Abstract
Nigerian women continue to die in childbirth due to inadequate health services such as antenatal care (ANC). Among other factors, the inadequate receipt or non-use of ANC appears to be associated with the age of women, remoteness, and poor households. This cross-sectional study aimed to compare the factors associated with inadequate receipt of the components and non-use of ANC among pregnant adolescents, and young and older women in Nigeria. Data for this study were from the 2018 Nigeria Demographic and Health Survey (NDHS) and covered a weighted total of 21,911 eligible women. Survey multinomial logistic regression analyses that adjusted for cluster, and survey weights were conducted to examine factors associated with adolescent, young, and older women. Adolescent women reported a higher prevalence of inadequate receipts and non-use of ANC than young and older women. Increased odds of inadequate receipt of the components of ANC were associated with residence in the North–East region and rural areas for all three categories of women. For adolescent women, the increased odds of inadequate receipt of the components of ANC were associated with delivering a baby at home and a big problem with distance to health facilities. Limited education or no schooling was associated with the increased odds of receiving inadequate ANC among older women. Implementing interventions to improve maternal and child health care should focus on the factors associated with the increased odds of receipt of inadequate or non-use of ANC services among Nigerian adolescent women, particularly those living in rural areas in the North–East region.
1. Introduction
Adequate antenatal care (ANC) services remain one of the four pillars of the safe motherhood initiative, aimed at providing care that will improve the survival of women and babies [1,2,3]. The World Health Organization (WHO) recently recommended at least eight ANC visits for all pregnant women, irrespective of age and risk status, to ensure a more positive pregnancy outcome [2].
Antenatal care is a strategy geared towards curtailing the high maternal and newborn mortality, which Nigeria records at an unacceptably high rate of 39 deaths per 1000 live births in the 2018 Nigeria Demographic and Health Survey (NDHS), contributing to the global burden of maternal and newborn death [4]. There is evidence of a direct link between maternal health and perinatal and neonatal outcomes. Integrating maternal and newborn care into routine health services in low- and middle-income countries, including Nigeria, may improve overall health outcomes in women and children [5]. Providing accessible quality ANC has been identified as a major intervention to minimize maternal, perinatal, and neonatal mortality [6,7]. A significant component of regular ANC is the maternal and fetal assessment in identifying high-risk pregnancies, which require referral to the next level of maternal care [2,7]. Worldwide, almost 86% of pregnant women receive at least one ANC care from a skilled health professional. Nonetheless, only 65% received the recommended eight ANC visits [8]. Nigeria has consistently had a low ANC coverage rate. Recent data showed a slight increase of about 3% from the previous 58% in 2008 NDHS to 61% in 2013 NDHS, but this is far below the recommended 90% coverage rate required for a meaningful reduction in newborn and maternal death through early detection and treatment of some causes of death [9].
The documented national average ANC coverage rate in Nigeria is not the exact reflection of the country’s status considering the variations across regions, states, and urban and rural locations [10]. Additionally, there are variations in the coverage of ANC between adolescent pregnant women and older women. Pregnancy and childbearing are critical for adolescent women and, therefore, of great public health concern. Adolescents are at greater odds of adverse pregnancy and delivery complications than older women [10], and they are about twice as likely to die from maternal-related causes than non-adolescents [11,12].
Every year, about 16 million girls aged 15–19 give birth, 95% are in low and middle-income countries, particularly sub-Saharan Africa, with 2 million girls giving birth before the age of 15 in these countries [11]. Adolescent pregnancy is still high in Nigeria. According to the most recent Nigerian Demographic Health Survey (NDHS), the birth rate among adolescents is 106 births per 1000 women and even higher in some regions, like the northern regions, requiring intense ANC among adolescents [4].
Adolescents are less likely to receive four or more ANC visits and have a skilled healthcare provider at ANC clinics than women in the older age groups [13]. This is because they face multiple barriers that reduce their access to maternal healthcare information and services [13,14], Adolescent women are less likely to utilize maternal healthcare services such as ANC, which is a complex phenomenon influenced by many factors. These factors are the lack of adolescent-centered services and socioeconomic challenges found to be more prevalent in adolescents, thereby lowering their access to maternal health services [15,16].
To meet the sustainable development goals (SDGs 3) target of improving maternal health and the reduction of maternal mortality to a reasonable level by 2030, it is important to understand the actual access to ANC services by women, including adolescents, who have been found to be one of the vulnerable groups, in terms of motherhood. Furthermore, utilization of ANC has been found to be associated with the age of women; the risk of its inadequacy is higher among older women (aged 31 years or older) [17,18], although a past study from Vietnam observed that age did not affect the utilization of ANC [19].
A number of studies examined the utilization of ANC services and factors associated with them in Nigeria [20,21,22]. One study compared factors associated with the underutilization of ANC services in urban and rural Nigeria [22]. However, there has yet to be a recent study in Nigeria comparing factors associated with inadequate and non-utilization of ANC services among women of different age groups and emphasizing adolescents. This research, therefore, aimed to undertake a comparative study on the factors associated with inadequate and non-utilization of ANC services among women aged 15–19 years, 20–34 years, and 35–49 years. Findings from our study may provide vital information to policymakers and healthcare administrators to design and/or revise strategies geared towards providing adequate ANC services to Nigerian women, particularly adolescents.
2. Materials and Methods
2.1. Data Sources
The analysis is a secondary data analysis of the 2018 Nigeria Demographic and Health Survey (NDHS-6). The survey was conducted by National Population Commission (NPC) with technical assistance provided by the Inner-City Fund (ICF) International. The representative sample consisted of women aged 15–49 years [4]. Two-stage sampling was used to retrieve data for both the rural and urban areas. The first stage consisted of designating the village units as primary sample units and the urban units as census enumeration areas for sampling the households. Across Nigeria, nearly 42,000 households were selected for sampling, and the response rate was 99% [4].
Our analysis was restricted to the women with the most recent singleton live-birth infants within the five years preceding the survey. A weighted total of 21,911 women were considered for the survey. Additionally, our restriction of the sample aimed to reduce the recall bias of women regarding their previous pregnancies.
2.2. Outcome Variables
The World Health Organization (WHO) recommends a number of appropriate components of ANC to be patronized by all pregnant women at ANC clinics. These are blood pressure measurement; screening for conditions and diseases such as anaemia, STIs (particularly syphilis), and HIV infection; tetanus vaccination; intermittent preventive treatment for malaria during pregnancy (IPTp); deworming treatment; and iron–folic-acid supplements [23]. Furthermore, the WHO has recommended that all pregnant women attend an appropriate number of ANC visits. The recommendation is broken down into the following categories: (a) ≥8 ANC visits (b) 4–7 ANC visits, and (c) <4 ANC visits from a skilled health provider for the most recent birth [24].
In our current study, six of the components were used: (a) being given iron tablets/syrup, (b) being given drugs for intestinal parasites, (c) vaccination against tetanus toxoid, (d) checking blood pressure, (e) having blood samples taken, and (f) had urine samples were taken. The current study considered two outcome variables: (i) non-ANC use (no ANC visit and none of the recommended WHO components) and (ii) receipt of inadequate ANC (receiving at most eight ANC visits and receiving less than six recommended WHO components). In our analysis, adequate receipt of ANC was assigned “1”, of inadequate receipt ANC was categorized as “2” and non-use of ANC was assigned “3” and were examined by three categories: adolescent women (15–19 years), young women (20–34 years), and older women (35–49 years).
2.3. Potential Confounding Variables
In this current study, we chose the potential confounding factors based on a behavioral model for health services utilization, proposed by Andersen, and grouped the factors potentially associated with ANC [25]. The Andersen model has been broadly used to examine health service utilization factors [1,18,26,27]. Furthermore, the choice of potential confounding factors was informed by the available variables in the datasets of the NDHS-6. The independent variables were categorized into external, predisposing (socio-demographic and health knowledge), and enabling factors [1,28]. The underlying conceptual framework for this current study is presented in Figure 1.
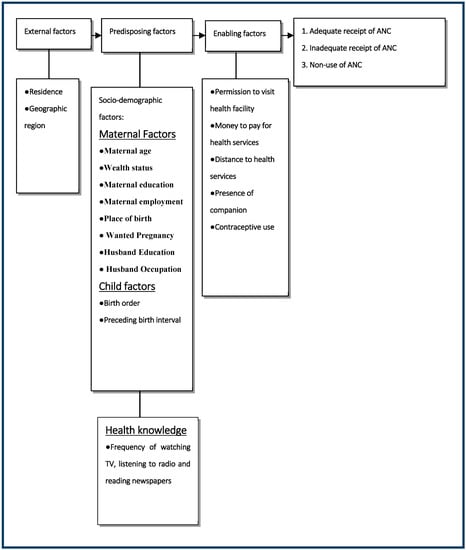
Figure 1.
Conceptual framework of factors associated with no ANC or receipt of inadequate ANC services in Nigeria.
2.4. Statistical Analysis
We conducted our statistical analyses using STATA/MP version 17 (Stata Corp, College Station, TX, USA) [29]. The “Svy” commands were employed to allow for adjustments for the cluster-sampling design and weight. We conducted frequency tabulations to describe the data used in the study and the distributions of inadequate ANC. We used the Taylor series linearization method in the surveys to estimate confidence intervals (CIs) around prevalence estimates of receipt of inadequate quality ANC.
We performed a four-stage model as part of the multinomial logistic regression analysis to calculate the adjusted odds ratios of receipt of inadequate ANC. We entered the basic factors in the first model and undertook a manually executed elimination procedure to examine factors associated with the receipt of inadequate ANC at a 0.05 significance level. In the second model, we added the significant factors in the first stage to the underlying factors, followed by the elimination process. The third and fourth stages used a similar approach for the other factors.
Any co-linearity in the final model was tested and reported. Furthermore, we computed the odds ratios with 95% confidence intervals to assess the factors associated with the independent (possible confounding) variables.
3. Results
3.1. Characteristics of the Sample among Adolescent, Young, and Older Women
Table 1 presents the characteristics of the participants among adolescent, young, and older women. According to Table 1, most women had no formal education and were not working, which was mostly among adolescent women (60.5% and 59.4%). The majority of women across all the age brackets were married, with 89.7%, 94.3%, and 94.8% in the 15–19 years, 20–34 years and 35–49 years age brackets, respectively. Most adolescent women delivered at home 72.1% against 41.4% and 43.1% younger and older women. Most women in all three age brackets (84.8% for 15–19 years, 88.5% for 20–34 years, and 87.9% for 35–49 years) had no problem seeking permission to attend a medical facility on their own, but more reported getting money to pay for health services as a big problem and this was more among the age group 15–19 years (52.3%, 47.7%, 48.6%). The majority of the women aged 15–19 years (adolescent women) lived in rural areas (79.9%), and poor households (62.3%). Most adolescent women did not have access to the mass media (94.6%, 62.4%, and 72.5% of them did not have access to newspapers/magazines, radio, and television, respectively). Only 6.5% of adolescent women attended the minimum of eight ANC clinics, as against 15.6% and 17.2% for younger and older women.

Table 1.
Distribution of characteristics among adolescent, young, and older women in Nigeria (n = 21,872), 2018 NDHS.
3.2. Components of ANC Services Received by Participants
Table 2 presents the receipt of ANC services by pregnant Nigerian women. Overall, more than 6 out of every 10 (63.9%) participants received iron tablets or syrup. The lowest prevalence of iron tablets or syrup intake was among the women in the 15–19 years age bracket (62.6%). Less than 20% of the general participants (16.7%) took any intestinal parasite drugs. The lowest prevalence of participants who took drugs for intestinal parasites was the adolescent (15–19 years) group (12.7%). Nearly 70% of the general participants (69.6%) had tetanus injections before delivery, with the lowest prevalence (60.7%) among the adolescent group. Most participants had their blood pressure checked during pregnancy (71.1%). The adolescent participants had the lowest prevalence of blood pressure checks (60.6%). More than two-thirds of the general participants had their blood samples taken during pregnancy; The adolescent participants had the lowest prevalence of women who had their blood samples taken (53.7%). A little over 65% (65.3%) of the general participants had their urine samples taken during pregnancy, and the adolescent participants had the lowest prevalence of those who had their urine samples taken (53.9%).

Table 2.
Components of antenatal care services received by adolescent, young, and older women during the last pregnancy, 2018 NDHS.
3.3. Prevalence and 95% Confidence Intervals (Cis) of Receipt of ANC Services
Figure 2 shows the prevalence and 95% confidence intervals of receipt of ANC services among adolescent, young, and older women. The prevalence of non-use of ANC ranged from 30.1% to 36.5%, with adolescent women reporting the highest prevalence and young women with the lowest prevalence. However, this prevalence among women did not differ statistically because the confidence intervals overlap. Over 50% of all women reported inadequate receipt of ANC.
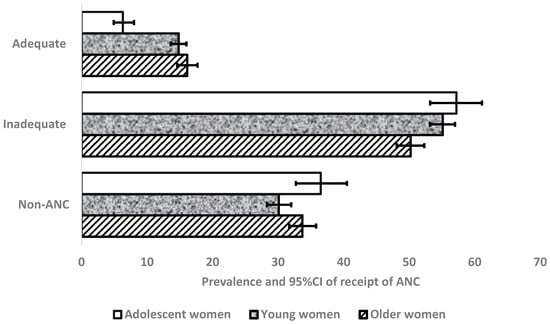
Figure 2.
Prevalence and 95% confidence level of receipts of ANC by adolescent, young, and older women.
3.4. Factors Associated with Inadequate Receipt and Non-Use of ANC Services
3.4.1. Women Aged 15–19 Years
Among the women aged 15–19 years, increased odds of inadequate receipt of ANC were associated with delivery at home [(adjusted odds ratios (OR): 3.40; 95% confidence interval (CI): 1.52, 7.61)], acquisition of medical assistance for any distance to a health facility [OR: 2.06; 95% CI: (0.91, 4.69)], living in the North–East region [OR: 5.02; 95% CI: (1.38, 18.26)], and residence in a rural area [OR: 3.40; 95% CI: (1.52, 7.61)] (Table 3). Decreased odds of inadequate receipt of ANC were associated with residence in the South–South region [OR: 0.09; 95% CI: (0.03, 0.36)] among women aged 15–19 years.

Table 3.
Factors associated with receipt of inadequate receipt of ANC and non-use of ANC among Adolescent women group (15–19 years), 2018 NDHS.
Increased odds of non-use of ANC were associated with delivery at home [OR: 4.70; 95% CI: (2.08, 11.35)], distance to a health facility being a big problem [OR: 16.53; 95% CI: (6.71, 40.73)] and living in a rural area [OR: 16.53; 95% CI: (6.71, 40.73)]. Residence in the South–South region was associated with decreased odds of non-use of ANC among women aged 15–19 years [OR: 0.09; 95% CI: (0.03, 0.36)].
3.4.2. Women Aged 20–34 Years
Among women aged between 20 and 34 years, increased odds of inadequate receipt of ANC were significantly associated with no schooling [OR: 1.52; 95% CI: (1.24, 1.87)], non-use of contraceptives [OR: 1.44; 95% CI: (1.21, 1.71)], non-intention for pregnancy [OR: 1.44; 95% CI: (1.21, 1.71)], belonging to middle-class households [OR: 1.30; 95% CI: (1.05, 1.61)], residing in the North–East region [OR: 4.28; 95% CI: (2.58, 7.08)], and living in a rural area [OR: 1.57; 95% CI: (1.31, 1.88)] (Table 4). Decreased odds of inadequate receipt of ANC were significantly associated with not reading newspapers [OR: 0.70; 95% CI: (0.51, 0.96)] and living in the South–South region [OR: 0.12; 95% CI: (0.09, 0.18)] among women aged 20–34 years (Table 4).

Table 4.
Factors associated with receipt of inadequate components ANC and non-ANC use among young women aged 20–34 years, 2018 NDHS.
Increased odds of non-use of ANC were associated with no schooling [OR: 3.09; 95% CI: (2.34, 4.08)], non-intention for pregnancy [OR: 2.37; 95% CI: (1.41, 3.99)], non-use of contraceptives [OR: 1.73; 95% CI: (1.42, 2.11)], not listening to the radio [OR: 1.43; 95% CI: (1.14, 1.78)], getting permission to attend a health facility being a big problem [OR: 1.62; 95% CI: (1.17, 2.24)], getting the money needed for treatment being a big problem [OR: 1.31; 95% CI: (1.03, 1.66)], being from a poor household [OR: 1.51; 95% CI: (1.10, 2.08)], and living in a rural area [OR: 4.06; 95% CI: (3.33, 4.95)].
3.4.3. Women Aged 35–49 Years
Among women aged 35–49 years, increased odds of inadequate receipt of ANC were associated with no schooling [OR: 1.52; 95% CI: (1.00, 2.31)], living in the North–East region [OR: 3.77; 95% CI: (2.02, 7.03)], being from a poor household [OR: 1.87; 95% CI: (1.29, 2.70)], and living in a rural area [OR: 2.15; 95% CI: (1.59, 2.90)] (Table 5). Decreased odds of inadequate receipt of ANC were associated with being employed [OR: 0.54; 95% CI: (0.38, 0.75)] among women aged 35–49 years (Table 5).

Table 5.
Factors associated with receipt of inadequate components of ANC and non-ANC use among older women aged 35–49 years, 2018 NDHS.
Increased odds of non-use of ANC among women aged 35–49 years were associated with having no schooling [OR: 3.07; 95% CI: (2.00, 4.70)], distance to a health facility being a big problem [OR: 1.81; 95% CI: (1.31, 2.51)], non-use of contraceptives [OR: 1.35; 95% CI: (1.05, 1.75)], living in the North–West region [OR: 2.22; 95% CI: (1.30, 3.80)], being from a poor household [OR: 1.75; 95% CI: (1.16, 2.65)], and living in a rural area [OR: 5.61; 95% CI: (3.99, 7.89)].
4. Discussion
This current study aimed to compare the factors associated with receipt of inadequate or non-use of ANC services among adolescent, younger, and older women in Nigeria, using data extracted from the NDHS-6. The lowest prevalence of receipt of adequate utilization of ANC services and the highest prevalence of receipt of both inadequate and non-use of ANC services was among the adolescent participants. Furthermore, the majority of the participants who lived in rural areas were adolescents. Rural residence was a common predictor of receipt of inadequate or non-use of ANC among all three age brackets of participants. Additionally, more education was needed to be provided as a common predictor of receipt of inadequate or non-use of ANC services among the older participants (20–34 years and 35–49 years).
Previous studies revealed that women with lower educational levels usually have limited knowledge about ANC and more difficulties accessing ANC services [1,30,31,32]. This was confirmed in our current study, where participants’ limited education level was associated with increased odds of receiving inadequate or non-use of ANC services among older women (both women in the 20–34 years and 35–49 years brackets). The association between the level of education and the receipt of inadequate ANC services is consistent with findings from past studies in developing countries [33,34]. The impact of education on the use of maternal health care services could be explained in several ways. Educated women are more likely to know the long-term benefits of utilizing skilled maternity care services for both mother and baby than their less-educated counterparts. The woman’s education is likely to enhance female autonomy, which may consequently help develop greater confidence and capability to make appropriate decisions about their health [35]. There is also the likelihood of educated women seeking higher quality health services and having a higher ability to use health care inputs that provide adequate care [36].
This study found that among women of all three age brackets, residence in a rural area was associated with increased odds of inadequate receipt and non-use of ANC services, consistent with a past study from Bangladesh [37]. The reasons for the decreased odds of receipt of inadequate or non-use of ANC services among urban women compared to their rural counterparts are the ease of access to services and increased knowledge of the adverse health outcomes due to pregnancy-related complications. Moreover, the tendency of rural women to be influenced by traditional practices which contravene modern health care is higher than that of their urban counterparts [38].
In this current study, delivering a baby at home was associated with increased odds of receiving no or inadequate quality ANC among adolescent participants. This is consistent with findings from a past study in Timor-Leste [39], which revealed that home delivery was positively associated with an increased risk of receipt of inadequate and non-use of ANC among adolescent women. There are cultural practices and beliefs associated with the choice of a place of delivery [40]; if a woman’s previous birth was at home and there were no complications, there is the tendency for her not to attend subsequent ANC visits, or she may limit the frequency of such visits. Women who deliver their babies at home are those with higher parity who feel they are experienced in delivering a baby; and tend not to seek assistance, especially when there are no complications [41]. Such women consider child delivery a natural procedure, so they are likely to feel confident about delivering their babies at home. Furthermore, there is evidence that the association between home delivery and non-ANC use may be attributed to a woman’s bad experience with health workers during her previous deliveries [42]. The decision of women to give birth at home may be due to the distance from their homes to health facilities or their socioeconomic status [43]. For example, a study conducted in rural Tanzania observed that women were significantly more likely to deliver at home if the nearest health facility to their home was outside their village [44].
In our current study, with regards to the quality of ANC services received, the prevalence of all six variables of quality ANC services, namely, administering of iron tablets/syrup, drugs for intestinal parasites, and tetanus injection before delivery, as well as blood pressure testing and supplying of both blood and urine samples, was lowest among the adolescent participants.
The extant literature reveals that the increased health risk of a mother and her baby is associated with adolescent pregnancy and childbearing [45]. For instance, a past study reported higher rates of preterm deliveries, prolonged labor, and cephalic pelvic disproportion among teenage girls compared to older women [46]. Other past studies also observed that teenage women’s odds of death during pregnancy and childbirth are higher [47,48]. Apart from the mother, adolescent pregnancy also poses a danger to the baby. Babies born to adolescent women have an increased risk of low birth weight [48]. Babies born to adolescent women in low-income countries also face a 50% chance of stillbirth or death before they turn one month, compared to women aged above 20 years [49]. From these observations, it may be suggested that while minimizing the rate of teenage pregnancies is crucial, a concurrent goal would be to support teenage women towards a safe and healthy pregnancy, delivery, and baby through increased access and utilization of skilled maternal health care [50].
As with participants from the older age brackets, the increased odds of receipt of inadequate or non-use of ANC services were associated with residence in the North–East region of Nigeria. This ought to be expected because of the wide gap in socioeconomic development between the northern and southern parts of the country [51]. There is also evidence to the effect that the North–East region was one of the regions with relatively low ANC services [52].
A major strength of this study was the utilization of NDHS-6 data, population-based and nationally representative, with a large sample size. However, the study’s cross-sectional nature limits the ability to draw any causal inferences, and we could not rule out any residual confounding resulting from other socio-demographic and psychosocial-related determinants. Furthermore, most of the information inquired about in the study was self-reported, which could have led to the under-reporting of certain determinants. Additionally, data were collected retrospectively from participants, which may have resulted in recall bias.
5. Conclusions
Findings from this current study highlight the receipt of inadequate utilization of ANC services among women of all ages, particularly adolescents in Nigeria. The situation appeared to be worse in rural areas, where most of the women live, and most are poor. Results of the study reveal that the factors influencing the utilization of ANC services are mostly socioeconomic- and demographic-related. The rural–urban and regional variations in the ANC services revoke the need to make quality maternal health service facilities available in Nigeria. Consequently, government and other stakeholders should conduct mass media campaigns to highlight the benefits of utilizing ANC services and harmful traditional practices. This can be achieved by informing, educating, and communicating with the rural, lower-educated, and the poor in a bid to promote safe motherhood and a happy and healthy reproductive life among adolescents in Nigeria.
Author Contributions
Conceptualization, E.A.E. and K.E.A.; methodology, K.E.A. and E.A.E.; software, K.E.A.; validation, K.E.A., E.A.E. and M.V.D.; formal analysis, K.E.A. and B.S.; investigation, M.V.D. and B.S.; resources, K.E.A. and M.V.D.; data curation, K.E.A., E.A.E. and A.I.I.; writing—original draft preparation, K.E.A. and A.I.I.; writing—review and editing, E.A.E., A.I.I., M.V.D., B.S. and K.E.A.; visualization, B.S. and E.A.E.; supervision, K.E.A. and E.A.E. project administration, E.A.E., A.I.I., M.V.D., B.S. and K.E.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was based on an analysis of existing survey datasets available online (https://dhsprogram.com/ (accessed on 12 July 2021)), with all identifier information removed. Written informed consent for the present analysis was not necessary because secondary data analysis did not involve interaction with the participants. The surveys were approved by the Ethics Review Board at the International Institute for Population Sciences, Mumbai, India, granted Measure DHS/ICF International ethical approvals before the surveys were conducted, with written informed consent obtained from participants during the surveys. The questionnaires used for the survey were reviewed and approved by ICF International Institutional Review Board (IRB) to ensure they met the United States Department of Health and Human Services regulations for the protection of human participants, as well as the host country’s IRB, to ensure compliance with national laws in Nigeria. We obtained approval from Measure DHS to download and use the data for this study.
Informed Consent Statement
Not applicable.
Data Availability Statement
The study was based on an analysis of existing survey datasets that are available to apply online, with all identifier information removed. Written informed consent for the present analysis was not necessary because secondary data analysis did not involve interaction with the participants. The data collection methods for the NDHS-6 data used in this analysis, including the consent process, have been previously described [4]. Written informed consent for the present analysis was not necessary because secondary data analysis did not involve interaction with the participants.
Acknowledgments
The authors are grateful to Measure DHS, ICF International, Rockville, MD, USA for providing the data for this study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
ANC: Antenatal care; NDHS: Nigeria Demographic and Health Survey; NPC: National Population Commission; ICF: Inner-City Fund; WHO: World Health Organization; SDGs: Sustainable Development Goals; LMIC: low and middle-income countries; AOR: Adjusted Odds ratio; CI: Confidence interval.
References
- Titaley, C.R.; Dibley, M.J.; Roberts, C.L. Factors associated with underutilisation of antenatal care services in Indonesia: Results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health 2010, 10, 485. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Recommendations on Antenatal Care for a Positive Pregnancy Experience; WHO: Geneva, Switzerland, 2016; Available online: https://www.who.int/publications/i/item/9789241549912 (accessed on 19 October 2022).
- World Health Organisation (WHO). Opportunities for Africa’s Newborns: Practical Data, Policy and Programmatic Support for Newborn Care in Africa 2006. Available online: https://asksource.info/resources/opportunities-africas-newborns-practical-data-policy-and-programmatic-support-newborn-care (accessed on 20 October 2022).
- National Population Commission (NPC) [Nigeria]. Nigeria Demographic and Health Survey: 2018 (2018 NDHS); NPC: Abuja, Nigeria; ICF: Rockville, MD, USA, 2019.
- Bhutta, Z.A.; Lassi, Z.S.; Blanc, A.; Donnay, F. Linkages among reproductive health, maternal health, and perinatal outcomes. Semin. Perinatol. 2010, 34, 434–445. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. SDG 3: Ensure Healthy Lives and Promote Wellbeing for All at All Ages. Available online: https://www.who.int/sdg/targets/en/ (accessed on 11 November 2022).
- Campbell, O.M.; Graham, W.J.; Lancet Maternal Survival Series Steering Group. Strategies for reducing maternal mortality: Getting on with what works. Lancet 2006, 368, 1284–1299. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Antenatal Care 2020. Available online: https://data.unicef.org/topic/maternal-health/antenatal-care/#:~:text=Currently%20available%20data%20indicate%20that,at%20least%20four%20antenatal%20visits (accessed on 21 October 2022).
- Dahiru, T.; Oche, O.M. Determinants of antenatal care, institutional delivery and postnatal care services utilisation in Nigeria. Pan Afr. Med. J. 2015, 22. [Google Scholar] [CrossRef]
- Shahabuddin, A.; Delvaux, T.; Abouchadi, S.; Sarker, M.; De Brouwere, V. Utilization of maternal health services among adolescent women in Bangladesh: A scoping review of the literature. Trop. Med. Int. Health 2015, 20, 822–829. [Google Scholar] [CrossRef]
- Mekonnen, T.; Dune, T.; Perz, J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: A systematic scoping review. BMC Pregnancy Childbirth 2019, 19, 366. [Google Scholar] [CrossRef]
- Banke-Thomas, O.E.; Banke-Thomas, A.O.; Ameh, C.A. Factors influencing utilisation of maternal health services by adolescent mothers in Low-and middle-income countries: A systematic review. BMC Pregnancy Childbirth 2017, 17, 65. [Google Scholar] [CrossRef]
- Carvajal, L.; Wilson, E.; Requejo, J.H.; Newby, H.; de Carvalho Eriksson, C.; Liang, M.; Dennis, M.; Gohar, F.; Simen-Kapeu, A.; Idele, P.; et al. Basic maternal health care coverage among adolescents in 22 sub-Saharan African countries with high adolescent birth rate. J. Glob. Health 2020, 10, 021401. [Google Scholar] [CrossRef]
- Owolabi, O.O.; Wong, K.L.; Dennis, M.L.; Radovich, E.; Cavallaro, F.L.; Lynch, C.A.; Benova, L. Comparing the use and content of antenatal care in adolescent and older first-time mothers in 13 countries of West Africa: A cross-sectional analysis of Demographic and Health Surveys. Lancet Child Adolesc. Health 2017, 1, 203–212. [Google Scholar] [CrossRef]
- Singh, A.; Kumar, A.; Pranjali, P. Utilization of maternal healthcare among adolescent mothers in urban India: Evidence from DLHS-3. PeerJ 2014, 2, e592. [Google Scholar] [CrossRef]
- Ahmed, S.; Creanga, A.A.; Gillespie, D.G.; Tsui, A.O. Economic status, education and empowerment: Implications for maternal health service utilisation in developing countries. PLoS ONE 2010, 5, e11190. [Google Scholar] [CrossRef]
- Rurangirwa, A.A.; Mogren, I.; Nyirazinyoye, L.; Ntaganira, J.; Krantz, G. Determinants of poor utilisation of antenatal care services among recently delivered women in Rwanda; a population-based study. BMC Pregnancy Childbirth 2017, 17, 142. [Google Scholar] [CrossRef]
- Gupta, S.; Yamada, G.; Mpembeni, R.; Frumence, G.; Callaghan-Koru, J.A.; Stevenson, R.; Brandes, N.; Baqui, A.H. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS ONE 2014, 9, e101893. [Google Scholar] [CrossRef]
- Swenson, I.; Thang, N.M.; Nhan, V.; Tieu, P.X. Factors related to the utilisation of prenatal care in Vietnam. J. Trop. Med. Hyg. 1993, 96, 76–85. [Google Scholar]
- Fagbamigbe, A.F.; Idemudia, E.S. Barriers to antenatal care use in Nigeria: Evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth 2015, 15, 95. [Google Scholar] [CrossRef]
- Agho, K.E.; Ezeh, O.K.; Ogbo, F.A.; Enoma, A.I.; Raynes-Greenow, C. Factors associated with inadequate receipt of components and use of antenatal care services in Nigeria: A population-based study. Int. Health 2018, 10, 172–181. [Google Scholar] [CrossRef]
- Adewuyi, E.O.; Auta, A.; Khanal, V.; Bamidele, O.D.; Akuoko, C.P.; Adefemi, K.; Zhao, Y. Prevalence and factors associated with underutilisation of antenatal care services in Nigeria: A comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLoS ONE 2018, 13, e0197324. [Google Scholar] [CrossRef]
- Lincetto, O.; Mothebesoane-Anoh, S.; Gomez, P.; Munjanja, S. Antenatal Care. Opportunities for Africa’s Newborns: Practical Data, Policy and Programmatic Support for Newborn Care in Africa; World Health Organisation (WHO): Cape Town, South Africa, 2006; pp. 51–62. [Google Scholar]
- United Nations Children’s Fund. Guide to DHS Statistics DHS-7. Available online: https://dhsprogram.com/Data/Guide-to-DHS-Statistics (accessed on 29 October 2022).
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Deri, C. Social networks and health service utilisation. J. Health Econ. 2005, 24, 1076–1107. [Google Scholar] [CrossRef]
- Alanazy, W.; Brown, A. Individual and healthcare system factors influencing antenatal care attendance in Saudi Arabia. BMC Health Serv. Res. 2020, 20, 49. [Google Scholar] [CrossRef]
- Karkee, R.; Lee, A.H.; Khanal, V. Need factors for utilisation of institutional delivery services in Nepal: An analysis from Nepal Demographic and Health Survey, 2011. BMJ Open 2014, 4, e004372. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata: Release 17. Statistical Software; StataCorp LP.: College Station, TX, USA, 2021. [Google Scholar]
- Trinh, L.T.T.; Dibley, M.J.; Byles, J. Determinants of antenatal care utilisation in three rural areas of Vietnam. Public Health Nurs. 2007, 24, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Nagdev, N.; Ogbo, F.A.; Dhami, M.V.; Diallo, T.; Lim, D.; Agho, K.E. Factors associated with inadequate receipt of components and non-use of antenatal care services in India: A regional analysis. BMC Public Health 2023, 23, 6. [Google Scholar] [CrossRef] [PubMed]
- Shariff, A.; Singh, G. Determinants of Maternal Health Care Utilisation in India: Evidence from a Recent Household Survey; National Council of Applied Economic Research: New Dehli, India, 2002. [Google Scholar]
- Addai, I. Determinants of use of maternal-child health services in rural Ghana. J. Biosoc. Sci. 2000, 32, 1–15. [Google Scholar] [CrossRef]
- Chakraborty, N.; Islam, M.A.; Chowdhury, R.I.; Bari, W.; Akhter, H.H. Determinants of the use of maternal health services in rural Bangladesh. Health Promot. Int. 2003, 18, 327–337. [Google Scholar] [CrossRef]
- Raghupathy, S. Education and the use of maternal health care in Thailand. Soc. Sci. Med. 1996, 43, 459–471. [Google Scholar] [CrossRef]
- Celik, Y.; Hotchkiss, D.R. The socioeconomic determinants of maternal health care utilisation in Turkey. Soc. Sci. Med. 2000, 50, 1797–1806. [Google Scholar] [CrossRef]
- Kamal, S.M. Factors affecting utilisation of skilled maternity care services among married adolescents in Bangladesh. Asian Popul. Stud. 2009, 5, 153–170. [Google Scholar] [CrossRef]
- Mekonnen, Y.; Mekonnen, A. Utilization of maternal health care services in Ethiopia. Calverton, MD: ORC Macro. BMC Public Health 2002, 12, 30. [Google Scholar]
- Khanal, V.; Lee, A.H.; da Cruz, J.L.N.B.; Karkee, R. Factors associated with non-utilisation of health service for childbirth in Timor-Leste: Evidence from the 2009-2010 Demographic and Health Survey. BMC Int. Health Hum. Rights 2014, 14, 1. [Google Scholar] [CrossRef]
- Samson, G. Utilization and Factors Affecting Delivery in Health Facility among Recently Delivered Women in Nkasi District; Muhimbili University of Health and Allied Sciences: Dar es Salaam, Tanzania, 2012. [Google Scholar]
- Kitui, J.; Lewis, S.; Davey, G. Factors influencing place of delivery for women in Kenya: An analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy Childbirth 2013, 13, 40. [Google Scholar] [CrossRef]
- Hazarika, I. Factors that determine the use of skilled care during delivery in India: Implications for achievement of MDG-5 targets. Matern. Child Health J. 2011, 15, 1381–1388. [Google Scholar] [CrossRef]
- Atuhaire, S.; Mugisha, J. Determinants of antenatal care visits and their impact on the choice of birthplace among mothers in Uganda: A systematic review. Obstet. Gynecol. Int. J. 2020, 11, 77–81. [Google Scholar] [CrossRef]
- Rockers, P.C.; Wilson, M.L.; Mbaruku, G.; Kruk, M.E. Source of antenatal care influences facility delivery in rural Tanzania: A population-based study. Matern. Child Health J. 2009, 13, 879. [Google Scholar] [CrossRef]
- Nove, A.; Matthews, Z.; Neal, S.; Camacho, A.V. Maternal mortality in adolescents compared with women of other ages: Evidence from 144 countries. Lancet Glob. Health 2014, 2, e155–e164. [Google Scholar] [CrossRef]
- Kumbi, S.; Isehak, A. Obstetric outcome of teenage pregnancy in northwestern Ethiopia. East Afr. Med. J. 1999, 76, 138–140. [Google Scholar]
- Morris, J.L.; Rushwan, H. Adolescent sexual and reproductive health: The global challenges. Int. J. Gynecol. Obstet. 2015, 131, S40–S42. [Google Scholar] [CrossRef]
- Kurth, F.; Belard, S.; Mombo-Ngoma, G.; Schuster, K.; Adegnika, A.A.; Bouyou-Akotet, M.K.; Kremsner, P.G.; Ramharter, M. Adolescence as risk factor for adverse pregnancy outcome in Central Africa–a cross-sectional study. PLoS ONE 2010, 5, e14367. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Adolescent Pregnancy. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy (accessed on 21 December 2022).
- World Health Organisation (WHO). Making Pregnancy Safer: The Critical Role of the Skilled Attendant: A Joint Statement by WHO, ICM and FIGO; World Health Organization: Geneva, Switzerland, 2004; Available online: https://apps.who.int/iris/handle/10665/42955 (accessed on 15 January 2023).
- Ejembi, C.L.; Dahiru, T.; Aliyu, A.A. Contextual Factors Influencing Modern Contraceptive Use in Nigeria; DHS Working Papers; ICF International: Rockville, MD, USA, 2015. [Google Scholar]
- Okoli, C.; Hajizadeh, M.; Rahman, M.M.; Khanam, R. Geographical and socioeconomic inequalities in the utilisation of maternal healthcare services in Nigeria: 2003–2017. BMC Health Serv. Res. 2020, 20, 849. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).