Motivational Interviewing and Childhood Caries: A Randomised Controlled Trial
Abstract
1. Introduction
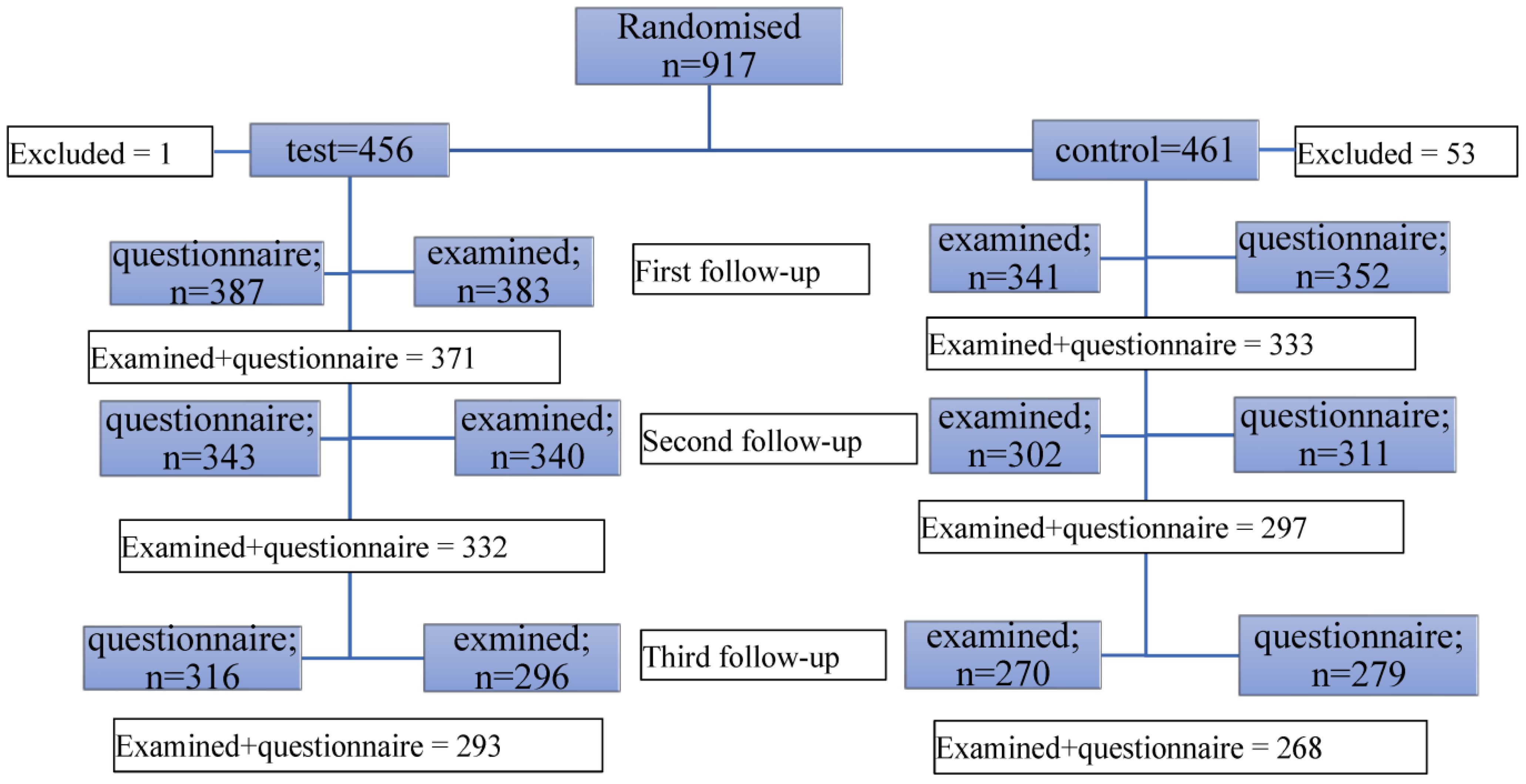
2. Materials and Methods
- rapport establishment and identification of oral health and nutritional needs using empathic reflective listening;
- presentation of a menu of options and information with permission;
- discussion of options and elicitation of “change talk”;
- elicitation of parental importance and confidence in behavioural change;
- the development of a behaviour change plan; and
- a schedule of follow-up.
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arrow, P.; Raheb, J.; Miller, M. Brief oral health promotion intervention among parents of young children to reduce early childhood dental decay. BMC Public Health 2013, 13, 245. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-245 (accessed on 1 November 2022). [CrossRef]
- Ha, D.H.; Roberts-Thomson, K.F.; Arrow, P.; Peres, K.G.; Do, L.G. Children’s Oral Health Status in Australia, 2012–2014. In Oral Health of Australian Children: The National Child Oral Health Study 2012-14; Do, L.G., Spencer, A.J., Eds.; University of Adelaide Press: Adelaide, Australia, 2016; pp. 86–152. [Google Scholar]
- Alcaino, E.; Kilpatrick, N.; Kingsford Smith, E. Utilization of day stay general anaesthesia for the provision of dental treatment to children in New South Wales, Australia. Int. J. Paediatr. Dent. 2000, 10, 206–212. [Google Scholar] [CrossRef]
- Hallett, K.; O’Rourke, P. Caries experience in pre-school children referred for specialist dental care in hospital. Aust. Dent. J. 2006, 51, 124–129. [Google Scholar] [CrossRef]
- Gomes, M.C.; Pinto-Sarmento, T.C.; Costa, E.M.; Martins, C.C.; Granville-Garcia, A.F.; Paiva, S.M. Impact of oral health conditions on the quality of life of preschool children and their families: A cross-sectional study. Health Qual. Life Outcomes 2014, 12, 55. [Google Scholar] [CrossRef]
- Kramer, P.; Feldens, C.; Ferreira, S.; Bervian, J.; Rodrigues, P.; Peres, M. Exploring the impact of oral diseases and disorders on quality of life of preschool children. Community Dent. Oral Epidemiol. 2013, 41, 327–335. [Google Scholar] [CrossRef]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on children’s oral health: A conceptual model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef]
- Kay, E.J.; Locker, D. Is dental health education effective? A systematic review of current evidence. Community Dent. Oral Epidemiol. 1996, 24, 231–235. [Google Scholar] [CrossRef]
- Stein, C.; Santos, N.M.L.; Hilgert, J.B.; Hugo, F.N. Effectiveness of oral health education on oral hygiene and dental caries in schoolchildren: Systematic review and meta-analysis. Community Dent. Oral Epidemiol. 2017, 46, 30–37. [Google Scholar] [CrossRef]
- Weinstein, P.; Harrison, R.; Benton, T. Motivating parents to prevent caries in their young children: One-year findings. J. Am. Dent. Assoc. 2004, 135, 731–738. [Google Scholar] [CrossRef]
- Rollnick, S.; Miller, W.; Butler, C. Motivational Interviewing in Health Care: Helping Patients Change Behaviour; The Guildford Press: New York, NY, USA, 2008. [Google Scholar]
- Naidu, R.; Nunn, J.; Irwin, J.D. The effect of motivational interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: An exploratory cluster randomised controlled study. BMC Oral Health 2015, 15, 101. Available online: https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-015-0068-9 (accessed on 1 November 2022). [CrossRef] [PubMed]
- Harrison, R.; Benton, T.; Everson-Stewart, S.; Weinstein, P. Effect of motivational interviewing on rates of early childhood caries: A randomized trial. Pediatr. Dent. 2007, 29, 16–22. [Google Scholar] [PubMed]
- Weinstein, P.; Harrison, R.; Benton, T. Motivating mothers to prevent caries: Confirming the beneficial effect of counselling. J. Am. Dent. Assoc. 2006, 137, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Plonka, K.; Pukallus, M.; Barnett, A.; Holcombe, T.; Walsh, L.; Seow, W. A controlled, longitudinal study of home visits compared to telephone contacts to prevent early childhood caries. Int. J. Paediatr. Dent. 2013, 23, 23–31. [Google Scholar] [CrossRef]
- Harrison, R.; Veronneau, J.; Leroux, B. Effectiveness of maternal counseling in reducing caries in Cree children. J. Dent. Res. 2012, 91, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Ismail, A.; Ondersma, S.; Jedele, J.; Little, R.; Lepkowski, J. Evaluation of a brief tailored motivational intervention to prevent early childhood caries. Community Dent. Oral Epidemiol. 2011, 39, 433–448. [Google Scholar] [CrossRef]
- Albino, J.; Tiwari, T. Preventing childhood caries: A review of recent behavioral research. J. Dent. Res. 2016, 95, 35–42. [Google Scholar] [CrossRef]
- Yevlahova, D.; Satur, J. Models for individual oral health promotion and their effectiveness: A systematic review. Aust. Dent. J. 2009, 54, 190–197. [Google Scholar] [CrossRef]
- Colvara, B.C.; Faustino-Silva, D.D.; Meyer, E.; Hugo, F.N.; Celeste, R.K.; Hilgert, J.B. Motivational interviewing for preventing early childhood caries: A systematic review and meta-analysis. Community Dent. Oral Epidemiol. 2021, 49, 10–16. [Google Scholar] [CrossRef]
- Faghihian, R.; Faghihiam, E.; Kazemi, A.; Tarrahi, M.J.; Zakizade, M. Impact of motivational interviewing on early childhood caries:A systematic review and meta-analysis. J. Am. Dent. Assoc. 2020, 151, 650–659. [Google Scholar] [CrossRef]
- Plutzer, K.; Spencer, A. Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dent. Oral Epidemiol. 2008, 36, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.; Rose, G. Toward a theory of motivational interviewing. Am. Psychol. 2009, 64, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Finlayson, T.; Siefert, K.; Ismail, A.; Sohn, W. Psychosocial factors and early childhood caries among low-income African-American children in Detroit. Community Dent. Oral Epidemiol. 2007, 35, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Albino, J.; Centers, E.C.C.C.; Tiwari, T.; Gansky, S.A.; Henshaw, M.M.; Barker, J.C.; Brega, A.G.; Gregorich, S.E.; Heaton, B.; Batliner, T.S.; et al. The basic research factors questionaire for studying early childhood caries. BMC Oral Health 2017, 17, 83. Available online: https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-017-0374-5 (accessed on 1 November 2022). [CrossRef]
- de Silva-Sanigorski, A.; Ashbolt, R.; Green, J.; Calache, H.; Keith, B.; Riggs, E.; Waters, E. Parental self-efficacy and oral health-related knowledge are associated with parent and child oral health behaviors and self-reported oral health status. Community Dent. Oral Epidemiol. 2013, 41, 345–352. [Google Scholar] [CrossRef]
- Finlayson, T.L.; Siefert, K.; Ismail, A.; Sohn, W. Maternal self-efficacy and 1–5-year-old children’s brushing habits. Community Dent. Oral Epidemiol. 2007, 35, 272–281. [Google Scholar] [CrossRef]
- International Caries Detection and Assessment System Coordinating Committee. Criteria Manual: International Caries Detection and Assessment System (ICDAS II). 2013. Available online: https://www.icdas.org/uploads/ICDAS%20Criteria%20Document%20corrected%202013.pdf (accessed on 1 November 2013).
- Silness, J.; Löe, H. Periodontal disease in pregnancy, II. Correlation between oral hygiene and periodontal condition. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef]
- Finlayson, T.; Siefert, K.; Ismail, A.; Delva, J.; Sohn, W. Reliability and validity of brief measures of oral health-related knowledge, fatalism, and self-efficacy in mothers of African-American children. Pediatr. Dent. 2005, 27, 422–428. [Google Scholar]
- Raheb, J.; Arrow, P. An evaluation of workshop training in motivational interviewing for oral health counsellors. J. Contemp. Med. Educ. 2013, 1, 220–224. [Google Scholar] [CrossRef]
- Nowak, A.; Casamassimo, P. Using anticipatory guidance to provide early dental intervention. J. Am. Dent. Assoc. 1995, 126, 1156–1163. [Google Scholar] [CrossRef]
- Long, J.S.; Freese, J. Regression Models for Categorical Dependent Variables Using STATA, 3rd ed.; Stata Press: College Station, TX, USA, 2014. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 17; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Arrow, P. Oral health of school children in Western Australia. Aust. Dent. J. 2016, 61, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Henshaw, M.; Borrelli, B.; Gregorich, S.; Heaton, B.; Tooley, E.; Santo, W.; Cheng, N.; Rasmussen, M.; Helman, S.; Shain, S.; et al. Randomized Trial of Motivational Interviewing to Prevent Early Childhood Caries in Public Housing. JDR Clin. Trans. Res. 2018, 3, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Batliner, T.S.; Tiwari, T.; Henderson, W.G.; Wilson, A.R.; Gregorich, S.E.; Fehringer, K.A.; Brega, A.G.; Swyers, E.; Zacher, T.; Harper, M.M.; et al. Randomized Trial of Motivational Interviewing to Prevent Early Childhood Caries in American Indian Children. JDR Clin. Trans. Res. 2018, 3, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Cheng, N.F.; Guo, Z.; Gregorish, S.; Ismail, A.I.; Gansky, S.A. Mediation analysis for count and zero-inflated count data. Stat. Methods Med. Res. 2017, 27, 2756–2774. Available online: http://journals.sagepub.com.proxy.library.adelaide.edu.au/doi/full/10.1177/0962280216686131 (accessed on 1 November 2022). [CrossRef] [PubMed]
- Leske, A.M.; Mustchin, C.; Clarke-Errey, S.; Satur, J.; Bhujel, N.; Rajan, S. Motivational interviewing versus conventional caries prevention strategies in high-caries-risk children and families: A non-randomised trial. Br. Dent. J. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, L.; Smithers, L.; Hedges, J.; Parker, E.; Mills, H.; Kapellas, K.; Lawrence, H.P.; Broughton, J.R.; Ju, X. Dental Disease Outcomes Following a 2-Year Oral Health Promotion Program for Australian Aboriginal Children and Their Families: A 2-Arm Parallel, Single-blind, Randomised Controlled Trial. EClinicalMedicine 2018, 1, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Bailie, R.; Roberts-Thomson, K.; Leach, A.J.; Raye, I.; Endean, C.; Simmons, B.; Morris, P. Effect of health promotion and fluoride varnish on dental caries among Australian Aboriginal children: Results from a community-randomized controlled trial. Community Dent. Oral Epidemiol. 2011, 39, 29–43. [Google Scholar] [CrossRef]
- Azimi, S.; Taheri, J.B.; Tennant, M.; Kruger, E.; Molaei, H.; Ghorbani, Z. Relationship Between Mothers’ Knowledge and Attitude towards the Importance of Oral Health and Dental Status of their Young Children. Oral Health Prev. Dent. 2018, 16, 265–270. [Google Scholar]
- Lawrence, C.; Villar, E.D.; Armando, Ó. Fatalism and Health Behavior: A Meta-Analytic Review; Universidad Autónoma de Ciudad Juárez: Ciudad Juárez, Mexico, 2015. [Google Scholar]
- Leske, A.M.; Mustchin, C.; Bhujel, N.; Rajan, S.; Satur, J. Fidelity of motivational interviewing with families in high-caries-risk children. Community Dent. Oral Epidemiol. 2021, 49, 410–419. [Google Scholar] [CrossRef]
- Albino, J.; Tiwari, T. Behavior Change for Caries Prevention: Understanding Inconsistent Results. JDR Clin. Trans. Res. 2020, 5, 6–9. [Google Scholar] [CrossRef]
- Jamieson, L.M.; Garcia, R.I.; Sohn, W.; Albino, J. Challenges and Solutions for Improved Oral Health: Examples from Motivational Interviewing Trials. JDR Clin. Trans. Res. 2020, 5, 107–108. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristic | Test | Control | p Value |
|---|---|---|---|
| Sex; n (%) | |||
| Girls = 472 (51.4) Boys = 445 (48.6) | 234 (49.6) 221 (49.7) | 238 (50.4) 224 (50.3) | 0.98 |
| Location: n (%) | |||
| Fluoridated = 680 (76.3) Non-fluoridated = 211 (23.7) | 352 (77.4) 103 (22.6) | 328 (75.2) 108 (24.8) | 0.45 |
| Education level: n (%) | |||
| ≤year12 = 167 (18.7) Technical/Trade = 282 (31.7) Tertiary = 442 (49.6) | 78 (17.7) 135 (30.5) 229 (51.8) | 89 (19.8) 147 (32.7) 213 (47.4) | 0.42 |
| Family income: n (%) | |||
| <AUD$80 K = 392 (43.1) ≥AUD$80 K = 518 (56.9) | 190 (48.5) 261 (50.4) | 202 (51.5) 257 (49.6) | 0.57 |
| Child’s Age at baseline (months): n = 864 mean (SD); 3.2 (2.2) | n = 454 3.2 (2.1) | n = 410 3.4 (2.3) | 0.63 |
| Parent Baby Bottle Use Attitude: n = 916 mean (SD); 3.4 (3.4) | n = 454 3.4 (3.4) | n = 462 3.4 (3.3) | 0.70 |
| Parent Baby Oral Hygiene Needs Attitude: n = 916; mean (SD); 1.7 (2.2) | n = 453 1.9 (2.3) | n = 462 1.6 (2.1) | 0.07 |
| Fatalism: | |||
| Fatalistic = 205 (22.5) Non-fatalistic = 708 (77.6) | 104 (23.0) 348 (77.0) | 101 (21.9) 360 (78.1) | 0.60 |
| Parent self-efficacy: n = 913 mean (SD); 18.2 (5.4) | n = 453 18.1 (5.4) | n = 460 18.3 (5.4) | 0.58 |
| Parental Stress: n = 916 mean (SD); 15.8 (3.8) | n = 454 15.9 (3.7) | n = 462 15.7 (3.9) | 0.32 |
| Parental Support: n (%): n = 916 | |||
| Errands | |||
| Yes = 768 (83.8) No = 148 (16.2) | 387 (85.2) 67 (14.8) | 381 (82.5) 81 (17.5) | 0.25 |
| Lend money | |||
| Yes = 792 (86.5) No = 124 (13.5) | 394 (86.8) 60 (13.2) | 398 (86.2) 64 (13.9) | 0.78 |
| Babysit | |||
| Yes = 807 (88.1) No = 109 (11.9) | 398 (87.7) 56 (12.3) | 409 (88.5) 53 (11.5) | 0.69 |
| Lend car | |||
| Yes = 775 (84.6) No = 141 (15.4) | 387 (85.2) 67 (14.8) | 388 (84.0) 74 (16.0) | 0.46 |
| Factors | Test | p Value | Control | p Value |
|---|---|---|---|---|
| Parent Baby Bottle Use Attitude: Baseline Followup | n = 381 3.2 (3.5) 3.0 (3.2) | 0.20 | n = 351 3.3 (3.4) 3.7 (3.6) | 0.10 |
| Parent Baby Oral Hygiene Needs Attitude: Baseline Followup | n = 377 1.8 (2.2) 1.5 (1.9) | 0.005 | n = 350 1.5 (2.0) 1.6 (2.1) | 0.35 |
| Fatalism: Non-fatalistic—Fatalistic Fatalistic—Non-fatalistic | n = 375 33 42 McNemar’s Chi Sq | 0.30 | n = 350 35 38 McNemar’s Chi Sq | 0.73 |
| Parent self-efficacy: Baseline Followup | n = 377 18.4 (5.4) 17.6 (5.5) | 0.004 | n = 346 18.5 (5.5) 17.2 (5.5) | <0.001 |
| Parental Stress: Baseline Followup | n = 379 15.8 (3.8) 14.2 (3.4) | <0.001 | n = 350 15.6 (4.0) 14.0 (3.7) | <0.001 |
| Test | Control | Statistics | |
|---|---|---|---|
| First follow-up (prevalence, %, (n)) | 1.1, (4) | 0.9, (3) | p = 0.81 |
| Second follow-up (prevalence, %, (n)) | 4.7, (16) | 6.3, (17) | p = 0.39 |
| Third follow-up (prevalence, %, (n)) | 15.6, (47) | 14.0, (38) | p = 0.60 |
| First follow-up (caries experience), dmfs dmft | 0.21 (2.32) 0.06 (0.66) | 0.07 (1.15) 0.04 (0.57) | Mann-Whitney p = 0.81 p = 0.82 |
| Second follow-up (caries experience), dmfs dmft | 0.21 (1.86) 0.10 (0.71) | 0.26 (1.64) 0.13 (0.75) | Mann-Whitney p = 0.36 p = 0.59 |
| Third follow-up (caries experience), dmfs, dmft | 0.72 (2.61) 0.42 (1.26) | 1.05 (4.69) 0.48 (1.66) | Mann-Whitney p = 0.67 p = 0.55 |
| Second follow-up (plaque score) | 1.68 (2.06) | 1.72 (2.16) | Mann-Whitney p = 0.88 |
| Third follow-up (plaque score) | 3.23 (2.23) | 3.45 (2.30) | Mann-Whitney p = 0.29 |
| Independent Factor | IRR, (95% CI) | p Value |
|---|---|---|
| Group: | ||
| Control: referent Test | 1.5 (0.7–2.9) | 0.27 |
| Sex; n (%): | ||
| Boys: referent Girls | 0.8 (0.4–1.7) | 0.62 |
| Location: | ||
| Fluoridated: referent Non-fluoridated | 1.5 (0.8–2.9) | 0.23 |
| Education: | ||
| ≤year12: referent Technical/Trade Tertiary | 0.6 (0.2–1.9) 0.5 (0.2–1.4) | 0.41 0.19 |
| Family income: | ||
| <AUD$80 K: referent ≥AUD$80 K | 0.5 (0.3–1.0) | 0.07 |
| Baseline Fatalism: | ||
| Non-fatalistic: referent Fatalistic | 2.9 (1.4–6.1) | 0.01 |
| Baseline Parental Support | ||
| Errands: | ||
| No: referent Yes | 0.5 (0.2–1.2) | 0.11 |
| Lend money: | ||
| No: referent Yes | 0.6 (0.2–2.0) | 0.38 |
| Babysit: | ||
| No: referent Yes | 0.5 (0.1–2.2) | 0.39 |
| Lend car: | ||
| No: referent Yes | 0.6 (0.2–1.8) | 0.33 |
| Child’s Age at final follow-up | 1.4 (0.8–2.3) | 0.21 |
| Change in Parent Baby Bottle Attitude | 1.0 (0.9–1.0) | 0.29 |
| Change in Parent Baby Oral Hygiene Needs Attitude | 1.0 (0.8–1.2) | 0.87 |
| Change in Parent self-efficacy | 1.0 (0.9–1.1) | 0.68 |
| Change in Parental Stress | 1.1 (1.0–1.2) | 0.22 |
| Variable | IRR | 95% CI | p Value |
|---|---|---|---|
| Intervention: | |||
| Test: referent control | 1.5 | 0.7–3.2 | 0.26 |
| Region: | |||
| Fluoridated: referent Non-fluoridated | 4.2 | 1.8–10.2 | 0.001 |
| Income: | |||
| <AUD$80 K: referent ≥AUD$80 K | 0.8 | 0.4–1.7 | 0.64 |
| Fatalism: | |||
| non-fatalistic: referent fatalistic | 3.5 | 1.7–7.3 | 0.001 |
| Change in stress | 1.1 | 1.0–1.2 | 0.27 |
| Age at final follow-up | 2.2 | 1.4–3.6 | 0.001 |
| Change in baby bottle use attitude | 1.0 | 0.9–1.1 | 0.53 |
| Education: | |||
| non-tertiary: referent tertiary | 0.5 | 0.2–1.0 | 0.04 |
| Family Support | |||
| Do Errands: | |||
| No: referent yes | 0.5 | 0.1–1.7 | 0.27 |
| Lend money: | |||
| No: referent yes | 1.7 | 0.6–5.1 | 0.31 |
| Babysitting: | |||
| No: referent yes | 1.5 | 0.3–7.2 | 0.59 |
| Transport: | |||
| No: referent yes | 0.9 | 0.3–3.2 | 0.85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arrow, P.; Raheb, J.; McInnes, R. Motivational Interviewing and Childhood Caries: A Randomised Controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 4239. https://doi.org/10.3390/ijerph20054239
Arrow P, Raheb J, McInnes R. Motivational Interviewing and Childhood Caries: A Randomised Controlled Trial. International Journal of Environmental Research and Public Health. 2023; 20(5):4239. https://doi.org/10.3390/ijerph20054239
Chicago/Turabian StyleArrow, Peter, Joseph Raheb, and Rowena McInnes. 2023. "Motivational Interviewing and Childhood Caries: A Randomised Controlled Trial" International Journal of Environmental Research and Public Health 20, no. 5: 4239. https://doi.org/10.3390/ijerph20054239
APA StyleArrow, P., Raheb, J., & McInnes, R. (2023). Motivational Interviewing and Childhood Caries: A Randomised Controlled Trial. International Journal of Environmental Research and Public Health, 20(5), 4239. https://doi.org/10.3390/ijerph20054239





