Mental Health Disorders and Coping Strategies in Healthcare Workers during the COVID-19 Pandemic: An Analytical Cross-Sectional Study in Southeastern Mexico
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Study Setting
2.3. Participants and Procedure
2.4. Measures, Variables, and Data Collection
2.5. Statistical Analysis
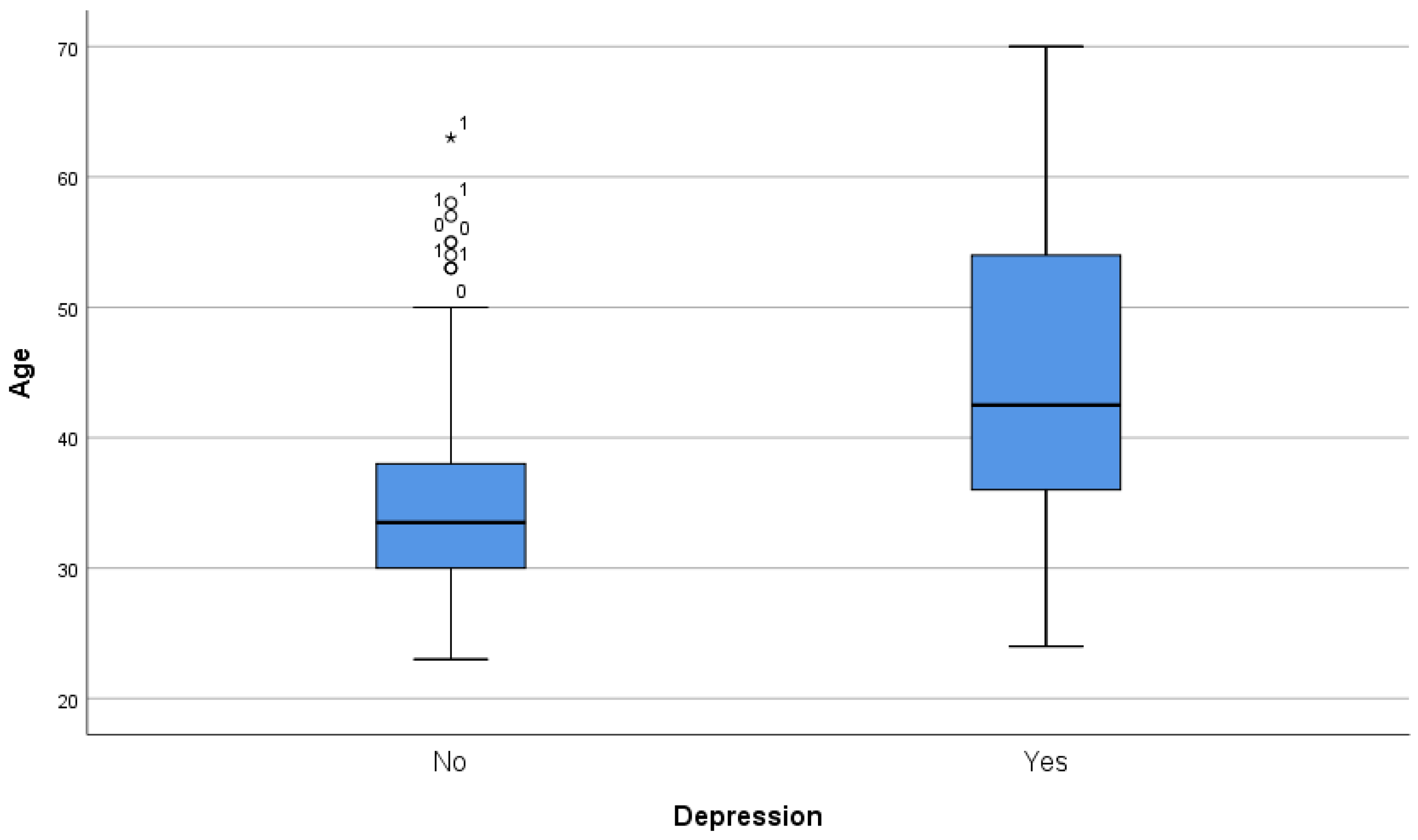
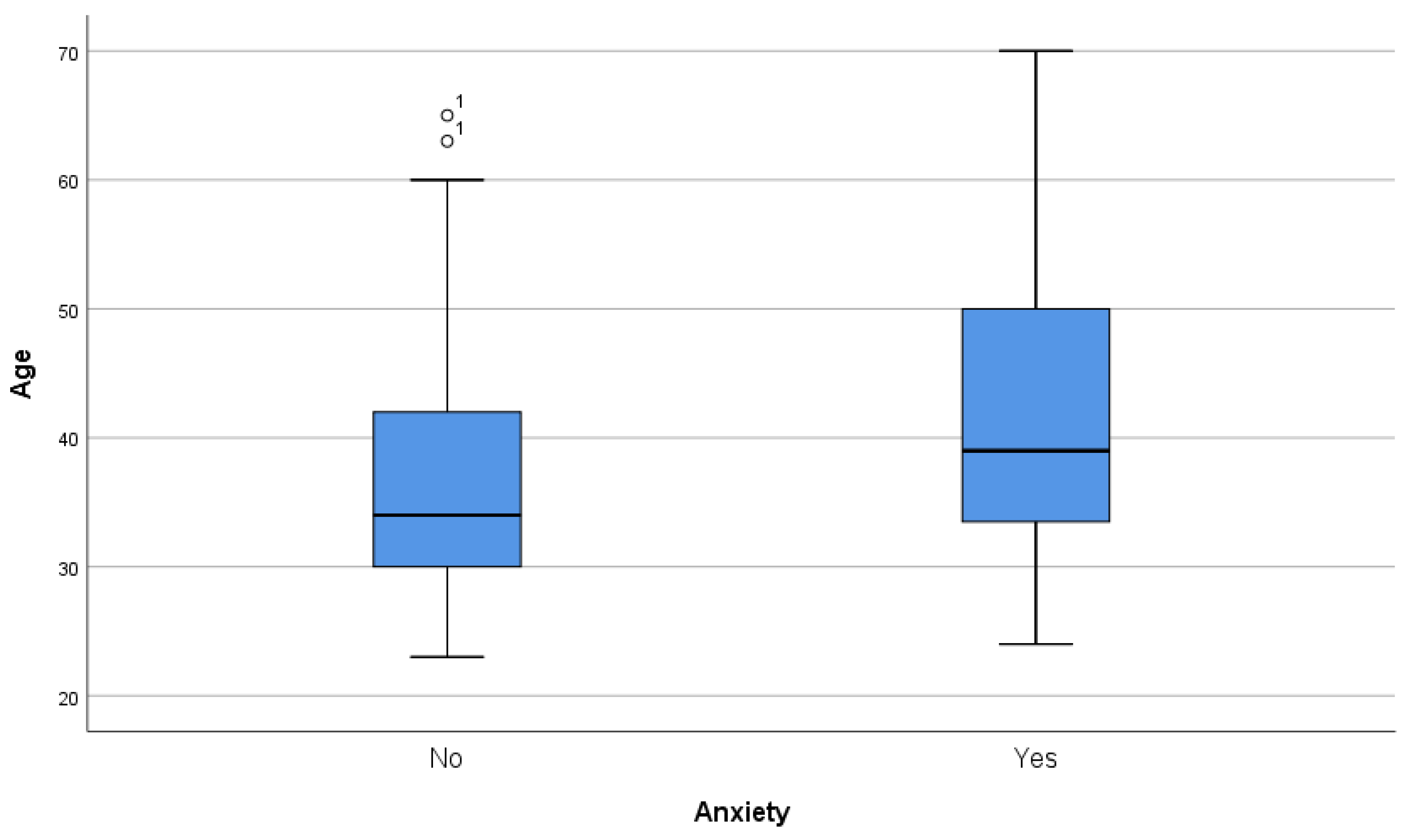
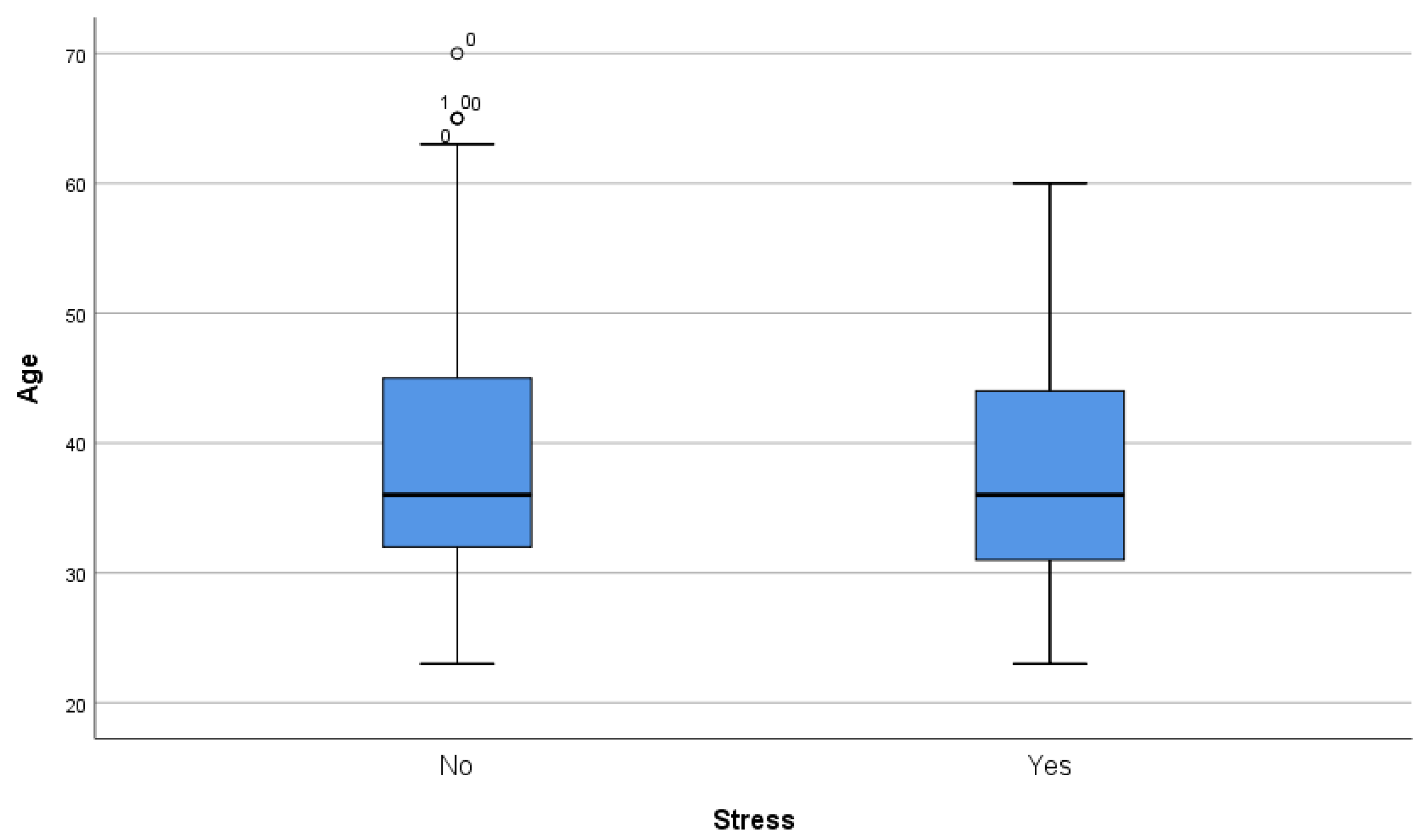
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kwong, A.S.F.; Pearson, R.M.; Adams, M.J.; Northstone, K.; Tilling, K.; Smith, D.; Fawns-Ritchie, C.; Bould, H.; Warne, N.; Zammit, S.; et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br. J. Psychiatry 2020, 218, 334–343. Available online: https://pubmed.ncbi.nlm.nih.gov/33228822/ (accessed on 11 February 2023). [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. Available online: https://pubmed.ncbi.nlm.nih.gov/32799105/ (accessed on 11 February 2023). [CrossRef] [PubMed]
- Santomauro, D.F.; Herrera, A.M.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Taquet, M.; Holmes, E.A.; Harrison, P.J. Depression and anxiety disorders during the COVID-19 pandemic: Knowns and unknowns. Lancet 2021, 398, 1665–1666. Available online: https://pubmed.ncbi.nlm.nih.gov/34634251/ (accessed on 11 February 2023). [CrossRef]
- Chaturvedi, K.; Vishwakarma, D.K.; Singh, N. COVID-19 and its impact on education, social life and mental health of students: A survey. Child. Youth Serv. Rev. 2021, 121, 105866. [Google Scholar] [CrossRef]
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; Murphy, J.; McBride, O.; Fox, R.; Bondjers, K.; Karatzias, T.; Bentall, R.P.; Martinez, A.; Vallières, F. A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID-19 pandemic. Psychiatry Res. 2021, 300, 113905. Available online: https://pubmed.ncbi.nlm.nih.gov/33827013/ (accessed on 14 February 2023). [CrossRef]
- Gori, A.; Topino, E. Across the COVID-19 Waves; Assessing Temporal Fluctuations in Perceived Stress, Post-Traumatic Symptoms, Worry, Anxiety and Civic Moral Disengagement over One Year of Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5651. Available online: https://www.mdpi.com/1660-4601/18/11/5651/htm (accessed on 14 February 2023). [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Hossain, M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Research 2020, 9, 636. Available online: https://pubmed.ncbi.nlm.nih.gov/33093946/ (accessed on 25 January 2023). [CrossRef]
- Bonati, M.; Campi, R.; Segre, G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: A systematic review of the evidence. Epidemiol. Psychiatr. Sci. 2022, 31, e27. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, S.; Dayama, S.; Galhotra, A. COVID-19 mental health challenges: A scoping review. J. Educ. Health Promot. 2022, 11, 375. Available online: https://pubmed.ncbi.nlm.nih.gov/36618463/ (accessed on 25 January 2023). [PubMed]
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. Available online: https://pubmed.ncbi.nlm.nih.gov/34958144/ (accessed on 25 January 2023). [CrossRef] [PubMed]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020, 51, 102119. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef] [PubMed]
- Biber, J.; Ranes, B.; Lawrence, S.; Malpani, V.; Trinh, T.T.; Cyders, A.; English, S.; Staub, C.L.; McCausland, K.L.; Kosinski, M.; et al. Mental health impact on healthcare workers due to the COVID-19 pandemic: A U.S. cross-sectional survey study. J. Patient Rep. Outcomes 2022, 6, 63. Available online: https://jpro.springeropen.com/articles/10.1186/s41687-022-00467-6 (accessed on 25 January 2023). [CrossRef] [PubMed]
- Du, J.; Mayer, G.; Hummel, S.; Oetjen, N.; Gronewold, N.; Zafar, A.; Schultz, J.-H. Mental health burden in different professions during the final stage of the COVID-19 lockdown in China: Cross-sectional survey study. J. Med. Internet Res. 2020, 22, e24240. [Google Scholar] [CrossRef]
- Shoib, S.; Buitrago, J.E.T.G.; Shuja, K.H.; Aqeel, M.; de Filippis, R.; Abbas, J.; Ullah, I.; Arafat, S.M.Y. Suicidal behavior sociocultural factors in developing countries during COVID-19. Encephale 2022, 48, 78–82. Available online: https://pubmed.ncbi.nlm.nih.gov/34654566/ (accessed on 25 January 2023). [CrossRef] [PubMed]
- Maniruzzaman; Islam, M.; Ali, H.; Mukerjee, N.; Maitra, S.; Kamal, M.A.; Ghosh, A.; Castrosanto, M.A.; Alexiou, A.; Ashraf, G.M.; et al. COVID-19 diagnostic methods in developing countries. Environ. Sci. Pollut. Res. Int. 2022, 29, 51384–51397. Available online: https://pubmed.ncbi.nlm.nih.gov/35619009/ (accessed on 25 January 2023).
- Smith, M.M.; Saklofske, D.H.; Keefer, K.V.; Tremblay, P.F. Coping Strategies and Psychological Outcomes: The Moderating Effects of Personal Resiliency. J. Psychol. 2016, 150, 318–332. Available online: https://pubmed.ncbi.nlm.nih.gov/25951375/ (accessed on 26 January 2023). [CrossRef]
- Mayordomo, T.; Viguer, P.; Sales, A.; Satorres, E.; Meléndez, J.C. Resilience and Coping as Predictors of Well-Being in Adults. J. Psychol. Interdiscip. Appl. 2016, 150, 809–821. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Tapia, J.; Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Ruiz, M.; Nieto, C.; Rey, R.R. Coping, personality and resilience: Prediction of subjective resilience from coping strategies and protective personality factors 1. Behav. Psychol./Psicol. Conduct. 2019, 27, 375–389. [Google Scholar]
- Stanisławski, K. The Coping Circumplex Model: An Integrative Model of the Structure of Coping With Stress. Front. Psychol. 2019, 10, 694. [Google Scholar] [CrossRef] [PubMed]
- Goh, Y.W.; Sawang, S.; Oei, T.P.S. The Revised Transactional Model (RTM) of Occupational Stress and Coping: An Improved Process Approach. Aust. N. Z. J. Organ. Psychol. 2010, 3, 13–20. Available online: https://www.researchgate.net/publication/50933792_The_Revised_Transactional_Model_RTM_of_Occupational_Stress_and_Coping_An_Improved_Process_Approach (accessed on 15 February 2023). [CrossRef]
- Obbarius, N.; Fischer, F.; Liegl, G.; Obbarius, A.; Rose, M. A Modified Version of the Transactional Stress Concept According to Lazarus and Folkman Was Confirmed in a Psychosomatic Inpatient Sample. Front. Psychol. 2021, 12, 405. [Google Scholar] [CrossRef]
- Compas, B.E.; Vreeland, A.; Henry, L. Coping Models of Stress and Resilience. In The Oxford Handbook of Stress and Mental Health; Oxford University Press: Oxford, UK, 2018; pp. 584–600. Available online: https://academic.oup.com/edited-volume/28307/chapter/215018965 (accessed on 15 February 2023).
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Chua, H.C.; Sim, K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Singap. Med. J. 2020, 61, 350–356. Available online: https://pubmed.ncbi.nlm.nih.gov/32241071/ (accessed on 26 January 2023). [CrossRef]
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Sim, K. Psychological and Coping Responses of Health Care Workers Toward Emerging Infectious Disease Outbreaks: A Rapid Review and Practical Implications for the COVID-19 Pandemic. J. Clin. Psychiatry 2020, 81, 20r13450. [Google Scholar] [CrossRef]
- Ponizovsky, A.M.; Finkelstein, I.; Poliakova, I.; Mostovoy, D.; Goldberger, N.; Rosca, P. Interpersonal distances, coping strategies and psychopathology in patients with depression and schizophrenia. World J. Psychiatry 2013, 3, 74. Available online: https://pmc/articles/PMC3832865/ (accessed on 26 January 2023). [CrossRef]
- Zainel, A.A.; Qotba, H.; Al-Maadeed, A.; Al-Kohji, S.; Al Mujalli, H.; Ali, A.; Al Mannai, L.; Aladab, A.; AlSaadi, H.; AlKarbi, K.A.; et al. Psychological and Coping Strategies Related to Home Isolation and Social Distancing in Children and Adolescents During the COVID-19 Pandemic: Cross-sectional Study. JMIR Form Res. 2021, 5, e24760. Available online: https://pubmed.ncbi.nlm.nih.gov/33851577/ (accessed on 26 January 2023). [CrossRef]
- El-Hage, W.; Hingray, C.; Lemogne, C.; Yrondi, A.; Brunault, P.; Bienvenu, T.; Etain, B.; Paquet, C.; Gohier, B.; Bennabi, D.; et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks? Encephale 2020, 46, S73–S80. [Google Scholar] [CrossRef]
- Gurrola Peña, G.; Balcázar Nava, P.; Bonilla Muños, M.; Virseda Heras, J. Estructura factorial y consistencia interna de la escala de depresión ansiedad y estrés (dass-21) en una muestra no clínica. Psicol. Cienc. Soc. 2006, 8, 3–7. Available online: http://redalyc.uaemex.mx (accessed on 26 January 2023).
- Omar, A.G. Stress y Coping: Las Estrategias de Coping y Sus Interrelaciones Con los Niveles Biológico y Psicológico, 1st ed.; Lumen: Buenos Aires, Argentina, 1995; Volume 1. [Google Scholar]
- Folkman, S. Stress: Appraisal and Coping. In Encyclopedia of Behavioral Medicine; Springer Science + Business Media: New York, NY, USA, 2013; pp. 1913–1915. Available online: https://link.springer.com/referenceworkentry/10.1007/978-1-4419-1005-9_215 (accessed on 15 February 2023).
- Paris, L. Estrés Laboral en Trabajadores de la Salud, 1st ed.; UAI Editorial: Rosario, Argentina, 2007; Volume 1, pp. 1–317. Available online: https://uai.edu.ar/media/109543/paris-estres-laboral.pdf (accessed on 26 January 2023).
- Javed, B.; Sarwer, A.; Soto, E.B.; Mashwani, Z.U.R. Impact of SARS-CoV-2 (Coronavirus) Pandemic on Public Mental Health. Front. Public Health 2020, 8, 292. Available online: http://www.ncbi.nlm.nih.gov/pubmed/32656175 (accessed on 27 January 2023). [CrossRef] [PubMed]
- Weich, S. Mental health after covid-19. BMJ 2022, 376, o326. Available online: https://pubmed.ncbi.nlm.nih.gov/35172977/ (accessed on 27 January 2023). [CrossRef] [PubMed]
- Lindert, J.; Jakubauskiene, M.; Bilsen, J. The COVID-19 disaster and mental health-assessing, responding and recovering. Eur. J. Public Health 2021, 31, IV31–IV35. Available online: https://pubmed.ncbi.nlm.nih.gov/34751367/ (accessed on 27 January 2023). [CrossRef]
- Cui, J.; Lu, J.; Weng, Y.; Yi, G.Y.; He, W. COVID-19 impact on mental health. BMC Med. Res. Methodol. 2022, 22, 15. Available online: https://pubmed.ncbi.nlm.nih.gov/35026998/ (accessed on 27 January 2023). [CrossRef]
- Hernández-Díaz, Y.; Genis-Mendoza, A.D.; Fresán, A.; González-Castro, T.B.; Tovilla-Zárate, C.A.; Juárez-Rojop, I.E.; López-Narváez, M.L.; Martínez-Magaña, J.J.; Nicolini, H. Knowledge, emotions and stressors in front-line healthcare workers during the covid-19 outbreak in Mexico. Int. J. Environ. Res. Public Health 2021, 18, 5622. [Google Scholar] [CrossRef]
- Ghaleb, Y.; Lami, F.; Al Nsour, M.; Rashak, H.A.; Samy, S.; Khader, Y.S.; Al Serouri, A.; BahaaEldin, H.; Afifi, S.; Elfadul, M.; et al. Mental health impacts of COVID-19 on healthcare workers in the Eastern Mediterranean Region: A multi-country study. J. Public Health 2021, 43, iii34–iii42. Available online: https://pubmed.ncbi.nlm.nih.gov/34642765/ (accessed on 27 January 2023). [CrossRef]
- Aymerich, C.; Pedruzo, B.; Pérez, J.L.; Laborda, M.; Herrero, J.; Blanco, J.; Mancebo, G.; Andrés, L.; Estévez, O.; Fernandez, M.; et al. COVID-19 pandemic effects on health worker’s mental health: Systematic review and meta-analysis. Eur. Psychiatry 2022, 65, e10. Available online: https://pubmed.ncbi.nlm.nih.gov/35060458/ (accessed on 27 January 2023). [CrossRef]
- Ghahramani, S.; Kasraei, H.; Hayati, R.; Tabrizi, R.; Marzaleh, M.A. Health care workers’ mental health in the face of COVID-19: A systematic review and meta-analysis. Int. J. Psychiatry Clin. Pract. 2022, 1–10. [Google Scholar] [CrossRef]
- Saragih, I.D.; Tonapa, S.I.; Saragih, I.S.; Advani, S.; Batubara, S.O.; Suarilah, I.; Lin, C.-J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 121, 104002. [Google Scholar] [CrossRef]
- Robles, R.; Rodríguez, E.; Vega-Ramírez, H.; Álvarez-Icaza, D.; Madrigal, E.; Durand, S.; Morales-Chainé, S.; Astudillo, C.; Real-Ramírez, J.; Medina-Mora, M.-E.; et al. Mental health problems among healthcare workers involved with the COVID-19 outbreak. Braz. J. Psychiatry 2021, 43, 494–503. Available online: https://pubmed.ncbi.nlm.nih.gov/33331498/ (accessed on 27 January 2023). [CrossRef] [PubMed]
- Salgado de Snyder, V.N.; Villatoro, A.P.; McDaniel, M.D.; Ocegueda, A.S.; Garcia, D.; Parra-Medina, D. Occupational Stress and Mental Health Among Healthcare Workers Serving Socially Vulnerable Populations During the COVID-19 Pandemic. Front. Public Health 2021, 9, 782846. Available online: https://pubmed.ncbi.nlm.nih.gov/34957034/ (accessed on 27 January 2023). [CrossRef] [PubMed]
- Abeldaño Zuñiga, R.A.; Juanillo-Maluenda, H.; Sánchez-Bandala, M.A.; Burgos, G.V.; Müller, S.A.; Rodríguez López, J.R. Mental Health Burden of the COVID-19 Pandemic in Healthcare Workers in Four Latin American Countries. Inquiry 2021, 58, 469580211061059. Available online: https://pubmed.ncbi.nlm.nih.gov/34865558/ (accessed on 27 January 2023). [CrossRef] [PubMed]
- Mascayano, F.; van der Ven, E.; Moro, M.F.; Schilling, S.; Alarcón, S.; Al Barathie, J.; Alnasser, L.; Asaoka, H.; Ayinde, O.; Balalian, A.A.; et al. The impact of the COVID-19 pandemic on the mental health of healthcare workers: Study protocol for the COVID-19 HEalth caRe wOrkErS (HEROES) study. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 633–645. Available online: https://pubmed.ncbi.nlm.nih.gov/35064280/ (accessed on 27 January 2023). [CrossRef]
- Parker, G.; Brotchie, H. Gender differences in depression. Int. Rev. Psychiatry 2010, 22, 429–436. Available online: https://pubmed.ncbi.nlm.nih.gov/21047157/ (accessed on 27 January 2023). [CrossRef]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. Available online: https://pubmed.ncbi.nlm.nih.gov/27856392/ (accessed on 27 January 2023). [CrossRef]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol. Bull. 2017, 143, 783–822. Available online: https://pmc/articles/PMC5532074/ (accessed on 15 February 2023). [CrossRef]
- Francis, B.; Ken, C.S.; Han, N.Y.; Ariffin, M.A.A.; Yusuf, M.H.; Wen, L.J.; Petrus, C.F.; Chin, B.H.; Gill, J.S.; Sulaiman, A.H.; et al. Religious Coping During the COVID-19 Pandemic: Gender, Occupational and Socio-economic Perspectives Among Malaysian Frontline Healthcare Workers. Alpha Psychiatry 2021, 22, 194. Available online: https://pubmed.ncbi.nlm.nih.gov/28447828/ (accessed on 15 February 2023). [CrossRef]
- Skapinakis, P.; Bellos, S.; Oikonomou, A.; Dimitriadis, G.; Gkikas, P.; Perdikari, E.; Mavreas, V. Depression and Its Relationship with Coping Strategies and Illness Perceptions during the COVID-19 Lockdown in Greece: A Cross-Sectional Survey of the Population. Depress. Res. Treat. 2020, 2020, 3158954. Available online: https://pubmed.ncbi.nlm.nih.gov/32908697/ (accessed on 27 January 2023). [CrossRef]
- Onieva-Zafra, M.D.; Fernández-Muñoz, J.J.; Fernández-Martínez, E.; García-Sánchez, F.J.; Abreu-Sánchez, A.; Parra-Fernández, M.L. Anxiety, perceived stress and coping strategies in nursing students: A cross-sectional, correlational, descriptive study. BMC Med. Educ. 2020, 20, 370. [Google Scholar] [CrossRef]
- Ghafouri, R.; Qadimi, A.; Khomaam, H.K. Coping strategy with coronavirus disease-2019 health anxiety in nursing students. J. Educ. Health Promot. 2022, 11, 381. Available online: https://pubmed.ncbi.nlm.nih.gov/36618466/ (accessed on 27 January 2023). [CrossRef]
- Thompson, R.J.; Mata, J.; Jaeggi, S.M.; Buschkuehl, M.; Jonides, J.; Gotlib, I.H. Maladaptive coping, adaptive coping, and depressive symptoms: Variations across age and depressive state. Behav. Res. Ther. 2010, 48, 459–466. [Google Scholar] [CrossRef]
- Glynn, J.R. Protecting workers aged 60–69 years from COVID-19. Lancet Infect. Dis. 2020, 20, 1123. Available online: http://www.thelancet.com/article/S147330992030311X/fulltext (accessed on 15 February 2023). [CrossRef]
- Pit, S.; Fisk, M.; Freihaut, W.; Akintunde, F.; Aloko, B.; Berge, B.; Burmeister, A.; Ciacâru, A.; Deller, J.; Dulmage, R.; et al. COVID-19 and the ageing workforce: Global perspectives on needs and solutions across 15 countries. Int. J. Equity Health 2021, 20, 221. Available online: https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-021-01552-w (accessed on 15 February 2023). [CrossRef] [PubMed]
- Denova-Gutiérrez, E.; Flores, Y.N.; Gallegos-Carrillo, K.; Ramírez-Palacios, P.; Rivera-Paredez, B.; Muñoz-Aguirre, P.; Velázquez-Cruz, R.; Torres-Ibarra, L.; Meneses-León, J.; Méndez-Hernández, P.; et al. Health workers cohort study: Methods and study design. Salud Pública Méx. 2016, 58, 708–716. Available online: https://www.saludpublica.mx/index.php/spm/article/view/8299/10976 (accessed on 15 February 2023). [CrossRef] [PubMed]
- Montañez-Hernández, J.C.; Alcalde-Rabanal, J.E.; Nigenda-López, G.H.; Aristizábal-Hoyos, G.P.; Dini, L. Gender inequality in the health workforce in the midst of achieving universal health coverage in Mexico. Hum. Resour. Health 2020, 18, 40. Available online: https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-020-00481-z (accessed on 15 February 2023). [CrossRef] [PubMed]
- Márquez-González, H.; Klünder-Klünder, M.; de La Rosa-Zamboni, D.; Ortega-Riosvelasco, F.; López-Martínez, B.; Jean-Tron, G.; Chapa-Koloffon, G.; Ávila-Hernández, V.; Garduño-Espinosa, J.; Villa-Guillén, M.; et al. Risk conditions in healthcare workers of a pediatric COVID center in Mexico City. Bol. Méd. Hosp. Infant. Méx. 2021, 78, 110–115. Available online: https://www.bmhim.com (accessed on 15 February 2023). [PubMed]
| Variable | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
| Chi-Square Test | OR (95% CI) | Chi-Square Test | OR (95% CI) | Chi-Square Test | OR (95% CI) | |
| Gender | 0.047 * | 0.6 (.36 to 0.99) | 0.2 | 0.72 (0.44 to 1.18) | 0.04 * | 1.78 (1.02 to 3.02) |
| Comorbidities | <0.001 ** | 10.9 (6.1 to 19.65) | <0.001 ** | 4.18 (2.47 to 7) | 0.4 | 1.24 (0.72 to 2.12) |
| Psychiatric background | 0.01 * | 2.17 (1.19 to 3.96) | 0.004 ** | 2.43 (1.06 to 1.39) | <0.001 ** | 3.58 (1.6 to 8) |
| COVID-19 infection | 0.45 | 1.24 (0.7 to 2.18) | 0.49 | 1.78 (1.01 to 3.13) | 0.009 ** | 1.25 (1.03 to 1.52) |
| Death of relatives | 0.16 | 0.68 (0.4 to 1.1) | 0.1 | 1.54 (0.91 to 2.58) | 0.059 | 1.69 (0.97 to 2.95) |
| Occupation | Depression | Anxiety | Stress | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n,%) | No (n, %) | Chi-Square Test | Yes (n,%) | No (n, %) | Chi-Square Test | Yes (n,%) | No (n, %) | Chi-Square Test | |
| Administrative | 7, 46.6 | 8, 53.33 | p = 0.003 ** | 10, 66.66 | 5, 33,33 | p = 0.01 * | 4, 26.66% | 11, 73.33 | 0.13 |
| Medical doctor | 39, 54.16 | 33, 45.83 | 38, 52.77 | 34, 47.22 | 15, 20.83 | 57, 51.38 | |||
| Nurse | 42, 41.17 | 60, 58.82 | 47, 46.07 | 55, 53.92 | 35, 34.31 | 67, 65.68 | |||
| Technician | 4, 12.9 | 27, 87.09 | 7, 22.58 | 24, 77.41 | 7, 22.58 | 24, 77.41 | |||
| Others | 18, 50 | 18, 50 | 21, 58.33 | 15, 41.66 | 15, 41.66 | 21, 58.33 | |||
| Occupation | Maladaptive Coping | Resolution Coping | Resignation Coping | Distancing Coping | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n,%) | No (n, %) | Chi-Square Test | Yes (n,%) | No (n, %) | Chi-Square Test | Yes (n,%) | No (n, %) | Chi-Square Test | Yes (n,%) | No (n, %) | Chi-Square Test | |
| Administrative | 7, 46.6 | 8, 53.33 | p = 0.01 * | 6, 40 | 9, 60 | p = 0.35 | 7, 46.6 | 8, 53.33 | p = 0.03 * | 3, 20 | 12, 80 | p < 0.001 ** |
| Medical doctor | 26, 36.1 | 46, 63.88 | 34, 47.22 | 38, 52.77 | 41, 56.94 | 31, 43.05 | 29, 40.27 | 43, 59.72 | ||||
| Nurse | 41, 40.19 | 61, 59.8 | 38, 37.25 | 64, 62.74 | 55, 53.92 | 47, 46.07 | 51, 50 | 51, 50 | ||||
| Technician | 3, 9.67 | 28, 90.32 | 17, 54.83 | 14, 45.16 | 12, 38.7 | 19, 61.29 | 24, 77.41 | 7, 22.58 | ||||
| Others | 12, 33.33 | 24, 66.66 | 13, 36.11 | 23, 63.88 | 10, 27.77 | 26, 72.22 | 26, 72.22 | 10, 27.77 | ||||
| Coping Strategies | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
| Chi-Square Test | OR (95% CI) | Chi-Square Test | OR (95% CI) | Chi-Square Test | OR (95% CI) | |
| Maladaptive | p < 0.001 ** | 2.94 (1.73 to 5) | p < 0.001 ** | 4.46 (2.56 to 7.78) | p < 0.001 ** | 3.68 (2.1 to 6.47) |
| Resolution | p < 0.001 ** | 0.35 (0.2 to 0.59) | p < 0.001 ** | 0.22 (0.13 to 0.38) | p = 0.02 * | 0.52 (0.3 to 0.92) |
| Resignation | p = 0.06 | 1.59 (0.96 to 2.62) | p = 0.13 | 1.45 (0.88 to 2.37) | p = 0.052 | 0.58 (0.33 to 1) |
| Distancing | p = 0.29 | 0.76 (0.46 to 1.26) | p = 0.78 | 1.07 (0.65 to 1.75) | p = 0.33 | 1.3 (0.76 to 2.23) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granados Villalpando, J.M.; Baeza Flores, G.d.C.; Ble Castillo, J.L.; Celorio Méndez, K.d.S.; Juárez Rojop, I.E.; Morales Contreras, J.A.; Olvera Hernández, V.; Quiroz Gómez, S.; Romero Tapia, S.d.J.; Ruíz Quiñones, J.A.; et al. Mental Health Disorders and Coping Strategies in Healthcare Workers during the COVID-19 Pandemic: An Analytical Cross-Sectional Study in Southeastern Mexico. Int. J. Environ. Res. Public Health 2023, 20, 4230. https://doi.org/10.3390/ijerph20054230
Granados Villalpando JM, Baeza Flores GdC, Ble Castillo JL, Celorio Méndez KdS, Juárez Rojop IE, Morales Contreras JA, Olvera Hernández V, Quiroz Gómez S, Romero Tapia SdJ, Ruíz Quiñones JA, et al. Mental Health Disorders and Coping Strategies in Healthcare Workers during the COVID-19 Pandemic: An Analytical Cross-Sectional Study in Southeastern Mexico. International Journal of Environmental Research and Public Health. 2023; 20(5):4230. https://doi.org/10.3390/ijerph20054230
Chicago/Turabian StyleGranados Villalpando, Jesús Maximiliano, Guadalupe del Carmen Baeza Flores, Jorge Luis Ble Castillo, Karla del Socorro Celorio Méndez, Isela Esther Juárez Rojop, José Antonio Morales Contreras, Viridiana Olvera Hernández, Sergio Quiroz Gómez, Sergio de Jesús Romero Tapia, Jesús Arturo Ruíz Quiñones, and et al. 2023. "Mental Health Disorders and Coping Strategies in Healthcare Workers during the COVID-19 Pandemic: An Analytical Cross-Sectional Study in Southeastern Mexico" International Journal of Environmental Research and Public Health 20, no. 5: 4230. https://doi.org/10.3390/ijerph20054230
APA StyleGranados Villalpando, J. M., Baeza Flores, G. d. C., Ble Castillo, J. L., Celorio Méndez, K. d. S., Juárez Rojop, I. E., Morales Contreras, J. A., Olvera Hernández, V., Quiroz Gómez, S., Romero Tapia, S. d. J., Ruíz Quiñones, J. A., & Guzmán Priego, C. G. (2023). Mental Health Disorders and Coping Strategies in Healthcare Workers during the COVID-19 Pandemic: An Analytical Cross-Sectional Study in Southeastern Mexico. International Journal of Environmental Research and Public Health, 20(5), 4230. https://doi.org/10.3390/ijerph20054230










