Effect of Physical Activity/Exercise on Cardiorespiratory Fitness in Children and Adolescents with Type 1 Diabetes: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Information Sources and Searching Strategy
2.2. Inclusion Criteria
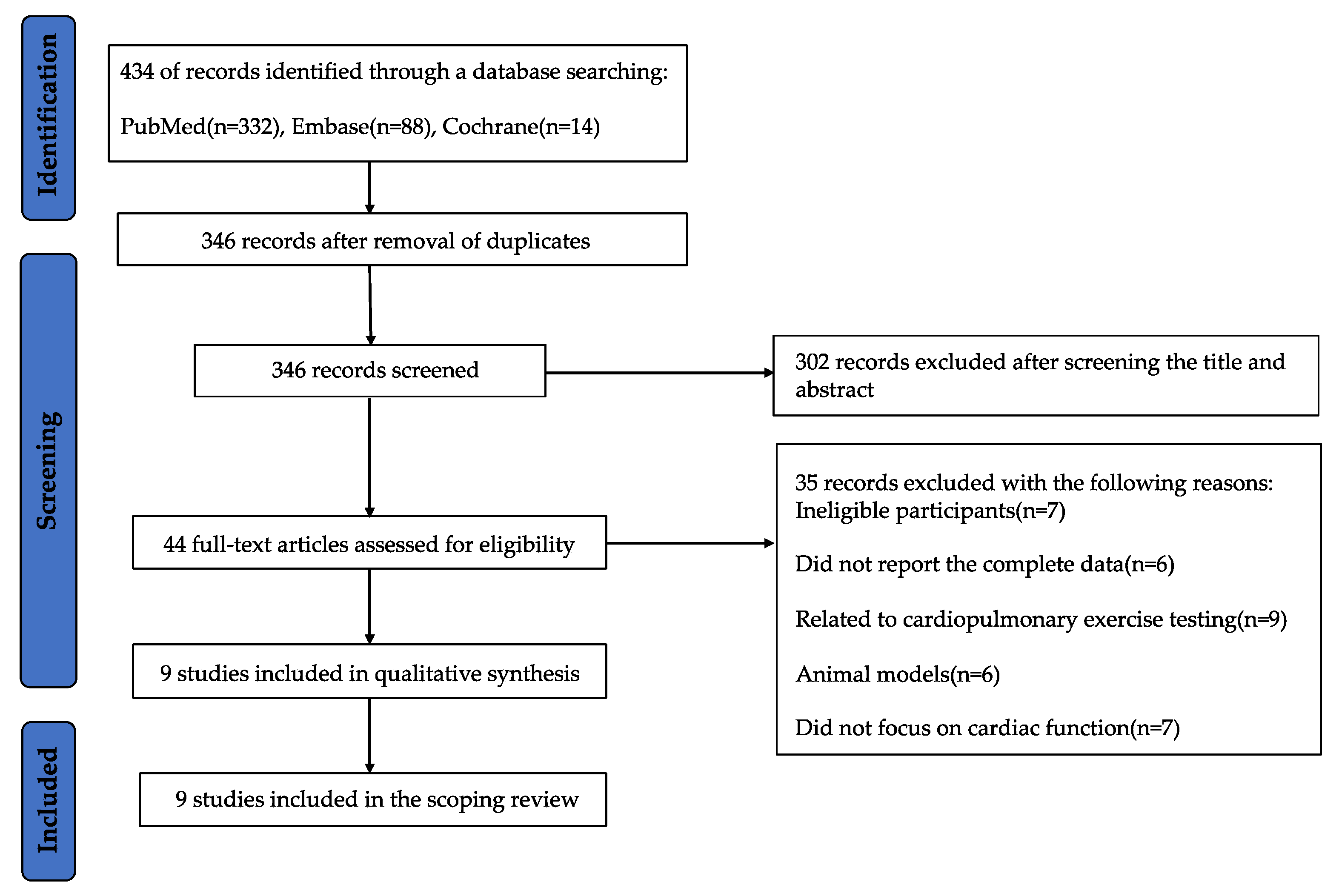
2.3. Study Selection
2.4. Data Extraction and Synthesis
3. Results
3.1. The Selection of Studies
3.2. Characteristics of the Final Included Studies
3.3. Characteristics of Study Participants
3.4. Characteristics of Exercise in the Included Studies
3.5. Pivotal Discoveries of the Included Studies Relating to Cardiac Function and Lipid Profile
3.5.1. CRF
3.5.2. Lipid Profile
3.5.3. Blood Pressure and HbA1
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aloke, C.; Egwu, C.O.; Aja, P.M.; Obasi, N.A.; Chukwu, J.; Akumadu, B.O.; Ogbu, P.N.; Achilonu, I. Current Advances in the Management of Diabetes Mellitus. Biomedicines 2022, 10, 2436. [Google Scholar] [CrossRef] [PubMed]
- Kakleas, K.; Soldatou, A.; Karachaliou, F.; Karavanaki, K.; Kostas, K.; Alexandra, S.; Feneli, K.; Kyriaki, K. Associated autoimmune diseases in children and adolescents with type 1 diabetes mellitus (T1DM). Autoimmun. Rev. 2015, 14, 781–797. [Google Scholar] [CrossRef] [PubMed]
- Sperling, M.A.; Laffel, L.M. Current Management of Glycemia in Children with Type 1 Diabetes Mellitus. N. Engl. J. Med. 2022, 386, 1155–1164. [Google Scholar] [CrossRef] [PubMed]
- Colom, C.; Rull, A.; Sanchez-Quesada, J.L.; Pérez, A. Cardiovascular Disease in Type 1 Diabetes Mellitus: Epidemiology and Management of Cardiovascular Risk. J. Clin. Med. 2021, 10, 1798. [Google Scholar] [CrossRef]
- Miculis, C.P.; de Campos, W.; Gasparotto, G.S.; Silva, M.P.; Mascarenhas, L.P.; Boguszewski, M.C. Correlation of cardiorespiratory fitness with risk factors for cardiovascular disease in children with type 1 diabetes mellitus. J. Diabetes Complicat. 2012, 26, 419–423. [Google Scholar] [CrossRef]
- Galassetti, P.; Riddell, M.C. Exercise and type 1 diabetes (T1DM). Compr. Physiol. 2013, 3, 1309–1336. [Google Scholar]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef]
- Lin, X.; Zhang, X.; Guo, J.; Roberts, C.K.; McKenzie, S.; Wu, W.C.; Liu, S.; Song, Y. Effects of Exercise Training on Cardiorespiratory Fitness and Biomarkers of Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2015, 4, e002014. [Google Scholar] [CrossRef]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical activity/exercise and diabetes: A position statement of the American diabetes association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef]
- Flores, E.B.; Reichert, T.; Farinha, J.B.; Kruel, L.F.M.; Costa, R.R. Exercise Training and Neuromuscular Parameters in Patients with Type 1 Diabetes: Systematic Review and Meta-Analysis. J. Phys. Act. Health 2021, 18, 748–756. [Google Scholar] [CrossRef]
- Hattersley, A.; Bruining, J.; Shield, J.; Njolstad, P.; Donaghue, K.; International Society for Pediatric and Adolescent Diabetes. ISPAD Clinical Practice Consensus Guidelines 2006–2007. The diagnosis and management of monogenic diabetes in children. Pediatr. Diabetes 2006, 7, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Minnebeck, K.; Vorona, E.; Zinn, S.; Gellner, R.; Hinder, J.; Brand, S.-M.; Kabar, I.; Alten, F.; Schmitz, B. Four weeks of high-intensity interval training (HIIT) improve the cardiometabolic risk profile of overweight patients with type 1 diabetes mellitus (T1DM). Eur. J. Sport Sci. 2020, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.D.; Galassetti, P. Exercise in pediatric type 1 diabetes. Pediatr. Exerc. Sci. 2014, 26, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Vazeou, A.; Papadopoulou, A.; Miha, M.; Drakatos, A.; Georgacopoulos, D. Cardiovascular impairment in children, adolescents, and young adults with type 1 diabetes mellitus (T1DM). Eur. J. Pediatr. 2008, 167, 877–884. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Sigal, R.J.; Kenny, G.P.; Wasserman, D.H.; Castaneda-Sceppa, C. Physical activity/exercise and type 2 diabetes. Diabetes Care 2004, 27, 2518–2539. [Google Scholar] [CrossRef]
- Campaigne, B.N.; Gilliam, T.B.; Spencer, M.L.; Lampman, R.M.; Schork, M.A. Effects of a physical activity program on metabolic control and cardiovascular fitness in children with insulin-dependent diabetes mellitus. Diabetes Care 1984, 7, 57–62. [Google Scholar] [CrossRef]
- Faulkner, M.S.; Michaliszyn, S.F.; Hepworth, J.T. A personalized approach to exercise promotion in adolescents with type 1 diabetes. Pediatr. Diabetes 2010, 11, 166–174. [Google Scholar] [CrossRef]
- Herbst, A.; Kordonouri, O.; Schwab, K.; Schmidt, F.; Holl, B. Impact of physical activity on cardiovascular risk factors in children with type 1 diabetes. Diabetes Care 2007, 30, 2098–2100. [Google Scholar] [CrossRef]
- Mohammed, M.H.H.; Al-Qahtani, M.H.H.; Takken, T. Effects of 12 weeks of recreational football (soccer) with caloric control on glycemia and cardiovascular health of adolescent boys with type 1 diabetes. Pediatr. Diabetes 2021, 22, 625–637. [Google Scholar] [CrossRef]
- Heyman, E.; Toutain, C.; Delamarche, P.; Berthon, P.; Briard, D.; Youssef, H.; Dekerdanet, M.; Gratas-Delamarche, A. Exercise training and cardiovascular risk factors in type 1 diabetic adolescent girls. Pediatr. Exerc. Sci. 2007, 19, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Salem, M.A.; AboElAsrar, M.A.; Elbarbary, N.S.; ElHilaly, R.A.; Refaat, Y.M. Is exercise a therapeutic tool for improvement of cardiovascular risk factors in adolescents with type 1 diabetes mellitus? A randomized controlled trial. Diabetol. Metab. Syndr. 2010, 2, 47. [Google Scholar] [CrossRef] [PubMed]
- Shin, K.O.; Moritani, T.; Woo, J.; Jang, K.S.; Bae, J.Y.; Yoo, J.; Kang, S. Exercise training improves cardiac autonomic nervous system activity in type 1 diabetic children. J. Phys. Ther. Sci. 2014, 26, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, J.; Deda, L.; Clarson, C.L.; Stein, R.I.; Cuerden, M.S.; Mahmud, F.H. Assessment of Habitual Physical Activity in Adolescents with Type 1 Diabetes. Can. J. Diabetes 2014, 38, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Michaliszyn, S.F.; Faulkner, M.S. Physical activity and sedentary behavior in adolescents with type 1 diabetes. Res. Nurs. Health 2010, 33, 441–449. [Google Scholar] [CrossRef]
- American Diabetes Association. 13. Children and Adolescents: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43 (Suppl. S1), S163–S182. [Google Scholar] [CrossRef] [PubMed]
- Moser, O.; Riddell, M.C.; Eckstein, M.L.; Adolfsson, P.; Rabasa-Lhoret, R.; van den Boom, L.; Gillard, P.; Nørgaard, K.; Oliver, N.S.; Zaharieva, D.P.; et al. ISPAD GUIDELINES Glucose management for exercise using continuous glucose monitoring (CGM) and intermittently scanned CGM (isCGM) systems in type 1 diabetes: Position statement of the European Association for the Study of Diabetes (EASD) and of the International Society for Pediatric and Adolescent Diabetes (ISPAD) endorsed by JDRF and supported by the American Diabetes Association (ADA). Pediatr. Diabetes 2020, 21, 1375–1393. [Google Scholar]
- Chaput, J.P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Katzmarzyk, P.T. 2020 WHO Guidelines on Physical Activity and Sedentary Behaviour for Children and Adolescents Aged 5–17 Years: Summary of the Evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef]
- The DCCT Research Group. Lipid and Lipoprotein Levels in Patients with IDDM Diabetes Control and Complication Trial Experience. Diabetes Care 1992, 15, 886–894. [Google Scholar] [CrossRef]
- Laaksonen, D.E.; Atalay, M.; Niskanen, L.K.; Mustonen, J.; Sen, C.K.; Lakka, T.A.; Uusitupa, M.I. Aerobic exercise and the lipid profile in type 1 diabetic men: A randomized controlled trial. Med. Sci. Sports Exerc. 2000, 32, 1541–1548. [Google Scholar] [CrossRef]
- Badhwar, S.; Chandran, D.S.; Jaryal, A.K.; Narang, R.; Patel, C.; Deepak, K.K. Differential role of central and peripheral arterial stiffness in determining brachial artery resting retrograde flow in patients with ischemic heart disease vs healthy subjects. J. Hum. Hypertens. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Vila, M.D.M.; Igual, L.; Remeseiro, B.; Elosua, R.; Ramos, R.; Valdivielso, J.M.; Martí-Lluch, R.; Marrugat, J.; Grau, M. Polyvascular Subclinical Atherosclerosis: Correlation between Ankle Brachial Index and Carotid Atherosclerosis in a Population-Based Sample. Angiology 2022, 0, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Study ID | Country | Study Design | Duration | Type, Intensity, Time, Frequency, and Grouping |
|---|---|---|---|---|
| Campaigne 1984 [17] | United States | Experimental (RCT) | 12 weeks | Type and intensity: participated in the exercise sessions (running, games, and movement to music). Time and frequency: three 30 min sessions per week Grouping: IG: participated in the exercise sessions; CG: usual care. |
| Faulkner 2010 [18] | United States | Experimental (pre–post) | 16 weeks | Type and intensity: aerobic exercises (between 60–75% peak heart rate, walking, kickboxing, dance revolution, etc.). Time and frequency: 60 min of moderate-to-vigorous physical activity (MVPA) each day for a goal of five days per week. |
| Herbst 2007 [19] | Germany | Observational (cross-sectional) | Grouping: regular physical activity (RPA) 0: none; RPA1: one–two times per week; RPA2: three times per week. | |
| Mohammed 2021 [20] | Netherlands | Experimental (RCT) | 12 weeks | Type and intensity: football program (between 79% and 84.6% peak heart rate). Time and frequency: two 90 min football exercises per week Grouping: football and diet (performed at high-intensity); football (performed at high-intensity); diet; the control group. |
| Heyman 2007 [21] | France | Experimental (RCT) | 6 months | Type and intensity: exercises that combine aerobics and strength (running, aerobic dance, step, football, basketball, volleyball, rock climbing, gymnastics, etc.). Time and frequency: supervised session of two hours and unsupervised session for one hour per week. Grouping: training group: supervised session of two hours and unsupervised session for one hour per week; exercise about aerobics and strength; non-training control; usual care. |
| Salem 2010 [22] | Egypt | Experimental (RCT) | 6 months | Type and intensity: Aerobic exercises (30 min, between 85–95% peak heart rate, e.g., cycling and treadmill). Leg extension and leg curl (30 min). Free strength and endurance exercises (10 min, e.g., bent calf knee raises, standing calf lifts, and toe curls). Flexibility exercises (5 min). Neuromuscular exercises (5 min). Warm-ups neck flexion (10 min, rotation, eversion, and foot inversion etc.). Grouping: Group A: participants did not attend the exercise program; Group B: participants joined the exercise sessions one times per week; Group C: participants attended the exercise sessions three times per week. Group B and C consisted of a balanced exercise regimen and an exercise training program (aerobic and anaerobic, different free strength and endurance, leg extension and leg curl, flexibility, and neuromuscular exercises). |
| Shin 2014 [23] | Republic of Korea | Experimental (pre–post) | 12 weeks | Type and intensity: walking program (following a warm-up exercise at 4.0 km/h for 3 min, the exercise load was increased by increasing the incline grade by 2% every 2 min, at a walking speed of 4.8 km/h) Time and frequency: three times per week |
| Mohammed 2014 [24] | Canada | Observational (cross-sectional) | Grouping: very active (jumping, skating, running, skipping, swimming, cycling, and games that require significant movement); somewhat active (shopping, walking, or engaging in light household chores); somewhat inactive (reading, sitting, playing video games, watching television, time in front of the computer, activities that are performed mostly sitting down and playing games); inactive (resting, lying down, sleeping) | |
| Michaliszyn 2010 [25] | United States | Experimental (pre–post) | 16 weeks | Type and intensity: aerobic exercises (between 60–75% peak heart rate; walking, kickboxing, dance revolution, etc.) Time and frequency: no more than 60 min per day, five days per week Grouping: sedentary (<2.0 METS); light (2.0–3.0 METs); moderate (3.0–5.99 METs); moderate vigorous (≥3.0 metabolic equivalent (MET) units); vigorous (≥6.0 METs) |
| Study ID | Grouping | Number (n) | Age (Range) | Age (Mean ± SD) | Males (n/%) |
|---|---|---|---|---|---|
| Campaigne 1984 [17] | IG | 9 | 5–11 | 9.0 ± 0.5 | N/A |
| CG | 10 | 8.5 ± 0.6 | N/A | ||
| Faulkner 2010 [18] | T1DM | 12 | 12–19 | 14.2 ± 1.4 | 9/75% |
| Herbst 2007 [19] | RPA0 | 10,392 | 3–18 | 12.7 ± 4.3 | N/A |
| RPA1 | 8607 | 12.6 ± 3.7 | N/A | ||
| RPA2 | 4252 | 13.9 ± 3.1 | N/A | ||
| Mohammed 2021 [20] | CG | 10 | 12–18 | 14.4 ± 2.0 | N/A |
| DG | 10 | 15.6 ± 1.8 | N/A | ||
| FG | 10 | 17.8 ± 0.4 | N/A | ||
| FDG | 10 | 14.5 ± 1.4 | N/A | ||
| Heyman 2007 [21] | Training Group | 9 | <18.5 | 15.9 ± 1.5 | 0/0 |
| Non-training Control | 10 | 16.3 ± 1.2 | 0/0 | ||
| Salem 2010 [22] | Group A | 48 | 12–18 | 15 ± 2.4 | N/A |
| Group B | 75 | 14.7 ± 2.2 | N/A | ||
| Group C | 73 | 14.5 ± 2.4 | N/A | ||
| Shin 2014 [23] | T1DM | 15 | 13 ± 1 | 13.0 ± 1.0 | 15/100% |
| Mohammed 2014 [24] | T1DM | 66 | 14–18 | 16.0 ± 1.3 | 35/53.03% |
| Michaliszyn 2010 [25] | T1DM | 16 | 12–17 | 14.4 ± 1.6 | 10/62.5% |
| Study ID | Peak VO2 (L/min) | Peak VO2 (mL/kg/min) | Peak VE (L/min) | Peak Heart Rate (Beats/min) | HbA1 (%) | FBG (mg/dL) |
|---|---|---|---|---|---|---|
| Campaigne 1984 [13] |  |  |  | ⊠ |  |  |
| Faulkner 2010 [14] | ⊠ | ⊠ | N/A | N/A | ⊠ | N/A |
| Herbst 2007 [15] | N/A | N/A | N/A | N/A |  | N/A |
| Mohammed 2021 [17] | N/A | N/A | N/A | N/A | ⊠ | ⊠ |
| Heyman 2007 [18] | N/A | N/A | N/A | N/A | N/A | N/A |
| Salem 2010 [19] | N/A | N/A | N/A | N/A |  | N/A |
| Shin 2014 [20] | N/A | ⊠ | N/A | N/A | ⊠ | N/A |
| Mohammed 2014 [21] | N/A | N/A | N/A | N/A |  | N/A |
| Michaliszyn 2010 [22] | N/A |  | N/A | N/A |  | N/A |
 : significant improvement; ⊠: no significant difference; N/A: not applicable; FBG: fasting blood glucose; HbA1: hemoglobin A1.
: significant improvement; ⊠: no significant difference; N/A: not applicable; FBG: fasting blood glucose; HbA1: hemoglobin A1.| Study ID | Triglycerides (mg/dL) | Apolipoprotein B:A-1 Ratio | Cholesterol (mg/dL) | LDL Cholesterol (mg/dL) | HDL Cholesterol (mg/dL) | SBP (mmHg) | DBP (mmHg) |
|---|---|---|---|---|---|---|---|
| Herbst 2007 [15] |  | N/A |  |  |  | ⊠ |  |
| Mohammed 2021 [17] | ⊠ | N/A | ⊠ | ⊠ | ⊠ | ⊠ | ⊠ |
| Heyman 2007 [18] | ⊠ |  | ⊠ | ⊠ | ⊠ | N/A | N/A |
| Salem 2010 [19] |  | N/A |  |  | ⊠ | ⊠ | ⊠ |
| Shin 2014 [20] | ⊠ | N/A |  | N/A |  |  |  |
| Mohammed 2014 [21] |  | N/A |  |  |  |  | ⊠ |
| Michaliszyn 2010 [22] |  | N/A | N/A |  |  | N/A | N/A |
 : significant improvement; ⊠: no significant difference; N/A: not applicable.
: significant improvement; ⊠: no significant difference; N/A: not applicable.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, X.; Wang, Z.; Guo, H.; Xu, Y.; Ogihara, A. Effect of Physical Activity/Exercise on Cardiorespiratory Fitness in Children and Adolescents with Type 1 Diabetes: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 1407. https://doi.org/10.3390/ijerph20021407
Chang X, Wang Z, Guo H, Xu Y, Ogihara A. Effect of Physical Activity/Exercise on Cardiorespiratory Fitness in Children and Adolescents with Type 1 Diabetes: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(2):1407. https://doi.org/10.3390/ijerph20021407
Chicago/Turabian StyleChang, Xinyi, Ziheng Wang, Hongzhi Guo, Yinghan Xu, and Atsushi Ogihara. 2023. "Effect of Physical Activity/Exercise on Cardiorespiratory Fitness in Children and Adolescents with Type 1 Diabetes: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 2: 1407. https://doi.org/10.3390/ijerph20021407
APA StyleChang, X., Wang, Z., Guo, H., Xu, Y., & Ogihara, A. (2023). Effect of Physical Activity/Exercise on Cardiorespiratory Fitness in Children and Adolescents with Type 1 Diabetes: A Scoping Review. International Journal of Environmental Research and Public Health, 20(2), 1407. https://doi.org/10.3390/ijerph20021407







