Abstract
Background: Social support and Quality of life (QoL) are important aspects of life and should be explored during the specific scenario of the pandemic. Aims: (i) to compare the perceived social support (PSS) in caregivers and the domains of QoL of the caregiver and the child with developmental disabilities (DD) and typical development (TD); (ii) to verify the existence of the association, in each group, between the PSS, and the domain of QoL of the caregiver and the child. Methods and Procedures: 52 caregivers of children with DD and 34 with TD participated remotely. We assessed PSS (Social Support Scale), children’s QoL (PedsQL-4.0-parent proxy) and caregivers’ QoL (PedsQL-Family Impact Module). The groups were compared for the outcomes using the Mann–Whitney test, and Spearman’s test evaluated the correlation between the PSS and the QoL (child and caregiver) in each of the groups. Outcomes and Results: There was no difference between groups for PSS. Children with DD presented lower values in PedsQL total, psychosocial health, physical health, social activities, and school activity. Caregivers of children with TD presented lower values in PedsQL family total, physical capacity, emotional aspect, social aspect, daily activities, and higher value in communication. In the DD group, we found a positive relationship between PSS with child: Psychosocial Health (r = 0.350) and Emotional Aspect (r = 0.380), and with family: Total (r = 0.562), Physical Capacity (r = 0.402), Emotional Aspect (r = 0.492), Social Aspect (r = 0.606), Communication (r = 0.535), Concern (r = 0.303), Daily Activities (r = 0.394) and Family Relationships (r = 0.369). In the TD group, we found that PSS was positively associated with Family: Social Aspect (r = 0.472) and Communication (r = 0.431). Conclusions and Implications: During the COVID-19 pandemic, despite both groups presenting similar PSS, there are important differences in QoL between them. For both groups, greater levels of perceived social support are associated with greater caregiver-reported in some domains of the child’s and caregiver’s QoL. These associations are more numerous, especially for the families of children with DD. This study provides a unique view into the relationships between perceived social support and QoL during the “natural experiment” of living through a pandemic.
1. Introduction
Primary home care of a child with developmental disabilities (DD) usually requires changes in the physical, psychological and social spheres of the family, resulting in higher physical, emotional, and even financial burdens compared to parents of children with typical development (TD). It can lead to chronic stress and trigger physical and psychological disorders for the caregiver, which may reflect on their and the child’s quality of life (QoL) [1,2].
Although caring for a child with DD can have positive effects on parents’ lives, such as personal growth, family unity and proximity, and greater sensitivity and tolerance towards diversity [3], several factors can be stressors inherent in the care and the routine. We highlight the loss of support of people and social stigma [4], changes in the routine of daily life with social restrictions [5], stress [6] and concerns about the health and development of the child [7]. Because of these greater demands, these families often need social support [8].
Social support is defined as the perceived availability or momentary level of receipt of social contacts to fulfill specific functions [9], and it is an important indicator of social relationships [10]. There are two forms of social support: informal, provided by family, friends, and other close people, and formal, provided by professionals, social, and health institutions [11]. In addition, formal or informal social support can promote and be related to health since it incentivizes health behaviors [12].
An important context that changed social relationships and people’s lives around the world was the COVID-19 pandemic [13,14]. In Brazil, while creating strategies against the pandemic, services such as schools, healthcare centers, and leisure and recreation centers were closed, in addition to prohibiting access to places and events that promoted overcrowding [15]. In this way, this new scenario of life drastically changed a family’s routine, from declines in their child’s motor, behavior, social, and communication skills to changes in therapy services [16]. Therefore, the perceived social support and the QoL gain even more attention in this context and should be explored.
Studies published before the pandemic have shown that health-related social support and QoL are positively associated in groups of parents of children with congenital malformations [17] and that the perceived social support of caregivers is related to fewer depressive symptoms [18]. One study reported that a high level of social support is related to a lower incidence of depression and parental stress in parents of children with cerebral palsy [19]. Also, receiving social support has a strong association with the family’s quality of life [20]. The importance of this relationship for the families of children with DD is remarkable.
Considering the specific context of the COVID-19 pandemic, there are studies indicating that caregivers of children with special healthcare needs received inadequate social support during the second wave of COVID-19 [21]. A qualitative study showed that informal support was an important factor for caregiving demands and resources for coping, according to parents of children with intellectual disabilities [22]. Also, the pandemic limited access to social support and services, impacting the mental health of children with disabilities and their parents [23,24,25].
Studies addressing the pandemic period have shown that caregiver concerns for the child are associated with caregivers’ symptoms of stress, depression, anxiety and behavioral and emotional deterioration during the lockdown [26,27,28,29]. In addition, studies have indicated an increase in demands on caregivers of children and youth with autism during the pandemic globally [23] and a greater burden of care for mothers who have a handicapped child [30]. A qualitative study of people with autism and caregivers of people with autism identified that the pandemic was related to mental health problems and a lack of access to support [31]. Although studies indicate negative aspects of the pandemic on the health of caregivers of children with disabilities, we did not find studies that evaluated the quality of life, addressing the physical functioning, emotional functioning, social functioning, and functioning in school domains, comparing children with DD and TD. This represents a gap in the literature during the COVID-19 pandemic.
Therefore, our study proposes to evaluate these aspects during the pandemic for several domains related to QoL, aiming to identify in which QoL domains this correlation exists and to allow the identification of more specific areas for evaluations and interventions focused on the family since the pandemic is a potential aggravator of these aspects.
The objectives of this study were, during the COVID-19 pandemic, (i) to compare the perceived social support in caregivers and the QoL in the domains of psychosocial, physical, emotional, social and schools activities of the caregiver and the child with developmental disabilities (DD) and typical development (TD), and (ii) to verify the existence of associations, in each group, between the perceived social support, and the QoL of the caregiver and the child, in the domains of psychosocial, physical, emotional, social and schools activities.
Taking into account other studies previous to the pandemic related to perceived social support and quality of life comparing groups with DD and TD, as well as the changes that the pandemic has brought about in an abrupt and unprecedented way, we expect to find that the perceived social support will be similar in both groups since the challenges of pandemic occurred in all people, and the difficulties in obtaining social support were not a function of having an impairment, but due to the mandated physical distancing. For the QoL, we expect that the DD group (children and caregivers) will show lower QoL when compared to the TD group since the pandemic might exacerbate the challenges for this group. Also, it is expected that greater social support will be associated with a higher quality of life for the caregiver and the child, especially in the group with DD, since caregivers and children with DD often need more social support [8] (Araújo et al., 2016) and the social support and QoL showed to be associated before pandemic [17] (Silva et al., 2020). These results will contribute to a better understanding of these aspects during the pandemic.
2. Methods
2.1. Study Design
This is an observational study with a cross-sectional design and a convenience sample, which followed STROBE guidelines [32], as well as the recommendations of the Check-list for Reporting Results of Internet E-Surveys (CHERRIES) statement guideline. It was approved by the Ethics Committee on Research in Human Beings of the Federal University of São Carlos (protocol number: 42344221.0.0000.5504).
2.2. Sample Calculation
The sample size was determined a priori using the software GPower (Version 3.1.3, University Düsseldorf, Düsseldorf, Germany). Based on the study by Varni et al. (2004) [33], considering the PedsQL Total as an outcome variable, the means of the healthy group and those with some health condition being 87.61 and 74.22, respectively. Thus, an effect size of 0.86 was obtained, and a test power of 90% and significance of 0.05 was used, which resulted in 30 children in each group.
2.3. Participants
Fifty-two caregivers of children aged 5–12 years with DD (n = 52) and TD (n = 34) took part in the study. We performed remote data collection, so we could evaluate participants from all geographic regions of Brazil. Recruitment occurred by dissemination of the research through social media.
To respond to the survey, participants should be the main caregiver of a child with or without DD and need to agree and virtually sign the Informed Consent Form (ICF). The reported diagnoses of children with DD included cerebral palsy, Down syndrome, myelomeningocele, congenital malformations, and Autism Spectrum Disorder, among others, as shown by the flowchart in Figure 1.
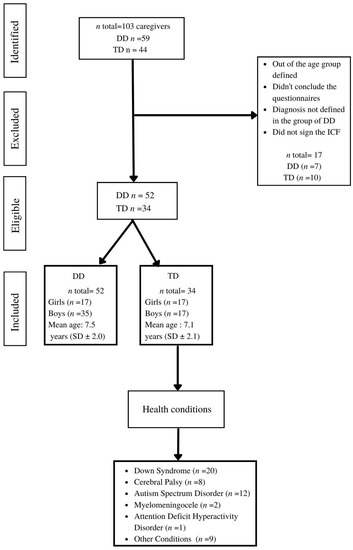
Figure 1.
Flowchart of the participants. Legend: n = number of participants; DD = developmental disabilities; TD = typical development; SD = standard deviation; ICF = Informed Consent Form.
2.4. Procedures
The participants were recruited through dissemination on social networks, Facebook and Instagram, radio, and email networks, carried out by the communication department of the university in which the study was developed. Data was collected through online Google® forms, between March 2020 and April 2021, at the height of the COVID-19 global pandemic. The results were sent directly to a password-protected Google Drive® of the researchers.
2.5. Measures
2.5.1. Social Support Scale
The Social Support Scale (SSS) was used to evaluate the perceived social support during the pandemic period of the caregivers from both groups, TD and DD. SSS is translated and validated for Brazilians, presenting high internal consistency in all its domains [34]. SSS encompasses 19 items that assess 3 domains of social support: emotional, material, and affective/interaction. For each of these items, on a 5-point scale from “never” (score 1); “rarely” (score 2); “sometimes” (score 3); “almost always” (score 4); to “always” (score 5), participants respond to how much they consider that they have that particular social support described [34]. Adding the scores for each item, the higher the gross score, the greater the perceived social support received by the respondent.
2.5.2. Pediatric Quality of Life Inventory (PedsQL) Version 4.0, Parent Proxy
PedsQL is a translated, adapted and valid instrument to measure Health-Related Quality of Life (HRQoL) in Brazilians [35], i.e., QoL related to the health of the individual [33]. Since this instrument is a parent proxy, it can be used in caregivers of children and adolescents aged 2 to 18 years, healthy or with any type of health condition. PedsQL is composed of 23 items divided into 4 different dimensions: physical functioning (8 items); emotional functioning (5 items); social functioning (5 items); and functioning in school (5 items). Items are scored as 0) it never constitutes a problem; (1) it is almost never a problem; (2) sometimes it is a problem; (3) it is often a problem; (4) it is almost always a problem. Although scores vary from 0–4, the final score is converted afterward into a scale of 0 to 100 and follows a decreasing pattern, i.e., the option “never” scores 100 and “almost always” scores 0.
The results can be reported in 3 ways: (a) the sum of both categories (total score of 23 items); (b) results addressing physical health (8 items); (c) results addressing psychosocial health (15 items). To achieve the total final score and domains’ scores separately, each item’s score is converted into a scale from 0 to 100, and then the scores of all items were summed and divided by the number of items [35]. To create the psychosocial health summary score, the mean is computed as the sum of the items over the number of items answered in the emotional, social, and school functioning scales. The physical health summary score is the same as the physical functioning Scale Score. Its completion takes approximately 5 min [36]. For statistical analysis, the total converted scores, physical health, and psychosocial health scores were used, and the higher the score, the better the reported QoL.
2.5.3. PedsQL Family Impact Module (PedsQL-FIM)
PedsQL-FIM evaluates the impact of chronic pediatric health conditions on parents and families. It was translated, adapted and validated for Brazilians [37]. The instrument has 36 items divided into 6 subscales that measure the functioning reported by parents in relation to their: Physical Functioning (6 items); Emotional functioning (5 items); Social Functioning (4 items); Cognitive functioning (5 items); Communication (3 items) and Concern (5 items). In addition to these 6 subscales, there are 2 more that assess caregiver functioning by the parents’ report: Daily Activities (3 items) and Family Relationship (5 items). Its completion takes, on average, 5 min. As well as in PedsQL, each item is scored from 0 to 4, and final scores are converted to a scale from 0 to 100, as occurs in PedsQL v.4.0 described in the item above [33].
The total final score is obtained by adding the converted points of each of the 36 items and dividing the sum by the number of items answered. This score was used in statistical analysis. In the case of subscores, the scores are obtained from the exclusive sum of the specific questions of each domain. The time to complete is approximately 5 min. In all cases, the final score indicates that the more points, the lower the negative impact on the life of this family member [37].
2.6. Statistical Analysis
Shapiro-Wilk test revealed the non-normality of the data. Therefore, the Mann–Whitney test compared measures between DD and TD groups. The compared measures were: (a) perceived social support; (b) Family QoL (Total PedsQL Family; PedsQL Physical Ability; PedsQL Emotional Aspect; PedsQL Social Aspect; PedsQL Mental Capacity; PedsQL Communication; PedsQL Concern; PedsQL Everyday Activities; PedsQL Family Relationships); and (c) child’s QoL by the parents’ report (Total PedsQL; PedsQL Psychosocial Health; PedsQL Physical Health; PedsQL Emotional Aspect; PedsQL Social Activities; PedsQL School activity).
Spearman’s correlation tested the association between perceived social support and QoL scores (child and caregiver) in each of the groups. Correlations were classified according to the Cohen and Holliday classification (1982) [38]: up to 0.19: very weak; between 0.20 and 0.39: weak; from 0.40 to 0.69: moderate; from 0.70 to 0.89: strong; and from 0.90 to 1: very strong). For all analyses, a significance level of 5% was adopted.
3. Results
3.1. Participants
Table 1 illustrates the characteristics of the sample considering groups with TD and DD, regarding sex (female vs. male) and age (years) for children and their caregivers, caregiver situation about work (work in person, work in a home office, do not work), maternal schooling (which increasingly categorizes: Incomplete Elementary, Complete Elementary, Incomplete high school, Complete high school, Incomplete Higher Education, Complete Higher Education), and socioeconomic classification (according to the Brazilian Economic Classification—ABEP (D–E, C1, C2, B1, B2, and A). ABEP addresses socioeconomic aspects based on the number of basic items in one’s house, educational level, availability of running water and paved street to the residence.

Table 1.
Characteristics of the sample of children with DD and TD and test of the difference between groups.
3.2. Comparison between Groups (DD × TD)
We did not find significant differences in perceived social support between the groups during the pandemic period. Regarding QoL, the children in the DD group presented significantly lower scores than the children with TD in the QoL variables of the Total PedsQL child; PedsQL Psychosocial Health; PedsQL Physical Health; PedsQL Social Activities; PedsQL School Activity; and in the QoL of the PedsQL Family Communication. Differently, children with DD presented higher scores in the variables Total PedsQL Family; PedsQL Family Physical Capacity; PedsQL Family Emotional Aspect; PedsQL Family Social Aspect; and PedsQL Family Daily Activities when compared to the TD. The results of the comparison are found in Table 2 and Table 3.

Table 2.
Comparison between the children with DD and TD for the children’s QoL variables.

Table 3.
Comparison between the children with DD and TD for perceived social support and caregivers’ QoL.
3.3. Correlation Analysis
For the DD group, we found significant correlations between perceived social support and the variables: PedsQL Child Psychosocial Health; PedsQL Child Emotional Aspect; PedsQL Family; PedsQL Family Physical Ability; PedsQL Family Emotional Aspect; PedsQL Family Social Aspect; PedsQL Family Communication; PedsQL Family Concern; PedsQL Family Everyday Activities and PedsQL Family Family Relationships.
For the TD group, significant correlations were found between perceived social support and the variables: PedsQL Family Social Aspect and PedsQL Family Communication. Table 4 illustrates the correlation results within the TD group and the DD group and shows the classification of significant correlations according to Cohen and Holliday (1982) [38].

Table 4.
Correlation between perceived social support with caregiver’s QoL and child’s QoL for the children with DD and TD and their caregivers.
4. Discussion
Our study aimed to compare the perceived social support in caregivers and the QoL in the domains of psychosocial, physical, emotional, social, and school activities of the caregiver and the child with DD and TD in a peculiar scenario of the COVID-19 pandemic. Moreover, for each of these groups, we tested the association between the perceived social support and QoL of children and their caregivers.
4.1. Perceived Social Support and Quality of Life
According to our initial expectations, we did not find significant differences in perceived social support between the groups. The reduced levels of social support experienced by families with children presenting DD are well documented in the literature [39,40]. However, during the pandemic, the discrepancies in relation to the availability of social support usually experienced by families of children with DD compared to families of children with TD did not happen. Possibly, due to the scenario of social isolation and restriction of interactions, families of typical children had a reduction in the social support they normally received from others. In turn, parents of children with DD already experience situations of limited social support, mainly restrictions on support from the government and schools [41]. We believe that these limitations remained, which explains the similarity in the results of the two groups.
The assessment of QoL regarding the children resulted in lower values of total QoL, psychosocial health, physical health, social activities, school activities and family communication for children with DD. Previous studies have reported lower QoL scores for children with DD [42,43]. The presence of some physical, motor or cognitive disorder in the child’s development may restrict access to opportunities for activities, recreation, and participation in various life contexts, consequently impacting their QoL [44,45,46]. During the pandemic, these characteristics remained, and the children kept showing reduced levels of physical and psychological health than their typical peers. In addition, the socioeconomic strata of our sample might have contributed to our results. There is a prevalence of lower socioeconomic levels for participants in the DD group. More than 50 percent of the caregivers are part of the socio-economic strata C1–C2 and D–E, which represent, respectively, middle and lower class). Otherwise, caregivers in the TD group are concentrated in classes A, B1 and B2, which represent higher socioeconomic strata. In fact, for children, a caregiver’s socioeconomic level might favor QoL since parents with greater purchasing power would be expected to be able to provide their kids with diverse and enriching experiences, especially related to fun. According to previous studies, a higher socioeconomic stratum can provide better treatment options, complementary therapies, and home adaptations and improve daily life [47,48], which might positively affect the child’s physical and psychosocial QoL, by granting greater comfort related to health and social interactions [49].
Still, regarding QoL, some results were not in accordance with our initial hypotheses. In this unprecedented pandemic scenario, we surprisingly found better caregiver QoL for physical capacity, emotional aspects, social aspects, daily activities, and in Total PedsQL Family for caregivers of children with DD compared to TD. These results may be associated with the peculiarities of the COVID-19 scenario. This is a very interesting result since, based on previously published studies [50,51,52], we initially expected to find a higher QoL for caregivers of the TD group, assuming that these caregivers do not have to deal with the challenges of raising a child with impairments. Nevertheless, our results pointed in the opposite direction. All around the world, families had to deal with the new and unexpected. In a qualitative study addressing mothers of children with multiple health conditions, Pozniak and Kraus de Camargo (2021) [53] reported that COVID-19 had forced society to adopt measures that benefit these caregivers, such as virtual services, supports, and community-building opportunities. These factors might have contributed to determining higher values of QoL for caregivers of children with DD since, for the very first time, these caregivers could participate in activities that they were not able to do before.
Other aspects might have also contributed to our results. Caregivers of children with TD possibly did not present such a high demand for full-time home care. Moreover, concerning the work situation of the caregivers, it was noticed that in the DD group, more than half of the sample was not working in that period, thus being able to devote themselves to the care of the children. While in the TD group, 91.1% of caregivers were working during the pandemic and, thus, had to conciliate their employment with the care of children at home and in remote education. Accordingly, the pandemic context, with the adoption of the remote teaching model for the child [54], may have contributed to caregivers of children with TD exhibiting lower QoL levels compared to the group of DD caregivers.
4.2. Relationship between Perceived Social Support and Quality of Life of the Child and Their Caregivers
For both groups, we found that greater perceived social support was associated with QoL. Nevertheless, for the group of children with DD, these associations were greater than in the group of children with TD.
The association between social support and quality of life is not a new idea in the literature. Fisher et al. (2022) [55] pointed out social support as a mediator of reduced stress and higher levels of life satisfaction. Accordingly, the availability of perceived social support seems to be directly linked to the greater opportunity for the caregiver to be in contact with friends [56] and have these people share their insecurity, uncertainties, and daily tasks. Previous studies reported similar results for other populations reporting that higher levels of social support were associated with better caregivers’ and children’s mental health [21].
Nevertheless, our results show us a very interesting point. It seems that the availability of perceived social support shows greater relevance for caregivers’ QoL than for children’s QoL. From these results, we can infer that greater levels of social support might help parents to deal with the challenge of raising their child, contributing to greater levels of caregiver QoL. Previous studies observed a positive relationship between perceived social support and parents’ QoL in families of children with DD [8]. Thus, it can be understood that parents who perceive the availability of social support usually show better QoL, which might contribute to improving their children’s well-being with emotional, social, and educational support even in a pandemic period. Caregivers of children with DD tend to be tired and can be frustrated and anxious [57]. Nevertheless, the support network can reduce the burden on these caregivers [58] because they can share their concerns and anxieties and receive help in daily activities, including the child’s home care.
It is also worth mentioning how perceived social support was much more related to the quality of life for caregivers of children with DD than for those with TD. In fact, the daily demands involved with raising a child with medical conditions are greater than the ones involved with raising typical children [59]. Therefore, for caregivers of children with DD, perceived social support seems to be more important than for caregivers with typical children since any available support has the potential to reduce the daily workload involved in raising these children. These results show us that even in a critical period, such as the pandemic, in which due to social distancing, interpersonal relationships may have been restricted in determining similar levels of social support for caregivers of children with DD.
5. Clinical Implications
The main clinical implications of our study come from our intriguing results. The peculiar features of social distancing and interruption of face-to-face activities seem to have changed the perceived social support for all families. Moreover, during the pandemic period, the unexpected finding of greater caregiver QoL levels for the DD group showed not only the resilience of these caregivers but also how much the perception and assessment of the quality of life in the face of a specific situation (e.g., COVID-19 pandemic. As mentioned by Pozniak and Kraus de Camargo (2021) [53], the silver lining of COVID-19 may be that it presents an opportunity to rethink existing social arrangements and rebuild a more equitable post-pandemic society.
Results point out also that even in this unprecedented scenario, the association between the perceived social support and quality of life of children with DD and their caregivers was clear. This association was especially evident for the caregiver’s QoL.
These results, obtained during a pandemic period, applied to a post-pandemic scenario, show how much the availability of social support for families of children with DD is relevant. Rehabilitation professionals providing family-centered therapy need to empower caregivers in the search for solid support networks which would contribute to higher levels of QoL. Future studies should investigate the main determinants of children’s QoL, ideally assessed directly instead of by proxy, in order to understand how to best improve it.
Considering we are now in a period where many of the previous restrictions have been lifted, it is important to keep attention on these aspects to enable the creation of strategies that favor improvements in QoL of the population, in general, but especially of children with DD and their caregivers.
6. Study Strengths and Limitations
Among the main limitations of our study, we may cite the assessment of children’s QoL by means of their parents’ reports. It is known that the reported QoL by parents might be lower than the reports provided by the children themselves [60]. Nevertheless, considering the pandemic scenario, which had allowed us to assess our participants remotely, a parents’ report was the best way we found to conduct the remote surveys. Another limitation was the absence of pre-pandemic data regarding children’s and caregivers’ social support and QoL, which would have provided us with the possibility to investigate COVID-19’s impact. Further data collection in a current post-pandemic scenario with a follow-up study would clarify to us the way families have been resuming their social support networks and the impact of this on their QoL and the QoL of their children.
A strength of the study is that it provides a unique view into the relationships between perceived social support and QoL during the “natural experiment” of living through a pandemic.
7. Conclusions
During the COVID-19 pandemic, the perceived level of social support for caregivers of children with DD and TD was similar, possibly reflecting social distancing effects. For children with DD, the caregiver-reported level of QoL in physical, psychosocial, and social activities was lower than in children with TD. Nevertheless, for their caregivers, the QoL levels were greater than the ones in the TD group. Finally, for both groups, greater levels of perceived social support were associated with greater caregiver-reported QoL of the child in the psychosocial domain and the caregiver, especially in the aspects of physical, emotional, social capacity, communication, concern, daily activities, and family relationships. These associations were more numerous, especially for the families of children with DD.
Author Contributions
Conceptualization, I.G.R.D.C., B.H.B. and N.A.C.F.R.; methodology, I.G.R.D.C., B.H.B., L.F. and N.A.C.F.R.; software, I.G.R.D.C. and B.H.B.; validation, I.G.R.D.C., B.H.B. and N.A.C.F.R. formal analysis, C.R.G.L.; investigation, I.G.R.D.C.; resources, I.G.R.D.C., B.H.B. and N.A.C.F.R.; data curation, I.G.R.D.C. and B.H.B.; writing—original draft preparation, I.G.R.D.C., B.H.B., C.R.G.L., O.K.d.C., L.F., S.L.P. and N.A.C.F.R.; writing—review and editing, I.G.R.D.C., B.H.B., C.R.G.L., O.K.d.C., S.L.P. and N.A.C.F.R.; visualization, I.G.R.D.C.; supervision, N.A.C.F.R.; project administration, N.A.C.F.R.; funding acquisition, I.G.R.D.C., B.H.B. and N.A.C.F.R. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Brazilian National Council for Scientific and Technological Development (CNPQ) [process number: 128495/2020-0], São Paulo Research Foundation (FAPESP) [processes number: 2017/11259-6, 2019/13570-6, 2019/13716-0, 2021/15016-6] and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Federal University of São Carlos (UFSCar) (protocol code 42344221.0.0000.5504).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset supporting the conclusion of this article is available from the authors upon reasonable request.
Acknowledgments
We are grateful to the families that participated in the study, CNPQ, FAPESP and CAPES for the financial support and the Brazilian institutes Amor pra Down, Mano Down, Avança Down, Amigos Especiais de Limeira (AEL), Associação de Reabilitação Infantil Limeirense (ARIL), Associação de Pais e Amigos dos Excepcionais (Apae), Casa da Criança Paralítica de Campinas and the Centro Municipal de Atendimento Educacional Especializado (CMAEE) de Piraquara (Paraná) and the school Professor Antônio Perches Loredello for the support and research disclosure.
Conflicts of Interest
The authors have declared that they have no conflict of interest.
References
- Lakhani, A.; Gavino, I.; Yousafzai, A. The impact of caring for children with mental retardation on families as perceived by mothers in Karachi, Pakistan. JPMA. J. Pak. Med. Assoc. 2013, 63, 1468–1471. [Google Scholar] [PubMed]
- Mantri-Langeveldt, A.; Dada, S.; Boshoff, K. Measures for social support in raising a child with a disability: A scoping review. Child Care Health Dev. 2019, 45, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Hastings, R.P.; Allen, R.; McDermott, K.; Still, D. Factors related to positive perceptions in mothers of children with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2002, 15, 269–275. [Google Scholar] [CrossRef]
- Ngo, H.; Shin, J.Y.; Nhan, N.V.; Yang, L.H. Stigma and restriction on the social life of families of children with intellectual disabilities in Vietnam. Singap. Med. J. 2012, 53, 451–457. [Google Scholar]
- Green, S.; Davis, C.; Karshmer, E.; Marsh, P.; Straight, B. Living stigma: The impact of labeling, stereotyping, separation, status loss, and discrimination in the lives of individuals with disabilities and their families. Sociol. Inq. 2005, 75, 197–215. [Google Scholar] [CrossRef]
- Hayes, S.A.; Watson, S.L. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J. Autism Dev. Disord. 2013, 43, 629–642. [Google Scholar] [CrossRef]
- Glascoe, F.P. Evidence-based approach to developmental and behavioural surveillance using parents’ concerns. Child Care Health Dev. 2000, 26, 137–149. [Google Scholar] [CrossRef]
- Araújo, C.A.; Paz-Lourido, B.; Gelabert, S.V. Types of support to families of children with disabilities and their influence on family quality of life. Tipos de apoyo a las familias con hijos con discapacidad y su influencia en la calidad de vida familiar. Cienc. Saude Coletiva 2016, 21, 3121–3130. [Google Scholar] [CrossRef]
- Emerson, E.; Fortune, N.; Llewellyn, G.; Stancliffe, R. Loneliness, social support, social isolation and wellbeing among working age adults with and without disability: Cross-sectional study. Disabil. Health J. 2021, 14, 100965. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, S. The relationships between social support and loneliness: A meta-analysis and review. Acta Psychol. 2022, 227, 103616. [Google Scholar] [CrossRef]
- Lu, S.; Wu, Y.; Mao, Z.; Liang, X. Association of Formal and Informal Social Support With Health-Related Quality of Life Among Chinese Rural Elders. Int. J. Environ. Res. Public Health 2020, 17, 1351. [Google Scholar] [CrossRef] [PubMed]
- Uchino, B.N. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J. Behav. Med. 2006, 29, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Klein, B.C.; Busis, N.A. COVID-19 is catalyzing the adoption of teleneurology. Neurology 2020, 94, 903–904. [Google Scholar] [CrossRef] [PubMed]
- Li, X.H. Efects of social support on the quality of life of parents of autistic children based on an empirical analysis of 509 parents. Popul. Soc. 2018, 34, 76–85. [Google Scholar]
- Aquino, E.M.L.; Silveira, I.H.; Pescarini, J.M.; Aquino, R.; De Souza-Filho, J.A.; Rocha, A.D.S.; Ferreira, A.; Victor, A.; Teixeira, C.; Machado, D.B.; et al. Medidas de distanciamento social no controle da pandemia de COVID-19: Potenciais impactos e desafios no Brasil. Ciênc. Saúde Coletiva 2021, 25, 2423–2446. [Google Scholar] [CrossRef]
- Allison, K.M.; Levac, D.E. Impact of the COVID-19 pandemic on therapy service delivery and functioning for school-aged children with disabilities in the United States. Disabil. Health J. 2022, 15, 101266. [Google Scholar] [CrossRef]
- Silva, G.; Moraes, D.; Konstantyner, T.; Leite, H.P. Apoio social e qualidade de vida de famílias de crianças com cardiopatia congênita [Social support and quality of life of families with children with congenital heart disease]. Cienc. Saude Coletiva 2020, 25, 3153–3162. [Google Scholar] [CrossRef]
- Suarez-Balcazar, Y.; Mirza, M.; Errisuriz, V.L.; Zeng, W.; Brown, J.P.; Vanegas, S.; Heydarian, N.; Parra-Medina, D.; Morales, P.; Torres, H.; et al. Impact of COVID-19 on the Mental Health and Well-Being of Latinx Caregivers of Children with Intellectual and Developmental Disabilities. Int. J. Environ. Res. Public Health 2021, 18, 7971. [Google Scholar] [CrossRef]
- Gugała, B.; Penar-Zadarko, B.; Pięciak-Kotlarz, D.; Wardak, K.; Lewicka-Chomont, A.; Futyma-Ziaja, M.; Opara, J. Assessment of Anxiety and Depression in Polish Primary Parental Caregivers of Children with Cerebral Palsy Compared to a Control Group, as well as Identification of Selected Predictors. Int. J. Environ. Res. Public Health 2019, 16, 4173. [Google Scholar] [CrossRef]
- Hassanein EE, A.; Adawi, T.R.; Johnson, E.S. Social support, resilience, and quality of life for families with children with intellectual disabilities. Res. Dev. Disabil. 2021, 112, 103910. [Google Scholar] [CrossRef]
- Geweniger, A.; Haddad, A.; Barth, M.; Högl, H.; Mund, A.; Insan, S.; Langer, T. Mental health of children with and without special healthcare needs and of their caregivers during COVID-19: A cross-sectional study. BMJ Paediatr. Open. 2022, 6, e001509. [Google Scholar] [CrossRef] [PubMed]
- Forslund, T.; Fernqvist, S.; Tegler, H. Parents with intellectual disability reporting on factors affecting their caregiving in the wake of the COVID-19 pandemic: A qualitative study. J. Appl. Res. Intellect. Disabil. JARID 2022, 35, 1380–1389. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.; Albaum, C.; Tablon Modica, P.; Ahmad, F.; Gorter, J.W.; Khanlou, N.; McMorris, C.; Lai, J.; Harrison, C.; Hedley, T.; et al. The impact of COVID-19 on the mental health and wellbeing of caregivers of autistic children and youth: A scoping review. Autism Res. Off. J. Int. Soc. Autism Res. 2021, 14, 2477–2494. [Google Scholar] [CrossRef] [PubMed]
- Currie, G.; Finlay, B.; Seth, A.; Roth, C.; Elsabbagh, M.; Hudon, A.; Hunt, M.; Jodoin, S.; Lach, L.; Lencucha, R.; et al. Mental health challenges during COVID-19: Perspectives from parents with children with neurodevelopmental disabilities. Int. J. Qual. Stud. Health Well-Being 2022, 17, 2136090. [Google Scholar] [CrossRef]
- Alenezi, S.; Temsah, M.H.; Alyahya, A.S.; Almadani, A.H.; Almarshedi, A.; Algazlan, M.S.; Alnemary, F.; Bashiri, F.A.; Alkhawashki, S.H.; Altuwariqi, M.H.; et al. Mental health impact of COVID-19 on Saudi families and children with special educational needs and disabilities in Saudi Arabia: A national perspective. Front. Public Health 2022, 10, 992658. [Google Scholar] [CrossRef]
- Grumi, S.; Provenzi, L.; Gardani, A.; Aramini, V.; Dargenio, E.; Naboni, C.; Vacchini, V.; Borgatti, R.; Engaging with Families through On-line Rehabilitation for Children during the Emergency (EnFORCE) Group. Rehabilitation services lockdown during the COVID-19 emergency: The mental health response of caregivers of children with neurodevelopmental disabilities. Disabil. Rehabil. 2021, 43, 27–32. [Google Scholar] [CrossRef]
- Dhiman, S.; Sahu, P.K.; Reed, W.R.; Ganesh, G.S.; Goyal, R.K.; Jain, S. Impact of COVID-19 outbreak on mental health and perceived strain among caregivers tending children with special needs. Res. Dev. Disabil. 2020, 107, 103790. [Google Scholar] [CrossRef]
- Varengue, R.; Brochard, S.; Bouvier, S.; Bailly, R.; Houx, L.; Lempereur, M.; Kandalaft, C.; Chatelin, A.; Vagnoni, J.; Vuillerot, C.; et al. Perceived impact of lockdown on daily life in children with physical disabilities and their families during the COVID-19 pandemic. Child Care Health Dev. 2022, 48, 942–955. [Google Scholar] [CrossRef]
- Zhang, S.; Hao, Y.; Feng, Y.; Lee, N.Y. COVID-19 Pandemic Impacts on Children with Developmental Disabilities: Service Disruption, Transition to Telehealth, and Child Wellbeing. Int. J. Environ. Res. Public Health 2022, 19, 3259. [Google Scholar] [CrossRef]
- Celik, M.Y. Assessment of Have Problems and Care Burdens of Mothers with Handicapped Children in COVID-19 Pandemic. Soc. Work Public Health 2021, 36, 638–646. [Google Scholar] [CrossRef]
- Fridell, A.; Norrman, H.N.; Girke, L.; Bölte, S. Effects of the Early Phase of COVID-19 on the Autistic Community in Sweden: A Qualitative Multi-Informant Study Linking to ICF. Int. J. Environ. Res. Public Health 2022, 19, 1268. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Sherman, S.A.; Burwinkle, T.M.; Dickinson, P.E.; Dixon, P. The PedsQL Family Impact Module: Preliminary reliability and validity. Health Qual. Life Outcomes 2004, 2, 55. [Google Scholar] [CrossRef] [PubMed]
- Griep, R.H.; Chor, D.; Faerstein, E.; Werneck, G.L.; Lopes, C.S. Validade de constructo de escala de apoio social do Medical Outcomes Study adaptada para o português no Estudo Pró-Saúde [Construct validity of the Medical Outcomes Study’s social support scale adapted to Portuguese in the Pró-Saúde Study]. Cad. Saude Publica 2005, 21, 703–714. [Google Scholar] [CrossRef]
- Klatchoian, D.A.; Len, C.A.; Terreri, M.T.R.; Silva, M.; Itamoto, C.; Ciconelli, R.M.; Varni, J.W.; Hilário, M.O.E. Qualidade de vida de crianças e adolescentes de São Paulo: Confiabilidade e validade da versão brasileira do questionário genérico Pediatric Quality of Life InventoryTM versão 4.0. J. De Pediatr. 2008, 84, 308–315. [Google Scholar] [CrossRef]
- Varni, J.W. The Pedsql Measurement Model for the Pediatric Quality of Life Inventory. The PedsQL Scoring Algorithm. 1998. Available online: http://www.pedsql.org/score.html (accessed on 15 December 2021).
- Scarpelli, A.C.; Paiva, S.M.; Pordeus, I.A.; Varni, J.W.; Viegas, C.M.; Allison, P.J. The Pediatric Quality of Life Inventory™ (PedsQL™) family impact module: Reliability and validity of the Brazilian version. Qual. Life Outcomes 2008, 6, 35. [Google Scholar] [CrossRef]
- Light, J.G.; Warner, W.J. Statistics for social scientists. By Louis Cohen and Michael Holliday. Harper & Row 1982. Int. J. Soc. Psychiatry 1983, 29, 236. [Google Scholar] [CrossRef]
- Matsukura, T.S.; Marturano, E.M.; Oishi, J.; Borasche, G. Stress and social support for mothers of children with special needs. Rev. Bras. Educ. Espec. 2007, 13, 415–428. [Google Scholar] [CrossRef]
- Pfeifer, L.I.; Silva, D.B.R.; Lopes, P.B.; Matsukura, T.S.; Santos, J.L.F.; Pinto, M.P.P. Social support provided to caregivers of children with cerebral palsy. Child Care Health Dev. 2013, 40, 363–369. [Google Scholar] [CrossRef]
- Zhao, M.; Fu, W.; Ai, J. The Mediating Role of Social Support in the Relationship Between Parenting Stress and Resilience Among Chinese Parents of Children with Disability. J. Autism Dev. Disord. 2021, 51, 3412–3422. [Google Scholar] [CrossRef]
- Makris, T.; Dorstyn, D.; Crettenden, A. Quality of life in children and adolescents with cerebral palsy: A systematic review with meta-analysis. Disabil. Rehabil. 2021, 43, 299–308. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.; Jacoby, P.; Whitehouse, A.; Kim, R.; Epstein, A.; Murphy, N.; Reid, S.; Leonard, H.; Reddihough, D.; Downs, J. Functioning, participation, and quality of life in children with intellectual disability: An observational study. Dev. Med. Child Neurol. 2021, 63, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Rozensztrauch, A.; Kołtuniuk, A. The Quality of Life of Children with Epilepsy and the Impact of the Disease on the Family Functioning. Int. J. Environ. Res. Public Health 2022, 19, 2277. [Google Scholar] [CrossRef]
- Yao, M.; Ma, Y.; Qian, R.; Xia, Y.; Yuan, C.; Bai, G.; Mao, S. Quality of life of children with spinal muscular atrophy and their caregivers from the perspective of caregivers: A Chinese cross-sectional study. Orphanet J. Rare Dis. 2021, 16, 7. [Google Scholar] [CrossRef]
- Gorgoraptis, N.; Zaw-Linn, J.; Feeney, C.; Tenorio-Jimenez, C.; Niemi, M.; Malik, A.; Ham, T.; Goldstone, A.P.; Sharp, D.J. Cognitive impairment and health-related quality of life following traumatic brain injury. NeuroRehabilitation 2019, 44, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Greiman, L.; Ravesloot, C.; Goddard, K.S.; Ward, B. Effects of a consumer driven home modification intervention on community participation for people with mobility disabilities. Disabil. Health J. 2022, 15, 101210. [Google Scholar] [CrossRef]
- Tsang, D.S.; Schulte, F. Beyond the brain: Socioeconomic status and race in pediatric brain tumor survivorship. Neuro-Oncology 2021, 23, 1050–1051. [Google Scholar] [CrossRef]
- Yeates, K.O.; Taylor, H.G.; Wade, S.L.; Drotar, D.; Stancin, T.; Minich, N. A prospective study of short- and long-term neuropsychological outcomes after pediatric traumatic brain injury. Neuropsychology 2002, 16, 514–523. [Google Scholar] [CrossRef]
- Guillamón, N.; Nieto, R.; Pousada, M.; Redolar, D.; Muñoz, E.; Hernández, E.; Boixadós, M.; Gómez-Zúniga, B. Quality of life and mental health among parents of children with cerebral palsy: The influence of self-efficacy and coping strategies. J. Clin. Nursing. 2013, 22, 1579–1590. [Google Scholar] [CrossRef]
- Barros, A.; de Gutierrez, G.M.; Barros, A.O.; Santos, M. Quality of life and burden of caregivers of children and adolescents with disabilities. Spec. Care Dent. 2019, 39, 380–388. [Google Scholar] [CrossRef]
- Isa, S.N.I.; Ishak, I.; Ab Rahman, A.; Saat, N.Z.M.; Din, N.C.; Lubis, S.H.; Ismail, M.F.M. Health and quality of life among the caregivers of children with disabilities: A review of literature. Asian J. Psychiatry 2016, 23, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Pozniak, K.; Kraus de Camargo, O. “Your ‘Only’ Is My Everything”: Mothering Children with Disabilities through COVID-19. In Mothers, Mothering, and COVID-19: Dispatches from the Pandemic; O’Reilly, A., Green, F.J., Eds.; Demeter Press: Bradford, ON, Canada, 2021; pp. 277–290. [Google Scholar]
- Lichand, G.; Doria, C.A.; Cossi Fernandes, J.P.; Leal-Neto, O. Association of COVID-19 Incidence and Mortality Rates With School Reopening in Brazil During the COVID-19 Pandemic. JAMA Health Forum. 2022, 3, e215032. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.H.; Sung, C.; Kammes, R.R.; Okyere, C.; Park, J. Social support as a mediator of stress and life satisfaction for people with intellectual or developmental disabilities during the COVID-19 pandemic. J. Appl. Res. Intellect. Disabil. JARID 2022, 35, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.M.; Wainwright, L.; Bennett, J. The double ABCX model of adaptation in racially diverse families with a school-age child with autism. J. Autism Dev. Disord. 2011, 41, 320–331. [Google Scholar] [CrossRef] [PubMed]
- Caicedo, C. Families with special needs children: Family health, functioning, and care burden. J. Am. Psychiatr. Nurses Assoc. 2014, 20, 398–407. [Google Scholar] [CrossRef] [PubMed]
- Chakraborti, M.; Gitimoghaddam, M.; McKellin, W.H.; Miller, A.R.; Collet, J.P. Understanding the Implications of Peer Support for Families of Children With Neurodevelopmental and Intellectual Disabilities: A Scoping Review. Front. Public Health 2021, 9, 719640. [Google Scholar] [CrossRef]
- Jackson, J.B.; Steward, S.R.; Roper, S.O.; Muruthi, B.A. Support Group Value and Design for Parents of Children with Severe or Profound Intellectual and Developmental Disabilities. J. Autism Dev. Disord. 2018, 48, 4207–4221. [Google Scholar] [CrossRef]
- Verhey, L.H.; Kulik, D.M.; Ronen, G.M.; Rosenbaum, P.; Lach, L.; Streiner, D.L.; Canadian Pediatric Epilepsy, N. Quality of life in childhood epilepsy: What is the level of agreement between youth and their parents? Epilepsy Behav. 2009, 14, 407–410. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).