M.; Miller, J.G.; Gotlib, I.H. Water contaminant levels interact with parenting environment to predict development of depressive symptoms in adolescents. Dev. Sci. 2020, 23, e12838. [Google Scholar] [CrossRef]
- Akter, S. Impact of drinking water salinity on children’s education: Empirical evidence from coastal Bangladesh. Sci. Total. Environ. 2019, 690, 1331–1341. [Google Scholar] [CrossRef]
- Song, Y.; Zhou, A.; Zhang, M.; Wang, H. Assessing the effects of haze pollution on subjective well-being based on Chinese General Social Survey. J. Clean. Prod. 2019, 235, 574–582. [Google Scholar] [CrossRef]
- Shultz, J.M.; Walsh, L.; Garfin, D.R.; Wilson, F.E.; Neria, Y. The 2010 Deepwater Horizon Oil Spill: The Trauma Signature of an Ecological Disaster. J. Behav. Health Serv. Res. 2014, 42, 58–76. [Google Scholar] [CrossRef]
- Berk, M.; Williams, L.J.; Andreazza, A.C.; Pasco, J.A.; Dodd, S.; Jacka, F.N.; Moylan, S.; Reiner, E.J.; Magalhaes, P.V. Pop, heavy metal and the blues: Secondary analysis of persistent organic pollutants (POP), heavy metals and depressive symptoms in the NHANES National Epidemiological Survey. BMJ Open 2014, 4, e005142. [Google Scholar] [CrossRef]
- Forns, J.; Lertxundi, N.; Aranbarri, A.; Murcia, M.; Gascon, M.; Martinez, D.; Grellier, J.; Lertxundi, A.; Julvez, J.; Fano, E.; et al. Prenatal exposure to organochlorine compounds and neuropsychological development up to two years of life. Environ. Int. 2012, 45, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Kyriklaki, A.; Vafeiadi, M.; Kampouri, M.; Koutra, K.; Roumeliotaki, T.; Chalkiadaki, G.; Anousaki, D.; Rantakokko, P.; Kiviranta, H.; Fthenou, E.; et al. Prenatal exposure to persistent organic pollutants in association with offspring neuropsychological development at 4years of age: The Rhea mother-child cohort, Crete, Greece. Environ. Int. 2016, 97, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Chen, Y.; Gao, D.; Jing, J.; Hu, Q. Prenatal and postnatal lead exposure and cognitive development of infants followed over the first three years of life: A prospective birth study in the Pearl River Delta region, China. Neurotoxicology 2014, 44, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Kweon, K.; Kim, H.-W.; Cho, S.W.; Park, J.; Sim, C.S. Negative Impact of Noise and Noise Sensitivity on Mental Health in Childhood. Noise Health 2018, 20, 199–211. [Google Scholar] [CrossRef]
- Staudt, K.; Dane’El, M.; Márquez-Velarde, G. In the shadow of a steel recycling plant in these neoliberal times: Health disparities among Hispanics in a border colonia. Local Environ. 2015, 21, 636–652. [Google Scholar] [CrossRef]
- Kannuri, N.K.; Jadhav, S. Generating toxic landscapes: Impact on well-being of cotton farmers in Telangana, India. Anthr. Med. 2018, 25, 121–140. [Google Scholar] [CrossRef]
- Díaz, J.; López-Bueno, J.; López-Ossorio, J.; Gónzález, J.; Sánchez, F.; Linares, C. Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain). Sci. Total. Environ. 2019, 710, 136315. [Google Scholar] [CrossRef]
- Min, J.-Y.; Min, K.-B. Night noise exposure and risk of death by suicide in adults living in metropolitan areas. Depress. Anxiety 2018, 35, 876–883. [Google Scholar] [CrossRef]
- Han, H.-J.; Kim, J.-H.; Chung, S.-E.; Park, J.-H.; Cheong, H.-K. Estimation of the National Burden of Disease and Vulnerable Population Associated with Natural Disasters in Korea: Heavy Precipitation and Typhoon. J. Korean Med. Sci. 2018, 33, e314. [Google Scholar] [CrossRef]
- Wass, S.V.; Smith, C.G.; Daubney, K.R.; Suata, Z.M.; Clackson, K.; Begum, A.; Mirza, F.U. Influences of environmental stressors on autonomic function in 12-month-old infants: Understanding early common pathways to atypical emotion regulation and cognitive performance. J. Child Psychol. Psychiatry 2019, 60, 1323–1333. [Google Scholar] [CrossRef] [PubMed]
- Ishiki, A.; Okinaga, S.; Tomita, N.; Kawahara, R.; Tsuji, I.; Nagatomi, R.; Taki, Y.; Takahashi, T.; Kuzuya, M.; Morimoto, S.; et al. Changes in Cognitive Functions in the Elderly Living in Temporary Housing after the Great East Japan Earthquake. PLoS ONE 2016, 11, e0147025. [Google Scholar] [CrossRef] [PubMed]
- Maclean, J.C.; Popovici, I.; French, M.T. Are natural disasters in early childhood associated with mental health and substance use disorders as an adult? Soc. Sci. Med. 2016, 151, 78–91. [Google Scholar] [CrossRef]
- Powers, J.R.; Loxton, D.; Baker, J.; Rich, J.L.; Dobson, A.J. Empirical evidence suggests adverse climate events have not affected Australian women’s health and well-being. Aust. N. Z. J. Public Health 2012, 36, 452–457. [Google Scholar] [CrossRef]
- Cherry, K.E.; Sampson, L.; Nezat, P.F.; Cacamo, A.; Marks, L.D.; Galea, S. Long-term psychological outcomes in older adults after disaster: Relationships to religiosity and social support. Aging Ment. Health 2015, 19, 430–443. [Google Scholar] [CrossRef] [PubMed]
- Bistricky, S.L.; Long, L.J.; Lai, B.S.; Gallagher, M.W.; Kanenberg, H.; Elkins, S.R.; Harper, K.L.; Short, M.B. Surviving the storm: Avoidant coping, helping behavior, resilience and affective symptoms around a major hurricane-flood. J. Affect. Disord. 2019, 257, 297–306. [Google Scholar] [CrossRef]
- Felix, E.D.; Afifi, W. The role of social support on mental health after multiple wildfire disasters. J. Community Psychol. 2015, 43, 156–170. [Google Scholar] [CrossRef]
- Felix, E.; Afifi, T.; Kia-Keating, M.; Brown, L.; Afifi, W.; Reyes, G. Family functioning and posttraumatic growth among parents and youth following wildfire disasters. Am. J. Orthopsychiatry 2015, 85, 191–200. [Google Scholar] [CrossRef]
- Afifi, W.A.; Felix, E.D.; Afifi, T.D. The impact of uncertainty and communal coping on mental health following natural disasters. Anxiety Stress Coping 2012, 25, 329–347. [Google Scholar] [CrossRef]
- Ritchie, A.; Sautner, B.; Omege, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; Greenshaw, A.; Chue, P.; et al. Long-Term Mental Health Effects of a Devastating Wildfire Are Amplified by Sociodemographic and Clinical Antecedents in College Students. Disaster Med. Public Health Prep. 2020, 15, 707–717. [Google Scholar] [CrossRef]
- Chen, Y.; Yuan, Y. The neighborhood effect of exposure to blue space on elderly individuals’ mental health: A case study in Guangzhou, China. Health Place 2020, 63, 102348. [Google Scholar] [CrossRef]
- Dempsey, S.; Devine, M.T.; Gillespie, T.; Lyons, S.; Nolan, A. Coastal blue space and depression in older adults. Health Place 2018, 54, 110–117. [Google Scholar] [CrossRef]
- Gascon, M.; Sánchez-Benavides, G.; Dadvand, P.; Martínez, D.; Gramunt, N.; Gotsens, X.; Cirach, M.; Vert, C.; Molinuevo, J.L.; Crous-Bou, M.; et al. Long-term exposure to residential green and blue spaces and anxiety and depression in adults: A cross-sectional study. Environ. Res. 2018, 162, 231–239. [Google Scholar] [CrossRef]
- Costello, L.; McDermott, M.-L.; Patel, P.; Dare, J. ‘A lot better than medicine’—Self-organised ocean swimming groups as facilitators for healthy ageing. Health Place 2019, 60, 102212. [Google Scholar] [CrossRef]
- Tosone, C.; McTighe, J.P.; Bauwens, J. Shared Traumatic Stress among Social Workers in the Aftermath of Hurricane Katrina. Br. J. Soc. Work 2015, 45, 1313–1329. [Google Scholar] [CrossRef]
- Generaal, E.; Timmermans, E.J.; Dekkers, J.E.C.; Smit, J.H.; Penninx, B.W.J.H. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychol. Med. 2018, 49, 149–161. [Google Scholar] [CrossRef]
- Bell, A. Life-course and cohort trajectories of mental health in the UK, 1991–2008—A multilevel age–period–cohort analysis. Soc. Sci. Med. 2014, 120, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Fryers, T.; Melzer, D.; Jenkins, R. Social inequalities and the common mental disorders—A systematic review of the evidence. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Cherry, N.; Haynes, W. Effects of the Fort McMurray wildfires on the health of evacuated workers: Follow-up of 2 cohorts. CMAJ Open 2017, 5, E638–E645. [Google Scholar] [CrossRef] [PubMed]
- Gould, D.W.; Teich, J.L.; Pemberton, M.R.; Pierannunzi, C.; Larson, S. Behavioral health in the gulf coast region following the Deepwater Horizon oil spill: Findings from two federal surveys. J. Behav. Health Serv. Res. 2014, 42, 6–22. [Google Scholar] [CrossRef]
- Buttke, D.; Vagi, S.; Bayleyegn, T.; Sircar, K.; Strine, T.; Morrison, M.; Allen, M.; Wolkin, A. Mental Health Needs Assessment After the Gulf Coast Oil Spill—Alabama and Mississippi, 2010. Prehospital Disaster Med. 2012, 27, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Clemens, S.L.; Berry, H.L.; McDermott, B.M.; Harper, C.M. Summer of sorrow: Measuring exposure to and impacts of trauma after Queensland’s natural disasters of 2010–2011. Med. J. Aust. 2013, 199, 552–555. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.W.; Elizalde, A.; Cummins, S.; Leyland, A.H.; Botha, W.; Briggs, A.; Tilley, S.; de Oliveira, E.S.; Roe, J.; Aspinall, P.; et al. Enhancing Health Through Access to Nature: How Effective are Interventions in Woodlands in Deprived Urban Communities? A Quasi-experimental Study in Scotland, UK. Sustainability 2019, 11, 3317. [Google Scholar] [CrossRef]
- Dzhambov, A.M. Residential green and blue space associated with better mental health: A pilot follow-up study in university students. Arch. Ind. Hyg. Toxicol. 2018, 69, 340–349. [Google Scholar] [CrossRef]
- Sarkar, C.; Gallacher, J.; Webster, C. Urban built environment configuration and psychological distress in older men: Results from the Caerphilly study. BMC Public Health 2013, 13, 695. [Google Scholar] [CrossRef]
- Díaz, S.; Demissew, S.; Carabias, J.; Joly, C.; Lonsdale, M.; Ash, N.; Larigauderie, A.; Adhikari, J.R.; Arico, S.; Báldi, A.; et al. The IPBES conceptual Framework–connecting nature and people. Curr Opin Environ Sustain. 2015, 14, 1016. [Google Scholar] [CrossRef]
- IPBES. Summary for Policymakers of the Global Assessment Report on Biodiversity and Ecosystem Services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services; Díaz, S., Settele, J., Brondízio, E.S., Ngo, H.T., Guèze, M., Agard, J., Arneth, A., Balvanera, P., Brauman, K.A., Butchart, S.H.M., et al., Eds.; IPBES secretariat: Bonn, Germany, 2019. [Google Scholar]
- Farinde, A.; Dose-Response Relationships. MSD Manual Professional Version. 2021. Available online: https://www.msdmanuals.com/en-gb/professional/clinical-pharmacology/pharmacodynamics/dose-response-relationships (accessed on 5 September 2022).
- Frumkin, H.; Gregory, N.; Bratman, G.N.; Breslow, S.J.; Cochran, B.; Kahn, P.H., Jr.; Lawler, J.J.; Levin, P.S.; Tandon, P.S.; Varanasi, U.; et al. Nature Contact and Human Health: A Research Agenda. Environ. Health Perspect. 2017, 125, 075001. [Google Scholar] [CrossRef]
- Merdjanoff, A.A.; Abramson, D.M.; Piltch-Loeb, R.; Findley, P.; Peek, L.; Beedasy, J.; Park, Y.S.; Sury, J.; Meltzer, G.Y. Examining the Dose–Response Relationship: Applying the Disaster Exposure Matrix to Understand the Mental Health Impacts of Hurricane Sandy. Clin. Soc. Work. J. 2021, 50, 400–413. [Google Scholar] [CrossRef]
- Few, R.; Lake, I.; Hunter, P.R.; Tran, P.G. ‘Seasonality, disease and behavior: Using multiple methods to explore socio-environmental health risks in the Mekong Delta’. Soc. Sci. Med. 2013, 80, 1–9. [Google Scholar] [CrossRef]
- Zeira, A. Mental Health Challenges Related to Neoliberal Capitalism in the United States. Community Ment. Health J. 2021, 58, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, R.; Pickett, K. The Spirit Level: Why Greater Equality Makes Societies Stronger; Bloomsbury Press: New York, NY, USA, 2009. [Google Scholar]
- IPBES. Global Assessment Report of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services; Brondízio, E.S., Settele, J., Díaz, S., Ngo, H.T., Eds.; IPBES secretariat: Bonn, Germany, 2019. [Google Scholar]
- Fanning, A.L.; O’Neill, D.W.; Hickel, J.; Roux, N. The social shortfall and ecological overshoot of nations. Nat. Sustain. 2021, 5, 26–36. [Google Scholar] [CrossRef]
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: A Report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- van Agteren, J.; Iasiello, M.; Lo, L.; Bartholomaeus, J.; Kopsaftis, Z.; Carey, M.; Kyrios, M. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat. Hum. Behav. 2021, 5, 631–652. [Google Scholar] [CrossRef] [PubMed]
- Carbone, S. What Works to Support the Mental Health and Wellbeing of Children Aged 0–12? A Review of the Latest Research Evidence; Prevention United: Melbourne, Australia, 2021. [Google Scholar]
- van Agteren, J.; Ali, K.; Fassnacht, D.B.; Iasiello, M.; Furber, G.; Howard, A.; Woodyatt, L.; Musker, M.; Kyrios, M. Testing the differential impact of an internet-based mental health intervention on outcomes of well-being and psychological distress during COVID-19: Uncontrolled intervention study. JMIR Mental Health 2021, 8, e28044. [Google Scholar] [CrossRef]
- Darcy, P.M.; Taylor, J.; Mackay, L.; Ellis, N.J.; Gidlow, C.J. Understanding the Role of Nature Engagement in Supporting Health and Wellbeing during COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 3908. [Google Scholar] [CrossRef]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.; de Vries, S.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.; et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef]
| Mental Health Keywords. | Environmental Science Keywords | Exclusions | ||
|---|---|---|---|---|
| “mental health” OR “mental ill*” OR “mental disorder” OR “mental health and wellbeing” OR “mental wellbeing” OR “cognitive development” OR “cognitive decline” OR “psychopatholog*” | AND | flood* OR drought OR wildfire OR “bush fire” OR “forest fire” OR landslide* OR “climate change” OR “global warming” OR landscape OR noise OR soundscape OR pollut* OR biodivers* OR tree* OR forest* OR wood* OR wild* OR “natural environment” OR “natural land” OR “natural space” OR “natural area” OR “air quality” OR “water quality” OR ecosystem OR lake OR river OR coastal OR erosion | NOT | mice OR mouse OR rat* OR rodent* OR drosophila |
| Research Question | Data Extracted |
|---|---|
| What is the current contribution of environmental science to mental health research? | Environmental science topic |
| Mental health area | |
| Interaction between environmental science and mental health 1 | |
| Measures (e.g., mean temperature, presence of oil spill, and prescription rates) | |
| Geographic location of study | |
| Study population characteristics (e.g., population, study sample size) | |
| What are the current research designs and methodological approaches being used in environmental science-mental health research? | Methods (e.g., rainfall records, self-report questionnaire) |
| Study design (lab, field, and secondary data) | |
| Analysis (e.g., regression, ANOVA, and content analysis) | |
| How does the relationship between environmental science and mental health research relate to existing evidence linking mental health and wellbeing to demographic, social, economic, and genetic determinants? | Additional determinants/variables |
| What are the evidence gaps and opportunities for the contribution of environmental science to mental health research? | Future research suggested by study authors |
| Theme (Sub-Theme) | Barton and Grant [25] Domains | Description | No. of Papers | |
|---|---|---|---|---|
| From scoping review | ||||
| Natural disasters (general) | Air, climate change, land, and water | A catastrophic natural event (e.g., hurricane, drought, landslide), excluding fire. | 50 | |
| Natural disasters (wildfire) | Climate change and land | A specific type of natural disaster caused by fire. | 20 | |
| Noise | n/a | Natural or anthropogenic noise. | 36 | |
| Pollution (general) | Air, land, and water | Chemical additions to environment, excluding oil spills. | 19 | |
| Pollution (oil spill) | Water | Chemical addition to environment in form of oil spill. | 14 | |
| Natural environments | Biodiversity, land, natural habitats, and water | Environments containing natural features, although may have varied levels of anthropogenic influences (e.g., agricultural land). | 32 | |
| Meteorological conditions (general) | Air, climate change, and water | Typical weather conditions experienced seasonally, monthly to daily such as fluctuations in humidity and rainfall, except temperature. More intensive storm and rainfall events (e.g., Typhoons, hurricanes) were covered in Natural disasters 1 (general). | 7 | |
| Meteorological conditions (temperature) | Air and climate change | Typical temperature conditions experienced seasonally, monthly to daily. | 16 | |
| From reviews | ||||
| Climate Change | Climate change | Change in global or regional climate conditions | n/a 2 | |
| Flooding | Water and climate change | Inundation of normally dry land by large volumes of water | n/a 2 | |
| Air pollution | Air | Chemical additions to the atmosphere | n/a 2 | |
| Urban green space | Land, natural habitats, and biodiversity | Natural environments in urban areas, predominately publicly accessible spaces | n/a 2 | |
| Mental Health Area | ICD-10 Classification | Definition | No. of Papers |
|---|---|---|---|
| General mental health | NA | Day-to-day mental health, not linked to specific disorder. | 100 |
| Wellbeing | NA | Conceptualised as a subjectively experienced positive mental state (see Box 1). | 27 |
| Schizophrenia and delusional disorders | F20–F29 | Including chronic, acute, and transient psychotic disorders, of which schizophrenia is the most prominent disorder. | 3 |
| Mood disorders | F30–F39 | Disorders in which the fundamental disturbance is a change in affect or mood to depression (with or without associated anxiety) or to elation. | 56 |
| Neurotic disorders | F40–F48 | Include anxiety, stress, obsessive-compulsive disorder, and dissociative disorders. | 30 |
| Behavioural disorders | F50–F69 and F90–F98 | Conditions and behaviour patterns of clinical significance which tend to be persistent and appear to be the expression of the individual’s characteristic lifestyle and mode of relating to themselves and others. Including sleep, eating and sexual disorders. | 4 |
| Substance abuse | F10–F19 | Disorders attributable to the use of one or more psychoactive substances. | 8 |
| Disorders of adult personality and behaviour | F60–F69 | Severe disturbances in the personality and behavioural tendencies of the individual. | 0 |
| Mental retardation | F70–F79 | A condition of arrested or incomplete development of the mind. | 0 |
| Disorders of psychological development | F80–F89 | Disorder with onset during infancy or childhood involving impairment or delay in development of functions that are strongly related to biological maturation of the central nervous system. | 0 |
| Suicide or self-harm | X60–X84 | Purposefully self-inflicted poisoning or injury. | 7 |
| Cognitive development | NA | Development of knowledge acquisition and application. Including memory, problem solving, reasoning, and executive function. | 7 |
| Cognitive decline | NA | Decline of knowledge acquisition and application. Including memory, problem solving, reasoning, and executive function. | 2 |
| Theme (Sub-Theme) | General Mental Health | Mental Wellbeing | Schizophrenia and Delusional Disorders | Mood Disorders | Neurotic Disorders | Behavioural Disorders | Substance Abuse | Suicide or Self-Harm | Cognitive Development | Cognitive Decline |
|---|---|---|---|---|---|---|---|---|---|---|
| Natural disasters (general) | 28 | 0 | 0 | 16 | 19 | 4 | 3 | 4 | 0 | 1 |
| Natural disasters (wildfire) | 9 | 3 | 1 | 11 | 15 | 1 | 3 | 2 | 0 | 0 |
| Noise | 19 | 1 | 0 | 12 | 9 | 3 | 0 | 3 | 1 | 0 |
| Pollution (general) | 5 | 1 | 1 | 5 | 3 | 1 | 1 | 2 | 7 | 0 |
| Pollution (oil spill) | 5 | 3 | 0 | 7 | 8 | 0 | 0 | 2 | 0 | 0 |
| Natural environments | 15 | 7 | 0 | 10 | 10 | 1 | 0 | 0 | 0 | 0 |
| Meteorological conditions (general) | 5 | 0 | 2 | 2 | 1 | 0 | 0 | 1 | 0 | 0 |
| Meteorological conditions (temperature) | 12 | 1 | 1 | 3 | 3 | 0 | 1 | 1 | 0 | 1 |
| Review Topic | Paper | Years Covered | Including Grey Literature | Geographic Scope | Mental Health Areas |
|---|---|---|---|---|---|
| Climate change | Berry et al., 2011 [83] | Not specified | Yes | Global | Depression, anxiety, psychosis, Post-Traumatic Stress Disorder (PTSD), and suicide |
| Chan et al., 2019 [84] | 2000–2018 | Yes | China | General mental health and PTSD | |
| van den Bosch and Meyer-Lindenberg, 2019 [85] | Not specified | Yes | Global | Depression and suicide | |
| Veenema et al., 2017 [9] | Not specified | No | Global | General mental health | |
| Hayes et al., 2019 [86] | 2000–2017 | Yes | Global | Substance abuse, depression, anxiety, PTSD, and suicide | |
| Hayes and Poland, 2018 [8] | 2000–2017 | Yes | Global | substance abuse, depression, anxiety, PTSD, and suicide | |
| Kinay et al., 2019 [87] | 2000 onwards | Yes | China | General mental health | |
| Jaakkola et al., 2018 [88] | 1990–2017 | Yes | Canada | Mental wellbeing | |
| Patz et al., 2014 [89] | 2009–2014 | Yes | Global | General mental health | |
| Dannenberg et al., 2018 [90] | Not specified | Yes | Global | General mental health | |
| Yusa et al., 2015 [91] | 1993–2013 | Yes | Global | Depression and suicide | |
| Flooding | Berry et al., 2011 [83] | Not specified | Yes | Global | Depression, anxiety, psychosis, PTSD, and suicide |
| Chan et al., 2019 [84] | 2000–2018 | Yes | China | General mental health and PTSD | |
| Veenema et al., 2017 [9] | Not specified | No | Global | General mental health | |
| Garcia and Sheehan, 2016 [92] | to 2015 | Yes | Global | General mental health | |
| Burton et al., 2016 [93] | 2005–2015 | Yes | Canada | General mental health and PTSD | |
| Du et al., 2010 [94] | 1998 onwards | Yes | Global | General mental health | |
| Mousavi et al., 2020 [95] | to 2017 | Yes | Iran | General mental health | |
| Schulte et al., 2016 [96] | 2008–2014 | Yes | Global | General mental health | |
| Verner et al., 2016 [97] | 1990–2014 | No | Global | General mental health | |
| Stanke et al., 2012 [98] | 2004–2010 | No | Global | General mental health | |
| Air pollution | van den Bosch and Meyer-Lindenberg, 2019 [85] | Not specified | Yes | Global | Depression and suicide |
| Braithwaite et al., 2019 [10] | 1974–2017 | No | Global | Psychiatric disorder, depression, anxiety, bipolar disorder, psychosis, and suicide | |
| Tzivian et al., 2015 [99] | Not specified | Yes | Global | Anxiety, mood disorders, cognition, Alzheimer’s, and cognitive decline | |
| Bos et al., 2014 [100] | 2009–2013 | No | Global | Cognition | |
| Cipriani et al., 2018 [101] | to 2017 | Yes | Global | Cognition, cognitive decline, Alzheimer’s, and dementia | |
| de Prado Bert et al., 2018 [102] | to 2017 | Yes | Global | Cognitive development | |
| Buoli et al., 2018 [103] | 1982- 2018 | Yes | Global | General mental health schizophrenia and delusional disorders, depression, anxiety, Attention Deficit Hyperactive Disorder (ADHD), autism, and suicide | |
| Green space | van den Bosch and Meyer-Lindenberg, 2019 [85] | Not specified | Yes | Global | Suicide and depression |
| Gladkikh et al., 2019 [104] | to 2018 | Yes | Global | General mental health | |
| Hankey and Marshall, 2017 [105] | Not specified | Yes | Global | Depression, anxiety, and cognitive decline | |
| Kabisch, 2019 [12] | 2013 onwards | No | Global | General mental health and wellbeing |
| Quantitative | Qualitative | Quantitative | Qualitative | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cognitive and Mental Health Area | Descriptive | Correlation | ANOVA | Regression | Delphi | Path Modelling/SEM | Bayesian Modelling | Case Crossover | Principal Component Analysis | Latent Class | Mediation Modelling | Risk Ratio | Chi Squared | Content Analysis | Phenomenological | Thematic Analysis | Grounded Theory | Mixed | Descriptive | Correlation | ANOVA | Regression | Delphi | Path Modelling/SEM | Bayesian Modelling | Case Crossover | Principal Component Analysis | Latent Class | Mediation Modelling | Risk Ratio | Chi Squared | Content Analysis | Phenomenological | Thematic Analysis | Grounded Theory | Mixed | ||
| Natural disasters (general) | Natural disasters (wildfire) | |||||||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||||||
| Behavioural disorders | ||||||||||||||||||||||||||||||||||||||
| Suicide or self-harm | ||||||||||||||||||||||||||||||||||||||
| Cognitive development | ||||||||||||||||||||||||||||||||||||||
| Cognitive decline | ||||||||||||||||||||||||||||||||||||||
| Pollution (general) | Pollution (oil spill) | |||||||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||||||
| Behavioural disorders | ||||||||||||||||||||||||||||||||||||||
| Suicide or self-harm | ||||||||||||||||||||||||||||||||||||||
| Cognitive development | ||||||||||||||||||||||||||||||||||||||
| Cognitive decline | ||||||||||||||||||||||||||||||||||||||
| Noise | Natural environments | |||||||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||||||
| Behavioural disorders | ||||||||||||||||||||||||||||||||||||||
| Suicide or self-harm | ||||||||||||||||||||||||||||||||||||||
| Cognitive development | ||||||||||||||||||||||||||||||||||||||
| Cognitive decline | ||||||||||||||||||||||||||||||||||||||
| Meteorological conditions (general) | Meteorological conditions (temperature) | |||||||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||||||
| Behavioural disorders | ||||||||||||||||||||||||||||||||||||||
| Suicide or self-harm | ||||||||||||||||||||||||||||||||||||||
| Cognitive development | ||||||||||||||||||||||||||||||||||||||
| Cognitive decline | ||||||||||||||||||||||||||||||||||||||
| Social | Economic | Demographic | Genetic | Social | Economic | Demographic | Genetic | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cognitive and Mental Health Domains | Social Class | Neighbourhood Characteristics | Community Resilience | Relationship Status | Social Contact and Support | Access to Car | Working Status | Quality of Life | Income | Gender | Age | Education | Health and Lifestyle | Children | Ethnicity | Family History | Social Class | Neighbourhood Characteristics | Community Resilience | Relationship Status | Social Contact and Support | Access to Car | Working Status | Quality of Life | Income | Gender | Age | Education | Health and Lifestyle | Children | Ethnicity | Family History | ||
| Natural disasters (general) | Natural disasters (wildfire) | |||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||
| Behavioural disorders | ||||||||||||||||||||||||||||||||||
| Suicide or self-harm | ||||||||||||||||||||||||||||||||||
| Cognitive Development | ||||||||||||||||||||||||||||||||||
| Cognitive Decline | ||||||||||||||||||||||||||||||||||
| Pollution (general) | Pollution (oil spill) | |||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||
| Behavioural syndromes | ||||||||||||||||||||||||||||||||||
| Suicide and self-harm | ||||||||||||||||||||||||||||||||||
| Cognitive Development | ||||||||||||||||||||||||||||||||||
| Cognitive Decline | ||||||||||||||||||||||||||||||||||
| Noise | Natural environments | |||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||
| Behavioural syndromes | ||||||||||||||||||||||||||||||||||
| Suicide and self-harm | ||||||||||||||||||||||||||||||||||
| Cognitive Development | ||||||||||||||||||||||||||||||||||
| Cognitive Decline | ||||||||||||||||||||||||||||||||||
| Meteorological conditions (general) | Meteorological conditions (temperature) | |||||||||||||||||||||||||||||||||
| General mental health | ||||||||||||||||||||||||||||||||||
| Wellbeing | ||||||||||||||||||||||||||||||||||
| Substance abuse | ||||||||||||||||||||||||||||||||||
| Schizophrenia and delusional disorders | ||||||||||||||||||||||||||||||||||
| Mood disorders | ||||||||||||||||||||||||||||||||||
| Neurotic disorders | ||||||||||||||||||||||||||||||||||
| Behavioural syndromes | ||||||||||||||||||||||||||||||||||
| Suicide and self-harm | ||||||||||||||||||||||||||||||||||
| Cognitive Development | ||||||||||||||||||||||||||||||||||
| Cognitive Decline | ||||||||||||||||||||||||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roberts, M.; Colley, K.; Currie, M.; Eastwood, A.; Li, K.-H.; Avery, L.M.; Beevers, L.C.; Braithwaite, I.; Dallimer, M.; Davies, Z.G.; et al. The Contribution of Environmental Science to Mental Health Research: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 5278. https://doi.org/10.3390/ijerph20075278
Roberts M, Colley K, Currie M, Eastwood A, Li K-H, Avery LM, Beevers LC, Braithwaite I, Dallimer M, Davies ZG, et al. The Contribution of Environmental Science to Mental Health Research: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(7):5278. https://doi.org/10.3390/ijerph20075278
Chicago/Turabian StyleRoberts, Michaela, Kathryn Colley, Margaret Currie, Antonia Eastwood, Kuang-Heng Li, Lisa M. Avery, Lindsay C. Beevers, Isobel Braithwaite, Martin Dallimer, Zoe G. Davies, and et al. 2023. "The Contribution of Environmental Science to Mental Health Research: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 7: 5278. https://doi.org/10.3390/ijerph20075278
APA StyleRoberts, M., Colley, K., Currie, M., Eastwood, A., Li, K.-H., Avery, L. M., Beevers, L. C., Braithwaite, I., Dallimer, M., Davies, Z. G., Fisher, H. L., Gidlow, C. J., Memon, A., Mudway, I. S., Naylor, L. A., Reis, S., Smith, P., Stansfeld, S. A., Wilkie, S., & Irvine, K. N. (2023). The Contribution of Environmental Science to Mental Health Research: A Scoping Review. International Journal of Environmental Research and Public Health, 20(7), 5278. https://doi.org/10.3390/ijerph20075278







