Association between the Cognitive-Related Behavioral Assessment Severity Stage and Activities of Daily Living Required for Discharge to Home in Patients with Stroke: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
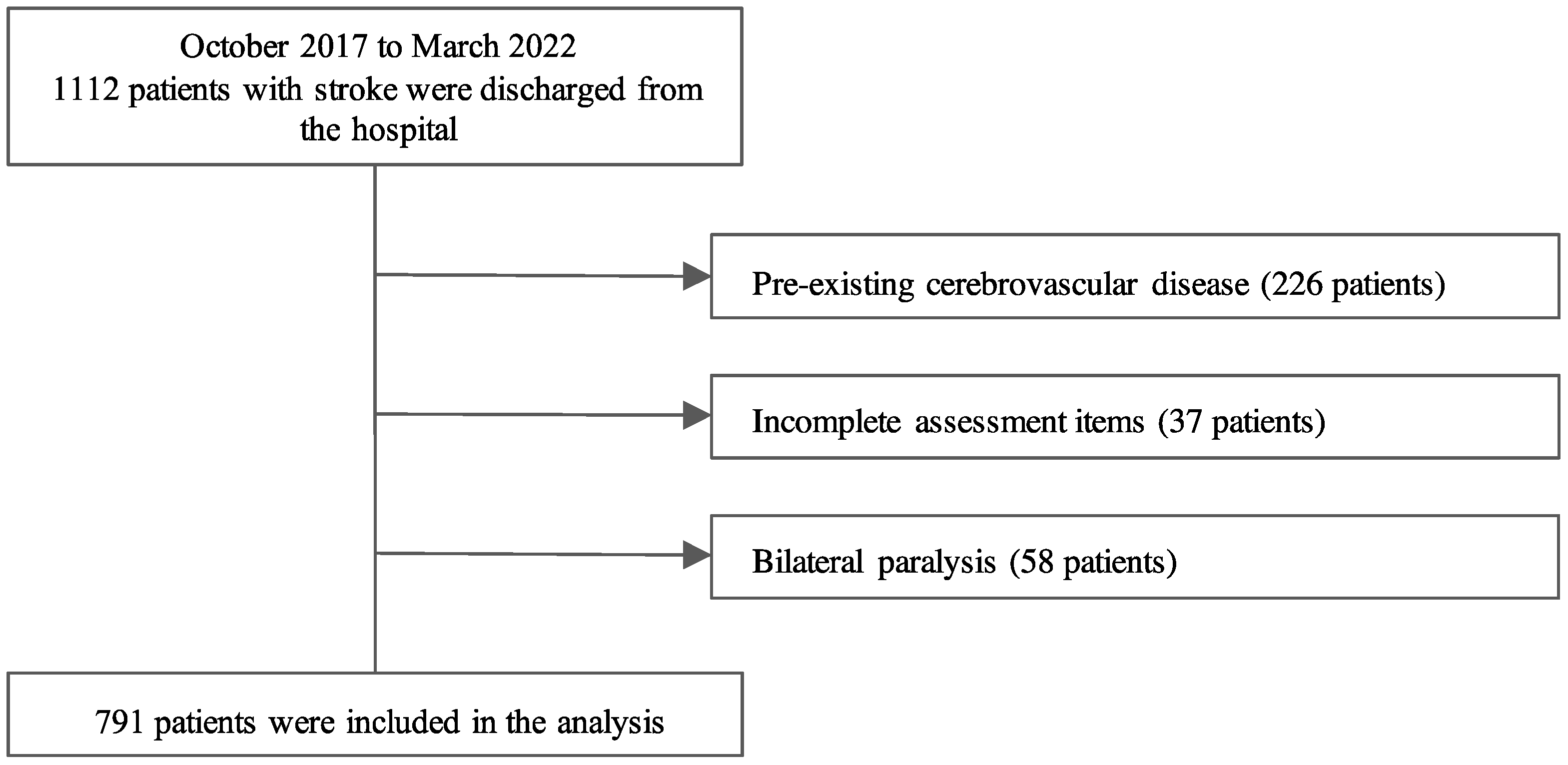
2.2. Study Design and Patients
2.3. Measurement Items
2.3.1. Patient Attributes
2.3.2. Cognitive-Related Behavioral Assessment (Table A1)
2.3.3. Functional Independence Measure
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
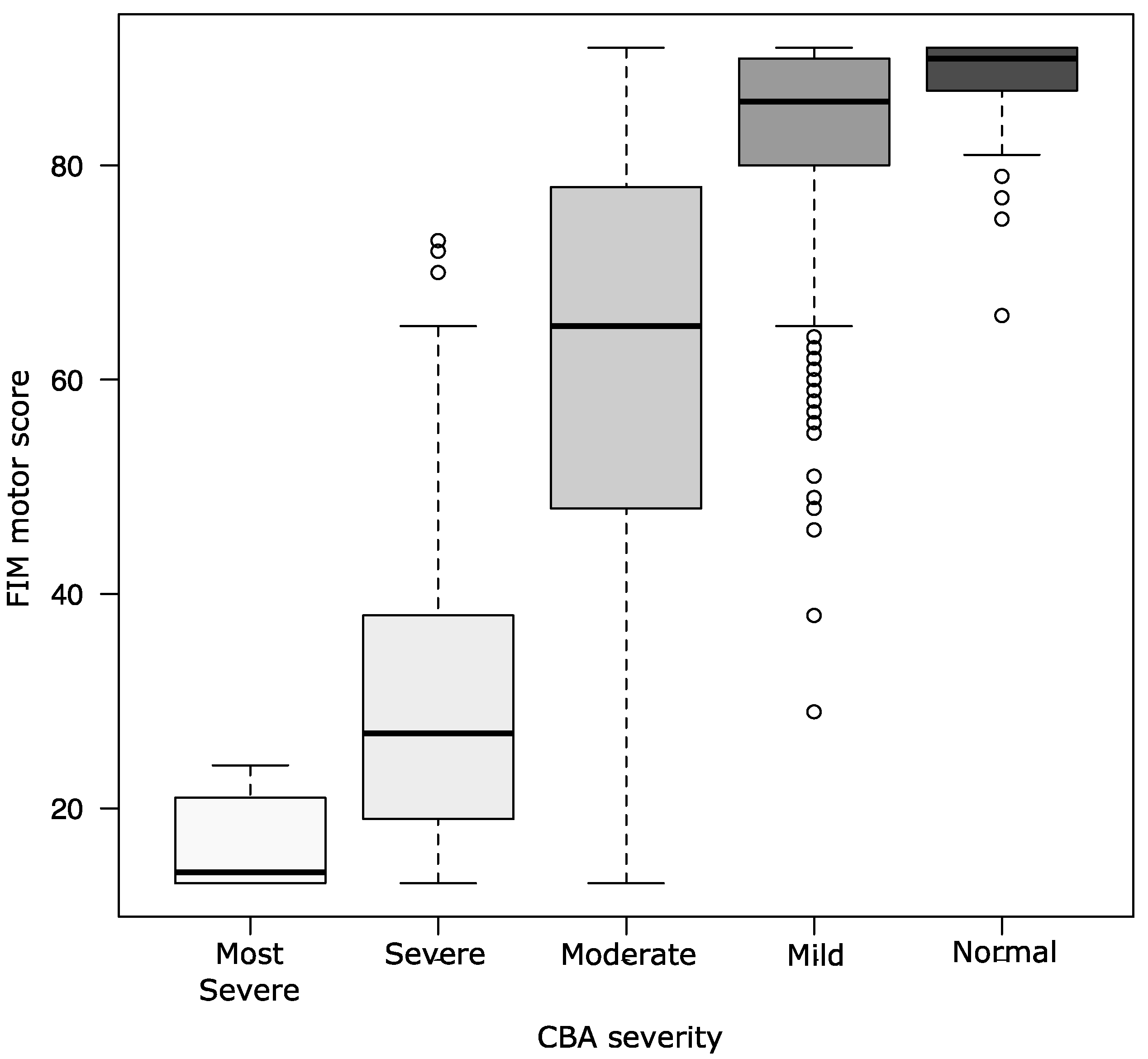
3.2. ADL Independence and Severity Levels of Cognitive Function Assessed by the CBA
3.3. Relationships between CBA Severity and Independence in Walking or ADLs Affecting Discharge to Home
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Area | Point of View | Severity | Definition | |
|---|---|---|---|---|
| Consciousness | 1. Eye-opening, awareness 2. Response to stimuli 3. Ease of thinking fatigue | 5 | Normal | Stable condition with a normal, energetic rhythm of life. Does not show fatigue or decreased responsiveness to thinking or speaking and has sufficient energy to sustain it. |
| 4 | Mild | Eyes are open during the day, but sometimes vision is blurred. He/she does not show fatigue in familiar situations but shows decreased responsiveness in novel situations. | ||
| 3 | Moderate | Eyes are open during the day, but facial expression is often blurred. Easily fatigued by thinking or speaking and shows a marked decrease in responsiveness during the process. | ||
| 2 | Severe | Tendency of occasional somnolence during the day. Fatigued easily when he/she thinks or talks and cannot sustain mental energy. | ||
| 1 | Most Severe | Tendency to be somnolent in the absence of daytime stimulation. | ||
| Emotion | 1. Initiative 2. Sorrow and pleasure 3. Emotional control | 5 | Normal | Willing and eager to try new activities. Shows age-appropriate emotional expression and is able to control his/her emotions according to the situation. |
| 4 | Mild | Performs habitual activities on his/her own but is unwilling to try new activities. Alternatively, he/she may show a mild tendency toward fixation, impulsivity, anger, depression, dependence, and regression. | ||
| 3 | Moderate | May require instruction or prompting to perform daily activities. Alternatively, the tendency to fixation, impulsivity, irritability, depression, dependence, or regression is observed. | ||
| 2 | Severe | May not initiate daily activities on his/her own and may not do so even when encouraged to do so. Alternatively, shows strong symptoms of fixation, impulsivity, irritability, depression, dependence, and regression. | ||
| 1 | Most Severe | Lacks the motivation to do anything and, therefore, requires assistance with personal care. Additionally, rarely able to express his/her feelings of joy, anger, or sadness, or only expresses his/her reactions of pleasure or displeasure. | ||
| Attention | 1. Attention selection 2. Sustained attention distribution and control | 5 | Normal | Able to perform two or more tasks simultaneously with no apparent performance decrement. Can respond appropriately to the presentation of other stimuli during the task and can return to the original task spontaneously. |
| 4 | Mild | Has a slight performance deficit when performing two tasks at the same time. Alternatively, he/she tends to hyperconcentrate and does not respond immediately to other stimuli. May require prompting to return to the original task. | ||
| 3 | Moderate | Tends to become more distracted the more interferences they receive. Complete a task to the end or sustain it for about 30 min, but his/her reaction time slows down, and errors increase during the process. | ||
| 2 | Severe | Unable to direct attention to the required object when other interfering stimuli are present. Alternatively, interrupts one task too soon and is unable to sustain it. | ||
| 1 | Most Severe | Hardly able to pay attention to the necessary stimuli. | ||
| Memory | 1. Ability to remember things in daily life 2. Scheduled memory | 5 | Normal | Generally accurate in recalling events from 2 to 3 days ago. A new recall of events from several weeks ago is generally possible. Forgetting appointments and commitments is rare and not a problem. |
| 4 | Mild | The patient is generally accurate in recalling events of the day but is uncertain about details of events 2 or 3 days prior. Alternatively, the patient occasionally forgets plans or appointments and makes mistakes. | ||
| 3 | Moderate | Able to recall some of the events of the day accurately and is ambiguous about details, such as incorrect person, place, or time. Alternatively, the patient often forgets appointments and commitments. | ||
| 2 | Severe | Has little or no recall of the events of the day. Or, the patient is completely unable to remember appointments and commitments and requires constant prompting. | ||
| 1 | Most Severe | Has little or no recall of events that occurred several hours ago. Often makes up stories and has obvious memory confusion. | ||
| Judgment | 1. Decision-making and problem-solving skills that take into account long-term impacts | 5 | Normal | Able to make decisions and solve problems taking into account long-term projection and social relationships several years later. |
| 4 | Mild | Able to make decisions with some degree of foresight into the near future but admits a tendency toward egocentricity or dependence on others. | ||
| 3 | Moderate | Has a scene-dependent or short-sighted (immediate benefit first) problem-solving approach. | ||
| 2 | Severe | Often relies on immediate emotional problem-solving. | ||
| 1 | Most Severe | Often engages in object-dependent problem-solving. | ||
| Consciousness of disease | 1. Understanding of diseases, disabilities, and abilities 2. Understanding of seriousness and utilization of surviving capacity 3. Environmental adaptation | 5 | Normal | Well aware of his/her illnesses, disabilities, and abilities, and can effectively use his/her remaining abilities and adapts to changes in the environment with his/her ingenuity. |
| 4 | Mild | Generally aware of his/her illness, disability, abilities, and seriousness of the illness. However, compared to the pre-symptomatic state, the patient has a clearly reduced range of social activities and is unable to fully use his/her remaining abilities. | ||
| 3 | Moderate | Has a general awareness of his/her illness, disability, and abilities, but it is not serious. Therefore, the patient is adaptable only in a well-organized environment. | ||
| 2 | Severe | Has only a rough perception of his/her disease or disability but not of abilities. Therefore, even in a well-developed environment, the patient requires the efforts of the people around him/her. | ||
| 1 | Most Severe | Completely unaware of his/her disease, disability, and abilities. Unable to use his/her residual abilities and is unable to adapt to the environment without the full support of those around him/her. | ||
References
- Appelros, P.; Karlsson, G.M.; Seiger, A.; Nydevik, I. Prognosis for Patients with Neglect and Anosognosia with Special Reference to Cognitive Impairment. J. Rehabil. Med. 2003, 35, 254–258. [Google Scholar] [CrossRef]
- Douiri, A.; Rudd, A.G.; Wolfe, C.D.A. Prevalence of Poststroke Cognitive Impairment: South London Stroke Register 1995–2010. Stroke 2013, 44, 138–145. [Google Scholar] [CrossRef]
- Jackson, D.; Thornton, H.; Turner-Stokes, L. Can Young Severely Disabled Stroke Patients Regain the Ability to Walk Independently More Than Three Months Post Stroke? Clin. Rehabil. 2000, 14, 538–547. [Google Scholar] [CrossRef]
- Paolucci, S.; Bragoni, M.; Coiro, P.; De Angelis, D.; Fusco, F.R.; Morelli, D.; Venturiero, V.; Pratesi, L. Quantification of the Probability of Reaching Mobility Independence at Discharge from a Rehabilitation Hospital in Nonwalking Early Ischemic Stroke Patients: A Multivariate Study. Cerebrovasc. Dis. 2008, 26, 16–22. [Google Scholar] [CrossRef]
- Öneş, K.; Yalçinkaya, E.Y.; Toklu, B.C.; Çağlar, N. Effects of Age, Gender, and Cognitive, Functional and Motor Status on Functional Outcomes of Stroke Rehabilitation. NeuroRehabilitation 2009, 25, 241–249. [Google Scholar] [CrossRef]
- Preston, E.; Ada, L.; Stanton, R.; Mahendran, N.; Dean, C.M. Prediction of Independent Walking in People Who Are Nonambulatory Early after Stroke: A Systematic Review. Stroke 2021, 52, 3217–3224. [Google Scholar] [CrossRef]
- Xu, T.; Clemson, L.; O’Loughlin, K.; Lannin, N.A.; Dean, C.; Koh, G. Risk Factors for Falls in Community Stroke Survivors: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2018, 99, 563–573.e5. [Google Scholar] [CrossRef]
- Lanctôt, K.L.; Lindsay, M.P.; Smith, E.E.; Sahlas, D.J.; Foley, N.; Gubitz, G.; Austin, M.; Ball, K.; Bhogal, S.; Blake, T.; et al. Canadian Stroke Best Practice Recommendations: Mood, Cognition and Fatigue Following Stroke, 6th Edition Update 2019. Int. J. Stroke 2020, 15, 668–688. [Google Scholar] [CrossRef]
- Stroke Guideline Committee of the Japan Stroke Society. Japanese Guidelines for the Management of Stroke 2021; Kyowa Kikaku: Tokyo, Japan, 2021. (In Japanese) [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-Mental State’. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Raven, J.; Court, J. Raven’s Colored Progressive Matrices; Pearson: Oxford, UK, 1995. [Google Scholar]
- Wilson, B.; Cockburn, J.; Halligan, P. Development of a Behavioral Test of Visuospatial Neglect. Arch. Phys. Med. Rehabil. 1987, 68, 98–102. [Google Scholar]
- Lassonde, M.; Sauerwein, H.C.; Gallagher, A.; Thériault, M.; Lepore, F. Neuropsychology: Traditional and New Methods of Investigation. Epilepsia. 2006, 47 (Suppl. S2), 9–13. [Google Scholar] [CrossRef]
- Jennett, B.; Snoek, J.; Bond, M.R.; Brooks, N. Disability after Severe Head Injury: Observations on the Use of the Glasgow Outcome Scale. J. Neurol. Neurosurg. Psychiatry. 1981, 44, 285–293. [Google Scholar] [CrossRef]
- Seniów, J.; Litwin, M.; Leśniak, M. The Relationship between Non-linguistic Cognitive Deficits and Language Recovery in Patients with Aphasia. J. Neurol. Sci. 2009, 283, 91–94. [Google Scholar] [CrossRef]
- Manchester, D.; Priestley, N.; Jackson, H. The Assessment of Executive Functions: Coming out of the Office. Brain Inj. 2004, 18, 1067–1081. [Google Scholar] [CrossRef]
- Azouvi, P.; Samuel, C.; Louis-Dreyfus, A.; Bernati, T.; Bartolomeo, P.; Beis, J.M.; Chokron, S.; Leclercq, M.; Marchal, F.; Martin, Y.; et al. Sensitivity of Clinical and Behavioural Tests of Spatial Neglect after Right Hemisphere Stroke. J. Neurol. Neurosurg. Psychiatry. 2002, 73, 160–166. [Google Scholar] [CrossRef]
- Whyte, J.; Hart, T.; Bode, R.K.; Malec, J.F. The Moss Attention Rating Scale for Traumatic Brain Injury: Initial Psychometric Assessment. Arch. Phys. Med. Rehabil. 2003, 84, 268–276. [Google Scholar] [CrossRef]
- Gillen, G. A Fork in the Road: An Occupational Hazard? Am. J. Occup. Ther. 2013, 67, 641–652. [Google Scholar] [CrossRef]
- Morita, A.; Ishikawa, M.; Kanai, K.; Makizako, H. Development of Cognitive-Related Behavioral Assessment for Neuropsychological Disorder by Observation. Gen. Rehabil. 2014, 42, 877–884. (In Japanese) [Google Scholar] [CrossRef]
- Tategami, S. Rusk Institute of Rehabilitation Medicine, Brain Injury Day Treatment Program; Igaku-Syoin Ltd.: Tokyo, Japan, 2010. (In Japanese) [Google Scholar]
- Yamadori, S. Introduction to Neuropsychology; Igaku-Syoin Ltd.: Tokyo, Japan, 1985. (In Japanese) [Google Scholar]
- Hishikawa, N.; Makizako, H.; Morita, A. Inter-rater Reliability of Cognitive-Related Behavioral Assessment in Subacute Stroke Patients. J. Aichi Phys. Ther. Soc. 2017, 29, 69–75. (In Japanese) [Google Scholar]
- Morita, A. Cognitive-Related Behavioral Assessment, Understanding Higher Brain Dysfunction from Daily Living; Miwa-Shoten Ltd.: Tokyo, Japan, 2016. (In Japanese) [Google Scholar]
- Mokler, P.J.; Sandstrom, R.; Griffin, M.; Farris, L.; Jones, C. Predicting Discharge Destination for Patients with Severe Motor Stroke: Important Functional Tasks. Neurorehabil. Neural Repair. 2000, 14, 181–185. [Google Scholar] [CrossRef]
- Data Management Service of the Uniform Data System for Medical Rehabilitation and the Center for Functional Assessment Research. Guide for Use of the Uniform Data Set for Medical Rehabilitation (Ver.3.0); State University of New York at Buffalo: New York, NY, USA, 1990.
- Meijer, R.; Ihnenfeldt, D.S.; van Limbeek, J.; Vermeulen, M.; de Haan, R.J. Prognostic Factors in the Subacute Phase after Stroke for the Future Residence after Six Months to One Year. A Systematic Review of the Literature. Clin. Rehabil. 2003, 17, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Hyndman, D.; Pickering, R.M.; Ashburn, A. The Influence of Attention Deficits on Functional Recovery Post Stroke During the First 12 Months after Discharge from Hospital. J. Neurol. Neurosurg. Psychiatry 2008, 79, 656–663. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Ohji, S.; Ishiyama, D.; Nishio, N.; Otobe, Y.; Suzuki, M.; Ogawa, H.; Ichikawa, T.; Taguchi, R.; Shino, S.; et al. Factors Associated with Functional Recovery in Japanese Patients with Convalescent Stroke Stratified by Age: A Multicenter Observational Study. Int. J. Rehabil. Res. 2019, 42, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Ullberg, T.; Zia, E.; Petersson, J.; Norrving, B. Changes in Functional Outcome over the First Year after Stroke: An Observational Study from the Swedish Stroke Register. Stroke 2015, 46, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Leśniak, M.; Bak, T.; Czepiel, W.; Seniów, J.; Członkowska, A. Frequency and Prognostic Value of Cognitive Disorders in Stroke Patients. Dement. Geriatr. Cogn. Disord. 2008, 26, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Jokinen, H.; Melkas, S.; Ylikoski, R.; Pohjasvaara, T.; Kaste, M.; Erkinjuntti, T.; Hietanen, M. Post-stroke Cognitive Impairment Is Common Even after Successful Clinical Recovery. Eur. J. Neurol. 2015, 22, 1288–1294. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Tyagi, S.; Hoenig, H.; Lee, K.E.; Venketasubramanian, N.; Menon, E.; De Silva, D.A.; Yap, P.; Tan, B.Y.; Young, S.H.; et al. Burden of Informal Care in Stroke Survivors and Its Determinants: A Prospective Observational Study in an Asian Setting. BMC Public Health. 2021, 21, 1945. [Google Scholar] [CrossRef] [PubMed]
- Achilike, S.; Beauchamp, J.E.S.; Cron, S.G.; Okpala, M.; Payen, S.S.; Baldridge, L.; Okpala, N.; Montiel, T.C.; Varughese, T.; Love, M.; et al. Caregiver Burden and Associated Factors among Informal Caregivers of Stroke Survivors. J. Neurosci. Nurs. 2020, 52, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, P.; Wu, S.; Yuan, R.; Liu, J.; Tao, W.; Wang, D.; Liu, M. Impaired Consciousness at Stroke Onset in Large Hemisphere Infarction: Incidence, Risk Factors and Outcome. Sci. Rep. 2020, 10, 13170. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Galvin, R.; Horgan, N.F. Fall-Related Experiences of Stroke Survivors: A Meta-ethnography. Disabil. Rehabil. 2017, 39, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Koyama, T.; Matsumoto, K.; Okuno, T.; Domen, K. Relationships between Independence Level of Single Motor-Fim Items and Fim-Motor Scores in Patients with Hemiplegia after Stroke: An Ordinal Logistic Modelling Study. J. Rehabil. Med. 2006, 38, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Stolwyk, R.J.; Mihaljcic, T.; Wong, D.K.; Chapman, J.E.; Rogers, J.M. Poststroke Cognitive Impairment Negatively Impacts Activity and Participation Outcomes: A Systematic Review and Meta-analysis. Stroke 2021, 52, 748–760. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Kabe, N.; Takano, A.; Isobe, K. Use of the Berg Balance Scale to Predict Independent Gait after Stroke: A Study of an Inpatient Population in Japan. PMR 2015, 7, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Garrett, M.; Gronley, J.K.; Mulroy, S.J. Classification of Walking Handicap in the Stroke Population. Stroke 1995, 26, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Douiri, A.; Grace, J.; Sarker, S.J.; Tilling, K.; McKevitt, C.; Wolfe, C.D.; Rudd, A.G. Patient-Specific Prediction of Functional Recovery after Stroke. Int. J. Stroke 2017, 12, 539–548. [Google Scholar] [CrossRef]
| n = 791 | |
|---|---|
| Age (years) | 73.00 [61.00, 81.00] |
| Sex, female/male | 331/460 |
| Type of stroke, cerebral infarction/cerebral hemorrhage/subarachnoid hemorrhage | 448/284/59 |
| Hemisphere of stroke, left/right/other * | 378/346/67 |
| Days between stroke onset and admission | 24.00 [17.00, 32.00] |
| Days between stroke onset and discharge | 118.00 [80.00, 153.00] |
| Days of admission | 94.00 [57.00, 125.00] |
| Brunnstrom Recovery Stage, n (%) | |
| Stage I | 8 (1.0) |
| Stage II | 54 (6.8) |
| Stage III | 87 (11.0) |
| Stage IV | 55 (7.0) |
| Stage V | 84 (10.6) |
| Stage VI | 294 (37.2) |
| None | 209 (26.4) |
| Cognitive-related Behavioral Assessment total score | 24.00 [20.00, 27.00] |
| Cognitive-related Behavioral Assessment severity, n (%) | |
| Most severe | 12 (1.5) |
| Severe | 84 (10.6) |
| Moderate | 231 (29.2) |
| Mild | 357 (45.1) |
| Normal | 107 (13.5) |
| Functional Independence Measure motor score | 81.00 [58.00, 89.00] |
| Functional Independence Measure cognitive score | 30.00 [22.00, 34.00] |
| Functional Independence Measure total score | 111.00 [83.00, 122.00] |
| Home discharge, n (%) | 567 (71.7) |
| Most Severe (n = 12) | Severe (n = 84) | Moderate (n = 231) | Mild (n = 357) | Normal (n = 107) | |
|---|---|---|---|---|---|
| Age (years) | 83.00 [75.25, 88.00] | 80.00 [74.00, 85.25] | 77.00 [68.00, 83.50] | 70.00 [58.00, 78.00] | 60.00 [50.00, 74.50] |
| Sex, female/male | 7/5 | 41/43 | 89/142 | 151/206 | 43/64 |
| Type of stroke, cerebral infarction/cerebral hemorrhage/subarachnoid hemorrhage | 7/4/1 | 52/27/5 | 131/84/16 | 194/131/32 | 64/38/5 |
| Hemisphere of stroke, left/right/other * | 9/3/0 | 39/38/7 | 111/102/18 | 170/153/34 | 49/50/8 |
| Days since stroke onset | 150.50 [137.50, 159.25] | 150.00 [125.75, 168.00] | 134.00 [103.00, 165.00] | 107.00 [77.00, 140.00] | 74.00 [52.50, 118.00] |
| Brunnstrom Recovery Stage, n (%) | |||||
| Stage I | 0 (0.0) | 2 (2.4) | 2 (0.9) | 3 (0.8) | 1 (0.9) |
| Stage II | 7 (58.3) | 22 (26.2) | 21 (9.1) | 4 (1.1) | 0 (0.0) |
| Stage III | 1 (8.3) | 14 (16.7) | 37 (16.0) | 31 (8.7) | 4 (3.7) |
| Stage IV | 2 (16.7) | 7 (8.3) | 16 (6.9) | 24 (6.7) | 6 (5.6) |
| Stage V | 2 (16.7) | 12 (14.3) | 27 (11.7) | 34 (9.5) | 9 (8.4) |
| Stage VI | 0 (0.0) | 15 (17.9) | 80 (34.6) | 153 (42.9) | 46 (43.0) |
| None | 0 (0.0) | 12 (14.3) | 48 (20.8) | 108 (30.3) | 41 (38.3) |
| Cognitive-related Behavioral Assessment total score | 9.00 [8.50, 9.00] | 14.00 [13.00, 15.00] | 20.00 [19.00, 21.00] | 26.00 [24.00, 27.00] | 30.00 [29.00, 30.00] |
| Cognitive-related Behavioral Assessment subitem score | |||||
| Consciousness | 2.00 [2.00, 2.00] | 3.00 [3.00, 4.00] | 4.00 [4.00, 4.00] | 5.00 [4.00, 5.00] | 5.00 [5.00, 5.00] |
| Emotion | 2.00 [1.00, 2.00] | 3.00 [2.75, 3.00] | 4.00 [3.00, 4.00] | 5.00 [4.00, 5.00] | 5.00 [5.00, 5.00] |
| Attention | 2.00 [1.00, 2.00] | 2.00 [2.00, 3.00] | 3.00 [3.00, 3.00] | 4.00 [4.00, 4.00] | 5.00 [4.50, 5.00] |
| Memory | 1.00 [1.00, 1.00] | 2.00 [2.00, 2.00] | 3.00 [3.00, 4.00] | 4.00 [4.00, 5.00] | 5.00 [5.00, 5.00] |
| Judgment | 1.00 [1.00, 1.00] | 2.00 [2.00, 2.00] | 3.00 [3.00, 3.00] | 4.00 [4.00, 4.00] | 5.00 [5.00, 5.00] |
| Consciousness of disease | 1.00 [1.00, 1.00] | 2.00 [1.00, 2.00] | 3.00 [3.00, 3.00] | 4.00 [4.00, 4.00] | 5.00 [5.00, 5.00] |
| Functional Independence Measure motor score | 14.00 [13.00, 20.00] | 27.00 [19.00, 38.00] | 65.00 [48.00, 78.00] | 86.00 [80.00, 90.00] | 90.00 [87.00, 91.00] |
| Functional Independence Measure cognitive score | 6.50 [5.00, 8.75] | 13.00 [10.00, 15.00] | 24.00 [19.50, 27.00] | 32.00 [30.00, 34.00] | 35.00 [35.00, 35.00] |
| Functional Independence Measure total score | 21.00 [19.00, 29.25] | 42.00 [30.00, 51.50] | 86.00 [70.50, 103.50] | 117.00 [110.00, 123.00] | 124.00 [122.00, 126.00] |
| Home discharge, n (%) | 1 (8.3) | 16 (19.0) | 131 (56.7) | 316 (88.5) | 103 (96.3) |
| Most Severe (n = 12) | Severe (n = 84) | Moderate (n = 231) | Mild (n = 357) | Normal (n = 107) | |
|---|---|---|---|---|---|
| Self-care | |||||
| Eating, n (%) | 0 (0.0) | 12 (14.3) | 163 (70.6) | 341 (95.5) | 106 (99.1) |
| Grooming, n (%) | 0 (0.0) | 2 (2.4) | 81 (35.1) | 322 (90.2) | 106 (99.1) |
| Bathing, n (%) | 0 (0.0) | 0 (0.0) | 19 (8.2) | 189 (52.9) | 90 (84.1) |
| Dress Up, n (%) | 0 (0.0) | 0 (0.0) | 81 (35.1) | 325 (91.0) | 107 (100.0) |
| Dress Low, n (%) | 0 (0.0) | 0 (0.0) | 80 (34.6) | 325 (91.0) | 106 (99.1) |
| Toileting, n (%) | 0 (0.0) | 2 (2.4) | 87 (37.7) | 327 (91.6) | 106 (99.1) |
| Sphincter control | |||||
| Bladder, n (%) | 0 (0.0) | 4 (4.8) | 104 (45.0) | 324 (90.8) | 107 (100.0) |
| Bowel, n (%) | 0 (0.0) | 4 (4.8) | 97 (42.0) | 317 (88.8) | 102 (95.3) |
| Transfers | |||||
| Bed Trans, n (%) | 0 (0.0) | 1 (1.2) | 86 (37.2) | 323 (90.5) | 107 (100.0) |
| Toilet Trans, n (%) | 0 (0.0) | 2 (2.4) | 82 (35.5) | 322 (90.2) | 106 (99.1) |
| Tub Trans, n (%) | 0 (0.0) | 0 (0.0) | 19 (8.2) | 170 (47.6) | 88 (82.2) |
| Locomotion | |||||
| Walking, n (%) | 0 (0.0) | 0 (0.0) | 62 (26.8) | 301 (84.3) | 104 (97.2) |
| Stair climbing, n (%) | 0 (0.0) | 2 (2.4) | 49 (21.2) | 236 (66.1) | 97 (90.7) |
| Dependent Variable (FIM Score 6–7) | Independent Variable | FIM Score 6–7, Percentage Applicable | Adjusted Model * | |
|---|---|---|---|---|
| OR (95% CI) # | p-Value | |||
| Dress Up | CBA severity (mild or normal) | 432/464 (93.1%) | 21.90 (13.50–35.70) | <0.01 |
| Bladder | 431/464 (92.9%) | 11.60 (7.21–18.60) | <0.01 | |
| Bed Trans | 430/464 (92.7%) | 18.30 (11.40–29.40) | <0.01 | |
| Toilet Trans | 428/464 (92.2%) | 18.30 (11.40–29.30) | <0.01 | |
| Walking | 405/464 (87.3%) | 16.60 (10.60–26.10) | <0.01 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maki, Y.; Morita, A.; Makizako, H. Association between the Cognitive-Related Behavioral Assessment Severity Stage and Activities of Daily Living Required for Discharge to Home in Patients with Stroke: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 3005. https://doi.org/10.3390/ijerph20043005
Maki Y, Morita A, Makizako H. Association between the Cognitive-Related Behavioral Assessment Severity Stage and Activities of Daily Living Required for Discharge to Home in Patients with Stroke: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(4):3005. https://doi.org/10.3390/ijerph20043005
Chicago/Turabian StyleMaki, Yoshiaki, Akiko Morita, and Hyuma Makizako. 2023. "Association between the Cognitive-Related Behavioral Assessment Severity Stage and Activities of Daily Living Required for Discharge to Home in Patients with Stroke: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 4: 3005. https://doi.org/10.3390/ijerph20043005
APA StyleMaki, Y., Morita, A., & Makizako, H. (2023). Association between the Cognitive-Related Behavioral Assessment Severity Stage and Activities of Daily Living Required for Discharge to Home in Patients with Stroke: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(4), 3005. https://doi.org/10.3390/ijerph20043005







