Religiosity, Theism, Perceived Social Support, Resilience, and Well-Being of University Undergraduate Students in Singapore during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
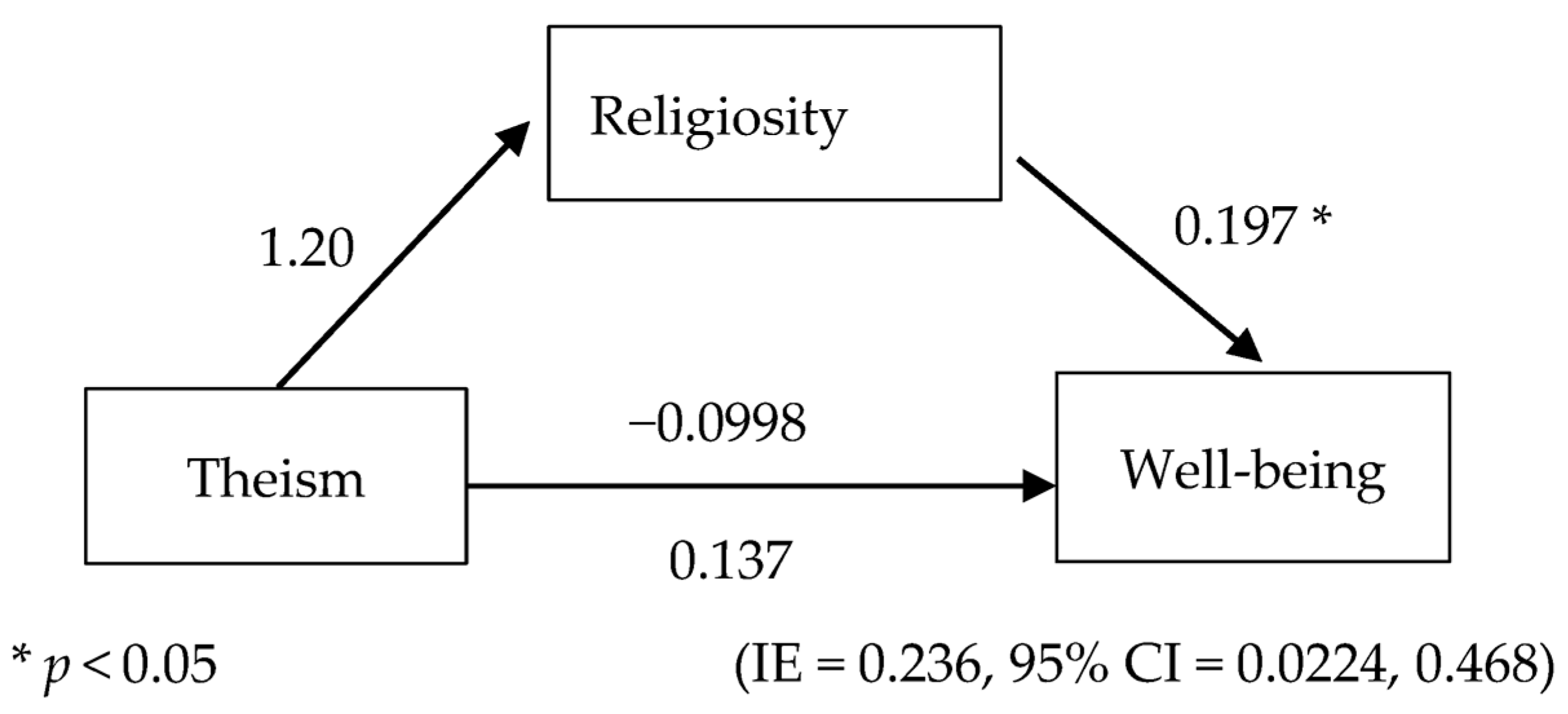
2.2. Mediation Analysis 1
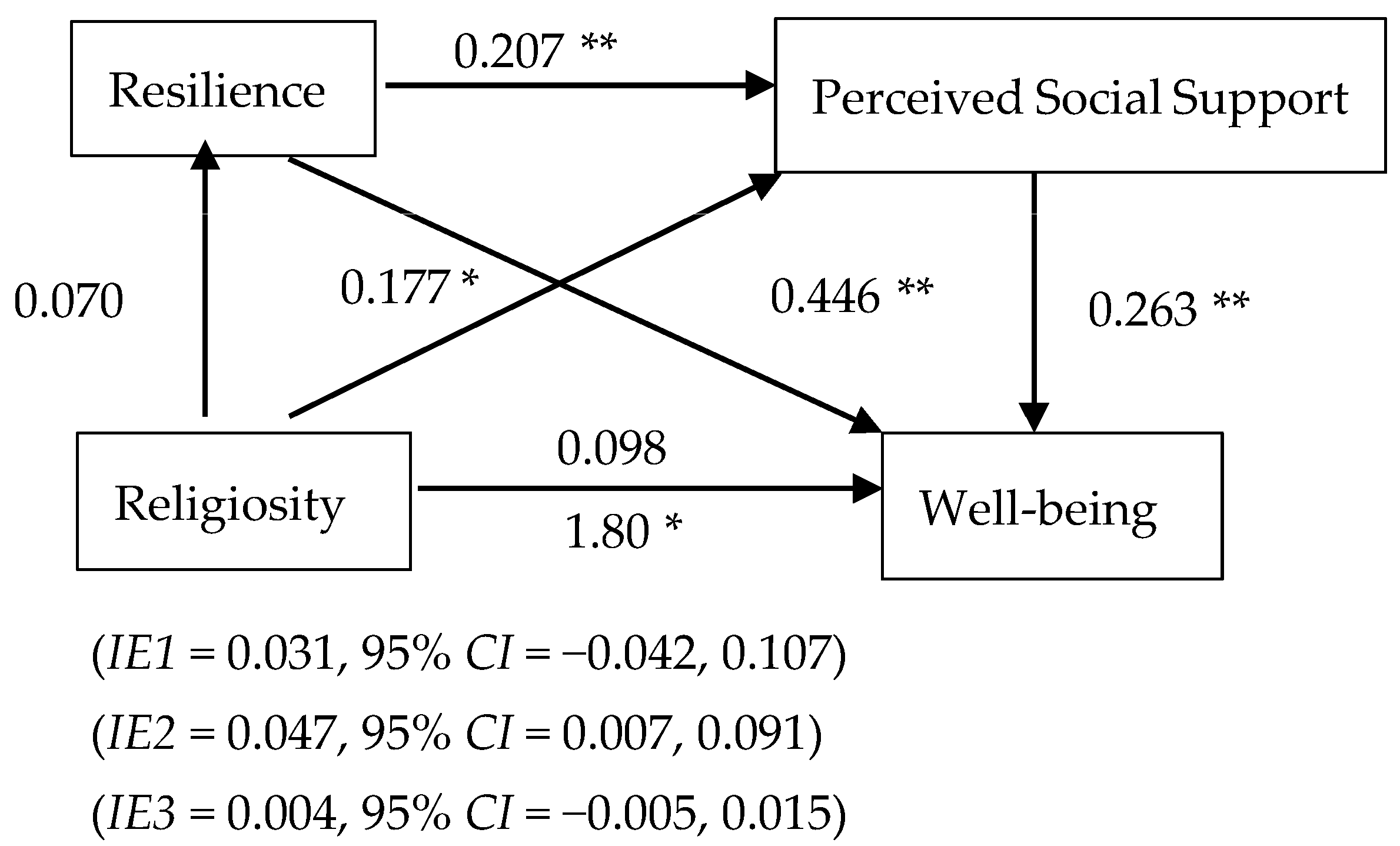
2.3. Mediation Analysis 2
2.4. Participants
2.5. Demographics
Interreligious Centrality of Religiosity Scale (CRSi-20)
2.6. Brief Resilience Scale (BRS)
2.7. Multidimensional Scale of Perceived Social Support (MSPSS)
2.8. Warwick–Edinburg Mental Well-Being Scale (WEMWBS)
2.9. Paranormal Belief Questionnaire (PBQ)
2.10. Exercise Behaviors
2.11. Procedure
2.12. Mediation Analysis
3. Results
3.1. Assumption Testing
3.2. Hypotheses Testing—Mediation Analysis 1
3.2.1. Correlation between Variables
3.2.2. Mediation Analysis
3.3. Hypotheses Testing—Mediation Analysis 2
3.3.1. Correlations between Variables
3.3.2. Mediation Analysis
4. Discussion
Limitations and Future Work
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Francis, P.C.; Horn, A.S. Mental Health Issues and Counseling Services in US Higher Education: An Overview of Recent Research and Recommended Practices. High. Educ. Policy 2017, 30, 263–277. [Google Scholar] [CrossRef]
- Liu, C.; McCabe, M.; Dawson, A.; Cyrzon, C.; Shankar, S.; Gerges, N.; Kellett-Renzella, S.; Chye, Y.; Cornish, K. Identifying Predictors of University Students’ Wellbeing during the COVID-19 Pandemic—A Data-Driven Approach. Int. J. Environ. Res. Public Health 2021, 18, 6730. [Google Scholar] [CrossRef] [PubMed]
- Heng, Z.S.-L.; Koh, D.W.-S.; Yeo, J.Y.; Ooi, C.-P.; Gan, S.K.-E. Effects of different delivery modes on teaching biomedical science practical skills in higher education during the 2021 pandemic measures. Biochem. Mol. Biol. Educ. 2022, 50, 403–413. [Google Scholar] [CrossRef]
- Rosenberg, C.E. Explaining Epidemics and Other Studies in the History of Medicine; Cambridge University Press: Cambridge, UK, 1992. [Google Scholar]
- Abdel-Khalek, A.M. Quality of life, subjective well-being, and religiosity in Muslim college students. Qual. Life Res. 2010, 19, 1133–1143. [Google Scholar] [CrossRef] [PubMed]
- Wildman, W.J.; Sosis, R. Post-Pandemic Religion. Relig. Brain Behav. 2021, 11, 237–238. [Google Scholar] [CrossRef]
- Boguszewski, R.; Makowska, M.; Bożewicz, M.; Podkowińska, M. The COVID-19 Pandemic’s Impact on Religiosity in Poland. Religions 2020, 11, 646. [Google Scholar] [CrossRef]
- Sahgal, N.; Connaughton, A. More Americans Than People in Other Advanced Economies Say COVID-19 Has Strengthened Religious Faith; Pew Research Center: Washington, DC, USA, 2021. [Google Scholar]
- Dilmaghani, M. Religiosity and subjective wellbeing in Canada. J. Happiness Stud. Interdiscip. Forum Subj. Well-Being 2018, 19, 629–647. [Google Scholar] [CrossRef]
- Krok, D. The Role of Meaning in Life within the Relations of Religious Coping and Psychological Well-Being. J. Relig. Health 2015, 54, 2292–2308. [Google Scholar] [CrossRef]
- Paterson, J.; Francis, A.J.P. Influence of religiosity on self-reported response to psychological therapies. Ment. Health Relig. Cult. 2017, 20, 428–448. [Google Scholar] [CrossRef]
- Revens, K.E.; Gutierrez, D.; Paul, R.; Reynolds, A.D.; Price, R.; DeHaven, M.J. Social Support and Religiosity as Contributing Factors to Resilience and Mental Wellbeing in Latino Immigrants: A Community-Based Participatory Research Study. J. Immigr. Minor. Health 2021, 23, 904–916. [Google Scholar] [CrossRef] [PubMed]
- Farag, P.; Behzadi, A. Investigating the Relationship between Religiosity and Psychological Distress among Surgical Inpatients: A Pilot Study. J. Relig. Health 2018, 57, 291–310. [Google Scholar] [CrossRef] [PubMed]
- Malinakova, K.; Tavel, P.; Meier, Z.; van Dijk, J.P.; Reijneveld, S.A. Religiosity and Mental Health: A Contribution to Understanding the Heterogeneity of Research Findings. Int. J. Environ. Res. Public Health 2020, 17, 494. [Google Scholar] [CrossRef]
- O’Connor, D.B.; Cobb, J.; O’Connor, R.C. Religiosity, stress and psychological distress: No evidence for an association among undergraduate students. Personal. Individ. Differ. 2003, 34, 211–217. [Google Scholar] [CrossRef]
- Diener, E.; Tay, L.; Myers, D.G. The religion paradox: If religion makes people happy, why are so many dropping out? J. Personal. Soc. Psychol. 2011, 101, 1278–1290. [Google Scholar] [CrossRef]
- Koushede, V.; Lasgaard, M.; Hinrichsen, C.; Meilstrup, C.; Nielsen, L.; Rayce, S.B.; Torres-Sahli, M.; Gudmundsdottir, D.G.; Stewart-Brown, S.; Santini, Z.I. Measuring mental well-being in Denmark: Validation of the original and short version of the Warwick-Edinburgh mental well-being scale (WEMWBS and SWEMWBS) and cross-cultural comparison across four European settings. Psychiatry Res. 2019, 271, 502–509. [Google Scholar] [CrossRef]
- Stewart-Brown, S. Defining and measuring mental health and wellbeing. In Public Mental Health: Global Perspectives; Open University Press: Maidenhead, UK, 2013; pp. 33–42. [Google Scholar]
- Koenig, H.G.; King, D.E.; Carson, V.B. Handbook of Religion and Health, 2nd ed.; Oxford University Press: New York, NY, USA, 2012; p. 1169-xv. [Google Scholar]
- Khodaveirdyzadeh, R.; Rahimi, R.; Rahmani, A.; Ghahramanian, A.; Kodayari, N.; Eivazi, J. Spiritual/Religious Coping Strategies and their Relationship with Illness Adjustment among Iranian Breast Cancer Patients. Asian Pac. J. Cancer Prev. 2016, 17, 4095–4099. [Google Scholar]
- Oman, D.; Syme, S.L. Weighing the Evidence: What Is Revealed by 100+ Meta-Analyses and Systematic Reviews of Religion/Spirituality and Health? In Why Religion and Spirituality Matter for Public Health: Evidence, Implications, and Resources; Oman, D., Ed.; Springer International Publishing: Cham, Switzerland, 2018; pp. 261–281. [Google Scholar]
- Roger, K.S.; Hatala, A. Religion, spirituality & chronic illness: A scoping review and implications for health care practitioners. J. Relig. Spiritual. Soc. Work: Soc. Thought 2018, 37, 24–44. [Google Scholar] [CrossRef]
- Gorsuch, R.L.; Smith, C.S. Attributions of Responsibility to God: An Interaction of Religious Beliefs and Outcomes. J. Sci. Study Relig. 1983, 22, 340–352. [Google Scholar] [CrossRef]
- Spilka, B.; Hood, R.W.; Hunsberger, B.; Gorsuch, R. The Psychology of Religion: An Empirical Approach; Guilford Press: New York, NY, USA, 2003. [Google Scholar]
- Schieman, S. The Religious Role and the Sense of Personal Control. Sociol. Relig. 2008, 69, 273–296. [Google Scholar] [CrossRef]
- Schieman, S. Socioeconomic Status and Beliefs about God’s Influence in Everyday Life. Sociol. Relig. 2010, 71, 25–51. [Google Scholar] [CrossRef]
- Tan, M.M.; Su, T.T.; Ting, R.S.; Allotey, P.; Reidpath, D. Religion and mental health among older adults: Ethnic differences in Malaysia. Aging Ment Health 2021, 25, 2116–2123. [Google Scholar] [CrossRef] [PubMed]
- Aydogdu, R.; Yildiz, M.; Orak, U. Religion and wellbeing: Devotion, happiness and life satisfaction in Turkey. Ment. Health Relig. Cult. 2021, 24, 961–975. [Google Scholar] [CrossRef]
- Murken, S.; Mülle, C.; Huber, S.; Rüddel, H.; Körber, J. The role of religion for coping with breast cancer. Int. J. Behav. Med. 2004, 11, 332. [Google Scholar]
- Formoso-Suárez, A.M.; Saiz, J.; Chopra, D.; Mills, P.J. The Impact of Religion and Social Support on Self-Reported Happiness in Latin American Immigrants in Spain. Religions 2022, 13, 122. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am. Psychol. 2001, 56, 218. [Google Scholar] [CrossRef]
- Helmreich, I.; Kunzler, A.; Chmitorz, A.; König, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst. Rev. 2017, 2017, CD012527. [Google Scholar] [CrossRef]
- Lin, N.; Ensel, W.M.; Simeone, R.S.; Kuo, W. Social Support, Stressful Life Events, and Illness: A Model and an Empirical Test. J. Health Soc. Behav. 1979, 20, 108–119. [Google Scholar] [CrossRef]
- Li, F.; Luo, S.; Mu, W.; Li, Y.; Ye, L.; Zheng, X.; Xu, B.; Ding, Y.; Ling, P.; Zhou, M.; et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 16. [Google Scholar] [CrossRef]
- Collins, S. Statutory Social Workers: Stress, Job Satisfaction, Coping, Social Support and Individual Differences. Br. J. Soc. Work 2007, 38, 1173–1193. [Google Scholar] [CrossRef]
- Dour, H.J.; Wiley, J.F.; Roy-Byrne, P.; Stein, M.B.; Sullivan, G.; Sherbourne, C.D.; Bystritsky, A.; Rose, R.D.; Craske, M.G. Perceived social support mediates anxiety and depressive symptom changes following primary care intervention. Depress. Anxiety 2014, 31, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Ibarra-Rovillard, M.S.; Kuiper, N.A. Social support and social negativity findings in depression: Perceived responsiveness to basic psychological needs. Clin. Psychol. Rev. 2011, 31, 342–352. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef]
- Stronge, S.; Overall, N.C.; Sibley, C.G. Gender differences in the associations between relationship status, social support, and wellbeing. J. Fam. Psychol. 2019, 33, 819–829. [Google Scholar] [CrossRef]
- Harper, F.W.K.; Peterson, A.M.; Albrecht, T.L.; Taub, J.W.; Phipps, S.; Penner, L.A. Satisfaction with support versus size of network: Differential effects of social support on psychological distress in parents of pediatric cancer patients. Psycho-Oncology 2016, 25, 551–558. [Google Scholar] [CrossRef]
- Koelmel, E.; Hughes, A.J.; Alschuler, K.N.; Ehde, D.M. Resilience Mediates the Longitudinal Relationships between Social Support and Mental Health Outcomes in Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2017, 98, 1139–1148. [Google Scholar] [CrossRef]
- The PLoS ONE Staff. Correction: Psychometric properties of the Resilience Scale for Adults (RSA) and its relationship with life-stress, anxiety and depression in a Hispanic Latin-American community sample. PLoS ONE 2018, 13, e0196139. [Google Scholar] [CrossRef]
- Helliwell, J.F.; Barrington-Leigh, C.; Harris, A.; Huang, H. International evidence on the social context of well-being. In International Differences in Well-Being; Oxford University Press: New York, NY, USA, 2010; pp. 291–327. [Google Scholar]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Burns, D.; Dagnall, N.; Holt, M. Assessing the Impact of the COVID-19 Pandemic on Student Wellbeing at Universities in the United Kingdom: A Conceptual Analysis. Front. Educ. 2020, 5, 582882. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Tugade, M.M.; Waugh, C.E.; Larkin, G.R. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J. Pers. Soc. Psychol. 2003, 84, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Vagni, M.; Maiorano, T.; Giostra, V.; Pajardi, D. Hardiness, Stress and Secondary Trauma in Italian Healthcare and Emergency Workers during the COVID-19 Pandemic. Sustainability 2020, 12, 5592. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J. Personal. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Jiang, J.; Du, X.; Gu, D.; Sun, Y.; Zhang, Y. Striving and happiness: Between- and within-person-level associations among grit, needs satisfaction and subjective well-being. J. Posit. Psychol. 2020, 15, 543–555. [Google Scholar] [CrossRef]
- Coulombe, S.; Pacheco, T.; Cox, E.; Khalil, C.; Doucerain, M.M.; Auger, E.; Meunier, S. Risk and Resilience Factors During the COVID-19 Pandemic: A Snapshot of the Experiences of Canadian Workers Early on in the Crisis. Front. Psychol. 2020, 11, 580702. [Google Scholar] [CrossRef] [PubMed]
- Block, J.; Kremen, A.M. IQ and ego-resiliency: Conceptual and empirical connections and separateness. J. Personal. Soc. Psychol. 1996, 70, 349–361. [Google Scholar] [CrossRef]
- Cohler, B.J. Adversity, resilience, and the study of lives. In The Invulnerable Child; The Guilford Press: New York, NY, USA, 1987; pp. 363–424. [Google Scholar]
- Klohnen, E.C. Conceptual analysis and measurement of the construct of ego-resiliency. J. Personal. Soc. Psychol. 1996, 70, 1067–1079. [Google Scholar] [CrossRef]
- Dijksterhuis, G.B.; van Bergen, G.; de Wijk, R.A.; Zandstra, E.H.; Kaneko, D.; Vingerhoeds, M. Exploring impact on eating behaviour, exercise and well-being during COVID-19 restrictions in the Netherlands. Appetite 2022, 168, 105720. [Google Scholar] [CrossRef]
- Martínez-de-Quel, Ó.; Suárez-Iglesias, D.; López-Flores, M.; Pérez, C.A. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite 2021, 158, 105019. [Google Scholar] [CrossRef]
- Ranasinghe, C.; Ozemek, C.; Arena, R. Exercise and well-being during COVID 19—Time to boost your immunity. Expert Rev. Anti-Infect. Ther. 2020, 18, 1195–1200. [Google Scholar] [CrossRef]
- Anderson, E.; Shivakumar, G. Effects of Exercise and Physical Activity on Anxiety. Front. Psychiatry 2013, 4, 27. [Google Scholar] [CrossRef] [PubMed]
- Petruzzello, S.J.; Landers, D.M.; Hatfield, B.D.; Kubitz, K.A.; Salazar, W. A Meta-Analysis on the Anxiety-Reducing Effects of Acute and Chronic Exercise. Sport. Med. 1991, 11, 143–182. [Google Scholar] [CrossRef]
- Jackson, E.M.; Dishman, R.K. Cardiorespiratory fitness and laboratory stress: A meta-regression analysis. Psychophysiology 2006, 43, 57–72. [Google Scholar] [CrossRef] [PubMed]
- Rimmele, U.; Zellweger, B.C.; Marti, B.; Seiler, R.; Mohiyeddini, C.; Ehlert, U.; Heinrichs, M. Trained men show lower cortisol, heart rate and psychological responses to psychosocial stress compared with untrained men. Psychoneuroendocrinology 2007, 32, 627–635. [Google Scholar] [CrossRef] [PubMed]
- De Kloet, E.R.; Joëls, M.; Holsboer, F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005, 6, 463–475. [Google Scholar] [CrossRef]
- Steckler, T.; Holsboer, F.; Reul, J.M. Glucocorticoids and depression. Best Pract. Res. Clin. Endocrinol. Metab. 1999, 13, 597–614. [Google Scholar] [CrossRef]
- Wu, G.; Feder, A.; Cohen, H.; Kim, J.; Calderon, S.; Charney, D.; Mathé, A. Understanding resilience. Front. Behav. Neurosci. 2013, 7, 10. [Google Scholar] [CrossRef]
- Mladenova, Z. Psychological responses, coping strategies, and physical activity during the COVID-19 pandemic: Bulgarian perspective. J. Appl. Sport. Sci. 2021, 1, 93–105. [Google Scholar] [CrossRef]
- Xu, S.; Liu, Z.; Tian, S.; Ma, Z.; Jia, C.; Sun, G. Physical Activity and Resilience among College Students: The Mediating Effects of Basic Psychological Needs. Int. J. Environ. Res. Public Health 2021, 18, 3722. [Google Scholar] [CrossRef]
- Sciolino, N.R.; Dishman, R.K.; Holmes, P.V. Voluntary exercise offers anxiolytic potential and amplifies galanin gene expression in the locus coeruleus of the rat. Behav. Brain Res. 2012, 233, 191–200. [Google Scholar] [CrossRef]
- Karlsson, R.M.; Holmes, A. Galanin as a modulator of anxiety and depression and a therapeutic target for affective disease. Amino Acids 2006, 31, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Cosmas, G. Psychological support in uplifting university students’ happiness in fighting the coronavirus lockdown. Postmod. Open. 2020, 11, 31–42. [Google Scholar] [CrossRef]
- Jackson, S.L. Faith, Resilience and Practice: The Relationship as the Medium for Connected Teaching. Soc. Work Christ. 2021, 48, 106–110. [Google Scholar] [CrossRef]
- Brewer-Smyth, K.; Koenig, H.G. Could Spirituality and Religion Promote Stress Resilience in Survivors of Childhood Trauma? Issues Ment. Health Nurs. 2014, 35, 251–256. [Google Scholar] [CrossRef]
- Freire de Medeiros, C.M.M.; Arantes, E.P.; Tajra, R.D.d.P.; Santiago, H.R.; Carvalho, A.F.; Libório, A.B. Resilience, religiosity and treatment adherence in hemodialysis patients: A prospective study. Psychol. Health Med. 2017, 22, 570–577. [Google Scholar] [CrossRef]
- Fradelos, E.C.; Latsou, D.; Mitsi, D.; Tsaras, K.; Lekka, D.; Lavdaniti, M.; Tzavella, F.; Papathanasiou, I.V. Assessment of the relation between religiosity, mental health, and psychological resilience in breast cancer patients. Contemp. Oncol./Współczesna Onkol. 2018, 22, 172–177. [Google Scholar] [CrossRef]
- Mosqueiro, B.P.; da Rocha, N.S.; Fleck, M.P.d.A. Intrinsic religiosity, resilience, quality of life, and suicide risk in depressed inpatients. J. Affect. Disord. 2015, 179, 128–133. [Google Scholar] [CrossRef]
- Del Castillo, F.; del Castillo, C.D.; Aliño, M.A.; Nob, R.; Ackert, M.; Ching, G. Validation of the Interreligious Forms of the Centrality of Religiosity Scale (CRSi-7, CRSi-14, and CRSi-20): Salience of Religion among Selected Youth in the Philippines. Religions 2020, 11, 641. [Google Scholar] [CrossRef]
- Del Castillo, F.; del Castillo, C.D.; Ching, G.; Ackert, M.; Aliño, M.A.; Nob, R. Validation of the Abrahamic Forms of the Centrality of Religiosity Scale (CRS-5, CRS-10, and CRS-15): Evidence from Selected University Students in the Philippines. Religions 2021, 12, 84. [Google Scholar] [CrossRef]
- Koenig, H.G.; Büssing, A. The Duke University Religion Index (DUREL): A Five-Item Measure for Use in Epidemological Studies. Religions 2010, 1, 78–85. [Google Scholar] [CrossRef]
- Pearce, L.D.; Hayward, G.M.; Pearlman, J.A. Measuring Five Dimensions of Religiosity across Adolescence. Rev. Relig. Res. 2017, 59, 367–393. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Religion, Spirituality, and Health: The Research and Clinical Implications. ISRN Psychiatry 2012, 2012, 278730. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Chapter 3—Religion and Coping. In Religion and Mental Health; Koenig, H.G., Ed.; Academic Press: San Diego, CA, USA, 2018; pp. 49–77. [Google Scholar]
- Cunha, V.F.d.; Pillon, S.C.; Zafar, S.; Wagstaff, C.; Scorsolini-Comin, F. Brazilian nurses’ concept of religion, religiosity, and spirituality: A qualitative descriptive study. Nurs. Health Sci. 2020, 22, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Milevsky, A. Religiosity and social support: A mediational model of adjustment in emerging adults. Ment. Health Relig. Cult. 2017, 20, 502–512. [Google Scholar] [CrossRef]
- Edara, I.R.; del Castillo, F.; Ching, G.S.; del Castillo, C.D. Religiosity, Emotions, Resilience, and Wellness during the COVID-19 Pandemic: A Study of Taiwanese University Students. Int. J. Environ. Res. Public Health 2021, 18, 6381. [Google Scholar] [CrossRef] [PubMed]
- Sosis, R.; Alcorta, C. Signaling, solidarity, and the sacred: The evolution of religious behavior. Evol. Anthropol. Issues News Rev. 2003, 12, 264–274. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Huber, S.; Huber, O.W. The Centrality of Religiosity Scale (CRS). Religions 2012, 3, 710–724. [Google Scholar] [CrossRef]
- Lee, J.C.-K.; Kuang, X. Validation of the Chinese Version of the Centrality of Religiosity Scale (CRS): Teacher Perspectives. Religions 2020, 11, 266. [Google Scholar] [CrossRef]
- Fung, S.-F. Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. Int. J. Environ. Res. Public Health 2020, 17, 1265. [Google Scholar] [CrossRef]
- Hidalgo-Rasmussen, C.A.; González-Betanzos, F. El tratamiento de la Aquiescencia y la Estructura Factorial de la Escala Breve de Resiliencia (BRS) en estudiantes universitarios mexicanos y chilenos. An. Psicol. Ann. Psychol. 2018, 35, 26–32. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Dambi, J.M.; Corten, L.; Chiwaridzo, M.; Jack, H.; Mlambo, T.; Jelsma, J. A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health Qual. Life Outcomes 2018, 16, 80. [Google Scholar] [CrossRef]
- Ekbäck, M.; Benzein, E.; Lindberg, M.; Årestedt, K. The Swedish version of the multidimensional scale of perceived social support (MSPSS)—A psychometric evaluation study in women with hirsutism and nursing students. Health Qual. Life Outcomes 2013, 11, 168. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wan, Q.; Huang, Z.; Huang, L.; Kong, F. Psychometric Properties of Multi-Dimensional Scale of Perceived Social Support in Chinese Parents of Children with Cerebral Palsy. Front. Psychol. 2017, 8, 2020. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.-G.; Jeong, Y.-J.; Bang, J.-A. Effect of social support on parenting stress of korean mothers of children with cerebral palsy. J. Phys. Sci. 2013, 25, 1339–1342. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.; Ding, K.; Zhao, J. The Relationships among Gratitude, Self-esteem, Social Support and Life Satisfaction among Undergraduate Students. J. Happiness Stud. 2015, 16, 477–489. [Google Scholar] [CrossRef]
- Zhao, J.; Kong, F.; Wang, Y. The role of social support and self-esteem in the relationship between shyness and loneliness. Personal. Individ. Differ. 2013, 54, 577–581. [Google Scholar] [CrossRef]
- Stewart, R.C.; Umar, E.; Tomenson, B.; Creed, F. Validation of the multi-dimensional scale of perceived social support (MSPSS) and the relationship between social support, intimate partner violence and antenatal depression in Malawi. BMC Psychiatry 2014, 14, 180. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Lloyd, K.; Devine, P. Psychometric properties of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS) in Northern Ireland. J. Ment. Health 2012, 21, 257–263. [Google Scholar] [CrossRef]
- Stewart-Brown, S.; Platt, S.; Tennant, A.; Maheswaran, H.; Parkinson, J.; Weich, S.; Tennant, R.; Taggart, F.; Clarke, A. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): A valid and reliable tool for measuring mental well-being in diverse populations and projects. J. Epidemiol. Community Health 2011, 65, A38–A39. [Google Scholar] [CrossRef]
- Taggart, F.; Friede, T.; Weich, S.; Clarke, A.; Johnson, M.; Stewart-Brown, S. Cross cultural evaluation of the Warwick-Edinburgh mental well-being scale (WEMWBS) -a mixed methods study. Health Qual. Life Outcomes 2013, 11, 27. [Google Scholar] [CrossRef] [PubMed]
- Dong, A.; Zhang, X.; Zhou, H.; Chen, S.; Zhao, W.; Wu, M.; Guo, J.; Guo, W. Applicability and cross-cultural validation of the Chinese version of the Warwick-Edinburgh mental well-being scale in patients with chronic heart failure. Health Qual. Life Outcomes 2019, 17, 55. [Google Scholar] [CrossRef] [PubMed]
- Soldevila-Domenech, N.; Forero, C.G.; Alayo, I.; Capella, J.; Colom, J.; Malmusi, D.; Mompart, A.; Mortier, P.; Puértolas, B.; Sánchez, N.; et al. Mental well-being of the general population: Direct and indirect effects of socioeconomic, relational and health factors. Qual. Life Res. 2021, 30, 2171–2185. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Partial, conditional, and moderated mediation: Quantification, inference, and interpretation. Commun. Monogr. 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Galen, L. Atheism, wellbeing, and the wager: Why not believing in God (with others) is good for you. Sci. Relig. Cult. 2015, 2, 54–69. [Google Scholar] [CrossRef]
- Abdullah, W.J. Religious Representation in Secular Singapore: A Case Study of MUIS and Parga’s. Asian Surv. 2013, 53, 1182–1204. [Google Scholar] [CrossRef]
- Hvidt, N.C.; Hvidtjørn, D.; Christensen, K.; Nielsen, J.B.; Søndergaard, J. Faith Moves Mountains—Mountains Move Faith: Two Opposite Epidemiological Forces in Research on Religion and Health. J. Relig. Health 2017, 56, 294–304. [Google Scholar] [CrossRef]
- Ang, D. MHA COS 2021: Integrity, Secularism and Protections under the Law; Ministry of Home Affairs: Singapore, 2021.
- Krause, N.M. Aging in the Church How Social Relationships Affect Health; Templeton Foundation Press: West Conshohocken, PA, USA, 2008. [Google Scholar]
- Shor, E.; Roelfs, D.J. The Longevity Effects of Religious and Nonreligious Participation: A Meta-Analysis and Meta-Regression. J. Sci. Study Relig. 2013, 52, 120–145. [Google Scholar] [CrossRef]
- Pedersen, H.F.; Birkeland, M.H.; Jensen, J.S.; Schnell, T.; Hvidt, N.C.; Sørensen, T.; la Cour, P. What brings meaning to life in a highly secular society? A study on sources of meaning among Danes. Scand. J. Psychol. 2018, 59, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Bentzen, J.S. In crisis, we pray: Religiosity and the COVID-19 pandemic. J. Econ. Behav. Organ. 2021, 192, 541–583. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.; Putnam, R.D. Religion, Social Networks, and Life Satisfaction. Am. Sociol. Rev. 2010, 75, 914–933. [Google Scholar] [CrossRef]
- Masters, K.S. Intrinsic Religiousness (Religiosity). In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1117–1118. [Google Scholar]
- Steffen, P.R.; Masters, K.S.; Baldwin, S. What Mediates the Relationship between Religious Service Attendance and Aspects of Well-Being? J. Relig. Health 2017, 56, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Arrowood, R.B.; Cox, C.R.; Weinstock, M.; Hoffman, J. Intrinsic religiosity protects believers from the existential fear of a human Jesus. Ment. Health Relig. Cult. 2018, 21, 534–545. [Google Scholar] [CrossRef]
- Schwalm, F.D.; Zandavalli, R.B.; de Castro Filho, E.D.; Lucchetti, G. Is there a relationship between spirituality/religiosity and resilience? A systematic review and meta-analysis of observational studies. J. Health Psychol. 2022, 27, 1218–1232. [Google Scholar] [CrossRef]
| Religion | Number of Participants |
|---|---|
| Christian | 39 (21.1%) |
| Buddhist | 38 (20.5%) |
| Hindu | 11 (5.9%) |
| Catholic | 9 (4.9%) |
| Muslim | 8 (4.3%) |
| Other Religions | 14 (7.6%) |
| Agnostic | 8 (4.3%) |
| No Religion | 24 (13.0%) |
| Freethinkers | 16 (8.6%) |
| Atheist | 3 (1.6%) |
| Unspecified | 15 (8.1%) |
| Variables | M(SD) | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| - | - | |||
| 2.77(0.994) | 0.432 ** | - | ||
| 45.0(9.67) | 0.049 | 0.181 * | - | |
| 2.04(1.51) | 0.084 | 0.035 | 0.068 | - |
| Variables | M(SD) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 2.77 (0.994) | - | ||||
| 3.02 (0.785) | 0.070 | - | |||
| 5.12 (1.02) | 0.185 * | 0.219 ** | - | ||
| 45.0 (9.67) | 0.181 * | 0.510 ** | 0.376 ** | - | |
| 2.04 (1.51) | 0.035 | 0.055 | 0.030 | 0.068 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gan, S.K.-E.; Wong, S.W.-Y.; Jiao, P.-D. Religiosity, Theism, Perceived Social Support, Resilience, and Well-Being of University Undergraduate Students in Singapore during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 3620. https://doi.org/10.3390/ijerph20043620
Gan SK-E, Wong SW-Y, Jiao P-D. Religiosity, Theism, Perceived Social Support, Resilience, and Well-Being of University Undergraduate Students in Singapore during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(4):3620. https://doi.org/10.3390/ijerph20043620
Chicago/Turabian StyleGan, Samuel Ken-En, Sibyl Weang-Yi Wong, and Peng-De Jiao. 2023. "Religiosity, Theism, Perceived Social Support, Resilience, and Well-Being of University Undergraduate Students in Singapore during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 4: 3620. https://doi.org/10.3390/ijerph20043620
APA StyleGan, S. K.-E., Wong, S. W.-Y., & Jiao, P.-D. (2023). Religiosity, Theism, Perceived Social Support, Resilience, and Well-Being of University Undergraduate Students in Singapore during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 20(4), 3620. https://doi.org/10.3390/ijerph20043620







