Getting Connected to M-Health Technologies through a Meta-Analysis
Abstract
1. Introduction
2. Acceptance Models
3. Materials and Methods
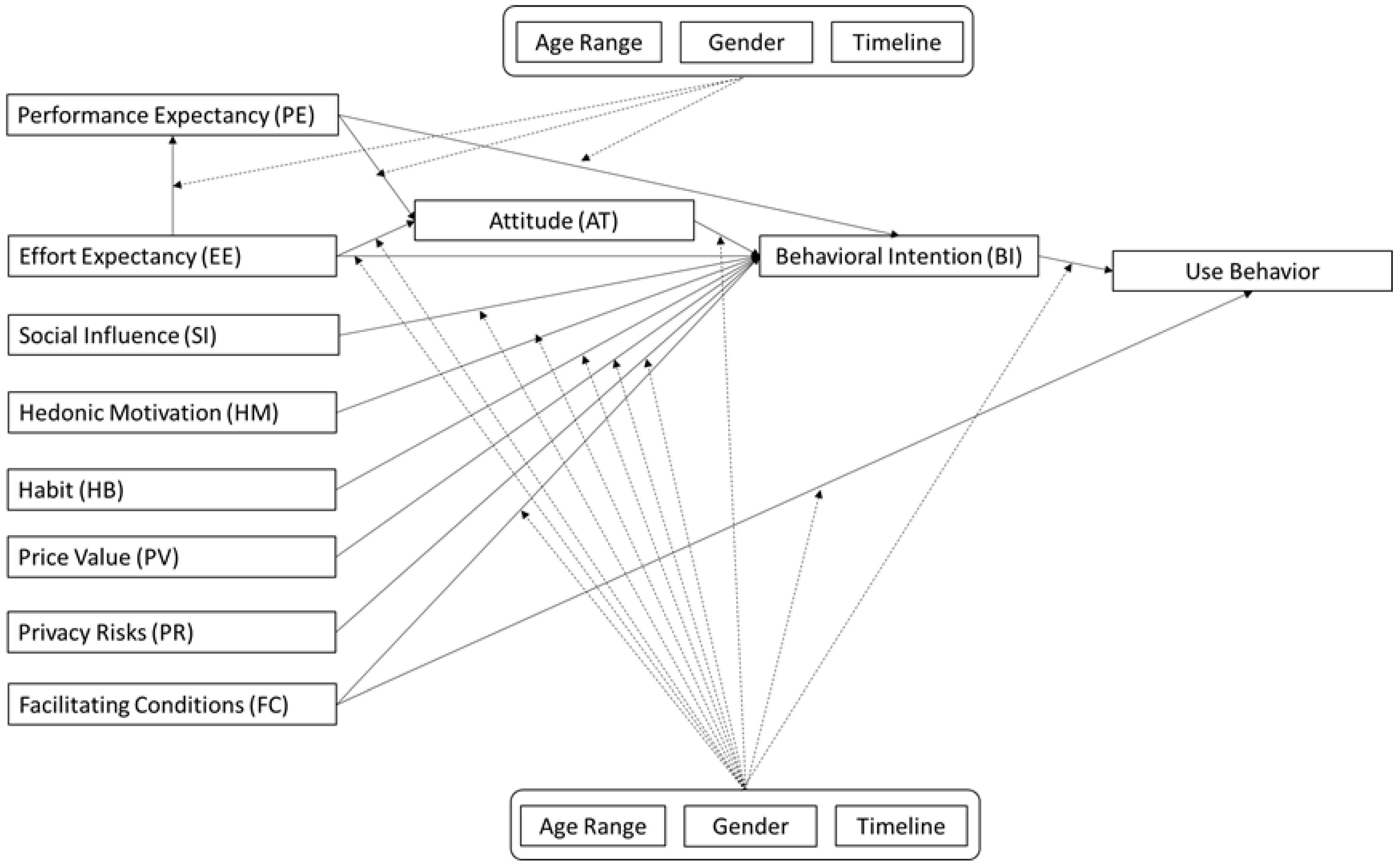
3.1. Proposed Model
3.1.1. Moderators
Gender
Age Range
Timeline
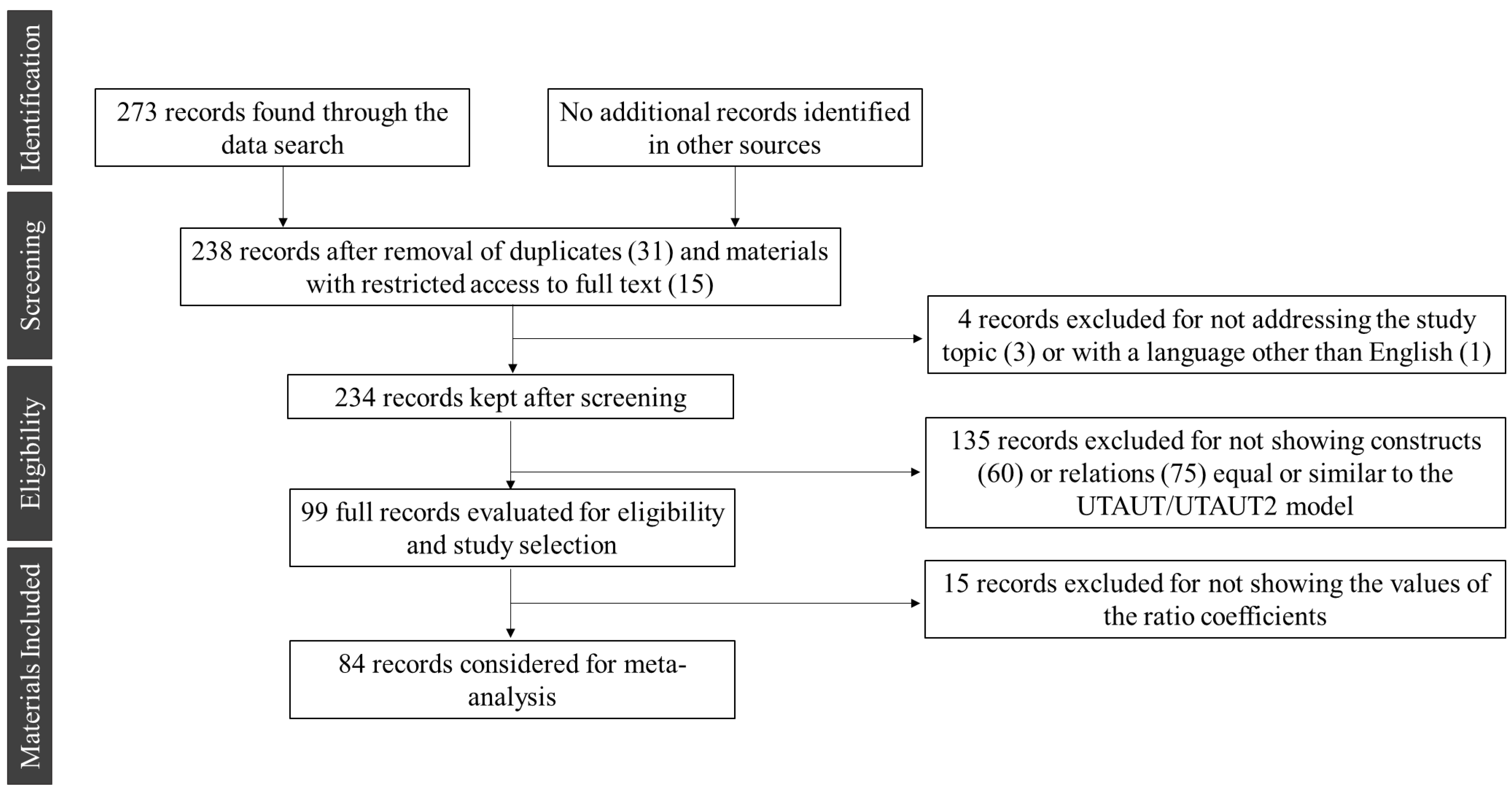
3.2. Sample
3.3. Coding
3.4. Analysis
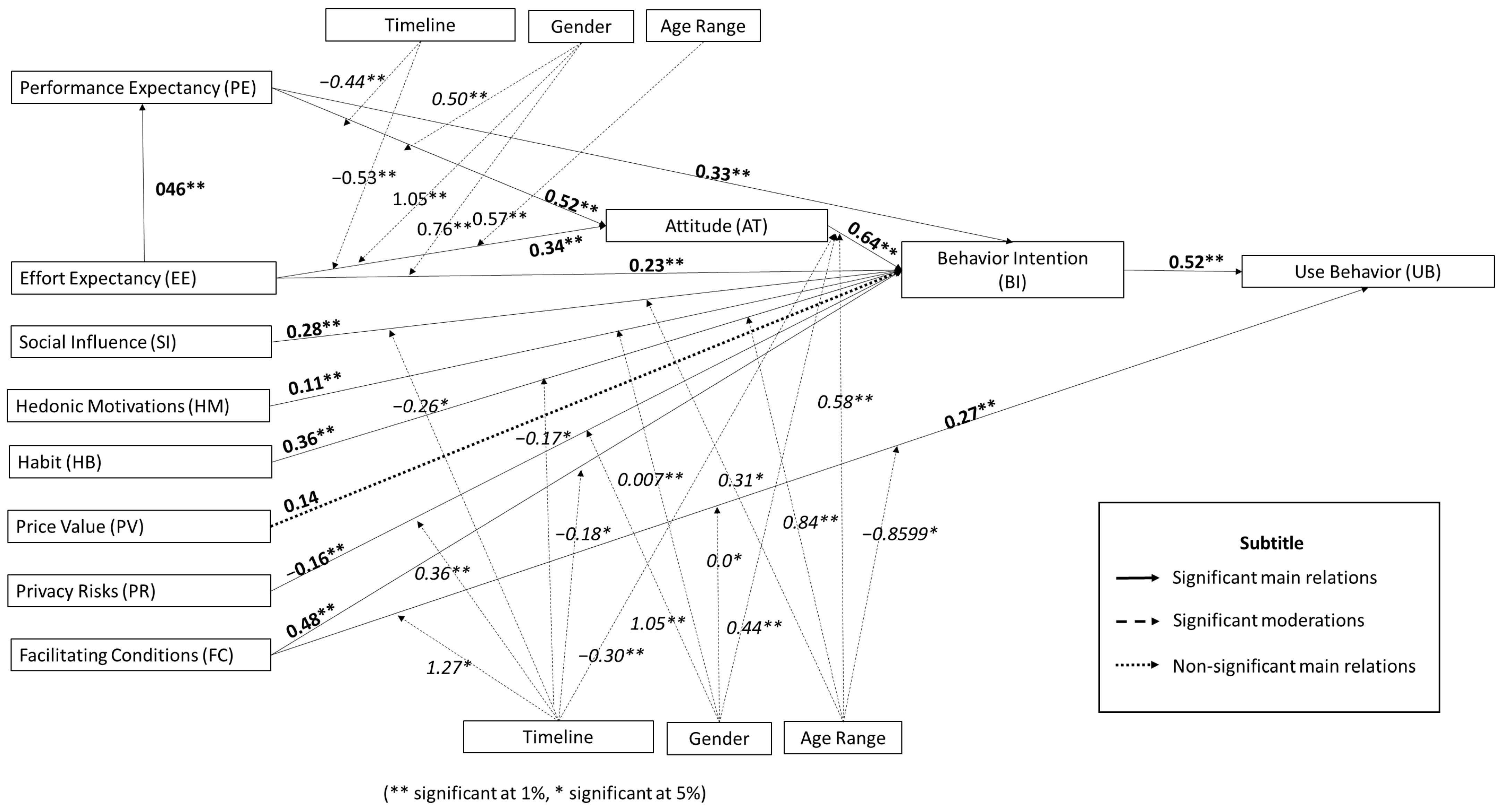
4. Results
4.1. Overview of the Studies Considered for the Meta-Analysis
4.2. Reliability of Constructs
4.3. Meta-Analysis of Model Correlations
5. Discussion
5.1. Main Relations of the Model
5.2. Relations of the Moderating Variables
5.2.1. Gender
5.2.2. Age Range
5.2.3. Timeline
5.3. Implications for Theory and Practice
5.4. Limitations and Directions for Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Relation | Label | N | Original Correlation |
|---|---|---|---|
| PE > BI | |||
| [96] | 195 | 0.260 | |
| [129] | 318 | 0.280 | |
| [33] | 58 | 0.280 | |
| [27] | 123 | 0.137 | |
| [27] | 112 | 0.390 | |
| [98] | 268 | 0.152 | |
| [90] | 787 | 0.400 | |
| [152] | 376 | 0.274 | |
| [29] | 256 | 0.101 | |
| [39] | 406 | 0.425 | |
| [30] | 325 | 0.493 | |
| [137] | 185 | 0.163 | |
| [26] | 660 | 0.113 | |
| [91] | 31 | 0.128 | |
| [93] | 217 | 0.086 | |
| [93] | 109 | 0.166 | |
| [93] | 108 | 0.458 | |
| [178] | 263 | −0.760 | |
| [179] | 311 | 0.222 | |
| [85] | 296 | 0.232 | |
| [148] | 340 | 0.223 | |
| [180] | 528 | 0.090 | |
| [181] | 458 | 0.212 | |
| [131] | 81 | 0.224 | |
| [182] | 100 | 0.055 | |
| [183] | 280 | 0.032 | |
| [183] | 280 | 0.488 | |
| [92] | 124 | 0.361 | |
| [84] | 452 | 0.259 | |
| [184] | 437 | 0.109 | |
| [185] | 582 | 0.080 | |
| [92] | 124 | 0.290 | |
| [186] | 633 | 0.322 | |
| [187] | 211 | 0.155 | |
| [188] | 410 | 0.322 | |
| [144] | 271 | 0.263 | |
| [32] | 392 | 0.273 | |
| [149] | 324 | 0.464 | |
| [31] | 927 | 0.359 | |
| [145] | 146 | 0.3193 | |
| [101] | 280 | 0.250 | |
| [189] | 247 | 0.155 | |
| [130] | 130 | 0.2095 | |
| [132] | 386 | 0.160 | |
| [138] | 363 | 0.155 | |
| [138] | 363 | 0.324 | |
| [190] | 234 | 0.081 | |
| [71] | 120 | 0.290 | |
| [191] | 314 | 0.480 | |
| [192] | 400 | 0.270 | |
| [77] | 245 | 0.132 | |
| [193] | 894 | 0.389 | |
| [193] | 894 | 0.308 | |
| [194] | 107 | 0.420 | |
| [72] | 388 | 0.099 | |
| [161] | 534 | 0.770 | |
| [161] | 534 | 0.352 | |
| [146] | 274 | 0.580 | |
| [195] | 156 | 0.180 | |
| [196] | 129 | 0.454 | |
| [197] | 313 | 0.386 | |
| [198] | 600 | 0.690 | |
| [199] | 210 | 0.370 | |
| [200] | 519 | 0.691 | |
| [198] | 436 | 0.320 | |
| [198] | 436 | 0.340 | |
| [201] | 927 | 0.280 | |
| [28] | 227 | 0.380 | |
| [150] | 164 | 0.504 | |
| [202] | 273 | 0.80 | |
| [203] | 225 | 0.750 | |
| [204] | 196 | 0.125 | |
| [203] | 225 | 0.3891 | |
| [147] | 462 | 0.427 | |
| [147] | 232 | 0.299 | |
| [147] | 230 | 0.308 | |
| [205] | 927 | 0.151 | |
| EE > BI | |||
| [96] | 195 | 0.020 | |
| [129] | 318 | −0.050 | |
| [33] | 58 | 0.133 | |
| [27] | 123 | 0.004 | |
| [27] | 112 | 0.097 | |
| [90] | 787 | 0.003 | |
| [152] | 376 | 0.220 | |
| [206] | 194 | −0.050 | |
| [29] | 256 | 0.004 | |
| [39] | 406 | 0.281 | |
| [30] | 325 | 0.206 | |
| [137] | 185 | 0.140 | |
| [26] | 660 | 0.194 | |
| [93] | 217 | 0.145 | |
| [93] | 109 | 0.072 | |
| [93] | 108 | 0.169 | |
| [178] | 263 | 0.126 | |
| [179] | 311 | 0.150 | |
| [85] | 296 | −0.032 | |
| [148] | 340 | 0.255 | |
| [181] | 458 | 0.261 | |
| [131] | 81 | 0.640 | |
| [182] | 100 | 0.305 | |
| [183] | 280 | 0.234 | |
| [183] | 280 | 0.209 | |
| [92] | 124 | 0.265 | |
| [84] | 452 | 0.067 | |
| [185] | 582 | 0.013 | |
| [92] | 124 | 0.128 | |
| [187] | 211 | −0.011 | |
| [188] | 410 | 0.622 | |
| [144] | 271 | 0.169 | |
| [32] | 392 | 0.622 | |
| [149] | 324 | 0.178 | |
| [31] | 927 | 0.377 | |
| [207] | 108 | 0.037 | |
| [208] | 423 | 0.197 | |
| [101] | 280 | 0.188 | |
| [189] | 247 | 0.010 | |
| [130] | 130 | 0.169 | |
| [132] | 386 | 0.701 | |
| [138] | 363 | 0.110 | |
| [138] | 363 | 0.169 | |
| [190] | 234 | −0.040 | |
| [71] | 120 | 0.340 | |
| [191] | 314 | 0.520 | |
| [192] | 400 | 0.570 | |
| [77] | 245 | 0.073 | |
| [72] | 388 | 0.135 | |
| [161] | 534 | 0.028 | |
| [161] | 534 | 0.340 | |
| [146] | 274 | 0.067 | |
| [195] | 156 | −0.010 | |
| [196] | 129 | 0.329 | |
| [209] | 141 | 0.220 | |
| [198] | 600 | 0.490 | |
| [200] | 519 | 0.145 | |
| [201] | 927 | 0.610 | |
| [28] | 227 | 0.132 | |
| [150] | 164 | 0.070 | |
| [203] | 225 | 0.128 | |
| [204] | 196 | 0.188 | |
| [203] | 225 | 0.570 | |
| [147] | 462 | 0.107 | |
| [147] | 232 | 0.024 | |
| [147] | 230 | 0.028 | |
| [205] | 927 | 0.130 | |
| EE > PE | |||
| [90] | 787 | 0.357 | |
| [91] | 31 | 0.170 | |
| [185] | 582 | 0.370 | |
| [159] | 322 | 0.500 | |
| [97] | 104 | 0.479 | |
| [186] | 633 | 0.026 | |
| [131] | 81 | 0.379 | |
| [145] | 146 | 0.305 | |
| [210] | 1400 | 0.390 | |
| [189] | 247 | 0.243 | |
| [193] | 894 | 0.650 | |
| [193] | 894 | 0.660 | |
| [190] | 234 | 0.379 | |
| [71] | 120 | 0.185 | |
| [198] | 600 | 0.610 | |
| [200] | 519 | 0.650 | |
| [211] | 343 | 0.280 | |
| [212] | 88 | 0.532 | |
| [39] | 406 | 0.280 | |
| [202] | 273 | 0.362 | |
| [149] | 324 | 0.320 | |
| PE > AT | |||
| [93] | 217 | 0.340 | |
| [92] | 124 | 0.123 | |
| [91] | 31 | 0.590 | |
| [94] | 303 | 0.644 | |
| [95] | 582 | 0.459 | |
| [97] | 104 | 0.193 | |
| [92] | 124 | 0.280 | |
| [186] | 633 | 0.781 | |
| [131] | 81 | 0.340 | |
| [213] | 1063 | 0.354 | |
| [214] | 411 | 0.345 | |
| [25] | 1000 | 0.310 | |
| [193] | 894 | 0.556 | |
| [193] | 894 | 0.510 | |
| [190] | 234 | 0.500 | |
| [196] | 129 | 0.345 | |
| [136] | 206 | 0.500 | |
| EE > AT | |||
| [92] | 124 | 0.410 | |
| [91] | 31 | 0.087 | |
| [94] | 303 | 0.120 | |
| [95] | 582 | 0.138 | |
| [97] | 104 | 0.112 | |
| [92] | 124 | 0.040 | |
| [186] | 633 | 0.030 | |
| [131] | 81 | 0.410 | |
| [213] | 1063 | 0.034 | |
| [214] | 411 | 0.760 | |
| [193] | 894 | 0.080 | |
| [193] | 894 | 0.310 | |
| [190] | 234 | 0.300 | |
| [196] | 129 | 0.760 | |
| [136] | 206 | 0.120 | |
| [212] | 88 | 0.635 | |
| AT > BI | |||
| [96] | 195 | 0.581 | |
| [91] | 31 | 0.740 | |
| [215] | 494 | 0.316 | |
| [97] | 104 | 0.494 | |
| [131] | 81 | 0.641 | |
| [190] | 234 | 0.641 | |
| [191] | 314 | 0.402 | |
| [191] | 314 | 0.368 | |
| [216] | 238 | 0.110 | |
| [212] | 88 | 0.637 | |
| SI > BI | |||
| [96] | 195 | 0.850 | |
| [129] | 318 | 0.230 | |
| [27] | 123 | 0.076 | |
| [27] | 112 | 0.189 | |
| [98] | 268 | 0.115 | |
| [152] | 376 | 0.252 | |
| [29] | 256 | 0.210 | |
| [39] | 406 | −0.005 | |
| [30] | 325 | 0.111 | |
| [137] | 185 | 0.071 | |
| [179] | 311 | 0.066 | |
| [85] | 296 | 0.121 | |
| [148] | 340 | 0.589 | |
| [159] | 322 | −0.109 | |
| [215] | 494 | 0.171 | |
| [182] | 100 | 0.188 | |
| [92] | 124 | 0.138 | |
| [84] | 452 | −0.013 | |
| [92] | 124 | 0.160 | |
| [188] | 410 | −0.042 | |
| [144] | 271 | −0.040 | |
| [32] | 392 | 0.475 | |
| [149] | 324 | 0.206 | |
| [31] | 927 | 0.193 | |
| [101] | 280 | 0.020 | |
| [130] | 130 | 0.224 | |
| [132] | 386 | 0.134 | |
| [138] | 363 | 0.397 | |
| [138] | 363 | 0.243 | |
| [71] | 120 | 0.220 | |
| [191] | 314 | 0.525 | |
| [191] | 314 | 0.185 | |
| [192] | 400 | 0.1441 | |
| [77] | 245 | 0.330 | |
| [161] | 534 | 0.170 | |
| [161] | 534 | 0.134 | |
| [146] | 274 | 0.2207 | |
| [195] | 156 | 0.110 | |
| [216] | 238 | 0.134 | |
| [196] | 129 | 0.199 | |
| [209] | 141 | 0.231 | |
| [217] | 482 | 0.140 | |
| [217] | 482 | 0.206 | |
| [217] | 482 | 0.455 | |
| [217] | 482 | 0.303 | |
| [139] | 212 | 0.184 | |
| [201] | 927 | 0.460 | |
| [28] | 227 | 0.219 | |
| [150] | 164 | 0.140 | |
| [202] | 273 | 0.240 | |
| [203] | 225 | 0.500 | |
| [204] | 196 | 0.687 | |
| [203] | 225 | 0.673 | |
| [147] | 462 | 0.768 | |
| [147] | 232 | 0.165 | |
| [147] | 230 | 0.184 | |
| [205] | 927 | 0.128 | |
| CF > BI | |||
| [129] | 318 | 0.280 | |
| [33] | 58 | 0.150 | |
| [27] | 123 | 0.231 | |
| [27] | 112 | 0.180 | |
| [98] | 268 | 0.009 | |
| [90] | 787 | 0.131 | |
| [206] | 194 | 0.163 | |
| [90] | 787 | 0.070 | |
| [29] | 256 | 0.191 | |
| [39] | 406 | 0.513 | |
| [30] | 325 | 0.275 | |
| [178] | 263 | −0.630 | |
| [188] | 296 | 0.034 | |
| [148] | 340 | 0.314 | |
| [159] | 322 | 0.327 | |
| [182] | 100 | −0.126 | |
| [183] | 280 | 0.254 | |
| [92] | 124 | 0.060 | |
| [84] | 452 | 0.040 | |
| [92] | 124 | 0.235 | |
| [188] | 410 | −0.016 | |
| [144] | 271 | 0.298 | |
| [32] | 392 | 0.130 | |
| [149] | 324 | 0.235 | |
| [31] | 927 | 0.300 | |
| [145] | 146 | 0.235 | |
| [101] | 280 | 0.258 | |
| [130] | 130 | 0.040 | |
| [132] | 386 | 0.510 | |
| [138] | 363 | −0.010 | |
| [77] | 245 | 0.183 | |
| [138] | 363 | −0.111 | |
| [161] | 534 | 0.126 | |
| [161] | 534 | 0.230 | |
| [146] | 274 | 0.131 | |
| [195] | 156 | 0.174 | |
| [196] | 129 | −0.050 | |
| [201] | 927 | 0.183 | |
| [150] | 164 | 0.080 | |
| [203] | 225 | 0.126 | |
| [203] | 225 | 0.067 | |
| [203] | 225 | 0.126 | |
| [205] | 927 | 0.250 | |
| HM > BI | |||
| [129] | 318 | −0.010 | |
| [33] | 58 | 0.267 | |
| [98] | 268 | 0.176 | |
| [29] | 256 | 0.127 | |
| [30] | 325 | −0.030 | |
| [179] | 311 | 0.065 | |
| [148] | 340 | 0.410 | |
| [159] | 322 | 0.107 | |
| [182] | 100 | 0.239 | |
| [188] | 410 | 0.098 | |
| [144] | 271 | 0.420 | |
| [32] | 392 | 0.071 | |
| [149] | 324 | 0.111 | |
| [130] | 130 | 0.015 | |
| [132] | 386 | 0.050 | |
| [197] | 313 | −0.050 | |
| [150] | 164 | 0.080 | |
| [204] | 196 | 0.151 | |
| [203] | 225 | 0.227 | |
| [202] | 273 | 0.257 | |
| [203] | 225 | 0.255 | |
| [147] | 462 | 0.190 | |
| [147] | 232 | 0.227 | |
| [147] | 230 | 0.213 | |
| HB > BI | |||
| [129] | 318 | 0.020 | |
| [33] | 58 | 0.212 | |
| [29] | 256 | 0.430 | |
| [148] | 340 | 0.533 | |
| [159] | 322 | 0.390 | |
| [32] | 392 | 0.160 | |
| [149] | 324 | 0.742 | |
| [130] | 130 | 0.421 | |
| [132] | 386 | 0.390 | |
| PV > BI | |||
| [129] | 318 | 0.040 | |
| [29] | 256 | −0.022 | |
| [178] | 263 | 0.026 | |
| [188] | 296 | 0.020 | |
| [148] | 340 | −0.013 | |
| [159] | 322 | 0.139 | |
| [144] | 271 | 0.180 | |
| [32] | 392 | 0.100 | |
| [149] | 324 | −0.046 | |
| [130] | 130 | 0.936 | |
| [132] | 386 | 0.100 | |
| [150] | 164 | 0.120 | |
| PR > BI | |||
| [98] | 268 | −0.111 | |
| [90] | 787 | −0.001 | |
| [152] | 376 | 0.055 | |
| [184] | 437 | −0.367 | |
| [101] | 280 | −0.090 | |
| [72] | 388 | −0.252 | |
| [157] | 333 | −0.270 | |
| [218] | 650 | −0.043 | |
| FC > UB | |||
| [161] | 534 | 0.953 | |
| [161] | 534 | 0.513 | |
| [77] | 245 | 0.082 | |
| [146] | 274 | 0.0979 | |
| [203] | 225 | 0.250 | |
| BI > UB | |||
| [137] | 185 | 0.326 | |
| [26] | 660 | 0.750 | |
| [31] | 927 | 0.251 | |
| [77] | 245 | 0.426 | |
| [161] | 534 | 0.581 | |
| [161] | 534 | 0.715 | |
| [146] | 274 | 0.414 | |
| [201] | 927 | 0.251 | |
| [203] | 225 | 0.367 | |
| [205] | 927 | 0.251 |
Appendix B
| Authors | Country | Title of Article |
|---|---|---|
| Gallos and Mantas (2015) [212] | Greece | The ‘SMART travel health’ mobile application assessment |
| Gao et al. (2015) [147] | China/USA | An empirical study of wearable technology acceptance in healthcare |
| Nisha et al. (2015) [205] | Bangladesh | Mobile health services: A new paradigm for health care systems |
| Cho (2016) [211] | South Korea | The impact of post-adoption beliefs on the continued use of health apps |
| Cho and Park (2016) [202] | South Korea | The influential factors on the diffusion of smartwatches in Korea |
| Dwivedi et al. (2016) [150] | UK | A generalised adoption model for services: A cross-country comparison of mobile health (m-health) |
| Guo et al. (2016) [218] | China | The privacy-personalization paradox in mHealth services acceptance of different age groups |
| Hoque (2016) [28] | Bangladesh | An empirical study of mHealth adoption in a developing country: The moderating effect of gender concern |
| Li et al. (2016) [157] | China | Examining individuals’ adoption of healthcare wearable devices: An empirical study from privacy calculus perspective |
| Lunney et al. (2016) [136] | USA | Wearable fitness technology: A structural investigation into acceptance and perceived fitness outcomes |
| Moon et al. (2016) [203] | South Korea | An Empirical Study of Impacts of User Intention for Smart Wearable Devices and Use Behavior |
| Nisha et al. (2016) [201] | Bangladesh | Exploring the role of service quality and knowledge for mobile health services |
| Pfeiffer et al. (2016) [204] | Germany | Quantify-ME: Consumer acceptance of wearable self-tracking devices |
| Wu et al. (2016) [219] | China | Exploring consumers’ intention to accept smartwatch |
| Hoque and Sorwar (2017) [146] | Finland | Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model |
| Khakurel et al. (2017) [196] | Finland | Intended use of Smartwatches and Pedometers in the University Environment: An Empirical Analysis |
| Könsgen et al. (2017) [199] | Germany | A user-centered perspective of mhealth: Understanding patients’ intentions to use mobile video consultation services |
| Lee et al. (2017) [197] | Bangladesh/Australia | Consumer choice of on-demand mHealth app services: Context and contents values using structural equation modeling |
| Miao et al. (2017) [200] | China | Factors that influence users’ adoption intention of mobile health: a structural equation modeling approach |
| Rajanen and Weng (2017) [195] | Finland | Digitization for fun or reward? A study of acceptance of wearable devices for personal healthcare |
| Schuster et al. (2017) [217] | Australia | Consumer Acceptance of mHealth Services: A Comparison of Behavioral Intention Models |
| Seol et al. (2017) [161] | South Korea | UX Analysis based on TR and UTAUT of Sports Smart Wearable Devices |
| Sergueeva and Shaw (2017) [209] | Canada | Improving Healthcare with Wearables: Overcoming the Barriers to Adoption |
| Zhang et al. (2017) [198] | Hong Kong | User acceptance of mobile health services from users’ perspectives: The role of self-efficacy and response-efficacy in technology acceptance |
| Zhu et al. (2017) [216] | USA | “Social Networkout”: Connecting Social Features of Wearable Fitness Trackers with Physical Exercise |
| Alsswey et al. (2018) [190] | Malaysia | Investigating the acceptance of mobile health application user interface cultural-based design to assist Arab elderly users |
| Chen and Lin (2018) [193] | Taiwan | Incorporation of health consciousness into the technology readiness and acceptance model to predict app download and usage intentions |
| Deng et al. (2018) [72] | China | What predicts patients’ adoption intention toward mhealth services in China: Empirical study |
| Kranthi and Ahmed (2018) [132] | India | Determinants of smartwatch adoption among IT professionals—an extended UTAUT2 model for smartwatch enterprise |
| Lai and Huang (2018) [71] | Taiwan | A Study on the Intention to Use the Wearable Device in Taiwan: A Case Study on Xiaomi Mi Band |
| Lee et al. (2018) [192] | South Korea | Factors affecting user acceptance in overuse of smartphones in mobile health services: An empirical study testing a modified integrated model in South Korea |
| Mital et al. (2018) [191] | India | Adoption of Internet of Things in India: A test of competing models using a structured equation modeling approach |
| Quaosar et al. (2018) [77] | China | Investigating factors affecting elderly’s intention to use m-health services: An empirical study |
| Reyes-Mercado (2018) [138] | Mexico | Adoption of fitness wearables Insights from partial least squares and qualitative comparative analysis |
| Rubin and Ophoff (2018) [130] | South Africa | Investigating Adoption Factors of Wearable Technology in Health and Fitness |
| Rupp et al. (2018) [194] | USA | The role of individual differences on perceptions of wearable fitness device trust, usability, and motivational impact |
| Aksoy et al. (2020) [214] | Turkey | Individuals’ intention to use sports wearables: the moderating role of technophobia |
| Alaiad et al. (2019) [101] | Jordania | The Determinants of M-Health Adoption in Developing Countries: An Empirical Investigation |
| Ali et al. (2019) [210] | China | Smoking-Cessation Acceptance Via Mobile Health and Quick Response Code Technologies: Empirical Evidence of a Pilot Study from China and Pakistan |
| Beh et al. (2019) [144] | Malaysia | Using smartwatches for fitness and health monitoring: the UTAUT2 combined with threat appraisal as moderators |
| Dhiman et al. (2019) [149] | India | Consumer adoption of smartphone fitness apps: an extended UTAUT2 perspective |
| Gastaldi et al. (2019) [25] | Italy | Consumer Adoption of Digital Technologies for Lifestyle Monitoring |
| Kim and Chiu (2019) [108] | South Korea/Hong Kong | Consumer acceptance of sports wearable technology: the role of technology readiness |
| Li et al. (2019) [145] | Hong Kong | Health monitoring through wearable technologies for older adults: Smart wearables acceptance model |
| Mbelwa et al. (2019) [207] | Tanzania | Acceptability and use of mobile health applications in health information systems: a case of eidsr and DHIS2 touch mobile applications in Tanzania |
| Nisha et al. (2019) [31] | Bangladesh | The changing paradigm of health and mobile phones: An innovation in the health care system |
| Talukder et al. (2019) [32] | China | Acceptance and use predictors of fitness wearable technology and intention to recommend |
| Wang and Lin (2019) [208] | China | Integrating TTF and IDT to evaluate user intention of big data analytics in mobile cloud healthcare system |
| Alam et al. (2020) [188] | Bangladesh | Do mobile health (mHealth) services ensure the quality of health life? An integrated approach from a developing country context |
| Alssey and Al-Samarraie (2020) [131] | Malaysia | Elderly users’ acceptance of mHealth user interface (UI) design-based culture: the moderator role of age |
| Binyamin and Hoque (2020) [29] | Saudi Arabia | Understanding the Drivers of Wearable Health Monitoring Technology: An Extension of the Unified Theory of Acceptance and Use of Technology |
| Chang et al. (2020) [84] | Taiwan | Exploring the Usage Intentions of Wearable Medical Devices: A Demonstration Study |
| Cheung et al. (2020) [187] | Australia/Hong Kong | Driving healthcare wearable technology adoption for Generation Z consumers in Hong Kong |
| Dahri et al. (2020) [137] | Pakistan | An overview of ai enabled m-iot wearable technology and its effects on the conduct of medical professionals in public healthcare in pakistan |
| Elprama et al. (2020) [92] | Belgium | Social Processes: What Determines Industrial Workers’ Intention to Use Exoskeletons? |
| Gangadharbatla (2020) [213] | USA | Biohacking: An exploratory study to understand the factors influencing the adoption of embedded technologies within the human body |
| Gupta et al. (2020) [93] | India | Gender differences in the wearable preferences, device and advertising value perceptions: Smartwatches vs. fitness trackers |
| Huang and Yang (2020) [181] | Taiwan | Empirical investigation of factors influencing consumer intention to use an artificial intelligence-powered mobile application for weight loss and health management |
| Klinker et al. (2020) [184] | Germany | Smart glasses in health care: A patient trust perspective |
| Lan et al. (2020) [148] | China | Investigating Influencing Factors of Chinese Elderly Users’ Intention to Adopt MHealth Based on the UTAUT2 Model |
| Li (2020) [94] | China | Healthcare at your fingertips: The acceptance and adoption of mobile medical treatment services among Chinese users |
| Liao et al. (2020) [183] | China | Comparison of Acceptance in Mobile Smart Wearable Technology between SEM and DEMATEL Methods |
| Lulin et al. (2020) [26] | China | Nurses’ Readiness in the Adoption of Hospital Electronic Information Management Systems in Ghana: The Application of the Structural Equation Modeling and the UTAUT Model |
| Meier et al. (2020) [179] | Switzerland/China | Wearable Technology Acceptance in Health Care Based on National Culture Differences: Cross-Country Analysis between Chinese and Swiss Consumers |
| Ndifon et al. (2020) [178] | Cameroon | Adoption of Mobile health Insurance Systems in Africa: evidence from Cameroon |
| Niknejad et al. (2020) [182] | Malaysia | A confirmatory factor analysis of the behavioral intention to use smart wellness wearables in Malaysia |
| Özdemir-Güngör et al. (2020) [97] | Turkey | An Acceptance Model for the Adoption of Smart Glasses Technology by Healthcare Professionals |
| Pai and Alathur (2020) [180] | India | Determinants of mobile health application awareness and use in India: An empirical analysis |
| Reith et al. (2020) [95] | Germany | Tracking fitness or sickness—Combining technology acceptance and privacy research to investigate the actual adoption of fitness trackers |
| Saheb (2020) [185] | Iran | An empirical investigation of the adoption of mobile health applications: integrating big data and social media services |
| Salgado et al. (2020) [159] | Portugal | Drivers of Mobile Health Acceptance and Use From the Patient Perspective: Survey Study and Quantitative Model Development |
| Talukder et al. (2020) [30] | Bangladesh | Predicting antecedents of wearable healthcare technology acceptance by elderly: A combined SEM-Neural Network approach |
| Tsai et al. (2020) [91] | Taiwan | Technology anxiety and resistance to change behavioral study of a wearable cardiac warming system using an extended TAM for older adults |
| Vongurai et al. (2020) [186] | Thailand | Factors influencing intention to use fitness trackers: A case study on Thais’ living in Bangkok |
| Wang et al. (2020) [39] | China | Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF |
| Zhang et al. (2020) [215] | China | Mobile health service adoption in China: Integration of theory of planned behavior, protection motivation theory and personal health differences |
| Huang et al. (2021) [33] | Taiwan | An Empirical Study on Factors Influencing Consumer Adoption Intention of an AI-Powered Chatbot for Health and Weight Management |
| Kim and Ho (2021) [98] | Taiwan | Validating the moderating role of age in multi-perspective acceptance model of wearable healthcare technology |
| Mahmood and Lee (2021) [152] | USA | Factors Influencing Older Adults’ Acceptance of HealthMonitoring Smart Clothing |
| Moudud-Ul-Huq et al. (2021) [27] | Bangladesh | Elderly and middle-aged intention to use m-health services: an empirical evidence from a developing country |
| Octavius and Antonio (2021) [90] | Indonesia | Antecedents of Intention to Adopt Mobile Health (mHealth) Application and Its Impact on Intention to Recommend: An Evidence from Indonesian Customers |
| Okpala and Nnaji (2021) [96] | USA | Wearable sensing devices acceptance behavior in construction safety and health: assessing existing models and developing a hybrid conceptual model |
| Olaleye et al. (2021) [206] | Finland | Please call my contact person: mobile devices for a rescue mission during an emergency |
| Rahman et al. (2021) [129] | Bangladesh | Teenagers’ behavioural intention towards wearable technologies and intention to recommend others: an empirical study in Bangladesh |
References
- Chau, K.Y.; Lam, M.H.S.; Cheung, M.L.; Tso, E.K.H.; Flint, S.W.; Broom, D.R.; Tse, G.; Lee, K.Y. Smart Technology for Healthcare: Exploring the Antecedents of Adoption Intention of Healthcare Wearable Technology. Health Psychol. Res. 2019, 7, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Geller, G.; Bernhardt, B.A.; Carrese, J.; Rushton, C.H.; Kolodner, K. What Do Clinicians Derive from Partnering with Their Patients?: A Reliable and Valid Measure of “Personal Meaning in Patient Care”. Patient Educ. Couns. 2008, 72, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Pison, U.; Welte, T.; Giersig, M.; Groneberg, D. Nanomedicine for Respiratory Diseases. Nanomed. Respir. Dis. Eur. J. Pharmacol. 2006, 533, 341–350. [Google Scholar] [CrossRef]
- Tantucci, A.; Ripani, C.; Giannini, C.; Fregonese, M.; De Angelis, M. Can a Program of Food and Diabetes Education Improve the Quality of the Lives of Diabetic Patients with a Previous Myocardial Infarction? Ann. Ig. 2018, 30, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Safi, S.; Danzer, G.; Schmailzl, K.J.G. Empirical Research on Acceptance of Digital Technologies in Medicine Among Patients and Healthy Users: Questionnaire Study. JMIR Hum. Factors 2019, 6, e13472. [Google Scholar] [CrossRef] [PubMed]
- Reeder, B.; David, A. Health at Hand: A Systematic Review of Smart Watch Uses for Health and Wellness. J. Biomed. Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef]
- Wang, Y.; Xue, H.; Huang, Y.; Huang, L.; Zhang, D. A Systematic Review of Application and Effectiveness of MHealth Interventions for Obesity and Diabetes Treatment and Self-Management. Adv. Nutr. 2017, 8, 449–462. [Google Scholar] [CrossRef]
- Sari, H.; Othman, M.; Al-Ghaili, A.M. A Proposed Conceptual Framework for Mobile Health Technology Adoption Among Employees at Workplaces in Malaysia. Adv. Intell. Syst. Comput. 2018, 843, 736–748. [Google Scholar] [CrossRef]
- Brito, J.M.C. Technological Trends for 5G Networks Influence of E-Health and IoT Applications. Res. Anthol. Dev. Optim. 5G Netw. Impact Soc. 2021, 2, 876–900. [Google Scholar]
- Idoudi, H. Smart Systems for E-Health: WBAN Technologies, Security and Applications; Springer: Cham, Switzerland, 2021. [Google Scholar]
- Papa, A.; Mital, M.; Pisano, P.; Del Giudice, M. E-Health and Wellbeing Monitoring Using Smart Healthcare Devices: An Empirical Investigation. Technol. Forecast. Soc. Chang. 2020, 153, 119226. [Google Scholar] [CrossRef]
- De Mattos, W.D.; Gondim, P.R.L. M-Health Solutions Using 5G Networks and M2M Communications. IT Prof. 2016, 18, 24–29. [Google Scholar] [CrossRef]
- Jin, X.; Yuan, Z.; Zhou, Z. Understanding the Antecedents and Effects of MHealth App Use in Pandemics: A Sequential Mixed-Method Investigation. Int. J. Environ. Res. Public Health 2023, 20, 834. [Google Scholar] [CrossRef]
- Akter, S.; Ray, P. Mhealth—An Ultimate Platform to Serve the Unserved. Yearb. Med. Inform. 2010, 94–100. [Google Scholar] [CrossRef]
- Mokhtari, F.; Shamshirsaz, M.; Latifi, M.; Foroughi, J. Nanofibers-Based Piezoelectric Energy Harvester for Self-Powered Wearable Technologies. Polymers 2020, 12, 2697. [Google Scholar] [CrossRef]
- Hayward, J.; Chansin, G.; Zervos, H. Wearable Technology 2017–2027: Markets, Players, Forecasts. IDTexEx Report. 2017. Available online: https://www.idtechex.com/en/research-report/wearable-technology-2017-2027-markets-players-forecasts/536 (accessed on 2 February 2021).
- Ometov, A.; Chukhno, O.; Simona, N.E.; Lohan, J. When Wearable Technology Meets Computing in Future Networks: A Road Ahead 1 PROJECT INFORMATION IN BRIEF. In Proceedings of the 18th ACM International Conference on Computing Frontiers, Virtual Event, Turin, Italy, 11–13 May 2021; 2021; pp. 185–190. [Google Scholar] [CrossRef]
- Nascimento, D.R.; Tortorella, G.L.; Fettermann, D. Association between the Benefits and Barriers Perceived by the Users in Smart Home Services Implementation. Kybernetes, 2022; ahead of print. [Google Scholar]
- Fettermann, D.C.; Echeveste, M.E.S. New Product Development for Mass Customization: A Systematic Review. Prod. Manuf. Res. 2014, 2, 266–290. [Google Scholar] [CrossRef]
- Calegari, L.P.; Barbosa, J.; Marodin, G.A.; Fettermann, D.C. A Conjoint Analysis to Consumer Choice in Brazil: Defining Device Attributes for Recognizing Customized Foods Characteristics. Food Res. Int. 2018, 109, 1–13. [Google Scholar] [CrossRef]
- Fettermann, D.C.; Cavalcante, C.G.S.; Ayala, N.F.; Avalone, M.C. Configuration of a Smart Meter for Brazilian Customers. Energy Policy 2020, 139, 111309. [Google Scholar] [CrossRef]
- Fettermann, D.C.; Borriello, A.; Pellegrini, A.; Rose, J.M.; Burke, P.F. Getting Smarter about Household Energy: The Who and What of Demand for Smart Meters. Build. Res. Inf. 2021, 49, 100–112. [Google Scholar] [CrossRef]
- Echeveste, M.E.S.; Rozenfeld, H.; Fettermann, D.D.C. Customizing Practices Based on the Frequency of Problems in New Product Development Process. Concurr. Eng. Res. Appl. 2017, 25, 245–261. [Google Scholar] [CrossRef]
- Gumz, J.; Fettermann, D.C. What Improves Smart Meters’ Implementation? A Statistical Meta-Analysis on Smart Meters’ Acceptance. Smart Sustain. Built Environ. 2021, 11, 1116–1136. [Google Scholar] [CrossRef]
- Gastaldi, L.; Lettieri, E.; Mandolfo, M. Consumer Adoption of Digital Technologies for Lifestyle Monitoring. In Proceedings of the 2019 IEEE 23rd International Symposium on Consumer Technologies (ISCT), Ancona, Italy, 19–21 June 2019; pp. 11–16. [Google Scholar] [CrossRef]
- Lulin, Z.; Owusu-Marfo, J.; Asante Antwi, H.; Antwi, M.O.; Xu, X. Nurses’ Readiness in the Adoption of Hospital Electronic Information Management Systems in Ghana: The Application of the Structural Equation Modeling and the UTAUT Model. Sage Open 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Moudud-Ul-Huq, S.; Sultana Swarna, R.; Sultana, M. Elderly and Middle-Aged Intention to Use m-Health Services: An Empirical Evidence from a Developing Country. J. Enabling Technol. 2021, 15, 23–39. [Google Scholar] [CrossRef]
- Hoque, M.R. An Empirical Study of MHealth Adoption in a Developing Country: The Moderating Effect of Gender Concern. BMC Med. Inform. Decis. Mak. 2016, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Binyamin, S.S.; Hoque, M.R. Understanding the Drivers of Wearable Health Monitoring Technology: An Extension of the Unified Theory of Acceptance and Use of Technology. Sustainability 2020, 12, 9605. [Google Scholar] [CrossRef]
- Talukder, M.S.; Sorwar, G.; Bao, Y.; Ahmed, J.U.; Palash, M.A.S. Predicting Antecedents of Wearable Healthcare Technology Acceptance by Elderly: A Combined SEM-Neural Network Approach. Technol. Forecast. Soc. Chang. 2020, 150, 119793. [Google Scholar] [CrossRef]
- Nisha, N.; Iqbal, M.; Rifat, A. The Changing Paradigm of Health and Mobile Phones: An Innovation in the Health Care System. J. Glob. Inf. Manag. 2019, 27, 19–46. [Google Scholar] [CrossRef]
- Talukder, M.S.; Chiong, R.; Bao, Y.; Hayat Malik, B. Acceptance and Use Predictors of Fitness Wearable Technology and Intention to Recommend: An Empirical Study. Ind. Manag. Data Syst. 2019, 119, 170–188. [Google Scholar] [CrossRef]
- Huang, C.Y.; Yang, M.C.; Huang, C.Y. An Empirical Study on Factors Influencing Consumer Adoption Intention of an Ai-Powered Chatbot for Health and Weight Management. Int. J. Perform. Eng. 2021, 17, 422–432. [Google Scholar] [CrossRef]
- Borenstein, L.H.M.; Higgins, J.; Rothstein, H. Introduction to Meta-Analysis; Wiley: New York, NY, USA, 2011. [Google Scholar]
- Gimpel, H.; Graf, V.; Graf-Drasch, V. A Comprehensive Model for Individuals’ Acceptance of Smart Energy Technology–A Meta-Analysis. Energy Policy 2020, 138, 111196. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. Manag. Inf. Syst. 2012, 36, 157–178. [Google Scholar] [CrossRef]
- Jayaseelan, R.; Koothoor, P.; Pichandy, C. Index Terms ICT, E-Health, UTAUT, Health Communication, Health Management, Medical Doctors. Technol. Accept. Med. India Anal. UTAUT Model Artic. Int. J. Sci. Technol. Res. 2020, 9, 3854–3857. [Google Scholar]
- Pal, D.; Arpnikanondt, C.; Funilkul, S.; Chutimaskul, W. The Adoption Analysis of Voice-Based Smart IoT Products. IEEE Internet Things J. 2020, 7, 10852–10867. [Google Scholar] [CrossRef]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding Consumer Acceptance of Healthcare Wearable Devices: An Integrated Model of UTAUT and TTF. Int. J. Med. Inform. 2020, 139, 104156. [Google Scholar] [CrossRef]
- Card, N.A. Applied Meta-Analysis for Social Science Research; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Brewster, L.; Mountain, G.; Wessels, B.; Kelly, C.; Hawley, M.; Fellow, T.; Dphil, B.W.; Frcslt, H.; Professor Of Health, C.; Research, S. Factors Affecting Front Line Staff Acceptance of Telehealth Technologies: A Mixed-Method Systematic Review. J. Adv. Nurs. 2014, 70, 21–33. [Google Scholar] [CrossRef]
- Hennemann, S.; Beutel, M.E.; Zwerenz, R. Drivers and Barriers to Acceptance of Web-Based Aftercare of Patients in Inpatient Routine Care: A Cross-Sectional Survey. J. Med. Internet Res. 2016, 18, e337. [Google Scholar] [CrossRef]
- Sadoughi, F.; Behmanesh, A.; Sayfouri, N. Internet of Things in Medicine: A Systematic Mapping Study. J. Biomed. Inform. 2020, 103, 103383. [Google Scholar] [CrossRef]
- Väisänen, J.; Koivumäki, T.; Lappi, M. Consumer Acceptance of Future My Data Based Preventive EHealth Services. J. Med. Internet Res. 2015, 19, e429. [Google Scholar]
- Yaraborough, A.K.; Smith, T.B. Technology Acceptance amongst Physicians. Med. Care Res. Rev. 2007, 64, 650–672. [Google Scholar] [CrossRef]
- Piotrowicz, E. The Management of Patients with Chronic Heart Failure: The Growing Role of e-Health. Expert Rev. Med. Devices 2017, 14, 271–277. [Google Scholar] [CrossRef]
- Hunter, J.E.; Schmidt, F.L. Methods of Meta-Analysis: Correcting Error and Bias in Research Findings; SAGE: Thousand Oaks, CA, USA, 2004. [Google Scholar]
- Rezaei, R.; Safa, L.; Ganjkhanloo, M.M. Understanding Farmers’ Ecological Conservation Behavior Regarding the Use of Integrated Pest Management—An Application of the Technology Acceptance Model. Glob. Ecol. Conserv. 2020, 22, e00941. [Google Scholar] [CrossRef]
- Wang, Y.N.; Jin, L.; Mao, H. Farmer Cooperatives’ Intention to Adopt Agricultural Information Technology—Mediating Effects of Attitude. Inf. Syst. Front. 2019, 21, 565–580. [Google Scholar] [CrossRef]
- Sagnier, C.; Loup-Escande, E.; Lourdeaux, D.; Thouvenin, I.; Valléry, G. User Acceptance of Virtual Reality: An Extended Technology Acceptance Model. Int. J. Hum. Computer Interact. 2020, 36, 993–1007. [Google Scholar] [CrossRef]
- Gumz, J.; Fettermann, D.C.; Sant’Anna, Â.M.O.; Tortorella, G. Social Influence as a Major Factor in Smart Meters’ Acceptance: Findings from Brazil. Results Eng. 2022, 15, 100510. [Google Scholar] [CrossRef]
- Nascimento, D.R.; Ciano, M.P.; Gumz, J.; Fettermann, D.C. The Acceptance Process of Smart Homes by Users: A Statistical Meta-Analysis. Behav. Inf. Technol. 2022. [Google Scholar] [CrossRef]
- Yuen, K.F.; Cai, L.; Qi, G.; Wang, X. Factors Influencing Autonomous Vehicle Adoption: An Application of the Technology Acceptance Model and Innovation Diffusion Theory. Technol. Anal. Strateg. Manag. 2021, 33, 505–519. [Google Scholar]
- Zhang, M.; Shu, L.; Luo, X.; Yuan, M.; Zheng, X. Virtual Reality Technology in Construction Safety Training: Extended Technology Acceptance Model. Autom. Constr. 2022, 135, 104113. [Google Scholar] [CrossRef]
- Lee, Y.H.; Hsieh, Y.C.; Chen, Y.H. An Investigation of Employees’ Use of e-Learning Systems: Applying the Technology Acceptance Model. Behav. Inf. Technol. 2013, 32, 173–189. [Google Scholar] [CrossRef]
- Lowe, B.; D’Alessandro, S.; Winzar, H.; Laffey, D.; Collier, W. The Use of Web 2.0 Technologies in Marketing Classes: Key Drivers of Student Acceptance. J. Consum. Behav. 2013, 12, 412–422. [Google Scholar] [CrossRef]
- Amirtha, R.; Sivakumar, V.J. Does Family Life Cycle Stage Influence E-Shopping Acceptance by Indian Women? An Examination Using the Technology Acceptance Model. Behav. Inf. Technol. 2018, 37, 267–294. [Google Scholar] [CrossRef]
- Taherdoost, H., II. Development of an Adoption Model to Assess User Acceptance of E-Service Technology: E-Service Technology Acceptance Model. Behav. Inf. Technol. 2018, 37, 173–197. [Google Scholar] [CrossRef]
- Mathew, V.; Soliman, M. Does Digital Content Marketing Affect Tourism Consumer Behavior? An Extension of t Echnology Acceptance Model. J. Consum. Behav. 2021, 20, 61–75. [Google Scholar] [CrossRef]
- Purohit, S.; Arora, R.; Paul, J. The Bright Side of Online Consumer Behavior: Continuance Intention for Mobile Payments. J. Consum. Behav. 2022, 21, 1–20. [Google Scholar] [CrossRef]
- Lee, E.J. Impact of Visual Typicality on the Adoption of Wearables. J. Consum. Behav. 2021, 20, 762–775. [Google Scholar] [CrossRef]
- Kwee-Meier, S.T.; Bützler, J.E.; Schlick, C. Development and Validation of a Technology Acceptance Model for Safety-Enhancing, Wearable Locating Systems. Behav. Inf. Technol. 2016, 35, 394–409. [Google Scholar] [CrossRef]
- Chauhan, S.; Jaiswal, M. A Meta-Analysis of e-Health Applications Acceptance: Moderating Impact of User Types and e-Health Application Types. J. Enterp. Inf. Manag. 2017, 30, 295–319. [Google Scholar] [CrossRef]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating Acceptance of Telemedicine Services through an Extended Technology Acceptance Model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Shemesh, T.; Barnoy, S. Assessment of the Intention to Use Mobile Health Applications Using a Technology Acceptance Model in an Israeli Adult Population. Telemed. e-Health 2020, 26, 1141–1149. [Google Scholar] [CrossRef]
- Davis, F. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 318–340. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Fishbein, M. Readings in Attitude Theory and Measurement; APA PsycNET: Washington, DC, USA, 1967. [Google Scholar]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. Manag. Inf. Syst. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Yousafzai, S.Y.; Foxall, G.R.; Pallister, J.G. Technology Acceptance: A Meta-analysis of the TAM: Part 2. J. Model. Manag. 2007, 2, 281–304. [Google Scholar] [CrossRef]
- Lai, Y.H.; Huang, F.F. A Study on the Intention to Use the Wearable Device in Taiwan: A Case Study on Xiaomi Mi Band. Adv. Intell. Syst. Comput. 2018, 661, 283–292. [Google Scholar] [CrossRef]
- Deng, Z.; Hong, Z.; Ren, C.; Zhang, W.; Xiang, F. What Predicts Patients’ Adoption Intention Toward MHealth Services in China: Empirical Study. JMIR mHealth uHealth 2018, 6, e9316. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.C.; Yang, S.Y.; Chang, Y.C. Predicting Older Adults’ Mobile Payment Adoption: An Extended TAM Model. Int. J. Environ. Res. Public Health 2023, 20, 1391. [Google Scholar] [CrossRef]
- Alsyouf, A.; Lutfi, A.; Alsubahi, N.; Alhazmi, F.N.; Al-Mugheed, K.; Anshasi, R.J.; Albugami, M. The Use of a Technology Acceptance Model (TAM) to Predict Patients’ Usage of a Personal Health Record System: The Role of Security, Privacy, and Usability. Int. J. Environ. Res. Public Health 2023, 20, 1347. [Google Scholar] [CrossRef]
- Patil, P.; Tamilmani, K.; Rana, N.P.; Raghavan, V. Understanding Consumer Adoption of Mobile Payment in India: Extending Meta-UTAUT Model with Personal Innovativeness, Anxiety, Trust, and Grievance Redressal. Int. J. Inf. Manag. 2020, 54, 102144. [Google Scholar] [CrossRef]
- Macdonald, E.M.; Perrin, B.M.; Hyett, N.; Kingsley, M.I.C. Factors Influencing Behavioural Intention to Use a Smart Shoe Insole in Regionally Based Adults with Diabetes: A Mixed Methods Study. J. Foot Ankle Res. 2019, 12, 29. [Google Scholar] [CrossRef]
- Quaosar, G.M.A.A.; Hoque, M.R.; Bao, Y. Investigating Factors Affecting Elderly’s Intention to Use m-Health Services: An Empirical Study. Telemed. e-Health 2018, 24, 309–314. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, M.; Fan, W.; Zhao, K. Understanding the Spread of COVID-19 Misinformation on Social Media: The Effects of Topics and a Political Leader’s Nudge. J. Assoc. Inf. Sci. Technol. 2022, 73, 726–737. [Google Scholar] [CrossRef]
- Reyhan Zaradi, D.; Suzianti, A.; Usman, X. Analysis of Technology Adoption Model on Health Monitoring via Smartwatches and Fitness Bands Across Generations in Indonesia. In Proceedings of the 5th International Conference on Communication and Information Processing, Chongqing, China, 15–17 November 2019. [Google Scholar] [CrossRef]
- Warshaw, P.R.; Davis, F.D. Disentangling Behavioral Intention and Behavioral Expectation. J. Exp. Soc. Psychol. 1985, 21, 213–228. [Google Scholar] [CrossRef]
- Brown, S.A.; Venkatesh, V. Model of Adoption of Technology in Households: A Baseline Model Test and Extension Incorporating Household Life Cycle. MIS Q. Manag. Inf. Syst. 2005, 29, 399–426. [Google Scholar] [CrossRef]
- Chang, A. UTAUT and UTAUT 2: A Review and Agenda for Future Research. Winners 2012, 13, 10–114. [Google Scholar] [CrossRef]
- Dodds, W.B. In Search of Value: How Price and Store Name Information Influence Buyers’ Product Perceptions. J. Consum. Mark. 1991, 8, 15–24. [Google Scholar] [CrossRef]
- Chang, C.-C. Exploring the Usage Intentions of Wearable Medical Devices: A Demonstration Study. Interact. J. Med. Res. 2020, 9, e19776. [Google Scholar] [CrossRef]
- Alam, M.M.D.; Alam, M.Z.; Rahman, S.A.; Taghizadeh, S.K. Factors Influencing mHealth Adoption and Its Impact on Mental Well-Being during COVID-19 Pandemic: A SEM-ANN Approach. J. Biomed. Inform. 2021, 116, 103722. [Google Scholar] [CrossRef]
- Limayem, M.; Hirt, S.G.; Cheung, C.M.K. How Habit Limits the Predictive Power of Intention: The Case of Information Systems Continuance. MIS Q. Manag. Inf. Syst. 2007, 31, 705–737. [Google Scholar] [CrossRef]
- Kim, S.H. A Study on Adoption Factors of Korean Smartphone Users: A Focus on TAM (Technology Acceptance Model) and UTAUT (Unified Theory of Acceptance and Use of Technology). Adv. Sci. Technol. Lett. 2014, 57, 27–30. [Google Scholar]
- Holden, R.J.; Karsh, B.T. The Technology Acceptance Model: Its Past and Its Future in Health Care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef]
- Alwi, S.S.E.; Murad, M.A.A. Online Information Seeking: A Review of the Literature in the Health Domain. Communities (OHCs) 2018, 2, 4. [Google Scholar]
- Octavius, G.S.; Antonio, F. Antecedents of Intention to Adopt Mobile Health (MHealth) Application and Its Impact on Intention to Recommend: An Evidence from Indonesian Customers. Int. J. Telemed. Appl. 2021, 2021, 1–14. [Google Scholar] [CrossRef]
- Tsai, T.H.; LIN, W.Y.; Chang, Y.S.; Chang, P.C.; Lee, M.Y. Technology Anxiety and Resistance to Change Behavioral Study of a Wearable Cardiac Warming System Using an Extended TAM for Older Adults. PLoS ONE 2020, 15, e0227270. [Google Scholar] [CrossRef] [PubMed]
- Elprama, S.A.; Vannieuwenhuyze, J.T.; De Bock, S.; Vanderborght, B.; De Pauw, K.; Meeusen, R.; Jacobs, A. Social Processes: What Determines Industrial Workers’ Intention to Use Exoskeletons? Hum. Factors 2020, 62, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Sinha, N.; Singh, P.; Chuah, S.H.W. Gender Differences in the Wearable Preferences, Device and Advertising Value Perceptions: Smartwatches vs. Fitness Trackers. Int. J. Technol. Mark. 2020, 14, 199–225. [Google Scholar] [CrossRef]
- Li, Q. Healthcare at Your Fingertips: The Acceptance and Adoption of Mobile Medical Treatment Services among Chinese Users. Int. J. Environ. Res. Public Health 2020, 17, 6895. [Google Scholar] [CrossRef] [PubMed]
- Reith, R.; Buck, C.; Lis, B.; Eymann, T. Tracking Fitness or Sickness—Combining Technology Acceptance and Privacy Research to Investigate the Actual Adoption of Fitness Trackers. In Proceedings of the Hawaii International Conference on System Sciences, Maui, HI, USA, 7–10 January 2020; pp. 3538–3547. [Google Scholar]
- Okpala, I.; Nnaji, C.; Awolusi, I. Wearable Sensing Devices Acceptance Behavior in Construction Safety and Health: Assessing Existing Models and Developing a Hybrid Conceptual Model. Constr. Innov. 2021, 22, 57–75. [Google Scholar] [CrossRef]
- Özdemir-Güngör, D.; Göken, M.; Basoglu, N.; Shaygan, A.; Dabić, M.; Daim, T.U. An Acceptance Model for the Adoption of Smart Glasses Technology by Healthcare Professionals. Int. Bus. Emerg. Econ. Firms 2020, 2, 163–194. [Google Scholar]
- Kim, T.B.; Ho, C.T.B. Validating the Moderating Role of Age in Multi-Perspective Acceptance Model of Wearable Healthcare Technology. Telemat. Inform. 2021, 61, 101603. [Google Scholar] [CrossRef]
- Chuah, S.H.W.; Rauschnabel, P.A.; Krey, N.; Nguyen, B.; Ramayah, T.; Lade, S. Wearable Technologies: The Role of Usefulness and Visibility in Smartwatch Adoption. Comput. Hum. Behav. 2016, 65, 276–284. [Google Scholar] [CrossRef]
- Lin, B.-S.; Wong, A.M.; Tseng, K.C. Community-Based ECG Monitoring System for Patients with Cardiovascular Diseases. J. Med. Syst. 2016, 40, 80. [Google Scholar] [CrossRef]
- Alaiad, A.; Alsharo, M.; Alnsour, Y. The Determinants of M-Health Adoption in Developing Countries: An Empirical Investigation. Appl. Clin. Inform. 2019, 10, 820–840. [Google Scholar] [CrossRef]
- Dickinger, A.; Arami, M.; Meyer, D. The Role of Perceived Enjoyment and Social Norm in the Adoption of Technology with Network Externalities. J. Comput. Inf. Syst. 2017, 17, 4–11. [Google Scholar] [CrossRef]
- Sun, Y.; Bhattacherjee, A. Looking inside the “It Black Box”: Technological Effects on It Usage. Eur. J. Inf. Syst. 2015, 54, 1–15. [Google Scholar] [CrossRef]
- Joe, S.; Kim, J.; Zemke, D.M.V. Effects of Social Influence and Perceived Enjoyment on Kiosk Acceptance: A Moderating Role of Gender. Int. J. Hosp. Tour. Adm. 2020, 23, 289–316. [Google Scholar] [CrossRef]
- Kanwal, F.; Rehman, M.; Asif, M.M. E-Learning Adoption and Acceptance in Pakistan: Moderating Effect of Gender and Experience. Mehran Univ. Res. J. Eng. Technol. 2020, 39, 324–341. [Google Scholar] [CrossRef]
- Scherer, R.; Teo, T. Editorial to the Special Section—Technology Acceptance Models: What We Know and What We (Still) Do Not Know. Br. J. Educ. Technol. 2019, 50, 2387–2393. [Google Scholar] [CrossRef]
- Arya, S.; Schwartz, T.A.; Ghaferi, A.A. Practical Guide to Meta-Analysis. JAMA Surg. 2020, 155, 430–431. [Google Scholar] [CrossRef]
- Gagnon, M.P.; Ngangue, P.; Payne-Gagnon, J.; Desmartis, M. M-Health Adoption by Healthcare Professionals: A Systematic Review. J. Am. Med. Inform. Assoc. 2016, 23, 212–220. [Google Scholar] [CrossRef]
- Harst, L.; Lantzsch, H.; Scheibe, M. Theories Predicting End-User Acceptance of Telemedicine Use: Systematic Review. J. Med. Internet Res. 2019, 21, e13117. [Google Scholar] [CrossRef]
- Kavandi, H.; Jaana, M. Factors That Affect Health Information Technology Adoption by Seniors: A Systematic Review. Health Soc. Care Community 2020, 28, 1827–1842. [Google Scholar] [CrossRef]
- Taherdoost, H. A Review of Technology Acceptance and Adoption Models and Theories. Procedia Manuf. 2018, 22, 960–967. [Google Scholar] [CrossRef]
- Tamilmani, K.; Rana, N.P.; Dwivedi, Y.K. Consumer Acceptance and Use of Information Technology: A Meta-Analytic Evaluation of UTAUT2. Inf. Syst. Front. 2021, 23, 987–1005. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Rana, N.P.; Jeyaraj, A.; Clement, M.; Williams, M.D. Re-Examining the Unified Theory of Acceptance and Use of Technology (UTAUT): Towards a Revised Theoretical Model. Inf. Syst. Front. 2019, 21, 719–734. [Google Scholar] [CrossRef]
- Hagger, M.S.; Polet, J.; Lintunen, T. The Reasoned Action Approach Applied to Health Behavior: Role of Past Behavior and Tests of Some Key Moderators Using Meta-Analytic Structural Equation Modeling. Soc. Sci. Med. 2018, 23, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, L.; Schnell, O.; Gehr, B.; Schloot, N.C.; Görgens, S.W.; Görgen, C. Digital Diabetes Management: A Literature Review of Smart Insulin Pens. J. Diabetes Sci. Technol. 2021, 16, 587–595. [Google Scholar] [CrossRef]
- Schroeders, U.; Kubera, F.; Gnambs, T. The Structure of the Toronto Alexithymia Scale (TAS-20): A Meta-Analytic Confirmatory Factor Analysis. Assessment 2021, 29, 1806–1823. [Google Scholar] [CrossRef]
- Sheeran, P.; Wright, C.E.; Avishai, A.; Villegas, M.E.; Lindemans, J.W.; Klein, W.M.; Ntoumanis, N. Self-Determination Theory Interventions for Health Behavior Change: Meta-Analysis and Meta-Analytic Structural Equation Modeling of Randomized Controlled Trials. J. Consult. Clin. Psychol. 2020, 88, 726. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: New York, NY, USA, 2021. [Google Scholar]
- Bitencourt, C.C.; de Oliveira Santini, F.; Zanandrea, G.; Froehlich, C.; Ladeira, W.J. Empirical Generalizations in Eco-Innovation: A Meta-Analytic Approach. J. Clean. Prod. 2020, 245, 118721. [Google Scholar] [CrossRef]
- de Oliveira Santini, F.; Ladeira, W.J.; Pinto, D.C.; Herter, M.M.; Sampaio, C.H.; Babin, B.J. Customer Engagement in Social Media: A Framework and Meta-Analysis. J. Acad. Mark. Sci. 2020, 48, 1211–1228. [Google Scholar] [CrossRef]
- Otto, A.S.; Szymanski, D.M.; Varadarajan, R. Customer Satisfaction and Firm Performance: Insights from over a Quarter Century of Empirical Research. J. Acad. Mark. Sci. 2019, 48, 543–564. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient Alpha and the Internal Structure of Tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Bacon, D.R.; Sauer, P.L.; Young, M. Composite Reliability in Structural Equations Modeling. Educ. Psychol. Meas. 1995, 55, 394–406. [Google Scholar] [CrossRef]
- Higgins, D.J.; McCabe, M.P.; Ricciardelli, L.A. Child Maltreatment, Family Characteristics and Adult Adjustment. J. Aggress. Maltreat. Trauma 2003, 6, 61–86. [Google Scholar] [CrossRef]
- Hunter, J.E.; Schmidt, F.L. Dichotomization of Continuous Variables: The Implications for Meta-Analysis. J. Appl. Psychol. 1990, 75, 334. [Google Scholar] [CrossRef]
- Nunnally, J.C. An Overview of Psychological Measurement. Clin. Diagn. Ment. Disord. 1978, 97–146. [Google Scholar] [CrossRef]
- Kijsanayotin, B.; Pannarunothai, S.; Speedie, S.M. Factors Influencing Health Information Technology Adoption in Thailand’s Community Health Centers: Applying the UTAUT Model. Int. J. Med. Inform. 2009, 78, 404–416. [Google Scholar] [CrossRef]
- Yen, P.Y.; McAlearney, A.S.; Sieck, C.J.; Hefner, J.L.; Huerta, T.R. Health Information Technology (HIT) Adaptation: Refocusing on the Journey to Successful HIT Implementation. JMIR Med. Inform. 2017, 5, e7476. [Google Scholar] [CrossRef]
- Rahman, M.S.; Das, S.; Hossain, G.M.S.; Tajrin, T. Teenagers’ Behavioural Intention towards Wearable Technologies and Intention to Recommend Others: An Empirical Study in Bangladesh. J. Sci. Technol. Policy Manag. 2021, 13, 110–131. [Google Scholar] [CrossRef]
- Rubin, A.; Ophoff, J. Investigating Adoption Factors of Wearable Technology in Health and Fitness. In Proceedings of the 2018 Open Innovations Conference (OI), Johannesburg, South Africa, 3–5 October 2018; pp. 176–186. [Google Scholar] [CrossRef]
- Alsswey, A.; Al-Samarraie, H. Elderly Users’ Acceptance of MHealth User Interface (UI) Design-Based Culture: The Moderator Role of Age. J. Multimodal User Interfaces 2020, 14, 49–59. [Google Scholar] [CrossRef]
- Kranthi, A.K.; Asraar Ahmed, K.A. Determinants of Smartwatch Adoption among IT Professionals—An Extended UTAUT2 Model for Smartwatch Enterprise. Int. J. Enterp. Netw. Manag. 2018, 9, 294–316. [Google Scholar] [CrossRef]
- Wu, B.; Chen, X. Continuance Intention to Use MOOCs: Integrating the Technology Acceptance Model (TAM) and Task Technology Fit (TTF) Model. Comput. Hum. Behav. 2017, 67, 221–232. [Google Scholar] [CrossRef]
- Wiegard, R.; Guhr, N.; Krylow, S.; Breitner, M.H. Analysis of Wearable Technologies’ Usage for Pay-as-You-Live Tariffs: Recommendations for Insurance Companies. Z. Gesamte Versicher. 2019, 108, 63–88. [Google Scholar] [CrossRef]
- Baba, N.M.; Suhaimi Baharudin, A.; Alomari, A.S. Determinants of User’s Inention to Use Smartwatch. J. Theor. Appl. Inf. Technol. 2019, 97, 4738–4750. [Google Scholar]
- Lunney, A.; Cunningham, N.R.; Eastin, M.S. Wearable Fitness Technology: A Structural Investigation into Acceptance and Perceived Fitness Outcomes. Comput. Human Behav. 2016, 65, 114–120. [Google Scholar] [CrossRef]
- Dahri, A.S.; Massan, S.-R.; Thebo, L.A. An Overview of AI Enabled M-IoT Wearable Technology and Its Effects on the Conduct of Medical Professionals in Public Healthcare in Pakistan. 3C Tecnol. Glosas Innov. Apl. Pyme 2020, 9, 87–111. [Google Scholar] [CrossRef]
- Reyes-Mercado, P. Adoption of Fitness Wearables: Insights from Partial Least Squares and Qualitative Comparative Analysis. J. Syst. Inf. Technol. 2018, 20, 103–127. [Google Scholar] [CrossRef]
- Wu, J.; Li, H.; Cheng, S.; Lin, Z. The Promising Future of Healthcare Services: When Big Data Analytics Meets Wearable Technology. Inf. Manag. 2016, 53, 1020–1033. [Google Scholar] [CrossRef]
- Ifinedo, P. Applying Uses and Gratifications Theory and Social Influence Processes to Understand Students’ Pervasive Adoption of Social Networking Sites: Perspectives from the Americas. Int. J. Inf. Manag. 2016, 36, 192–206. [Google Scholar] [CrossRef]
- Chang, Y.S.; Zhang, Y.; Gwizdka, J. Predicting Surrogates’ Health Information Seeking Behavior via Information Source and Information Evaluation. Proc. Assoc. Inf. Sci. Technol. 2021, 58, 36–47. [Google Scholar] [CrossRef]
- Vahdat, A.; Alizadeh, A.; Quach, S.; Hamelin, N. Would You like to Shop via Mobile App Technology? The Technology Acceptance Model, Social Factors and Purchase Intention. Australas. Mark. J. 2020, 29, 187–197. [Google Scholar] [CrossRef]
- Pluye, P.; El Sherif, R.; Granikov, V.; Hong, Q.N.; Vedel, I.; Galvao, M.C.B.; Grad, R. Health Outcomes of Online Consumer Health Information: A Systematic Mixed Studies Review with Framework Synthesis. J. Assoc. Inf. Sci. Technol. 2019, 70, 643–659. [Google Scholar] [CrossRef]
- Beh, P.K.; Ganesan, Y.; Iranmanesh, M.; Foroughi, B. Using Smartwatches for Fitness and Health Monitoring: The UTAUT2 Combined with Threat Appraisal as Moderators. Behav. Inf. Technol. 2019, 40, 282–299. [Google Scholar] [CrossRef]
- Li, J.; Ma, Q.; Chan, A.H.; Man, S.S. Health Monitoring through Wearable Technologies for Older Adults: Smart Wearables Acceptance Model. Appl. Ergon. 2019, 75, 162–169. [Google Scholar] [CrossRef]
- Hoque, M.R.; Bao, Y.; Sorwar, G. Investigating Factors Influencing the Adoption of E-Health in Developing Countries: A Patient’s Perspective. Inform. Health Soc. Care 2017, 42, 1–17. [Google Scholar] [CrossRef]
- Gao, Y.; Li, H.; Luo, Y. An Empirical Study of Wearable Technology Acceptance in Healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Lan, Z.; Liu, H.; Yang, C.; Liu, X.; Sorwar, G. Investigating Influencing Factors of Chinese Elderly Users’ Intention to Adopt MHealth Based on the UTAUT2 Model. In Proceedings of the Fourth International Conference on Biological Information and Biomedical Engineering, Chengdu, China, 21–23 July 2020; pp. 1–5. [Google Scholar] [CrossRef]
- Dhiman, N.; Arora, N.; Dogra, N.; Gupta, A. Consumer Adoption of Smartphone Fitness Apps: An Extended UTAUT2 Perspective. J. Indian Bus. Res. 2020, 12, 363–388. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Shareef, M.A.; Simintiras, A.C.; Lal, B.; Weerakkody, V. A Generalised Adoption Model for Services: A Cross-Country Comparison of Mobile Health (m-Health). Gov. Inf. Q. 2016, 33, 174–187. [Google Scholar] [CrossRef]
- Suki, N.M.; Suki, N.M. Exploring the Relationship between Perceived Usefulness, Perceived Ease of Use, Perceived Enjoyment, Attitude and Subscribers’ Intention towards Using 3G Mobile Services. J. Inf. Technol. Manag. 2011, 22, 1–7. [Google Scholar]
- Mahmood, N.; Lee, Y.A. Factors Influencing Older Adults’ Acceptance of Health Monitoring Smart Clothing. Fam. Consum. Sci. Res. J. 2021, 49, 376–392. [Google Scholar] [CrossRef]
- Becker, D. Acceptance of Mobile Mental Health Treatment Applications. Procedia Comput. Sci. 2016, 98, 220–227. [Google Scholar] [CrossRef]
- Bockting, W.; MacCrate, C.; Israel, H.; Mantell, J.E.; Remien, R.H. Engagement and Retention in HIV Care for Transgender Women: Perspectives of Medical and Social Service Providers in New York City. AIDS Patient Care STDS 2020, 34, 16–26. [Google Scholar] [CrossRef]
- Hilbert, J.; Yaggi, H.K. Patient-Centered Care in Obstructive Sleep Apnea: A Vision for the Future. Sleep Med. Rev. 2018, 37, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Shan, R.; Sarkar, S.; Martin, S.S. Digital Health Technology and Mobile Devices for the Management of Diabetes Mellitus: State of the Art. Diabetologia 2019, 62, 877–887. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wu, J.; Gao, Y.; Shi, Y. Examining Individuals’ Adoption of Healthcare Wearable Devices: An Empirical Study from Privacy Calculus Perspective. Int. J. Med. Inform. 2016, 88, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Xue, L.; Yen, C.C.; Chang, L.; Chan, H.C.; Tai, B.C.; Duh, H.B.L.; Choolani, M. A Study on Singaporean Women’s Acceptance of Using Mobile Phones to Seek Health Information. Int. J. Med. Inform. 2011, 80, e189–e202. [Google Scholar] [CrossRef] [PubMed]
- Salgado, T.; Tavares, J.; Oliveira, T. Drivers of Mobile Health Acceptance and Use From the Patient Perspective: Survey Study and Quantitative Model Development. JMIR mHealth uHealth 2020, 8, e17588. [Google Scholar] [CrossRef]
- Bhattacherjee, A.; Hikmet, N. Reconceptualizing Organizational Support and Its Effect on Information Technology Usage: Evidence from the Health Care Sector. J. Comput. Inf. Syst. 2008, 48, 69–76. [Google Scholar] [CrossRef]
- Seol, S.H.; Ko, D.S.; Yeo, I.S. UX Analysis Based on TR and UTAUT of Sports Smart Wearable Devices. KSII Trans. Internet Inf. Syst. 2017, 11, 4162–4179. [Google Scholar] [CrossRef]
- Tavares, J.; Oliveira, T. Electronic Health Record Portal Adoption: A Cross Country Analysis. BMC Med. Inform. Decis. Mak. 2017, 17, 1–17. [Google Scholar] [CrossRef]
- Khan, I.; Xitong, G.; Ahmad, Z.; Shahzad, F. Investigating Factors Impelling the Adoption of E-Health: A Perspective of African Expats in China. SAGE Open 2019, 9, 2158244019865803. [Google Scholar] [CrossRef]
- Gilbert, D.; Lee-Kelley, L.; Barton, M. Technophobia, Gender Influences and Consumer Decision-making for Technology-related Products. Eur. J. Innov. Manag. 2003, 6, 253–263. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, X.; Lai, K.H.; Guo, F.; Li, C. Understanding Gender Differences in M-Health Adoption: A Modified Theory of Reasoned Action Model. Telemed. e-Health 2013, 20, 39–46. [Google Scholar] [CrossRef]
- Dutta, B.; Peng, M.-H.; Sun, S.-L. Modeling the Adoption of Personal Health Record (PHR) among Individual: The Effect of Health-Care Technology Self-Efficacy and Gender Concern. Libyan J. Med. 2018, 13, 1500349. [Google Scholar] [CrossRef]
- Ono, H.; Zavodny, M. Gender and the Internet. Soc. Sci. Q. 2003, 84, 111–121. [Google Scholar] [CrossRef]
- Van Slyke, C.; Conca, C.; Trimmer, K. 9 Requirements for SME Information Technology. Globalisation and SMEs in East Asia; Edward Elgar Publishing: Cheltenham, UK, 2002. [Google Scholar]
- Cimperman, M.; Brenčič, M.M.; Trkman, P. Analyzing Older Users’ Home Telehealth Services Acceptance Behavior—Applying an Extended UTAUT Model 90. Int. J. Med. Inform. 2016, 90, 22–31. [Google Scholar] [CrossRef]
- Chang, C.M.; Liu, L.W.; Huang, H.C.; Hsieh, H.H. Factors Influencing Online Hotel Booking: Extending UTAUT2 with Age, Gender, and Experience as Moderators. Information 2019, 10, 281. [Google Scholar] [CrossRef]
- Choi, W. Older Adults’ Credibility Assessment of Online Health Information: An Exploratory Study Using an Extended Typology of Web Credibility. J. Assoc. Inf. Sci. Technol. 2020, 71, 1295–1307. [Google Scholar] [CrossRef]
- Vaziri, D.D.; Giannouli, E.; Frisiello, A.; Kaartinen, N.; Wieching, R.; Schreiber, D.; Wulf, V. Exploring Influencing Factors of Technology Use for Active and Healthy Ageing Support in Older Adults. Behav. Inf. Technol. 2020, 39, 1011–1021. [Google Scholar] [CrossRef]
- Mitzner, T.L.; Boron, J.B.; Fausset, C.B.; Adams, A.E.; Charness, N.; Czaja, S.J.; Sharit, J. Older Adults Talk Technology: Technology Usage and Attitudes. Comput. Hum. Behav. 2010, 26, 1710–1721. [Google Scholar] [CrossRef]
- Heinz, M.; Martin, P.; Margrett, J.A.; Yearns, M.; Franke, W.; Yang, H.I.; Wong, J.; Chang, C.K. Perceptions of Technology among Older Adults. J. Gerontol. Nurs. 2013, 39, 42–51. [Google Scholar] [CrossRef]
- Peek, S.T.M.; Wouters, E.J.M.; van Hoof, J.; Luijkx, K.G.; Boeije, H.R.; Vrijhoef, H.J.M. Factors Influencing Acceptance of Technology for Aging in Place: A Systematic Review. Int. J. Med. Inform. 2014, 83, 235–248. [Google Scholar] [CrossRef]
- Böhm, B.; Karwiese, S.D.; Böhm, H.; Oberhoffer, R. Effects of Mobile Health Including Wearable Activity Trackers to Increase Physical Activity Outcomes among Healthy Children and Adolescents: Systematic Review. JMIR mHealth uHealth 2019, 7, e8298. [Google Scholar] [CrossRef]
- Huvila, I.; Cajander, Å.; Daniels, M.; Åhlfeldt, R.M. Patients’ Perceptions of Their Medical Records from Different Subject Positions. J. Assoc. Inf. Sci. Technol. 2015, 66, 2456–2470. [Google Scholar] [CrossRef]
- Ndifon, N.M.; Bawack, R.E.; Kamdjoug, J.R.K. Adoption of Mobile Health Insurance Systems in Africa: Evidence from Cameroon. Health Technol. 2020, 10, 1095–1106. [Google Scholar] [CrossRef]
- Meier, D.Y.; Barthelmess, P.; Sun, W.; Liberatore, F. Wearable Technology Acceptance in Health Care Based on National Culture Differences: Cross-Country Analysis Between Chinese and Swiss Consumers. J. Med. Internet Res. 2020, 22, e18801. [Google Scholar] [CrossRef] [PubMed]
- Pai, R.R.; Alathur, S. Determinants of Mobile Health Application Awareness and Use in India: An Empirical Analysis. In Proceedings of the 13th International Conference on Theory and Practice of Electronic Governance, Athens, Greece, 23–25 September 2020; Volume 20, pp. 23–25. [Google Scholar] [CrossRef]
- Huang, C.Y.; Yang, M.C. Empirical Investigation of Factors Influencing Consumer Intention to Use an Artificial Intelligence-Powered Mobile Application for Weight Loss and Health Management. Telemed. e-Health 2020, 26, 1240–1251. [Google Scholar] [CrossRef]
- Niknejad, N.; Hussin, A.R.C.; Ghani, I.; Ganjouei, F.A. A Confirmatory Factor Analysis of the Behavioral Intention to Use Smart Wellness Wearables in Malaysia. Univers. Access Inf. Soc. 2019, 19, 633–653. [Google Scholar] [CrossRef]
- Liao, H.Y.; Chen, J.K. Comparison of Acceptance in Mobile Smart Wearable Technology between SEM and DEMATEL Methods. In Proceedings of the 2020 International Wireless Communications and Mobile Computing (IWCMC), Limassol, Cyprus, 15–19 June 2020; pp. 1413–1417. [Google Scholar] [CrossRef]
- Klinker, K.; Wiesche, M. Smart Glasses in Health Care: A Patient Trust Perspective. In Proceedings of the Hawaii International Conference on System Sciences, Maui, HI, USA, 7–10 January 2020; pp. 3548–3557. [Google Scholar] [CrossRef]
- Saheb, T. An Empirical Investigation of the Adoption of Mobile Health Applications: Integrating Big Data and Social Media Services. Health Technol. 2020, 10, 1063–1077. [Google Scholar] [CrossRef]
- Vongurai, R. Factors Influencing Intention to Use Fitness Trackers: A Case Study on Thais’ Living in Bangkok. Int. J. Econ. Bus. Adm. 2020, 8, 457–477. [Google Scholar] [CrossRef]
- Cheung, M.L.; Leung, W.K.S.; Chan, H. Driving Healthcare Wearable Technology Adoption for Generation Z Consumers in Hong Kong. Young Consum. 2020, 22, 10–27. [Google Scholar] [CrossRef]
- Alam, M.Z.; Alam, M.M.D.; Uddin, M.A.; Mohd Noor, N.A. Do Mobile Health (mHealth) Services Ensure the Quality of Health Life? An Integrated Approach from a Developing Country Context. J. Mark. Commun. 2020, 28, 152–182. [Google Scholar] [CrossRef]
- Kim, T.; Chiu, W. Consumer Acceptance of Sports Wearable Technology: The Role of Technology Readiness. Int. J. Sport. Mark. Spons. 2019, 20, 109–126. [Google Scholar] [CrossRef]
- ALsswey, A.; Naufal, I.; Bervell, B. Investigating the Acceptance of Mobile Health Application User Interface Cultural-Based Design to Assist Arab Elderly Users. Int. J. Adv. Comput. Sci. Appl. 2018, 9, 144–152. [Google Scholar] [CrossRef]
- Mital, M.; Chang, V.; Choudhary, P.; Papa, A.; Pani, A.K. Adoption of Internet of Things in India: A Test of Competing Models Using a Structured Equation Modeling Approach. Technol. Forecast. Soc. Chang. 2018, 136, 339–346. [Google Scholar] [CrossRef]
- Lee, S.J.; Choi, M.J.; Rho, M.J.; Kim, D.J.; Choi, I.Y. Factors Affecting User Acceptance in Overuse of Smartphones in Mobile Health Services: An Empirical Study Testing a Modified Integrated Model in South Korea. Front. Psychiatry 2018, 9, 658. [Google Scholar] [CrossRef]
- Chen, M.F.; Lin, N.P. Incorporation of Health Consciousness into the Technology Readiness and Acceptance Model to Predict App Download and Usage Intentions. Internet Res. 2018, 28, 351–373. [Google Scholar] [CrossRef]
- Rupp, M.A.; Michaelis, J.R.; McConnell, D.S.; Smither, J.A. The Role of Individual Differences on Perceptions of Wearable Fitness Device Trust, Usability, and Motivational Impact. Appl. Ergon. 2018, 70, 77–87. [Google Scholar] [CrossRef]
- Rajanen, D.; Weng, M. Digitization for Fun or Reward? A Study of Acceptance of Wearable Devices for Personal Healthcare. In Proceedings of the 21st International Academic Mindtrek Conference, Tampere, Finland, 20–21 September 2017; pp. 154–163. [Google Scholar] [CrossRef]
- Khakurel, J.; Knutas, A.; Immonen, M.; Porras, J. Intended Use of Smartwatches and Pedometers in the University Environment: An Empirical Analysis. In Proceedings of the 2017 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2017 ACM International Symposium on Wearable Computers, Maui, HI, USA, 11–15 September 2017; pp. 97–100. [Google Scholar] [CrossRef]
- Lee, E.; Han, S.; Jo, S.H. Consumer Choice of On-Demand mHealth App Services: Context and Contents Values Using Structural Equation Modeling. Int. J. Med. Inform. 2017, 97, 229–238. [Google Scholar] [CrossRef]
- Zhang, X.; Han, X.; Dang, Y.; Meng, F.; Guo, X.; Lin, J. User Acceptance of Mobile Health Services from Users’ Perspectives: The Role of Self-Efficacy and Response-Efficacy in Technology Acceptance. Inform. Health Soc. Care 2017, 42, 194–206. [Google Scholar] [CrossRef]
- Könsgen, R.; Schaarschmidt, M.; Vasylieva, O. Understanding Patients’ Intentions to Use mHealth Services A User-Centered Perspective of mHealth: Understanding Patients’ Intentions to Use Mobile Video Consultation Services. In Proceedings of the Americas Conference on Information Systems (AMCIS), Boston, MA, USA, 10–12 August 2017. [Google Scholar]
- Miao, R.; Wu, Q.; Wang, Z.; Zhang, X.; Song, Y.; Zhang, H.; Sun, Q.; Jiang, Z. Factors That Influence Users’ Adoption Intention of Mobile Health: A Structural Equation Modeling Approach. Int. J. Prod. Res. 2017, 55, 5801–5815. [Google Scholar] [CrossRef]
- Nisha, N.; Iqbal, M.; Rifat, A.; Idrish, S. Exploring the Role of Service Quality and Knowledge for Mobile Health Services. Int. J. E-Bus. Res. 2016, 12, 45–64. [Google Scholar] [CrossRef]
- Cho, I.; Park, H. The Influential Factors on the Diffusion of Smartwatches in Korea. Int. J. Technol. Manag. 2016, 72, 230–251. [Google Scholar] [CrossRef]
- Moon, Y.J.; Hwang, Y.H.; Cho, S. An Empirical Study of Impacts of User Intention for Smart Wearable Devices and Use Behavior. Lect. Notes Electr. Eng. 2016, 354, 357–365. [Google Scholar] [CrossRef]
- Pfeiffer, J.; Von Entreß-Fürsteneck, M.; Urbach, N.; Buchwald, A. Quantify-Me: Consumer Acceptance of Wearable Self-Tracking Devices. In Proceedings of the Twenty-Fourth European Conference on Information Systems (ECIS), Istanbul, Turkey, 12–15 June 2016. [Google Scholar]
- Nisha, N.; Iqbal, M.; Rifat, A.; Idrish, S. Mobile Health Services: A New Paradigm for Health Care Systems. Int. J. Asian Bus. Inf. Manag. 2015, 6, 1–17. [Google Scholar] [CrossRef]
- Olaleye, S.A.; Sanusi, I.T.; Agjei, R.O.; Adusei-Mensah, F. Please Call My Contact Person: Mobile Devices for a Rescue Mission during an Emergency. Inf. Discov. Deliv. 2021, 49, 114–122. [Google Scholar] [CrossRef]
- Mbelwa, J.T.; Kimaro, H.C.; Mussa, B. Acceptability and Use of Mobile Health Applications in Health Information Systems: A Case of EIDSR and DHIS2 Touch Mobile Applications in Tanzania. IFIP Adv. Inf. Commun. Technol. 2019, 551, 579–592. [Google Scholar] [CrossRef]
- Wang, S.L.; Lin, H.I. Integrating TTF and IDT to Evaluate User Intention of Big Data Analytics in Mobile Cloud Healthcare System. Behav. Inf. Technol. 2019, 38, 974–985. [Google Scholar] [CrossRef]
- Sergueeva, K.; Shaw, N. Improving Healthcare with Wearables: Overcoming the Barriers to Adoption. In HCI in Business, Government and Organizations. Proceedings of the Interacting with Information Systems: 4th International Conference, HCIBGO 2017, Held as Part of HCI International 2017, Vancouver, BC, Canada, 9–14 July 2017; Springer: Cham, Switzerland, 2017; pp. 209–223. [Google Scholar] [CrossRef]
- Ali, R.; Zhang, Z.; Soomro, M.B. Smoking-Cessation Acceptance via Mobile Health and Quick Response Code Technologies: Empirical Evidence of a Pilot Study from China and Pakistan. Curr. Psychol. 2019, 40, 6085–6097. [Google Scholar] [CrossRef]
- Cho, J. The Impact of Post-Adoption Beliefs on the Continued Use of Health Apps. Int. J. Med. Inform. 2016, 87, 75–83. [Google Scholar] [CrossRef]
- Gallos, P.; Mantas, J. The “SMART Travel Health” Mobile Application Assessment. In ICIMTH; IOS Press: Amsterdam, The Netherlands, 2015; pp. 227–229. [Google Scholar]
- Gangadharbatla, H. Biohacking: An Exploratory Study to Understand the Factors Influencing the Adoption of Embedded Technologies within the Human Body. Heliyon 2020, 6, e03931. [Google Scholar] [CrossRef]
- Aksoy, N.C.; Kocak Alan, A.; Tumer Kabadayi, E.; Aksoy, A. Individuals’ Intention to Use Sports Wearables: The Moderating Role of Technophobia. Int. J. Sport. Mark. Spons. 2020, 21, 225–245. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Wang, L.; Zhang, Y.; Wang, J. Mobile Health Service Adoption in China: Integration of Theory of Planned Behavior, Protection Motivation Theory and Personal Health Differences. Online Inf. Rev. 2020, 44, 1–23. [Google Scholar] [CrossRef]
- Zhu, Y.; Dailey, S.L.; Kreitzberg, D.; Bernhardt, J. “Social Networkout”: Connecting Social Features of Wearable Fitness Trackers with Physical Exercise. J. Health Commun. 2017, 22, 974–980. [Google Scholar] [CrossRef]
- Schuster, L.; Tossan, V.; Drennan, J. Consumer Acceptance of mHealth Services: A Comparison of Behavioral Intention Models. Serv. Mark. Q. 2017, 38, 115–128. [Google Scholar] [CrossRef]
- Guo, X.; Zhang, X.; Sun, Y. The Privacy–Personalization Paradox in MHealth Services Acceptance of Different Age Groups. Electron. Commer. Res. Appl. 2016, 16, 55–65. [Google Scholar] [CrossRef]
- Wu, L.-H.; Wu, L.-C.; Chang, S.-C. Exploring consumers’ intention to accept smartwatch. Comput. Hum. Behav. 2016, 64, 383–392. [Google Scholar] [CrossRef]
| Search Field | Technologies | Acceptance of New Technology | Models of Technolgy Acceptance | Statistical Methods | |||
|---|---|---|---|---|---|---|---|
| Search keywords | (m-health AND Health) OR (m-health AND Fitness) OR (Wearable AND Health) OR (Wearable AND Fitness) | AND | (User AND Accept*) OR (User AND Engag*) | AND | Technology Acceptance Model OR TAM OR Decomposed Theory of Planned Behavior OR DTPB OR Theory of Planned Behavior OR TPB OR Model of PC Utilization OR MPCU OR Theory of Reasoned Action OR TRA OR Innovation Diffusion Theory OR Motivational Model OR MM OR Social Cognitive Theory OR SCT OR Unified Theory of Acceptance and Use of Technology OR UTAUT OR Unified Theory of Acceptance and Use of Technology 2 OR UTAUT2 | AND | Partial Least Squares OR Structural Equation Modeling |
| EP | EE | AT | IS | CF | MH | HB | VP | RP | IC | CU | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Average reliability | 0.830 | 0.841 | 0.787 | 0.848 | 0.821 | 0.876 | 0.859 | 0.831 | 0.878 | 0.852 | 0.855 |
| Minimun | 0.657 | 0.650 | 0.700 | 0.642 | 0.690 | 0.779 | 0.649 | 0.700 | 0.700 | 0.652 | 0.700 |
| Maximum | 0.978 | 0.970 | 0.968 | 0.970 | 0.945 | 0.976 | 0.973 | 0.940 | 0.952 | 0.976 | 0.972 |
| Number of samples | 74 | 71 | 21 | 44 | 35 | 21 | 9 | 11 | 8 | 76 | 9 |
| Relations | N (Total) | K (Estudies) | Coefficient | Confidence Interval (95%) | Estat. Θ | p-Value |
|---|---|---|---|---|---|---|
| PE > BI | 26,098 | 77 | 0.339 | [0.293; 0.385] | 14.30 | <0.01 ** |
| PE > AT | 7030 | 17 | 0.525 | [0.475; 0.575] | 20.54 | <0.01 ** |
| EE > PE | 9028 | 21 | 0.468 | [0.389; 0.548] | 11.53 | <0.01 ** |
| EE > BI | 21,358 | 67 | 0.232 | [0.188; 0.277] | 10.22 | <0.01 ** |
| EE > AT | 5901 | 16 | 0.349 | [0.270; 0.428] | 8.640 | <0.01 ** |
| AT > BI | 2093 | 10 | 0.647 | [0.510; 0.784] | 9.250 | <0.01 ** |
| SI > BI | 18,600 | 57 | 0.280 | [0.224; 0.337] | 9.740 | <0.01 ** |
| FC > BI | 14,492 | 43 | 0.164 | [0.118; 0.211] | 6.940 | <0.01 ** |
| FC > UB | 1812 | 5 | 0.279 | [0.124; 0.434] | 3.530 | <0.01 ** |
| HM > BI | 6531 | 24 | 0.115 | [0.113; 0.116] | 147.8 | <0.01 ** |
| HB > BI | 2526 | 9 | 0.364 | [0.236; 0.492] | 5.580 | <0.01 ** |
| PV > BI | 3462 | 12 | 0.148 | [−0.040; 0.336] | 1.540 | 0.12 |
| PR > BI | 3519 | 8 | −0.160 | [−0.256; −0.070] | −3.340 | <0.01 ** |
| BI > UB | 5438 | 10 | 0.488 | [0.358; 0.618] | 7.350 | <0.01 ** |
| Moderator | Coef | Std. Error | Z | p > |z| | I2 (%) |
|---|---|---|---|---|---|
| PE > BI | |||||
| Gender | −0.20 | 0.21 | −0.97 | 0.33 | 99.97 |
| Age Range | 0.16 | 0.11 | 1.48 | 0.13 | |
| Timeline | −0.09 | 0.10 | −0.87 | 0.38 | |
| PE > AT | |||||
| Gender | 0.50 | 0.16 | 2.98 | <0.01 ** | 99.93 |
| Age Range | 0.13 | 0.08 | 1.53 | 0.12 | |
| Timeline | −0.44 | 0.10 | −4.06 | <0.01 ** | |
| EE > PE | |||||
| Gender | −0.06 | 0.27 | −0.25 | 0.80 | 99.86 |
| Age Range | 0.12 | 0.10 | 0.11 | 0.91 | |
| Timeline | −0.24 | 0.14 | −1.7 | 0.08 | |
| EE > BI | |||||
| Gender | 0.76 | 0.21 | 3.50 | <0.01 ** | 99.97 |
| Age Range | 0.14 | 0.11 | 1.27 | 0.20 | |
| Timeline | 0.05 | 0.10 | 0.53 | 0.59 | |
| EE > AT | |||||
| Gender | 1.05 | 0.29 | 3.61 | <0.01 ** | 99.89 |
| Age Range | 0.57 | 0.12 | 4.52 | <0.01 ** | |
| Timeline | −0.53 | 0.19 | −2.78 | <0.01 ** | |
| AT > BI | |||||
| Gender | 0.44 | 0.05 | 8.00 | <0.01 ** | 88.21 |
| Age Range | 0.58 | 0.02 | 24.32 | <0.01 ** | |
| Timeline | −0.30 | 0.03 | −7.64 | <0.01 ** | |
| SI > BI | |||||
| Gender | −0.16 | 0.22 | −0.73 | 0.46 | 99.98 |
| Age Range | 0.31 | 0.15 | 1.99 | 0.04 * | |
| Timeline | −0.26 | 0.11 | −2.25 | 0.02 * | |
| FC > BI | |||||
| Gender | −0.31 | 0.18 | −1.68 | 0.09 | 99.95 |
| Age Range | 0.13 | 0.10 | 1.22 | 0.22 | |
| Timeline | −0.18 | 0.08 | −2.23 | 0.02 * | |
| FC > UB | |||||
| Gender | 0 | - | −2.22 | 0.02 * | 99.98 |
| Age Range | −0.85 | 0.38 | 2.09 | 0.03 * | |
| Timeline | 1.27 | 0.61 | 2.42 | 0.01 * | |
| HM > BI | |||||
| Gender | <0.01 | <0.01 | 0.97 | <0.01 ** | 3.37 |
| Age Range | 0.06 | <0.01 | 19.68 | 0.06 | |
| Timeline | 0.16 | <0.01 | 61.97 | 0.16 | |
| HB > BI | |||||
| Gender | 0.01 | 0.22 | 0.08 | 0.93 | 99.49 |
| Age Range | 0.84 | 0.10 | 8.06 | <0.01 ** | |
| Timeline | −0.17 | 0.07 | −2.22 | 0.02 * | |
| PV > BI | |||||
| Gender | 0.15 | 0.23 | 0.69 | 0.49 | 99.56 |
| Age Range | −0.07 | 0.20 | −0.36 | 0.71 | |
| Timeline | 0.01 | 0.19 | 0.06 | 0.95 | |
| PR > BI | |||||
| Gender | 1.05 | 0.35 | 2.93 | <0.01 ** | 99.68 |
| Age Range | 0.03 | 0.15 | 0.24 | 0.80 | |
| Timeline | 0.36 | 0.12 | 2.85 | <0.01 ** | |
| BI > UB | |||||
| Gender | 0.27 | 0.69 | 0.39 | 0.69 | 99.99 |
| Age Range | 0.18 | 0.23 | 0.77 | 0.44 | |
| Timeline | 0.23 | 0.22 | 1.04 | 0.29 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calegari, L.P.; Tortorella, G.L.; Fettermann, D.C. Getting Connected to M-Health Technologies through a Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4369. https://doi.org/10.3390/ijerph20054369
Calegari LP, Tortorella GL, Fettermann DC. Getting Connected to M-Health Technologies through a Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(5):4369. https://doi.org/10.3390/ijerph20054369
Chicago/Turabian StyleCalegari, Luiz Philipi, Guilherme Luz Tortorella, and Diego Castro Fettermann. 2023. "Getting Connected to M-Health Technologies through a Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 5: 4369. https://doi.org/10.3390/ijerph20054369
APA StyleCalegari, L. P., Tortorella, G. L., & Fettermann, D. C. (2023). Getting Connected to M-Health Technologies through a Meta-Analysis. International Journal of Environmental Research and Public Health, 20(5), 4369. https://doi.org/10.3390/ijerph20054369








