Aspects of Dental Occlusion Assessed with the T-Scan System among a Group of Romanian Dental Students in a Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants’ Selection Process
2.2. sEMG Recordings
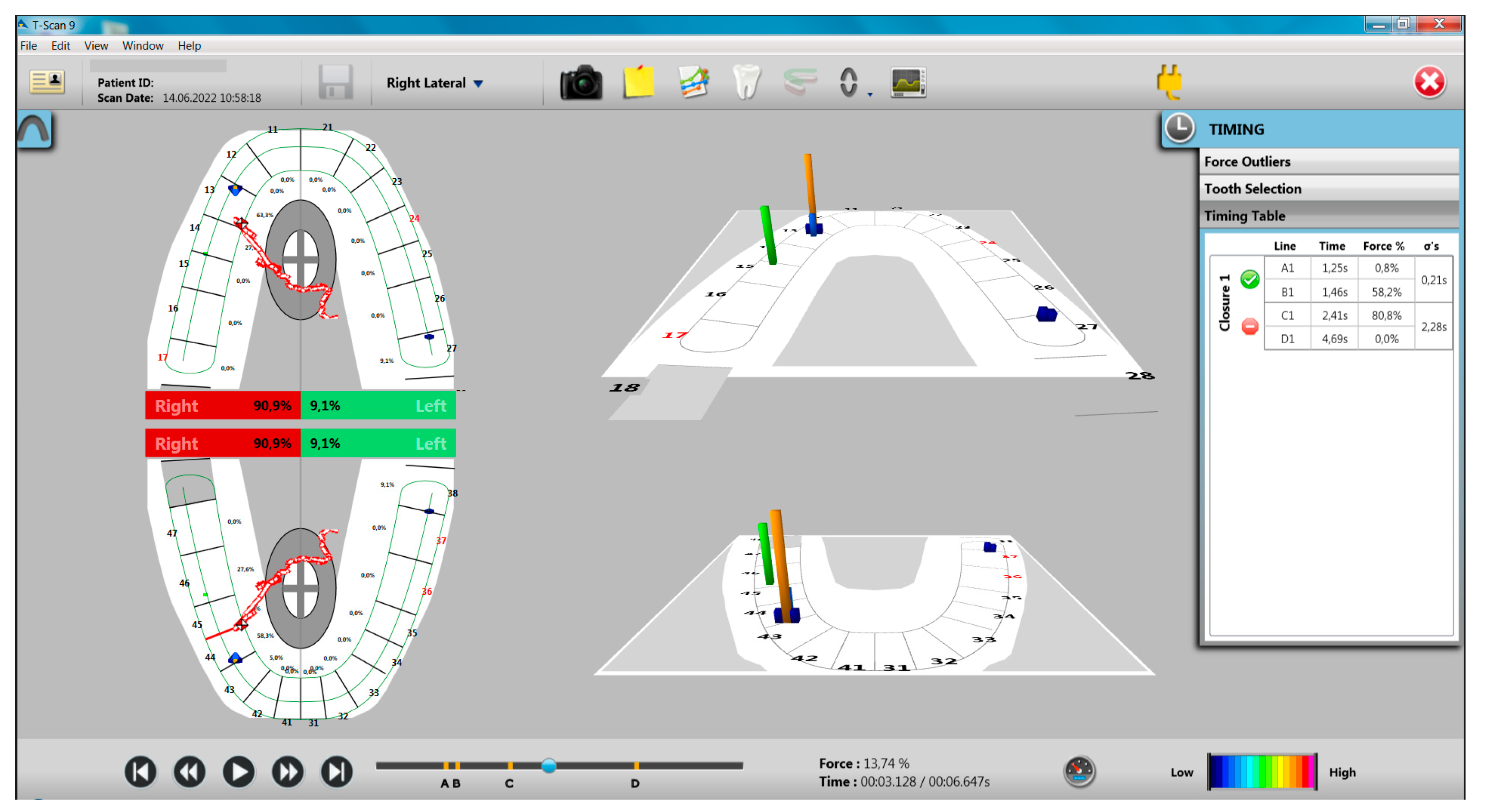
2.3. Occlusal Recordings with the T-Scan System
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Groups
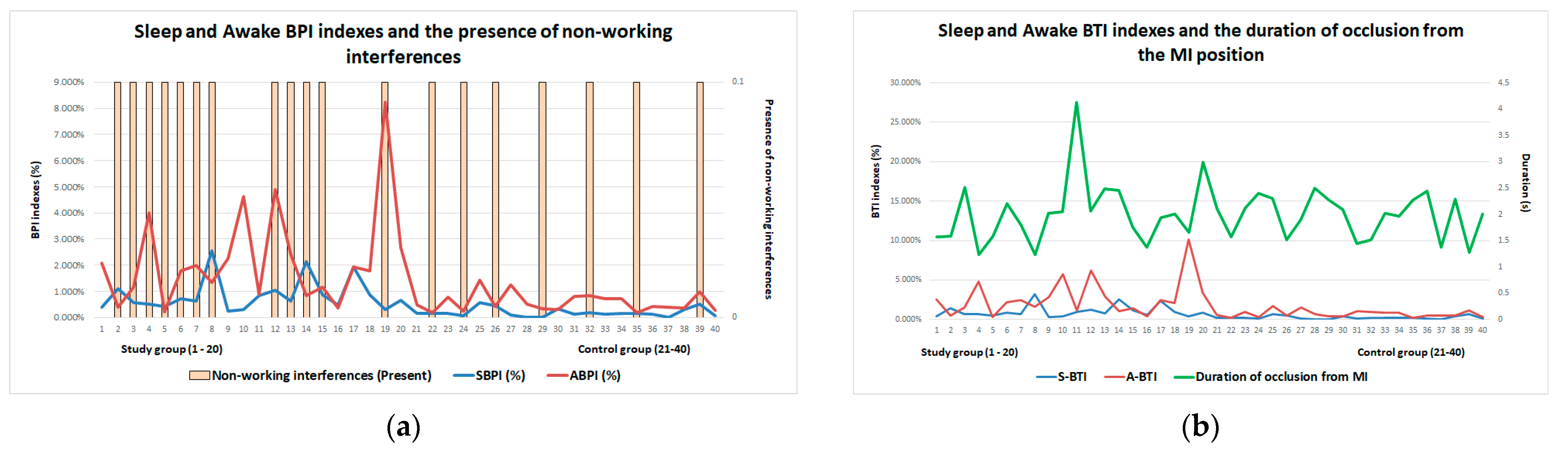
3.2. Occlusal Recordings
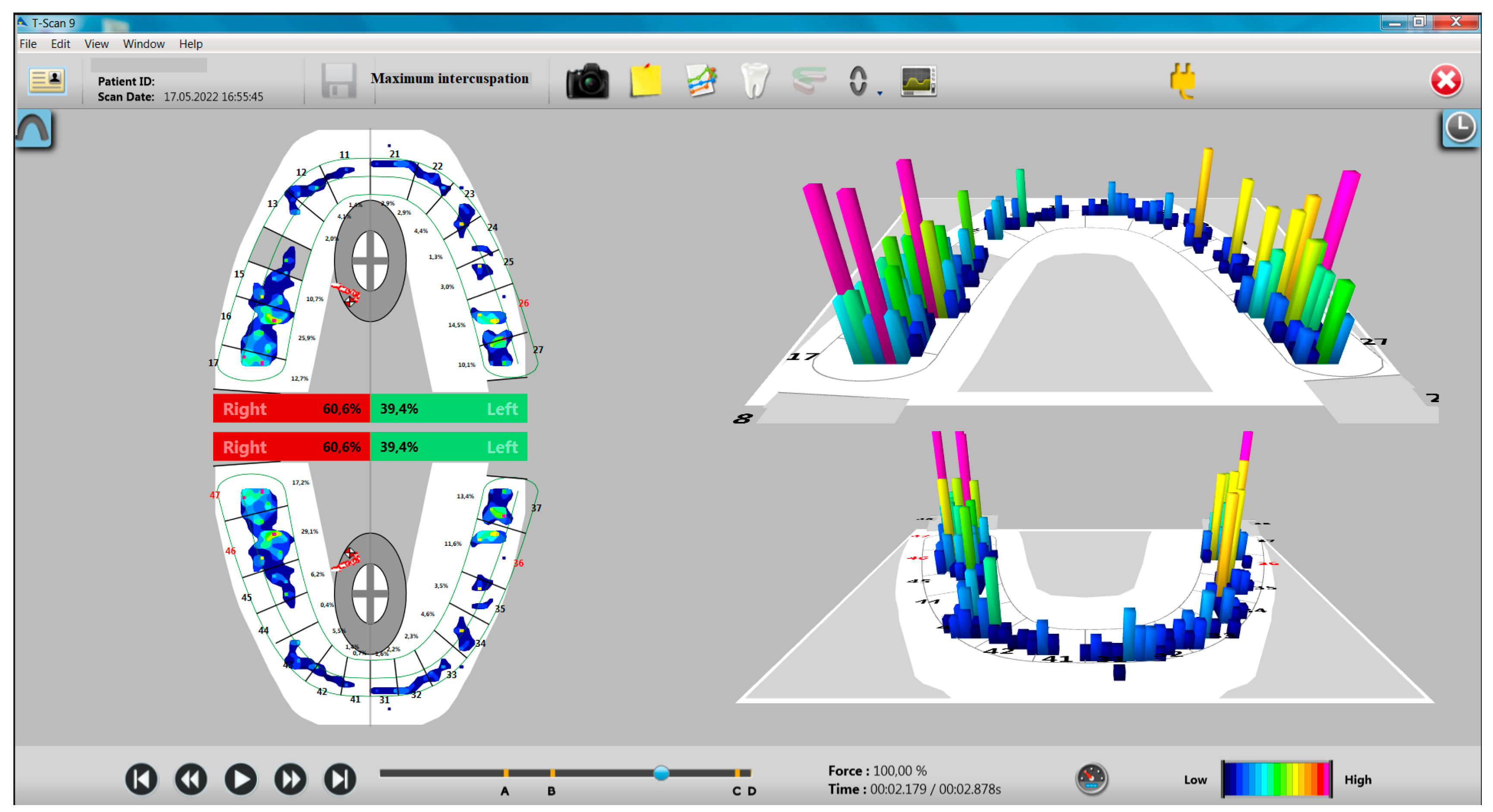
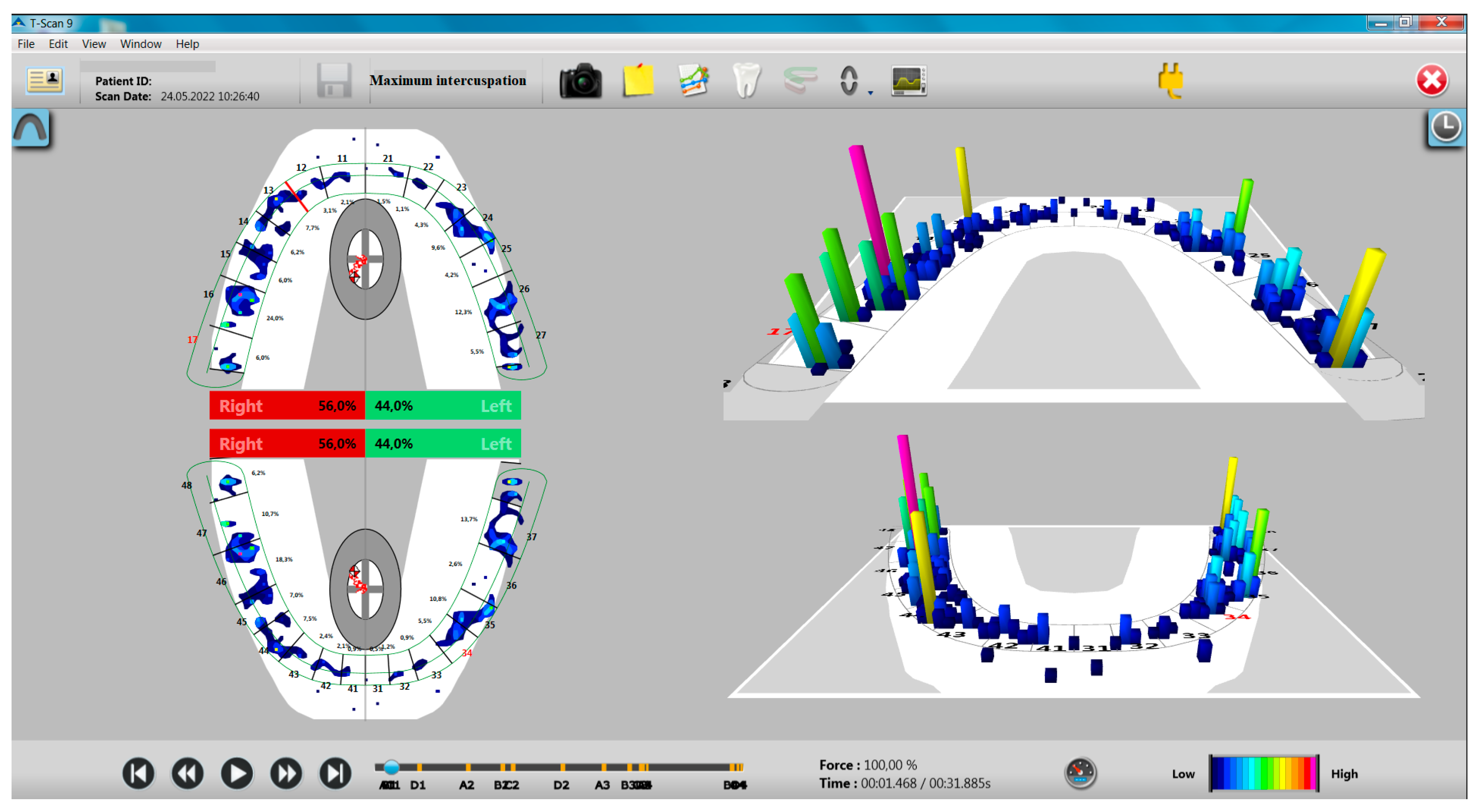
3.2.1. Evaluation of Recordings in the Position of MI
3.2.2. Evaluation of Recordings from Mandibular Movements
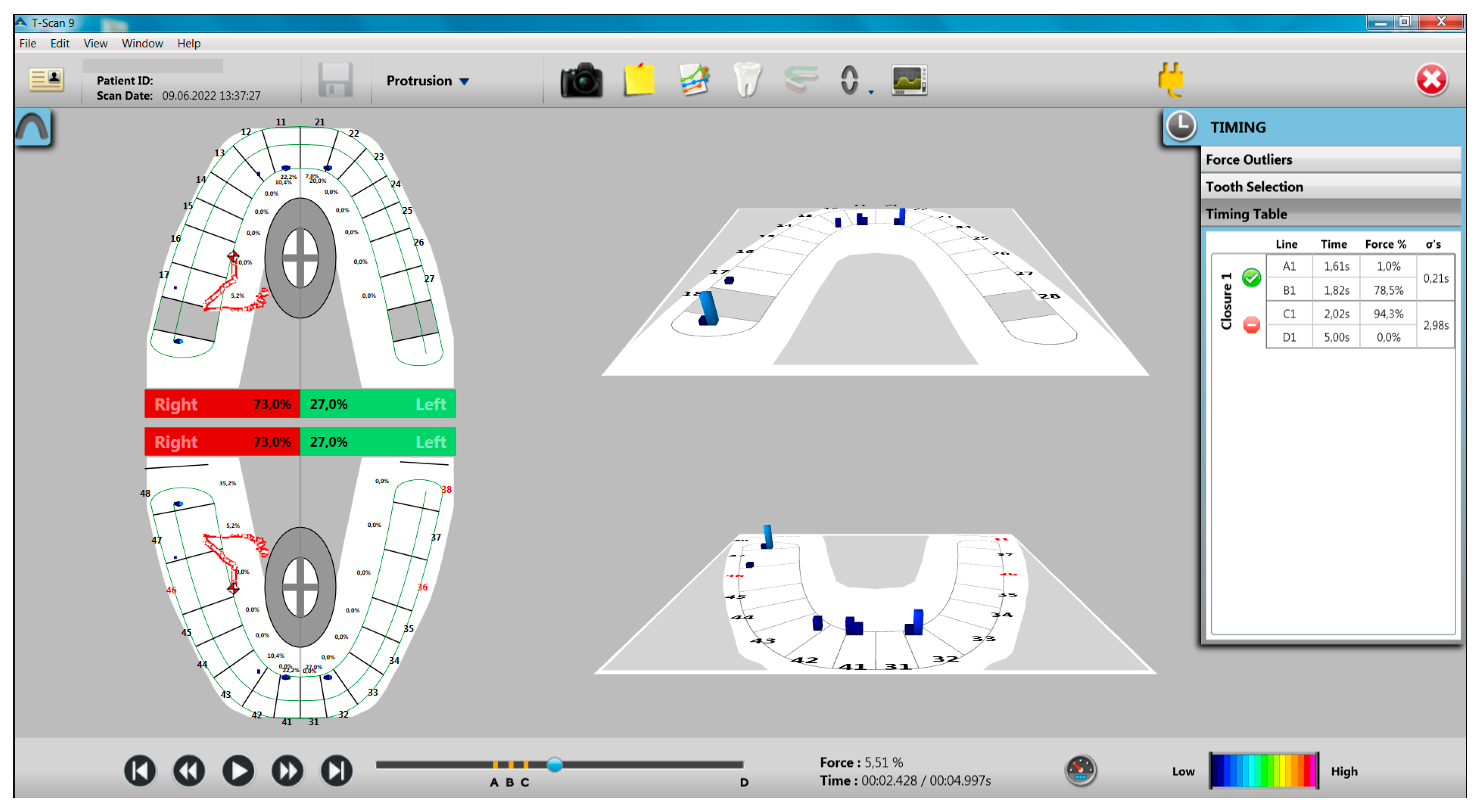
Evaluation of Protrusion Movement
- Participants with incisal guidance showed lower values of occlusal forces distributed on the right hemiarch in MI and higher values of occlusal forces distributed on the left hemiarch in MI, compared to participants without incisal guidance, differences between these groups being statistically significant (p < 0.0005);
- Participants with work interferences presented similar values of the distribution of occlusal forces at the level of the right and left hemiarch compared to participants without work interferences;
- Participants with non-working interferences presented higher values of forces distributed on the right hemiarch in MI and lower values of forces distributed on the left hemiarch in MI, compared to participants without non-working interferences, differences between these groups being statistically significant (p = 0.027 for forces from the level of the right hemiarch in MI and p = 0.025 for the forces from the level of the left hemiarch in MI) (Table 7).
- Group A—participants without working interferences and without non-working interferences;
- Group B—participants without working interferences and with non-working interferences;
- Group C—participants with working interferences and without non-working interferences;
- Group D—participants with work interferences and with non-work interferences.
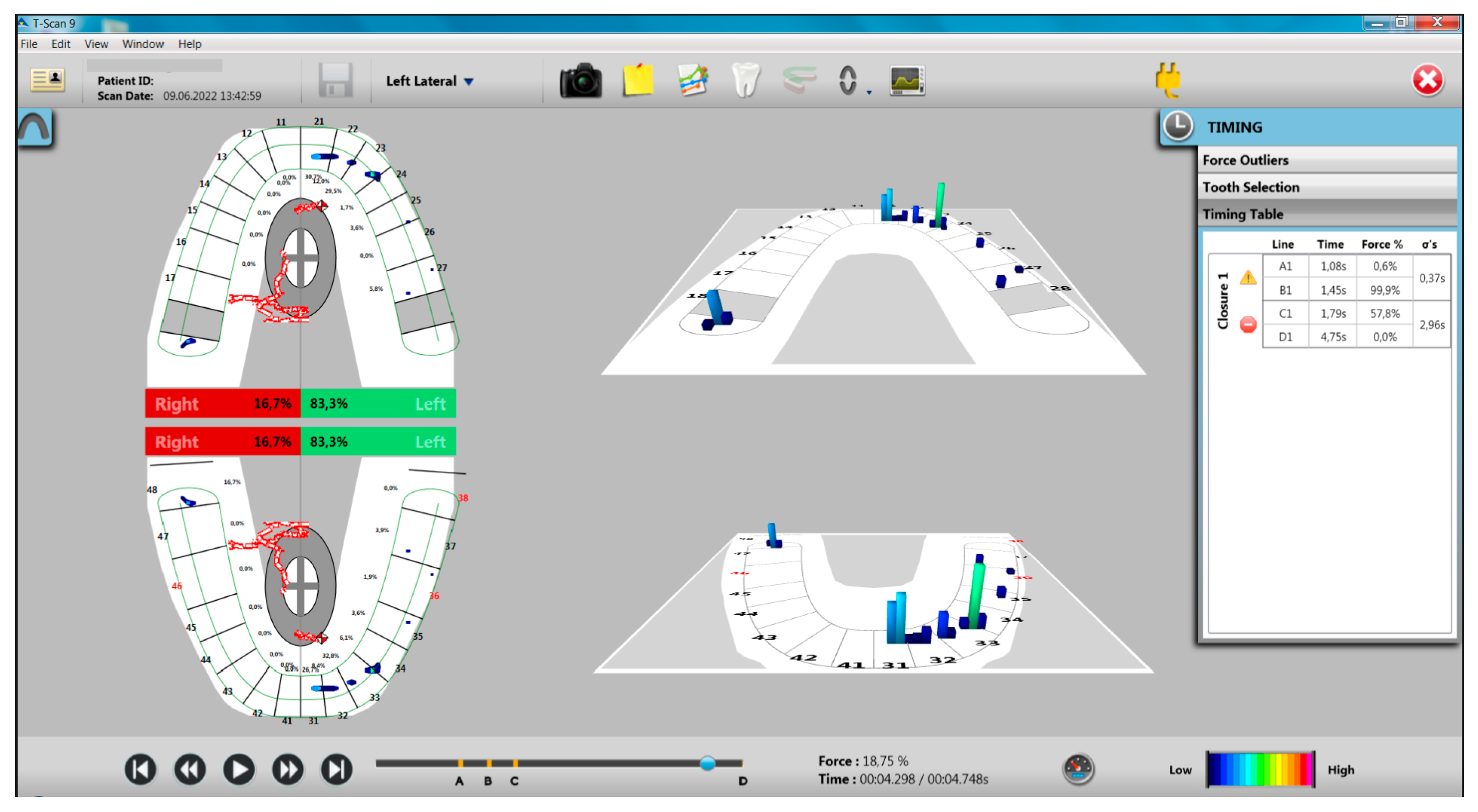
Evaluation of Laterotrusion Movements
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lobbezoo, F.; Ahlberg, J.; Glaros, A.G.; Kato, T.; Koyano, K.; Lavigne, G.J.; Manfredini, D.; Svensson, P.; Winocur, E. Bruxism defined and graded: An international consensus. J. Oral Rehabil. 2013, 40, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Ferro, K.J. The glossary of prosthodontic terms. J. Prosthet. Dent. 2005, 94, 10–92. [Google Scholar]
- International Classification of Sleep Disorders, 2nd ed.; American Academy of Sleep Medicine: Westchester, UK, 2005.
- De Leeuw, R. (Ed.) Orofacial Pain. Guidelines for Assessment, Diagnosis, and Management, 4th ed.; Quintessence Publishing Co., Inc.: Chicago, IL, USA, 2008; p. 316. [Google Scholar]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bender, S.; Bracci, A.; Cistulli, P.A.; Conti, P.C.; De Leeuw, R.; Durham, J.; Emodi-Perlman, A.; et al. Standardised Tool for the Assessment of Bruxism. J. Oral Rehabil. 2023, in press. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bracci, A.; Durham, J.; Emodi-Perlman, A.; Ettlin, D.; Gallo, L.M.; Häggman-Henrikson, B.; Koutris, M.; et al. The development of the Standardised Tool for the Assessment of Bruxism (STAB): An international road map. J. Oral Rehabil. 2022, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Bracci, A.; Lobbezoo, F.; Häggman-Henrikson, B.; Colonna, A.; Nykänen, L.; Pollis, M.; Ahlberg, J.; Manfredini, D. International Network for Orofacial Pain and Related Disorders Methodology. Current Knowledge and Future Perspectives on Awake Bruxism Assessment: Expert Consensus Recommendations. J. Clin. Med. 2022, 11, 5083. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Lobbezoo, F. Bruxism definition: Past, present, and future—What should a prosthodontist know? J. Prosthet. Dent. 2021, 128, 905–912. [Google Scholar] [CrossRef]
- Lavigne, G.; Kato, T.; Babiloni, A.H.; Huynh, N.; Fabbro, C.D.; Svensson, P.; Aarab, G.; Ahlberg, J.; Baba, K.; Carra, M.C.; et al. Research routes on improved sleep bruxism metrics: Toward a standardised approach. J. Sleep Res. 2021, 30, e13320. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bracci, A.; Durham, J.; Ettlin, D.; Gallo, L.M.; Koutris, M.; Wetselaar, P.; Svensson, P.; et al. Towards a Standardized Tool for the Assessment of Bruxism (STAB)-Overview and general remarks of a multidimensional bruxism evaluation system. J. Oral Rehabil. 2020, 47, 549–556. [Google Scholar] [CrossRef]
- Svensson, P.; Lavigne, G. Clinical bruxism semantics beyond academic debates: Normo- and patho-bruxism as a new proposal. J. Oral Rehabil. 2020, 47, 547–548. [Google Scholar] [CrossRef]
- Vlăduțu, D.E.; Ionescu, M.; Mercuț, R.; Stănuși, A.; Boțilă, M.R.; Nardin, M.; Popa, D.A.; Popescu, M.A.; Ionescu, A.G.; Mercuț, V. Bruxism as a contraction disorder of the masticatory muscles—Review. Rom. J. Oral Rehabil. 2022, 14, 26–34. [Google Scholar]
- Saczuk, K.; Lapinska, B.; Wawrzynkiewicz, A.; Witkowska, A.; Arbildo-Vega, H.I.; Domarecka, M.; Lukomska-Szymanska, M. Temporomandibular Disorders, Bruxism, Perceived Stress, and Coping Strategies among Medical University Students in Times of Social Isolation during Outbreak of COVID-19 Pandemic. Healthcare 2022, 10, 740. [Google Scholar] [CrossRef] [PubMed]
- Boscato, N.; Exposto, F.; Nascimento, G.G.; Svensson, P.; Costa, Y.M. Is bruxism associated with changes in neural pathways? A systematic review and meta-analysis of clinical studies using neurophysiological techniques. Brain Imaging Behav. 2022, 16, 2268–2280. [Google Scholar] [CrossRef] [PubMed]
- Boscato, N.; Nascimento, G.G.; Leite, F.R.M.; Horta, B.L.; Svensson, P.; Demarco, F.F. Role of occlusal factors on probable bruxism and orofacial pain: Data from the 1982 Pelotas birth cohort study. J. Dent. 2021, 113, 103788. [Google Scholar] [CrossRef] [PubMed]
- Bulanda, S.; Ilczuk-Rypuła, D.; Nitecka-Buchta, A.; Nowak, Z.; Baron, S.; Postek-Stefańska, L. Sleep Bruxism in Children: Etiology, Diagnosis, and Treatment-A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 9544. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M.; Türp, J.C. Risk factors for bruxism. Swiss. Dent. J. 2018, 128, 118–124. [Google Scholar] [PubMed]
- Klasser, G.D.; Rei, N.; Lavigne, G.J. Sleep bruxism etiology: The evolution of a changing paradigm. J. Can. Dent. Assoc. 2015, 81, f2. [Google Scholar] [PubMed]
- Lavigne, G.J.; Kato, T.; Kolta, A.; Sessle, B.J. Neurobiological mechanisms involved in sleep bruxism. Crit. Rev. Oral Biol. Med. 2003, 14, 30–46. [Google Scholar] [CrossRef]
- Ramfjord, S.P. Bruxism, a clinical and electromyographic study. J. Am. Dent. Assoc. 1961, 62, 21–44. [Google Scholar] [CrossRef]
- Lal, S.J.; Weber, D.D.S.K.K. Bruxism Management; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Huang, Z.; Zhou, N.; Lobbezoo, F.; Almeida, F.R.; Cistulli, P.A.; Dieltjens, M.; Huynh, N.T.; Kato, T.; Lavigne, G.J.; Masse, J.F.; et al. Dental sleep-related conditions and the role of oral healthcare providers: A scoping review. Sleep Med. Rev. 2023, 67, 101721. [Google Scholar] [CrossRef]
- Vlăduțu, D.; Popescu, S.M.; Mercuț, R.; Ionescu, M.; Scrieciu, M.; Glodeanu, A.D.; Stănuși, A.; Rîcă, A.M.; Mercuț, V. Associations between Bruxism, Stress, and Manifestations of Temporomandibular Disorder in Young Students. Int. J. Environ. Res. Public Health 2022, 19, 5415. [Google Scholar] [CrossRef]
- Ribeiro-Lages, M.B.; Jural, L.A.; Magno, M.B.; Vicente-Gomila, J.; Ferreira, D.M.; Fonseca-Gonçalves, A.; Maia, L.C. A world panorama of bruxism in children and adolescents with emphasis on associated sleep features: A bibliometric analysis. J. Oral Rehabil. 2021, 48, 1271–1282. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lobbezoo, F. Sleep bruxism and temporomandibular disorders: A scoping review of the literature. J. Dent. 2021, 111, 103711. [Google Scholar] [CrossRef] [PubMed]
- Ohlmann, B.; Waldecker, M.; Leckel, M.; Bömicke, W.; Behnisch, R.; Rammelsberg, P.; Schmitter, M. Correlations between Sleep Bruxism and Temporomandibular Disorders. J. Clin. Med. 2020, 9, 611. [Google Scholar] [CrossRef] [PubMed]
- Smardz, J.; Martynowicz, H.; Michalek-Zrabkowska, M.; Wojakowska, A.; Mazur, G.; Winocur, E.; Wieckiewicz, M. Sleep Bruxism and Occurrence of Temporomandibular Disorders-Related Pain: A Polysomnographic Study. Front. Neurol. 2019, 10, 168. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, G.J.; Khoury, S.; Abe, S.; Yamaguchi, T.; Raphael, K. Bruxism physiology and pathology: An overview for clinicians. J. Oral Rehabil. 2008, 35, 476–494. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Naeije, M. Bruxism is mainly regulated centrally, not peripherally. J. Oral Rehabil. 2001, 28, 1085–1091. [Google Scholar] [CrossRef]
- Tsukiyama, Y.; Baba, K.; Clark, G.T. An evidence-based assessment of occlusal adjustment as a treatment for temporomandibular disorders. J. Prosthet. Dent. 2001, 86, 57–66. [Google Scholar] [CrossRef]
- Clark, G.T.; Tsukiyama, Y.; Baba, K.; Watanabe, T. Sixty-eight years of experimental occlusal interference studies: What have we learned? J. Prosthet. Dent. 1999, 82, 704–713. [Google Scholar] [CrossRef]
- Griffin, K.M. Mandibular adaptive reposturing: The etiology of a common and multifaceted autodestructive syndrome. Gen. Dent. 2003, 51, 62–67. [Google Scholar]
- Goldstein, G.; DeSantis, L.; Goodacre, C. Bruxism: Best Evidence Consensus Statement. J. Prosthodont. 2021, 30, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Beddis, H.; Pemberton, M.; Davies, S. Sleep bruxism: An overview for clinicians. Br. Dent. J. 2018, 225, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Cantini, E.; Romagnoli, M.; Bosco, M. Prevalence of bruxism in patients with different research diagnostic criteria for temporomandibular disorders (RDC/TMD) diagnoses. Cranio 2003, 21, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Vlăduțu, D.E.; Ionescu, M.; Mercuț, R.; Noveri, L.; Lăzărescu, G.; Popescu, S.M.; Scrieciu, M.; Manolea, H.O.; Iacov Crăițoiu, M.M.; Ionescu, A.G.; et al. Ecological Momentary Assessment of Masseter Muscle Activity in Patients with Bruxism. Int. J. Environ. Res. Public Health 2023, 20, 581. [Google Scholar] [CrossRef] [PubMed]
- Colonna, A.; Noveri, L.; Ferrari, M.; Bracci, A.; Manfredini, D. Electromyographic Assessment of Masseter Muscle Activity: A Proposal for a 24 h Recording Device with Preliminary Data. J. Clin. Med. 2023, 12, 247. [Google Scholar] [CrossRef] [PubMed]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 8th ed.; Elsevier, Inc.: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Gu, D.A.; Miao, L.Y.; Liu, C. Application of Digital Occlusion Analysis System in Stomatological Clinical Medicine. Austin. J. Dent. 2022, 9, 1164. [Google Scholar]
- Thanathornwong, B.; Suebnukarn, S. Clinical Decision Support Model to Predict Occlusal Force in Bruxism Patients. Healthc. Inform. Res. 2017, 23, 255–261. [Google Scholar] [CrossRef]
- Kuć, J.; Szarejko, K.D.; Aleksandrowicz, K.; Gołębiewska, M. The role of soft tissue mobilization in reducing orofacial and general complaints in a patient with Kimmerle anomaly and temporomandibular joint disorder: A case report. Cranio 2021, 39, 74–87. [Google Scholar] [CrossRef]
- Kerstein, R.B. Handbook of Research on Computerized Occlusal Analysis Technology Applications in Dental Medicine; IGI Global Publishers: Hershey, PA, USA, 2015. [Google Scholar]
- Devi, S.; Nallaswamy, D.; Venugopalan, S. Prosthetic Occlusal Analyzers—A Comprehensive Review. Int. J. Dent. Oral Sci. 2021, 8, 3550–3554. [Google Scholar]
- Popsor, S.; Albert, L.E.; Sabau, D.C.; Mihai, A. Occlusal features in depressive patients with craniomandibular disfunction. Int. J. Med. Dent. 2019, 23, 106–111. [Google Scholar]
- Popsor, S.; Szasz, O.; Șoaita, L.C.; Liana Georgiana Hănțoiu, L.G. Adjusting of a Stabilization Splint by the Use of T-Scan III—BioEMG Integrated System. Rom. J. Oral Rehabil. 2010, 2, 14–20. [Google Scholar]
- Komali, G.; Ignatius, A.V.; Srivani, G.S.; Anuja, K. T-scan system in the management of temporomandibular joint disorders—A review. J. Indian Acad. Oral Med. Radiol. 2019, 31, 252–256. [Google Scholar]
- Agbaje, J.O.; Casteele, E.V.; Salem, A.S.; Anumendem, D.; Shaheen, E.; Sun, Y.; Politis, C. Assessment of occlusion with the T-Scan system in patients undergoing orthognathic surgery. Sci. Rep. 2017, 7, 5356. [Google Scholar] [CrossRef] [PubMed]
- Kalachev, Y.S.; Michailov, T.A.; Iordanov, P.I. Study of occlusal-articulation relationships with the help of T-SCAN apparatus. Folia Med. 2001, 43, 88–91. [Google Scholar]
- Iacob, S.M.; Chisnoiu, A.M.; Objelean, A.; Fluerașu, M.I.; Moga, R.R.; Buduru, S.D. Correlation between bruxism, occlusal dysfunction and musculo-articular status. Rom. J. Oral Rehabil. 2022, 14, 48–55. [Google Scholar]
- Gümüş, H.Ö.; Kılınç, H.İ.; Tuna, S.H.; Ozcan, N. Computerized analysis of occlusal contacts in bruxism patients treated with occlusal splint therapy. J. Adv. Prosthodont. 2013, 5, 256–261. [Google Scholar] [CrossRef]
- Wieczorek, A.; Loster, J.; Loster, B.W. Relationship between occlusal force distribution and the activity of masseter and anterior temporalis muscles in asymptomatic young adults. Biomed. Res. Int. 2013, 2013, 354017. [Google Scholar] [CrossRef]
- Suvinen, T.I.; Kemppainen, P. Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J. Oral Rehabil. 2007, 34, 631–644. [Google Scholar] [CrossRef]
- Safari, A.; Jowkar, Z.; Farzin, M. Evaluation of the relationship between bruxism and premature occlusal contacts. J. Contemp. Dent. Pract. 2013, 14, 616–621. [Google Scholar] [CrossRef]
- Williamson, E.H.; Lundquist, D.O. Anterior guidance: Its effect on electromyographic activity of the temporal and masseter muscles. J. Prosthet. Dent. 1983, 49, 816–823. [Google Scholar] [CrossRef]
- Manfredini, D.; Landi, N.; Romagnoli, M.; Bosco, M. Psychic and occlusal factors in bruxers. Aust. Dent. J. 2004, 49, 84–89. [Google Scholar] [CrossRef]
- Manfredini, D.; Landi, N.; Tognini, F.; Montagnani, G.; Bosco, M. Occlusal features are not a reliable predictor of bruxism. Minerva Stomatol. 2004, 53, 231–239, (In English, Italian). [Google Scholar]
- Demir, A.; Uysal, T.; Guray, E.; Basciftci, F.A. The relationship between bruxism and occlusal factors among seven-to 19-year-old Turkish children. Angle Orthod. 2004, 74, 672–676. [Google Scholar] [PubMed]
- Goncalves, L.P.; Toledo, O.; Otero, S.M. The relationship between bruxism, occlusal factors and oral habits. Dent. Press J. Orthod. 2010, 15, 97–104. [Google Scholar]
- Cheng, H.J.; Chen, Y.Q.; Yu, C.H.; Shen, Y.Q. The influence of occlusion on the incidence of bruxism in 779 children in Shanghai. Shanghai Kou Qiang Yi Xue 2004, 13, 98–99. (In Chinese) [Google Scholar] [PubMed]
- Manfredini, D.; Winocur, E.; Guarda-Nardini, L.; Lobbezoo, F. Self-reported bruxism and temporomandibular disorders: Findings from two specialised centres. J. Oral Rehabil. 2012, 39, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Brocard, D.; Laluque, J.F.; Knellesen, C. La Gestion du Bruxisme; Quintessence Internațional: Paris, France, 2007. [Google Scholar]
- Matusz, K.; Maciejewska-Szaniec, Z.; Gredes, T.; Pobudek-Radzikowska, M.; Glapiński, M.; Górna, N.; Przystańska, A. Common therapeutic approaches in sleep and awake bruxism—An overview. Neurol. Neurochir. Pol. 2022, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Paesani, D.A. Bruxism Theory and Practice, 1st ed.; Quintessence Publishing: Chicago, IL, USA, 2010. [Google Scholar]
- Shopova, D.; Bozhkova, T.; Yordanova, S.; Yordanova, M. Case Report: Digital analysis of occlusion with T-Scan Novus in occlusal splint treatment for a patient with bruxism. F1000Research 2021, 10, 915. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Okamoto, M.; Nishigawa, G.; Oki, K.; Minagi, S. The design of non-occlusal intraoral appliances on hard palate and their effect on masseter muscle activity during sleep. Cranio 2007, 25, 8–15. [Google Scholar] [CrossRef] [PubMed]
| Study Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Participants (N/%) | Age Interval | Mean ± SD | Participants (N/%) | Age Interval | Mean ± SD | |
| Females | 15 (75%) | 20–29 | 24.2 ± 2.78 | 15 (75%) | 21–53 | 26.46 ± 7.82 |
| Males | 5 (25%) | 25–35 | 29 ± 4.24 | 5 (25%) | 26–47 | 35 ± 9.11 |
| Overall | 20 (100%) | 20–35 | 25.4 ± 3.74 | 20 (100%) | 21–53 | 28.6 ± 8.76 |
| Parameter | Study Group (n = 20) Mean ± SD | Control Group (n = 20) Mean ± SD | |
|---|---|---|---|
| BTI (%) | Awake BTI (ABTI) | 2.788 ± 2.381 | 0.722 ± 0.422 |
| Sleep BTI (SBTI) | 1.055 ± 0.790 | 0.233 ± 0.201 | |
| BWI (%) | Awake BWI (ABWI) | 1.178 ± 1.028 | 0.310 ± 0.214 |
| Sleep BWI (SBWI) | 0.471 ± 0.330 | 0.098 ± 0.085 | |
| BPI (%) | Awake BPI (ABPI) | 2.251 ± 1.926 | 0.585 ± 0.351 |
| Sleep BPI (SBPI) | 0.860 ± 0.633 | 0.188 ± 0.162 | |
| Subgroup (N) | Right Hemiarcade (%) | Left Hemiarcade (%) | |||
|---|---|---|---|---|---|
| Mean ± SD | p * | Mean ± SD | p * | ||
| Group | Study (20) | 57.080 ± 8.566 | 0.110 | 42.920 ± 8.566 | 0.110 |
| Control (20) | 52.505 ± 7.476 | 47.425 ± 7.463 | |||
| Gender | Females (30) | 55.856 ± 7.551 | 0.187 1 | 44.110 ± 7.533 | 0.198 1 |
| Males (10) | 51.600 ± 9.864 | 48.360 ± 9.854 | |||
| Subgroup (N) | Occlusion Duration in MI | Duration of Disocclusion from MI | |||
|---|---|---|---|---|---|
| Mean ± SD | p * | Mean ± SD | p * | ||
| Group | Study (20) | 1.030 ± 0.671 | 0.839 | 0.785 ± 0.444 | 0.925 |
| Control (20) | 0.968 ± 0.385 | 0.778 ± 0.418 | |||
| Gender | Females (30) | 0.999 ± 0.557 | 0.914 1 | 0.742 ± 0.407 | 0.450 1 |
| Males (10) | 1.000 ± 0.519 | 0.896 ± 0.481 | |||
| Parameter | Value | Study Group (N = 20) | Control Group (N = 20) | p * |
|---|---|---|---|---|
| Protrusion—the presence of the incisive guidance | Absent | 2 (10%) | 1 (5%) | 0.500 |
| Present | 18 (90%) | 19 (95%) | ||
| Protrusion—working side interference | No | 10 (50%) | 13 (65%) | 0.337 |
| Yes | 10 (50%) | 7 (35%) | ||
| Protrusion—non-working side interference | No | 8 (40%) | 13 (65%) | 0.113 |
| Yes | 12 (60%) | 7 (35%) | ||
| Protrusion—edge-to-edge—premature contacts on the working side | No | 14 (70%) | 14 (70%) | 1 |
| Yes | 6 (30%) | 6 (30%) | ||
| Protrusion—edge-to-edge— premature non-working side contacts | No | 17 (85%) | 14 (70%) | 0.225 |
| Yes | 3 (15%) | 6 (30%) |
| Parameter | Protrusion without Non-Working Interference (N = 21) | Protrusion with Non-Working Interference (N = 19) | p * |
|---|---|---|---|
| SBPI (%) | 0.378 ± 0.437 | 0.685 ± 0.660 | 0.044 1 |
| SBTI (%) | 0.461 ± 0.536 | 0.845 ± 0.821 | 0.044 1 |
| Number of “grinding” events per night | 16.760 ± 43.380 | 28.950 ± 35.442 | 0.014 1 |
| Occlusal Status | Distribution of Occlusal Forces on the Right Hemiarch (%) | Distribution of Occlusal Forces on the Left Hemiarch (%) | |||
|---|---|---|---|---|---|
| Mean ± SD | p * | Mean ± SD | p * | ||
| Protrusion—incisive guidance | Absent (N = 3) | 69.866 ± 0.814 | <0.0005 1 | 30.133 ± 0.814 | <0.0005 1,2 |
| Present (N = 37) | 53.570 ± 7.316 | 46.391 ± 7.304 | |||
| Protrusion—working interferences | No (N = 23) | 55.339 ± 6.621 | 0.763 | 44.617 ± 6.597 | 0.774 |
| Yes (N = 17) | 54.052 ± 10.261 | 45.923 ± 10.250 | |||
| Protrusion—non-working interferences | No (N = 21) | 52.333 ± 6.573 | 0.027 | 47.619 ± 6.569 | 0.025 2 |
| Yes (N = 19) | 57.510 ± 9.231 | 42.468 ± 9.212 | |||
| Parameter | Group (N) | Protrusion Duration | |
|---|---|---|---|
| Mean ± SD | p * | ||
| Protrusion—working interferences | No (23) | 2.39 ± 0.945 | 0.978 * |
| Yes (17) | 2.36 ± 0.805 | ||
| Protrusion—non-working interferences | No (21) | 2.31 ± 0.845 | 0.357 |
| Yes (19) | 2.45 ± 0.929 | ||
| Parameter | Group A | Group B | Group C | Group D | p * |
|---|---|---|---|---|---|
| The duration of the protrusion movement | 2.27 ± 0.953 | 2.62 1 ± 0.947 | 2.40 ± 0.547 | 2.33 ± 0.942 | 0.651 |
| SBTI | 0.48 ± 0.591 | 0.70 ± 0.448 | 0.40 ± 0.404 | 0.95 1 ± 1.023 | 0.253 |
| ABTI | 1.46 ± 1.407 | 2.67 1 ± 3.598 | 1.53 ± 1.270 | 1.59 ± 1.369 | 0.997 |
| SBPI | 0.39 ± 0.481 | 0.57 ± 0.367 | 0.33 ± 0.332 | 0.76 1 ± 0.819 | 0.253 |
| ABPI | 1.18 ± 1.132 | 2.15 1 ± 2.906 | 1.21 ± 0.995 | 1.30 ± 1.139 | 0.997 |
| Parameter | Guidance Type, The Presence of Interferences and Premature Contacts | Study Group (N = 20) | Control Group (N = 20) | p * |
|---|---|---|---|---|
| Left laterotrusion movement, guidance type | Canine | 10 (50%) | 18 (90%) | 0.018 1 |
| Antero-lateral group | 8 (40%) | 1 (5%) | ||
| Side group | 2 (10%) | 1 (5%) | ||
| Left laterotrusion movement, working side interferences | No | 4 (20%) | 8 (40%) | 0.168 |
| Yes | 16 (80%) | 12 (60%) | ||
| Left laterotrusion movement, non-working side interferences | No | 5 (25%) | 10 (50%) | 0.102 |
| Yes | 15 (75%) | 10 (50%) | ||
| Left laterotrusion movement, edge–edge position, premature working side contacts | No | 14 (70%) | 13 (65%) | 0.736 |
| Yes | 6 (30%) | 7 (35%) | ||
| Left laterotrusion movement, edge–edge position, premature non-working side contacts | No | 13 (65%) | 18 (90%) | 0.064 |
| Yes | 7 (35%) | 2 (10%) |
| Parameter | Canine Guidance (N = 28) | Antero-Lateral Group Guidance (N = 9) | Side Group Guidance (N = 3) | p * |
|---|---|---|---|---|
| ABPI | 1.043 ± 1.095 | 2.702 ± 2.439 | 1.057 ± 0.835 | 0.030 1 |
| Sleep duration | 30.657 ± 8.198 | 39.255 ± 6.172 | 31.266 ± 6.296 | 0.023 1 |
| Duration of wakefulness | 68.917 ± 8.631 | 60.744 ± 6.172 | 68.7333 ± 6.296 | 0.033 1 |
| The number of nighttime clenching events | 16.610 ± 13.356 | 45.440 ± 31.285 | 34.670 ± 24.007 | 0.015 1 |
| ABTI | 1.286 ± 1.348 | 3.360 ± 3.014 | 1.310 ± 1.013 | 0.027 1 |
| Parameter | Guidance Type, The Presence of Interferences and Premature Contacts | Study Group (N = 20) | Control Group (N = 20) | p * |
|---|---|---|---|---|
| Right laterotrusion movement, guidance type. | Canine | 12 (60%) | 15 (75%) | 0.587 |
| Antero-lateral group | 6 (30%) | 4 (20%) | ||
| Side group | 2 (10%) | 1 (5%) | ||
| Right side movement, working side interferences. | No | 8 (40%) | 7 (35%) | 0.744 |
| Yes | 12 (60%) | 13 (65%) | ||
| Right laterotrusion movement, non-working side interferences. | No | 5 (25%) | 10 (50%) | 0.102 |
| Yes | 15 (75%) | 10 (50%) | ||
| Right laterotrusion movement, edge–edge position—premature contacts on the working side | No | 13 (65%) | 14 (70%) | 0.736 |
| Yes | 7 (35%) | 6 (30%) | ||
| Right laterotrusion movement, edge–edge position—premature non-working side contacts | No | 12 (60%) | 14 (70%) | 0.507 |
| Yes | 8 (40%) | 6 (30%) |
| Parameter | Study Group (N = 20) | Control Group (N = 20) | p * |
|---|---|---|---|
| Duration of protrusion | 2.60 ± 0.98 | 2.16 ± 0.71 | 0.064 |
| Duration of right laterotrusion | 2.81 ± 0.80 | 2.26 ± 0.78 | 0.036 |
| Duration of left laterotrusion | 2.57 ± 0.87 | 2.21 ± 0.92 | 0.110 |
| Parameter | Duration (Value/p *) | ||||
|---|---|---|---|---|---|
| Occlusion MI | Disocclusion MI | Protrusion | Left Laterotrusion | Right Laterotrusion | |
| SBTI | −0.046/0.675 | −0.054/0.624 | 0.310/0.005 | 0.305/0.006 1 | 0.325/0.003 1 |
| ABTI | 0.018/0.870 | −0.023/0.834 | 0.095/0.388 | 0.113/0.305 | 0.162/0.142 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vlăduțu, D.E.; Ionescu, M.; Noveri, L.; Manolea, H.O.; Scrieciu, M.; Popescu, S.M.; Turcu, A.A.; Ştefârță, A.; Lăzărescu, G.; Mercuț, V. Aspects of Dental Occlusion Assessed with the T-Scan System among a Group of Romanian Dental Students in a Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 4877. https://doi.org/10.3390/ijerph20064877
Vlăduțu DE, Ionescu M, Noveri L, Manolea HO, Scrieciu M, Popescu SM, Turcu AA, Ştefârță A, Lăzărescu G, Mercuț V. Aspects of Dental Occlusion Assessed with the T-Scan System among a Group of Romanian Dental Students in a Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(6):4877. https://doi.org/10.3390/ijerph20064877
Chicago/Turabian StyleVlăduțu, Diana Elena, Mihaela Ionescu, Lorenzo Noveri, Horia Octavian Manolea, Monica Scrieciu, Sanda Mihaela Popescu, Adina Andreea Turcu, Alexandru Ştefârță, Grigore Lăzărescu, and Veronica Mercuț. 2023. "Aspects of Dental Occlusion Assessed with the T-Scan System among a Group of Romanian Dental Students in a Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 6: 4877. https://doi.org/10.3390/ijerph20064877
APA StyleVlăduțu, D. E., Ionescu, M., Noveri, L., Manolea, H. O., Scrieciu, M., Popescu, S. M., Turcu, A. A., Ştefârță, A., Lăzărescu, G., & Mercuț, V. (2023). Aspects of Dental Occlusion Assessed with the T-Scan System among a Group of Romanian Dental Students in a Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(6), 4877. https://doi.org/10.3390/ijerph20064877






