Healthy Aging at Family Mealtimes: Associations of Clean Cooking, Protein Intake, and Dining Together with Mental Health of Chinese Older Adults amid COVID-19 Pandemic
Abstract
1. Introduction
2. Literature Review
2.1. Multifaceted Diet and Healthy Aging
2.2. Rural and Urban Disparities
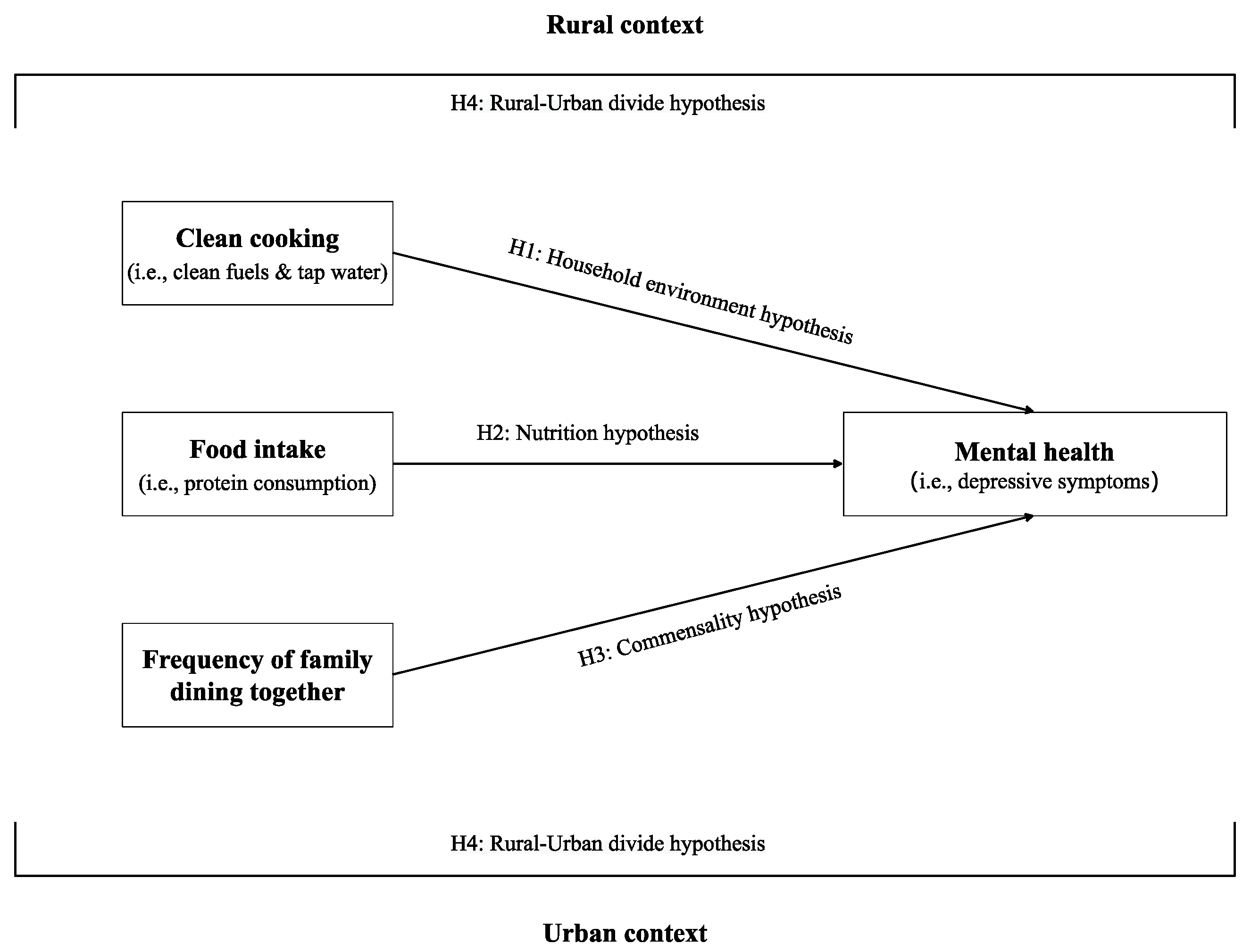
2.3. The Present Study
3. Materials and Methods
3.1. Data
3.2. Measurements
3.3. Data Analysis
4. Results
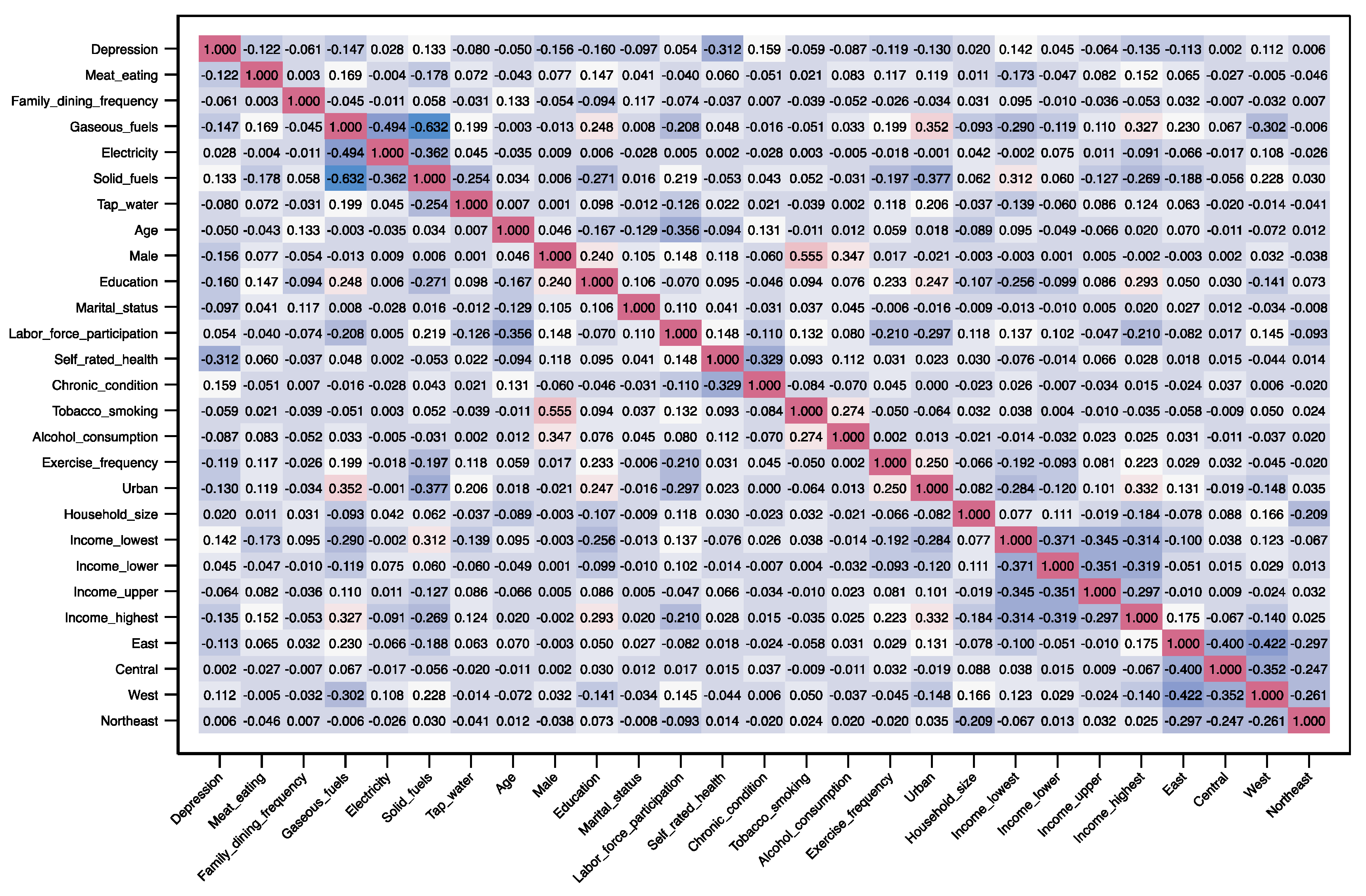
4.1. Descriptive Analysis
4.2. Regression Analysis
4.3. Supplementary Analysis
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- World Health Organization. Depression and other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/depression-global-health-estimates (accessed on 22 November 2022).
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A Systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, B.; Hülür, G. Well-Being and loneliness in Swiss older adults during the COVID-19 pandemic: The role of social relationships. The Gerontologist 2021, 61, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Veronese, N.; Thompson, T.; Kahl, K.G.; Fernandes, B.S.; Prina, A.M.; Solmi, M.; Schofield, P.; Koyanagi, A.; Tseng, P.-T.; et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2017, 36, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.; Thomas, A.J. Depression and dementia: Cause, consequence or coincidence? Maturitas 2014, 79, 184–190. [Google Scholar] [CrossRef]
- Walker, E.R.; McGee, R.E.; Druss, B.G. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 2015, 72, 334–341. [Google Scholar] [CrossRef]
- Fuller, H.R.; Huseth-Zosel, A. Lessons in resilience: Initial coping among older adults during the COVID-19 pandemic. The Gerontologist 2021, 61, 114–125. [Google Scholar] [CrossRef]
- Ang, S. Changing relationships between social contact, social support, and depressive symptoms during the COVID-19 pandemic. J. Gerontol. Ser. B 2022, 77, gbac063. [Google Scholar] [CrossRef]
- Ray, I.; Smith, K.R. Towards safe drinking water and clean cooking for all. Lancet Glob. Health 2021, 9, e361–e365. [Google Scholar] [CrossRef]
- Leck, H.; Conway, D.; Bradshaw, M.; Rees, J. Tracing the water–energy–food nexus: Description, theory and practice. Geogr. Compass 2015, 9, 445–460. [Google Scholar] [CrossRef]
- Firth, J.; Gangwisch, J.E.; Borsini, A.; Wootton, R.E.; Mayer, E.A. Food and mood: How do diet and nutrition affect mental wellbeing? BMJ 2020, 369, m2382. [Google Scholar] [CrossRef]
- Laborde, D.; Martin, W.; Swinnen, J.; Vos, R. COVID-19 risks to global food security. Science 2020, 369, 500–502. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Action Framework for Developing and Implementing Public Food Procurement and Service Policies for a Healthy Diet; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-001834-1. Available online: https://www.who.int/publications/i/item/9789240018341 (accessed on 22 November 2022).
- Moon, J.H.; Huh, J.S.; Won, C.W.; Kim, H.J. Living and eating alone on depressive symptoms by physical frailty status: A cross-sectional study based on the Korean Frailty and Aging Cohort Study. Arch. Gerontol. Geriatr. 2022, 98, 104570. [Google Scholar] [CrossRef] [PubMed]
- Ohara, Y.; Motokawa, K.; Watanabe, Y.; Shirobe, M.; Inagaki, H.; Motohashi, Y.; Edahiro, A.; Hirano, H.; Kitamura, A.; Awata, S.; et al. Association of eating alone with oral frailty among community-dwelling older adults in Japan. Arch. Gerontol. Geriatr. 2020, 87, 104014. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, R.J. Psychological correlates of habitual diet in healthy adults. Psychol. Bull. 2017, 143, 53–90. [Google Scholar] [CrossRef] [PubMed]
- Katz, D.L.; Meller, S. Can we say what diet is best for health? Annu. Rev. Public Health 2014, 35, 83–103. [Google Scholar] [CrossRef]
- Alkerwi, A. Diet quality concept. Nutrition 2014, 30, 613–618. [Google Scholar] [CrossRef]
- Biggs, E.M.; Bruce, E.; Boruff, B.; Duncan, J.M.A.; Horsley, J.; Pauli, N.; McNeill, K.; Neef, A.; Van Ogtrop, F.; Curnow, J.; et al. Sustainable development and the water–energy–food nexus: A perspective on livelihoods. Environ. Sci. Policy 2015, 54, 389–397. [Google Scholar] [CrossRef]
- Rosenthal, J.; Balakrishnan, K.; Bruce, N.; Chambers, D.; Graham, J.; Jack, D.; Kline, L.; Masera, O.; Mehta, S.; Mercado, I.R.; et al. Implementation science to accelerate clean cooking for public health. Environ. Health Perspect. 2017, 125, A3–A7. [Google Scholar] [CrossRef]
- Stoner, O.; Lewis, J.; Martínez, I.L.; Gumy, S.; Economou, T.; Adair-Rohani, H. Household cooking fuel estimates at global and country level for 1990 to 2030. Nat. Commun. 2021, 12, 5793. [Google Scholar] [CrossRef]
- Smith, L.; Veronese, N.; López Sánchez, G.F.; Butler, L.; Barnett, Y.; Shin, J.I.; Lee, S.; Oh, J.W.; Soysal, P.; Pizzol, D.; et al. The association of cooking fuels with depression and anxiety symptoms among adults aged ≥65 years from low- and middle-income countries. J. Affect. Disord. 2022, 311, 494–499. [Google Scholar] [CrossRef]
- Liu, P.; Han, C.; Teng, M. Does clean cooking energy improve mental health? Evidence from China. Energy Policy 2022, 166, 113011. [Google Scholar] [CrossRef]
- Ao, C.-K.; Dong, Y.; Kuo, P.-F. Industrialization, indoor and ambient air quality, and elderly mental health. China Econ. Rev. 2021, 69, 101676. [Google Scholar] [CrossRef]
- Hadley, C.; Wutich, A. Experience-Based measures of food and water security: Biocultural approaches to grounded measures of insecurity. Hum. Organ. 2009, 68, 451–460. [Google Scholar] [CrossRef]
- Smith, J.P.; Tian, M.; Zhao, Y. Community effects on elderly health: Evidence from CHARLS national baseline. J. Econ. Ageing 2013, 1–2, 50–59. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, Z. Industrial water pollution, water environment treatment, and health risks in China. Environ. Pollut. 2016, 218, 358–365. [Google Scholar] [CrossRef]
- Simiyu, S.; Bagayoko, M.; Gyasi, R.M. Associations between water, sanitation, and depression among older people in Ghana: Empirical evidence from WHO-SAGE wave 2 survey. Aging Ment. Health 2022, 26, 1112–1119. [Google Scholar] [CrossRef]
- Cockerham, W.C. Health lifestyle theory and the convergence of agency and structure. J. Health Soc. Behav. 2005, 46, 51–67. [Google Scholar] [CrossRef]
- de Ridder, D.; Kroese, F.; Evers, C.; Adriaanse, M.; Gillebaart, M. Healthy diet: Health impact, prevalence, correlates, and interventions. Psychol. Health 2017, 32, 907–941. [Google Scholar] [CrossRef]
- Katsas, K.; Mamalaki, E.; Kontogianni, M.D.; Anastasiou, C.A.; Kosmidis, M.H.; Varlamis, I.; Hadjigeorgiou, G.M.; Dardiotis, E.; Sakka, P.; Scarmeas, N.; et al. Malnutrition in older adults: Correlations with social, diet-related, and neuropsychological factors. Nutrition 2020, 71, 110640. [Google Scholar] [CrossRef]
- Bartali, B.; Frongillo, E.A.; Bandinelli, S.; Lauretani, F.; Semba, R.D.; Fried, L.P.; Ferrucci, L. Low nutrient intake is an essential component of frailty in older persons. J. Gerontol. Ser. A 2006, 61, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Júnior, H.J.; Rodrigues, B.; Uchida, M.; Marzetti, E. Low protein intake is associated with frailty in older adults: A systematic review and meta-analysis of observational studies. Nutrients 2018, 10, 1334. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, C.; Li, S.; Zhang, D. Association between dietary protein intake and the risk of depressive symptoms in adults. Br. J. Nutr. 2020, 123, 1290–1301. [Google Scholar] [CrossRef]
- Fischler, C. Commensality, society and culture. Soc. Sci. Inf. 2011, 50, 528–548. [Google Scholar] [CrossRef]
- Nyberg, M.; Olsson, V.; Ortman, G.; Pajalic, Z.; Andersson, H.S.; Blucher, A.; Lindborg, A.-L.; Wendin, K.; Westergren, A. The meal as a performance: Food and meal practices beyond health and nutrition. Ageing Soc. 2018, 38, 83–107. [Google Scholar] [CrossRef]
- Björnwall, A.; Mattsson Sydner, Y.; Koochek, A.; Neuman, N. Eating alone or together among community-living older people—A scoping review. Int. J. Environ. Res. Public. Health 2021, 18, 3495. [Google Scholar] [CrossRef]
- Kuroda, A.; Tanaka, T.; Hirano, H.; Ohara, Y.; Kikutani, T.; Furuya, H.; Obuchi, S.P.; Kawai, H.; Ishii, S.; Akishita, M.; et al. Eating alone as social disengagement is strongly associated with depressive symptoms in Japanese community-dwelling older adults. J. Am. Med. Dir. Assoc. 2015, 16, 578–585. [Google Scholar] [CrossRef]
- Yates, L.; Warde, A. Eating together and eating alone: Meal arrangements in British households. Br. J. Sociol. 2017, 68, 97–118. [Google Scholar] [CrossRef]
- Wang, X.; Shen, W.; Wang, C.; Zhang, X.; Xiao, Y.; He, F.; Zhai, Y.; Li, F.; Shang, X.; Lin, J. Association between eating alone and depressive symptom in elders: A cross-sectional study. BMC Geriatr. 2016, 16, 19. [Google Scholar] [CrossRef]
- Zorbas, C.; Palermo, C.; Chung, A.; Iguacel, I.; Peeters, A.; Bennett, R.; Backholer, K. Factors perceived to influence healthy eating: A systematic review and meta-ethnographic synthesis of the literature. Nutr. Rev. 2018, 76, 861–874. [Google Scholar] [CrossRef]
- Nazri, N.S.; Vanoh, D.; Leng, S.K. Malnutrition, low diet quality and its risk factors among older adults with low socio-economic status: A scoping review. Nutr. Res. Rev. 2021, 34, 107–116. [Google Scholar] [CrossRef]
- Yue, A.; Shi, Y.; Luo, R.; Zhang, L.; Johnson, N.; Rozelle, S.; Zhao, Q. The impact of investment on drinking water quality in rural China. China Agric. Econ. Rev. 2017, 9, 255–269. [Google Scholar] [CrossRef]
- Xie, Y.; Hu, J. An introduction to the China Family Panel Studies (CFPS). Chin. Sociol. Rev. 2014, 47, 3–29. [Google Scholar] [CrossRef]
- Xie, Y.; Lu, P. The sampling design of the China Family Panel Studies (CFPS). Chin. J. Sociol. 2015, 1, 471–484. [Google Scholar] [CrossRef] [PubMed]
- Kong, S.T.; Wu, Q. Chinese family and society dynamics using the China Family Panel Studies (CFPS) household panel. Aust. Econ. Rev. 2019, 52, 127–133. [Google Scholar] [CrossRef]
- Xie, Y.; Zhang, X.; Tu, P.; Ren, Q.; Sun, Y.; Lyu, P.; Ding, H.; Hu, J.; Wu, Q. China Family Panel Studies: User Manual, 3rd ed.; Institute of Social Science Survey of Peking University: Beijing, China, 2017; Available online: https://www.isss.pku.edu.cn/cfps/docs/20210511113545661703.pdf (accessed on 2 January 2023).
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Missinne, S.; Vandeviver, C.; Van de Velde, S.; Bracke, P. Measurement equivalence of the CES-D 8 depression-scale among the ageing population in eleven European countries. Soc. Sci. Res. 2014, 46, 38–47. [Google Scholar] [CrossRef]
- Gao, R.; Liang, L.; Yue, J.; Song, Q.; Zhao, X.; Fei, J.; Hu, Y.; Lv, J.; Yuan, T.; Guo, X.; et al. The relationship between Chinese adults’ self-assessments of family social status in childhood and depression: A moderated mediation model. J. Affect. Disord. 2023, 320, 284–290. [Google Scholar] [CrossRef]
- Briggs, R.; Carey, D.; O’Halloran, A.M.; Kenny, R.A.; Kennelly, S.P. Validation of the 8-Item Centre for Epidemiological Studies Depression Scale in a cohort of community-dwelling older people: Data from The Irish Longitudinal Study on Ageing (TILDA). Eur. Geriatr. Med. 2018, 9, 121–126. [Google Scholar] [CrossRef]
- Xu, T.; Zhu, G.; Han, S. Study of depression influencing factors with zero-inflated regression models in a large-scale population survey. BMJ Open 2017, 7, e016471. [Google Scholar] [CrossRef]
- Patel, V.; Burns, J.K.; Dhingra, M.; Tarver, L.; Kohrt, B.A.; Lund, C. Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry 2018, 17, 76–89. [Google Scholar] [CrossRef]
- Lawrence, S.D.; Plisco, M.K. Family mealtimes and family functioning. Am. J. Fam. Ther. 2017, 45, 195–205. [Google Scholar] [CrossRef]
- Wutich, A.; Brewis, A.; Tsai, A. Water and mental health. WIREs Water 2020, 7, e1461. [Google Scholar] [CrossRef]
- Febian, F.I.; Syed Annuar, S.N.; Memon, M.A. Functional food consumption among older consumers in Malaysia: A Health belief model perspective. Br. Food J. 2021, 123, 2880–2892. [Google Scholar] [CrossRef]
- van der Zanden, L.D.T.; van Kleef, E.; de Wijk, R.A.; van Trijp, H.C.M. Knowledge, perceptions and preferences of elderly regarding protein-enriched functional food. Appetite 2014, 80, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Grunert, K.G. Satisfaction with food-related life and beliefs about food health, safety, freshness and taste among the elderly in China: A segmentation analysis. Food Qual. Prefer. 2020, 79, 103775. [Google Scholar] [CrossRef]
- Szakos, D.; Ózsvári, L.; Kasza, G. Perception of older adults about health-related functionality of foods compared with other age groups. Sustainability 2020, 12, 2748. [Google Scholar] [CrossRef]
| Group | Variable | Total Sample (N = 7858) | Rural Residents (N = 4088) | Urban Residents (N = 3770) | |||
|---|---|---|---|---|---|---|---|
| Mean/% | SD | Mean/% | SD | Mean/% | SD | ||
| Mental health | Depressive symptoms | 5.44 | 4.35 | 6.03 | 4.56 | 4.99 | 4.13 |
| Diet characteristics | Protein intake | ||||||
| No-meat | 17.4% | 22.4% | 13.6% | ||||
| Meat-eating | 82.6% | 77.6% | 86.4% | ||||
| Frequency of family dining together | 6.13 | 2.04 | 6.19 | 2.04 | 6.08 | 2.03 | |
| Cooking fuels | |||||||
| Gaseous fuels | 48.9% | 31.3% | 62.4% | ||||
| Electricity | 24.7% | 26.0% | 23.6% | ||||
| Solid fuels | 26.5% | 42.8% | 13.9% | ||||
| Cooking water | |||||||
| Non-tap water | 26.4% | 35.7% | 19.3% | ||||
| Tap water | 73.6% | 64.3% | 80.7% | ||||
| Demographics | Age, years | 60.76 | 8.04 | 61.00 | 7.88 | 60.57 | 8.15 |
| Sex | |||||||
| Female | 49.1% | 48.6% | 49.5% | ||||
| Male | 50.9% | 51.4% | 50.5% | ||||
| Education, years | 6.96 | 4.38 | 5.80 | 4.11 | 7.85 | 4.38 | |
| Marital status | |||||||
| Unpartnered | 8.37% | 7.72% | 8.87% | ||||
| Married or cohabited | 91.6% | 92.3% | 91.1% | ||||
| Labor force participation | |||||||
| Not working | 32.8% | 20.1% | 42.5% | ||||
| Working | 67.2% | 79.9% | 57.5% | ||||
| Physical health | Self-rated health | 2.80 | 1.25 | 2.76 | 1.31 | 2.83 | 1.21 |
| Chronic condition | |||||||
| No | 77.6% | 77.0% | 78.1% | ||||
| Yes | 22.4% | 23.0% | 21.9% | ||||
| Healthy lifestyle | Tobacco smoking | ||||||
| No | 72.6% | 69.7% | 74.9% | ||||
| Yes | 27.4% | 30.3% | 25.1% | ||||
| Alcohol consumption | |||||||
| No | 82.3% | 82.2% | 82.5% | ||||
| Yes | 17.7% | 17.8% | 17.5% | ||||
| Exercise frequency | 1.78 | 2.63 | 1.09 | 2.21 | 2.31 | 2.79 | |
| Family context | Area of residence | ||||||
| Rural | 43.5% | - | - | ||||
| Urban | 56.5% | - | - | ||||
| Household size | 3.83 | 1.88 | 3.96 | 2.00 | 3.72 | 1.78 | |
| Net family income per capita | |||||||
| Lowest 25% | 24.0% | 37.7% | 13.4% | ||||
| Lower 25% | 26.0% | 32.2% | 21.2% | ||||
| Upper 25% | 26.6% | 20.9% | 31.0% | ||||
| Highest 25% | 23.5% | 9.22% | 34.4% | ||||
| Geographic location | |||||||
| East | 36.9% | 37.6% | 36.3% | ||||
| Central | 26.4% | 26.9% | 26.1% | ||||
| West | 22.7% | 25.2% | 20.7% | ||||
| Northeast | 14.0% | 10.3% | 16.9% | ||||
| Group | Variable | Crude Model | Adjusted Model | ||
|---|---|---|---|---|---|
| High-Risk | Zero-Inflation | High-Risk | Zero-Inflation | ||
| Diet characteristics | Protein intake | ||||
| No-meat (ref.) | |||||
| Meat-eating | 0.84 *** | 0.93 | 0.89 *** | 0.82 | |
| (0.02) | (0.20) | (0.03) | (0.18) | ||
| Frequency of family dining together | 0.97 *** | 1.07 | 0.98 *** | 1.05 | |
| (0.01) | (0.06) | (0.01) | (0.05) | ||
| Cooking fuels | |||||
| Gaseous fuels | 0.85 *** | 1.83 * | 0.98 | 1.39 | |
| (0.03) | (0.51) | (0.04) | (0.43) | ||
| Electricity | 0.99 | 1.52 | 1.04 | 1.32 | |
| (0.03) | (0.41) | (0.03) | (0.36) | ||
| Solid fuels (ref.) | |||||
| Cooking water | |||||
| Non-tap water (ref.) | |||||
| Tap water | 0.88 *** | 1.24 | 0.92 ** | 1.16 | |
| (0.03) | (0.27) | (0.03) | (0.24) | ||
| Demographics | Age | 0.99 *** | 1.01 | ||
| (0.00) | (0.01) | ||||
| Sex | |||||
| Female (ref.) | |||||
| Male | 0.88 *** | 1.79 ** | |||
| (0.03) | (0.36) | ||||
| Education | 0.99 * | 1.02 | |||
| (0.00) | (0.02) | ||||
| Marital status | |||||
| Unpartnered (ref.) | |||||
| Married or cohabited | 0.85 *** | 1.46 | |||
| (0.03) | (0.54) | ||||
| Labor force participation | |||||
| Not working (ref.) | |||||
| Working | 1.05 | 0.64 * | |||
| (0.03) | (0.12) | ||||
| Physical health | Self-rated health | 0.86 *** | 1.55 *** | ||
| (0.01) | (0.11) | ||||
| Chronic condition | |||||
| No (ref.) | |||||
| Yes | 1.09 ** | 0.62 * | |||
| (0.03) | (0.14) | ||||
| Healthy lifestyle | Tobacco smoking | ||||
| No (ref.) | |||||
| Yes | 1.05 | 1.04 | |||
| (0.03) | (0.20) | ||||
| Alcohol consumption | |||||
| No (ref.) | |||||
| Yes | 0.97 | 1.08 | |||
| (0.03) | (0.23) | ||||
| Exercise frequency | 0.99 | 1.08 * | |||
| (0.00) | (0.04) | ||||
| Family context | Area of residence | ||||
| Rural (ref.) | |||||
| Urban | 0.95 | 0.93 | |||
| (0.04) | (0.19) | ||||
| Household size | 0.99 | 1.04 | |||
| (0.01) | (0.05) | ||||
| Net family income per capita | |||||
| Lowest 25% (ref.) | |||||
| Lower 25% | 0.96 | 1.34 | |||
| (0.03) | (0.29) | ||||
| Upper 25% | 0.88 *** | 1.07 | |||
| (0.03) | (0.28) | ||||
| Highest 25% | 0.82 *** | 1.18 | |||
| (0.04) | (0.34) | ||||
| Geographic location | |||||
| East | 0.94 | 1.14 | |||
| (0.04) | (0.28) | ||||
| Central (ref.) | |||||
| West | 1.04 | 0.86 | |||
| (0.04) | (0.27) | ||||
| Northeast | 0.96 | 0.82 | |||
| (0.04) | (0.29) | ||||
| Diet Characteristics | Rural Residents (N = 4088) | Urban Residents (N = 3770) | ||
|---|---|---|---|---|
| High-Risk | Zero-Inflation | High-Risk | Zero-Inflation | |
| Protein intake | ||||
| No-meat (ref.) | ||||
| Meat-eating | 0.95 | 0.81 | 0.81 *** | 0.77 |
| (0.04) | (0.25) | (0.03) | (0.33) | |
| Frequency of family dining together | 0.97 *** | 1.04 | 0.98 * | 1.04 |
| (0.01) | (0.05) | (0.01) | (0.09) | |
| Cooking fuels | ||||
| Gaseous fuels | 0.96 | 1.50 | 1.04 | 2.76 |
| (0.04) | (0.54) | (0.07) | (2.81) | |
| Electricity | 1.04 | 1.14 | 1.09 | 3.19 |
| (0.04) | (0.35) | (0.07) | (3.40) | |
| Solid fuels (ref.) | ||||
| Cooking water | ||||
| Non-tap water (ref.) | ||||
| Tap water | 0.89 *** | 0.92 | 0.96 | 1.53 |
| (0.03) | (0.25) | (0.04) | (0.57) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, S.; Ding, X.; Leung, J.T.Y. Healthy Aging at Family Mealtimes: Associations of Clean Cooking, Protein Intake, and Dining Together with Mental Health of Chinese Older Adults amid COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 1672. https://doi.org/10.3390/ijerph20031672
Zhou S, Ding X, Leung JTY. Healthy Aging at Family Mealtimes: Associations of Clean Cooking, Protein Intake, and Dining Together with Mental Health of Chinese Older Adults amid COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(3):1672. https://doi.org/10.3390/ijerph20031672
Chicago/Turabian StyleZhou, Shuai, Xiangying Ding, and Janet Tsin Yee Leung. 2023. "Healthy Aging at Family Mealtimes: Associations of Clean Cooking, Protein Intake, and Dining Together with Mental Health of Chinese Older Adults amid COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 3: 1672. https://doi.org/10.3390/ijerph20031672
APA StyleZhou, S., Ding, X., & Leung, J. T. Y. (2023). Healthy Aging at Family Mealtimes: Associations of Clean Cooking, Protein Intake, and Dining Together with Mental Health of Chinese Older Adults amid COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 20(3), 1672. https://doi.org/10.3390/ijerph20031672








