Development of an Online Mind–Body Physical Activity Intervention for Young Adults during COVID-19: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
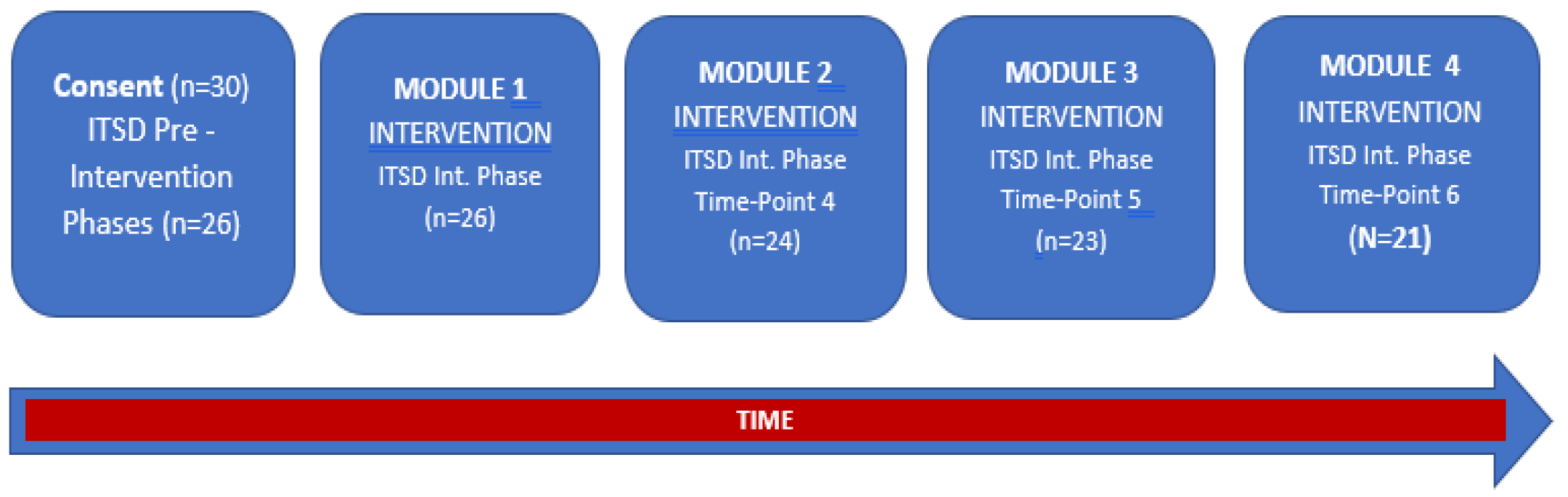
2.1. Study Protocol
2.2. Physical Activity Assessment
2.3. Assessment of Perceived Stress
2.4. Assessment of Well-Being
2.5. Description of Intervention
2.6. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Baseline Correlations
3.3. Multivariate Models
3.4. Univariate Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fairlie, R.; Loyalka, P. Schooling and Covid-19: Lessons from recent research on EdTech. Npj Sci. Learn. 2020, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Paltiel, A.D.; Zheng, A.; Walensky, R.P. Assessment of SARS-CoV-2 Screening Strategies to Permit the Safe Reopening of College Campuses in the United States. JAMA Netw. Open 2020, 3, e2016818. [Google Scholar] [CrossRef] [PubMed]
- Diamond, R.; Byrd, E. Standing up for health—Improving mental wellbeing during COVID-19 isolation by reducing sedentary behaviour. J. Affect. Disord. 2020, 277, 12312. [Google Scholar] [CrossRef] [PubMed]
- Grasdalsmoen, M.; Eriksen, H.R.; Lonning, K.J.; Sivertsen, B. Physical exercise, mental health problems, and suicide attempts in university students. BMC Psychiatry 2020, 20, 175. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Street, B.D. Metabolic Syndrome and Physical Activity Levels in College Students. Metab. Syndr. Relat. Disord. 2019, 17, 431–435. [Google Scholar] [CrossRef]
- Small, M.; Bailey-Davis, L.; Morgan, N.; Maggs, J. Changes in eating and physical activity behaviors across seven semesters of college: Living on or off campus matters. Health Educ. Behav. 2013, 40, 435–441. [Google Scholar] [CrossRef]
- Bai, Y.; Copeland, W.E.; Burns, R.D.; Nardone, H.; Devadanam, V.; Rettew, J.; Hudziak, J. Ecological momentary assessment of physical activity and wellness behaviors in college students throughout a school year: Longitudinal naturalistic study. JMIR Public Health Surveill. 2022, 8, e25375. [Google Scholar] [CrossRef]
- Van Dyck, D.; De Bourdeaudhuij, I.; Deliens, T.; Deforche, B. Can changes in psychosocial factors and residency explain the decrease in physical activity during the transition from high school to college or university? Int. J. Behav. Med. 2015, 22, 178–186. [Google Scholar] [CrossRef]
- Pfledderer, C.D.; Bai, Y.; Brusseau, T.A.; Burns, R.D.; King Jensen, J.L. Changes in college students’ health behaviors and substance use after a brief wellness intervention during COVID-19. Prev. Med. Rep. 2022, 26, 101743. [Google Scholar] [CrossRef]
- Brusseau, T.A.; Burns, R.D. Multicomponent school based physical activity interventions. In Handbook on Youth Physical Activity; Brusseau, T.A., Fairclough, S., Lubans, D., Eds.; Routledge: Abingdon, UK, 2020; pp. 557–576. [Google Scholar]
- Knapstad, M.; Sivertsen, B.; Knudsen, A.K.; Smith, O.R.F.; Aaro, L.E.; Lonning, K.J.; Skogen, J.C. Trends in self-reported psychological distress among college and university students from 2010 to 2018. Psychol. Med. 2021, 51, 470–478. [Google Scholar] [CrossRef]
- Powell, K.E.; King, A.C.; Buchner, D.M.; Campbell, W.W.; DiPietro, L.; Erickson, K.I.; Hillman, C.H.; Jakicic, J.M.; Janz, K.F.; Katzmarzyk, P.T.; et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J. Phys. Act. Health 2018, 16, 1–11. [Google Scholar] [CrossRef]
- Aldwin, C.M. Stress, Coping, and Development: An Integrative Perspective; Guilford Press: New York, NY, USA, 2007. [Google Scholar]
- Karyotaki, E.; Cuijpers, P.; Albor, Y.; Alonso, J.; Auerbach, R.P.; Bantjes, J.; Bruffaerts, R.; Ebert, D.D.; Hasking, P.; Kiekens, G.; et al. Sources of Stress and Their Associations with Mental Disorders among College Students: Results of the World Health Organization World Mental Health Surveys International College Student Initiative. Front. Psychol. 2020, 11, 1759. [Google Scholar] [CrossRef]
- Bigliassi, M. Psychological and Cardiovascular Effects of Meditation and Yoga. In Brain and Heart Dynamics; Govoni, S., Politi, P., Vanoli, E., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–8. [Google Scholar] [CrossRef]
- Kee, Y.H.; Li, C.; Kong, L.C.; Tang, C.J.; Chuang, K.L. Scoping review of mindfulness research: A topic modelling approach. Mindfulness 2019, 10, 1474–1488. [Google Scholar] [CrossRef]
- Schneider, J.; Malinowski, P.; Watson, P.M.; Lattimore, P. The role of mindfulness in physical activity: A systematic review. Obes. Rev. 2019, 20, 448–463. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-H.; Conroy, D.E. Mindfulness and physical activity: A systematic review and hierarchical model of mindfulness. Int. J. Sport Exerc. Psychol. 2020, 18, 794–817. [Google Scholar] [CrossRef]
- Wicker, P.; Frick, B. Intensity of physical activity and subjective well-being: An empirical analysis of the WHO recommendations. J. Public Health 2017, 39, e19–e26. [Google Scholar] [CrossRef]
- Kandola, A.; Lewis, G.; Osborn, D.P.J.; Stubbs, B.; Hayes, J.F. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: A prospective cohort study. Lancet Psychiatry 2020, 7, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.K.; Rosenbaum, S.; Loprinzi, P.D. Differential Experimental Effects of a Short Bout of Walking, Meditation, or Combination of Walking and Meditation on State Anxiety Among Young Adults. Am. J. Health Promot. 2018, 32, 949–958. [Google Scholar] [CrossRef]
- Salmoirago-Blotcher, E.; Druker, S.; Frisard, C.; Dunsiger, S.I.; Crawford, S.; Meleo-Meyer, F.; Bock, B.; Pbert, L. Integrating mindfulness training in school health education to promote healthy behaviors in adolescents: Feasibility and preliminary effects on exercise and dietary habits. Prev. Med. Rep. 2018, 9, 92–95. [Google Scholar] [CrossRef]
- Brems, C. Yoga as a Mind-Body Practice. In Nutrition, Fitness, and Mindfulness; Uribarri, J., Vassalotti, J.A., Eds.; Humana Press: Totowa, NJ, USA, 2020; pp. 137–155. [Google Scholar] [CrossRef]
- Erdogan Yuce, G.; Muz, G. Effect of yoga-based physical activity on perceived stress, anxiety, and quality of life in young adults. Perspect. Psychiatr. Care 2020, 56, 697–704. [Google Scholar] [CrossRef]
- Strehli, I.; Burns, R.D.; Bai, Y.; Ziegenfuss, D.H.; Block, M.E.; Brusseau, T.A. Mind-Body Physical Activity Interventions and Stress-Related Physiological Markers in Educational Settings: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 18, 224. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Liu, W.; McDonough, D.J.; Zeng, N.; Lee, J.E. The Dilemma of Analyzing Physical Activity and Sedentary Behavior with Wrist Accelerometer Data: Challenges and Opportunities. J. Clin. Med. 2021, 10, 5951. [Google Scholar] [CrossRef]
- Strehli, I.; Ziegenfuss, D.H.; Block, M.E.; Burns, R.D.; Bai, Y.; Brusseau, T.A. “I Felt Grounded and Clear-Headed”: Qualitative Exploration of a Mind-Body Physical Activity Intervention on Stress Among College Students During COVID-19. Inquiry 2022, 59, 469580221126307. [Google Scholar] [CrossRef] [PubMed]
- Ellis, K.; Kerr, J.; Godbole, S.; Lanckriet, G.; Wing, D.; Marshall, S. A random forest classifier for the prediction of energy expenditure and type of physical activity from wrist and hip accelerometers. Physiol. Meas. 2014, 35, 2191–2203. [Google Scholar] [CrossRef]
- Ozemek, C.; Kirschner, M.M.; Wilkerson, B.S.; Byun, W.; Kaminsky, L.A. Intermonitor reliability of the GT3X+ accelerometer at hip, wrist and ankle sites during activities of daily living. Physiol. Meas. 2014, 35, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, A.V.; Mirkes, E.M.; Yates, T.; Clemes, S.; Davies, M.; Khunti, K.; Edwardson, C.L. Accelerometer-assessed Physical Activity in Epidemiology: Are Monitors Equivalent? Med. Sci. Sports Exerc. 2018, 50, 257–265. [Google Scholar] [CrossRef]
- Scott, J.J.; Rowlands, A.V.; Cliff, D.P.; Morgan, P.J.; Plotnikoff, R.C.; Lubans, D.R. Comparability and feasibility of wrist- and hip-worn accelerometers in free-living adolescents. J. Sci. Med. Sport 2017, 20, 1101–1106. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Fuzeki, E.; Engeroff, T.; Banzer, W. Health Benefits of Light-Intensity Physical Activity: A Systematic Review of Accelerometer Data of the National Health and Nutrition Examination Survey (NHANES). Sports Med. 2017, 47, 1769–1793. [Google Scholar] [CrossRef]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef]
- Cain, K.L.; Sallis, J.F.; Conway, T.L.; Van Dyck, D.; Calhoon, L. Using accelerometers in youth physical activity studies: A review of methods. J. Phys. Act. Health 2013, 10, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Warttig, S.L.; Forshaw, M.J.; South, J.; White, A.K. New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). J. Health Psychol. 2013, 18, 1617–1628. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Ostergaard, S.D.; Sondergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Healy, S.; Colombo-Dougovito, A.; Judge, J.; Kwon, E.; Strehli, I.; Block, M.E. A practical guide to the development of an online course in adapted physical education. Palaestra 2017, 31, 48–54. [Google Scholar]
- Lamming, L.; Pears, S.; Mason, D.; Morton, K.; Bijker, M.; Sutton, S.; Hardeman, W. What do we know about brief interventions for physical activity that could be delivered in primary care consultations? A systematic review of reviews. Prev. Med. 2017, 99, 152–163. [Google Scholar] [CrossRef]
- Smyth, N.; Rossi, E.; Wood, C. Effectiveness of stress-relieving strategies in regulating patterns of cortisol secretion and promoting brain health. Int. Rev. Neurobiol. 2020, 150, 219–246. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Kraus, W.E.; Powell, K.E.; Campbell, W.W.; Janz, K.F.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Association between Bout Duration of Physical Activity and Health: Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1213–1219. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Sañudo, B.; Fennell, C.; Sánchez-Oliver, A.J. Objectively-Assessed Physical Activity, Sedentary Behavior, Smartphone Use, and Sleep Patterns Pre- and during-COVID-19 Quarantine in Young Adults from Spain. Sustainability 2020, 12, 5890. [Google Scholar] [CrossRef]
- López-Valenciano, A.; Suárez-Iglesias, D.; Sanchez-Lastra, M.A.; Ayán, C. Impact of COVID-19 Pandemic on University Students’ Physical Activity Levels: An Early Systematic Review. Front. Psychol. 2021, 11, 624567. [Google Scholar] [CrossRef] [PubMed]
- Romero-Blanco, C.; Rodríguez-Almagro, J.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Prado-Laguna, M.D.C.; Hernández-Martínez, A. Physical Activity and Sedentary Lifestyle in University Students: Changes during Confinement Due to the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6567. [Google Scholar] [CrossRef] [PubMed]
- Wasil, A.R.; Taylor, M.E.; Franzen, R.E.; Steinberg, J.S.; DeRubeis, R.J. Promoting Graduate Student Mental Health During COVID-19: Acceptability, Feasibility, and Perceived Utility of an Online Single-Session Intervention. Front. Psychol. 2021, 12, 569785. [Google Scholar] [CrossRef] [PubMed]
- Davidson, R.J.; McEwen, B.S. Social influences on neuroplasticity: Stress and interventions to promote well-being. Nat. Neurosci. 2012, 15, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, J. Neuroplasticity and Clinical Practice: Building Brain Power for Health. Front. Psychol. 2016, 7, 1118. [Google Scholar] [CrossRef]
- Kora, P.; Meenakshi, K.; Swaraja, K.; Rajani, A.; Raju, M.S. EEG based interpretation of human brain activity during yoga and meditation using machine learning: A systematic review. Complement. Ther. Clin. Pract. 2021, 43, 101329. [Google Scholar] [CrossRef]
- Van Loon, A.W.G.; Creemers, H.E.; Okorn, A.; Vogelaar, S.; Miers, A.C.; Saab, N.; Westenberg, P.M.; Asscher, J.J. The effects of school-based interventions on physiological stress in adolescents: A meta-analysis. Stress Health 2021, 38, 187–209. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Boulton, A.J.; Firestine, A.M.; Van Cappellen, P.; Algoe, S.B.; Brantley, M.M.; Kim, S.L.; Brantley, J.; Salzberg, S. Positive Emotion Correlates of Meditation Practice: A Comparison of Mindfulness Meditation and Loving-kindness Meditation. Mindfulness 2017, 8, 1623–1633. [Google Scholar] [CrossRef]
- Totzeck, C.; Teismann, T.; Hofmann, S.G.; von Brachel, R.; Pflug, V.; Wannemüller, A.; Margraf, J. Loving-kindness meditation promotes mental health in university students. Mindfulness 2020, 11, 1623–1631. [Google Scholar] [CrossRef]
| Characteristic | Mean ± SD or N (%) |
|---|---|
| Age (years) | 21.0 ± 2.2 |
| Height (m) | 1.7 ± 0.1 |
| Weight (kg) | 69.5 ± 17.5 |
| Body Mass Index (kg/m2) | 24.5 ± 4.5 |
| Sex | |
| Male | 4 (19%) |
| Female | 17 (81%) |
| Race/Ethnicity | |
| White | 17 (81%) |
| Hispanic or Latino | 2 (9%) |
| Black or African American | 1 (5%) |
| Asian or Pacific Islander | 1 (5%) |
| University Status | |
| Freshman | 5 (24%) |
| Sophomore | 4 (19%) |
| Junior | 6 (28%) |
| Senior | 5 (24%) |
| Graduate | 1 (5%) |
| Variable | Baseline (Mean ± SD) | Midpoint (Mean ± SD) | Postintervention (Mean ± SD) |
|---|---|---|---|
| Time in LPA (% of device wear time) | 15.0 ± 14.8 | 24.9 ± 16.3 ** | 26.3 ± 16.3 ** |
| Time in MVPA (% of device wear time) | 3.9 ± 3.9 | 7.3 ± 5.0 *** | 6.8 ± 5.1 *** |
| Variable | Timepoint 1 (Mean ± SD) | Timepoint 2 (Mean ± SD) | Timepoint 3 (Mean ± SD) | Timepoint 4 (Mean ± SD) | Timepoint 5 (Mean ± SD) | Timepoint 6 (Mean ± SD) |
|---|---|---|---|---|---|---|
| Stress (PSS-4) | 6.55 ± 2.61 | 6.71 ± 2.36 | 6.81 ± 2.67 | 5.81 ± 2.29 | 5.76 ± 3.17 | 6.00 ± 3.22 |
| Well-Being (WHO-5) | 14.05 ± 3.79 | 14.23 ± 3.76 | 13.95 ± 4.11 | 15.57 ± 3.82 | 15.66 ± 4.84 | 14.10 ± 5.69 |
| LPA | MVPA | Stress | Well-being | |
|---|---|---|---|---|
| LPA | 1 | |||
| MVPA | 0.86 *** | 1 | ||
| Stress | −0.52 * | 0.41 | 1 | |
| Well-being | −0.44 | -0.39 | −0.52 * | 1 |
| Outcome | Source | Sum of Squares | Degrees of Freedom | Mean Square | F-Statistic |
|---|---|---|---|---|---|
| Time in LPA (% of wear time) | Sex | 346.1 | 1 | 346.1 | 0.51 |
| Time | 741.1 | 2 | 379.8 | 6.43 ** | |
| Sex × Time | 13.5 | 2 | 6.7 | 0.12 | |
| Time in MVPA (% of wear time) | Sex | 132.5. | 1 | 132.5 | 0.53 |
| Time | 86.7 | 2 | 43.4 | 8.12 ** | |
| Sex × Time | 1.3 | 2 | 0.6 | 0.12 | |
| Stress | Sex | 5.96 | 1 | 5.96 | 0.23 |
| Time | 18.68 | 5 | 3.73 | 0.88 | |
| Sex × Time | 12.20 | 5 | 2.44 | 0.72 | |
| Well-being | Sex | 83.7 | 1 | 83.7 | 1.22 |
| Time | 29 | 5 | 5.74 | 0.63 | |
| Sex × Time | 15 | 5 | 3.06 | 0.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strehli, I.; Burns, R.D.; Bai, Y.; Ziegenfuss, D.H.; Block, M.E.; Brusseau, T.A. Development of an Online Mind–Body Physical Activity Intervention for Young Adults during COVID-19: A Pilot Study. Int. J. Environ. Res. Public Health 2023, 20, 4562. https://doi.org/10.3390/ijerph20054562
Strehli I, Burns RD, Bai Y, Ziegenfuss DH, Block ME, Brusseau TA. Development of an Online Mind–Body Physical Activity Intervention for Young Adults during COVID-19: A Pilot Study. International Journal of Environmental Research and Public Health. 2023; 20(5):4562. https://doi.org/10.3390/ijerph20054562
Chicago/Turabian StyleStrehli, Ildiko, Ryan D. Burns, Yang Bai, Donna H. Ziegenfuss, Martin E. Block, and Timothy A. Brusseau. 2023. "Development of an Online Mind–Body Physical Activity Intervention for Young Adults during COVID-19: A Pilot Study" International Journal of Environmental Research and Public Health 20, no. 5: 4562. https://doi.org/10.3390/ijerph20054562
APA StyleStrehli, I., Burns, R. D., Bai, Y., Ziegenfuss, D. H., Block, M. E., & Brusseau, T. A. (2023). Development of an Online Mind–Body Physical Activity Intervention for Young Adults during COVID-19: A Pilot Study. International Journal of Environmental Research and Public Health, 20(5), 4562. https://doi.org/10.3390/ijerph20054562










