Survival Analysis and Risk Factors of Pulpectomy among Children with Severe Early Childhood Caries Treated under General Anesthesia: A Retrospective Study
Abstract
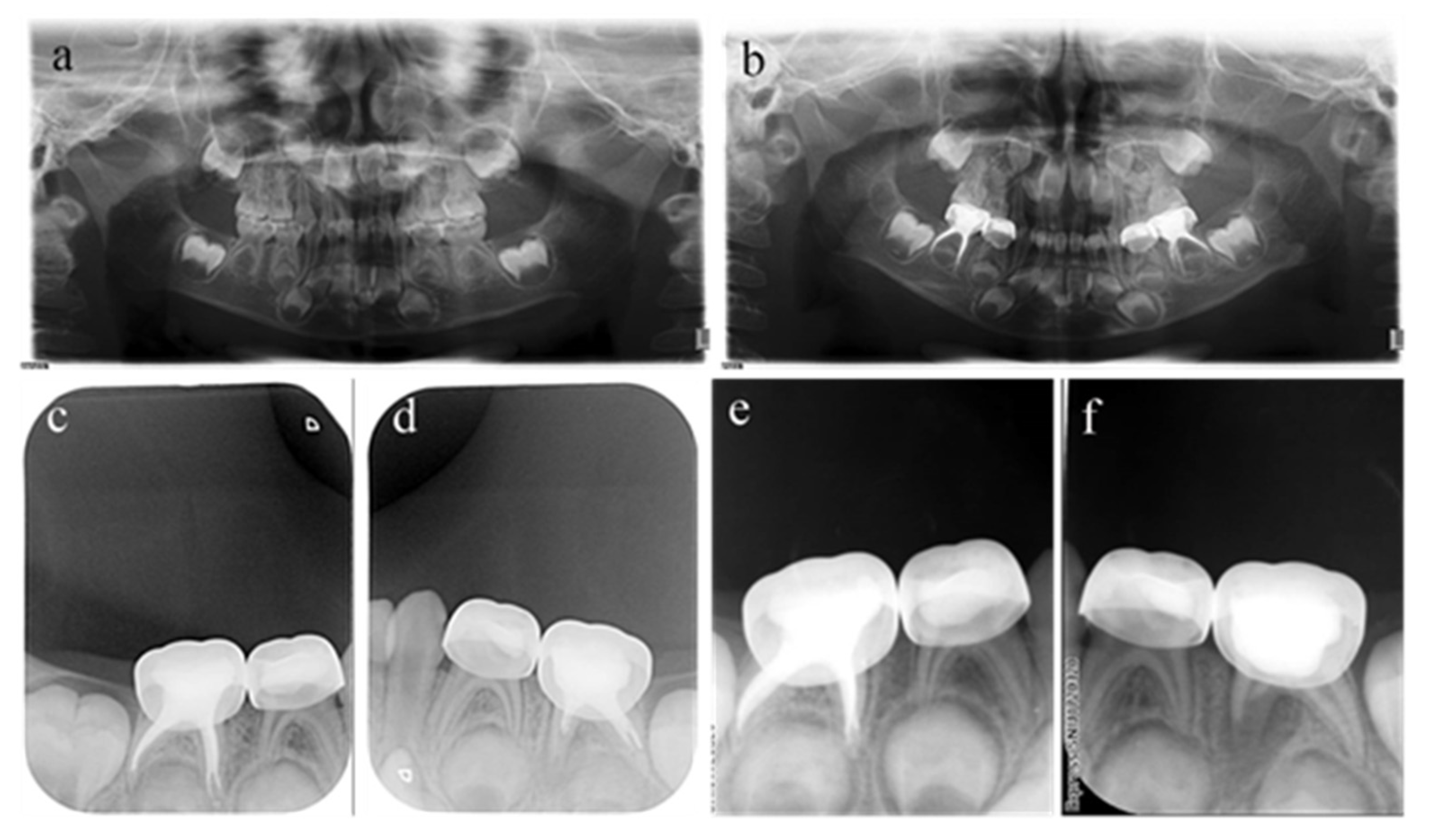
1. Introduction
2. Materials and Methods
2.1. Participants
- (1)
- Diagnosed with irreversible pulpitis, pulp necrosis, or periapical periodontitis but reserved;
- (2)
- Without internal resorption or radiolucency surrounding the tooth apex. For teeth with physiological or pathological root resorption, resorption should be limited to less than 1/3 of the root length.
- (1)
- The crown is seriously damaged and cannot be restored;
- (2)
- Root resorption involving more than 1/3 of the root length;
- (3)
- Inflammation has affected the permanent teeth;
- (4)
- Traumatic injury to the treated tooth during the observation period.
2.2. Pulpectomy Procedure
2.3. DGA Treatment Requirement
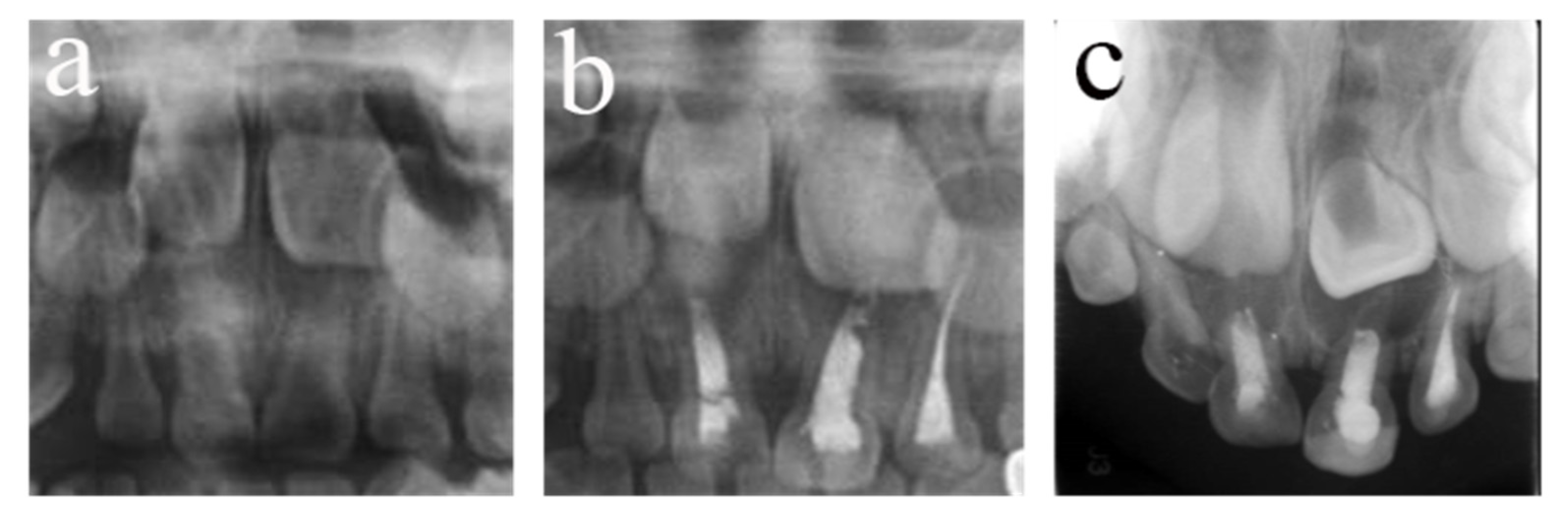
2.4. Criteria for the Outcome during the Follow-Up Examinations
- (1)
- No spontaneous pain or sensitivity to percussion;
- (2)
- The surrounding soft tissues are healthy, or the sinus tract and abscess recovered;
- (3)
- No abnormal mobility;
- (4)
- Has physical function.
- (1)
- The range of low-density shadows in the root area becomes small or disappears;
- (2)
- The bone around the permanent tooth is intact;
- (3)
- No pathological lesion presented in the successor permanent teeth;
- (4)
- No pathological root resorption is observed.
2.5. Data Extraction
2.6. Consistency Test
2.7. Statistical Analysis
3. Results
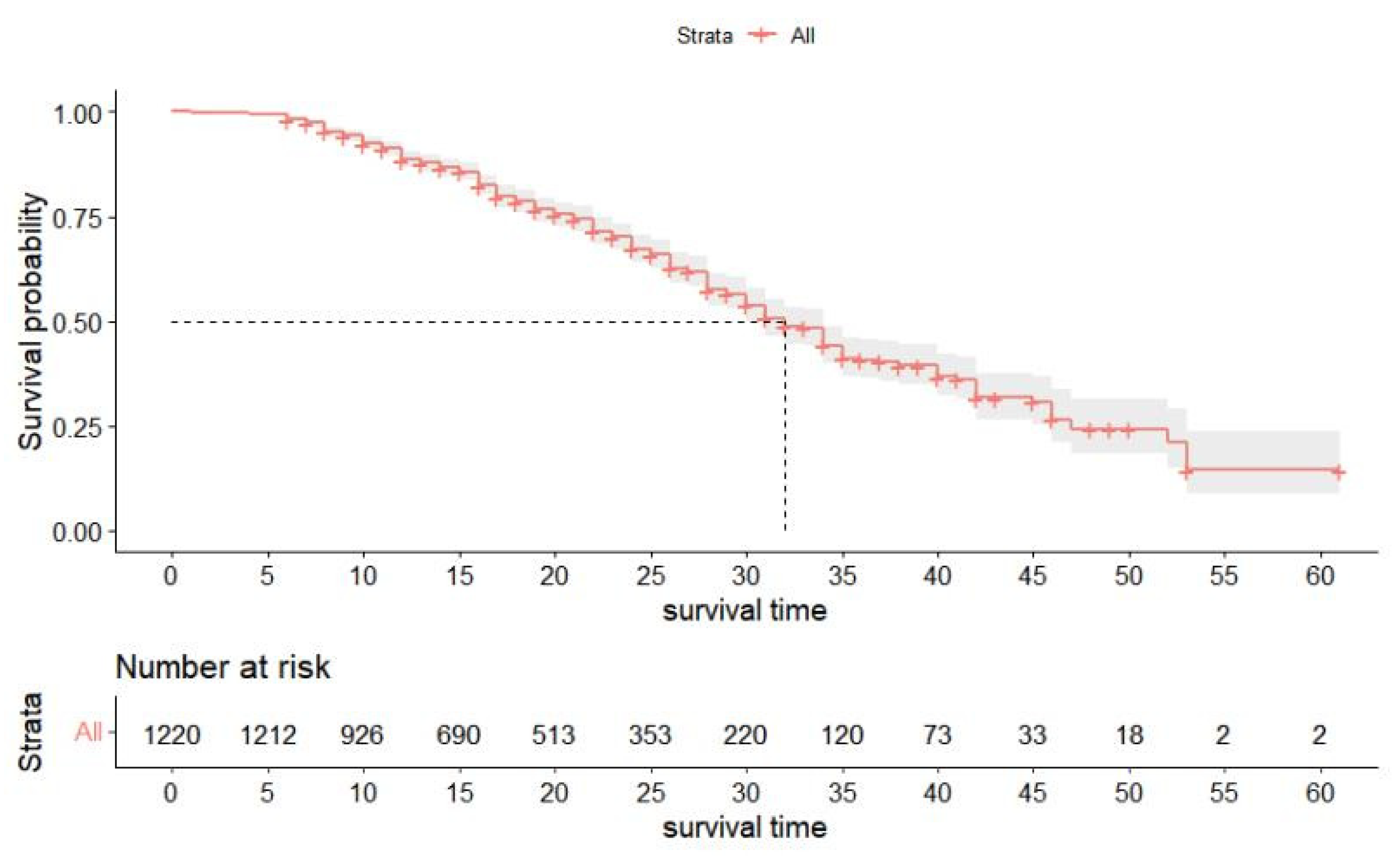
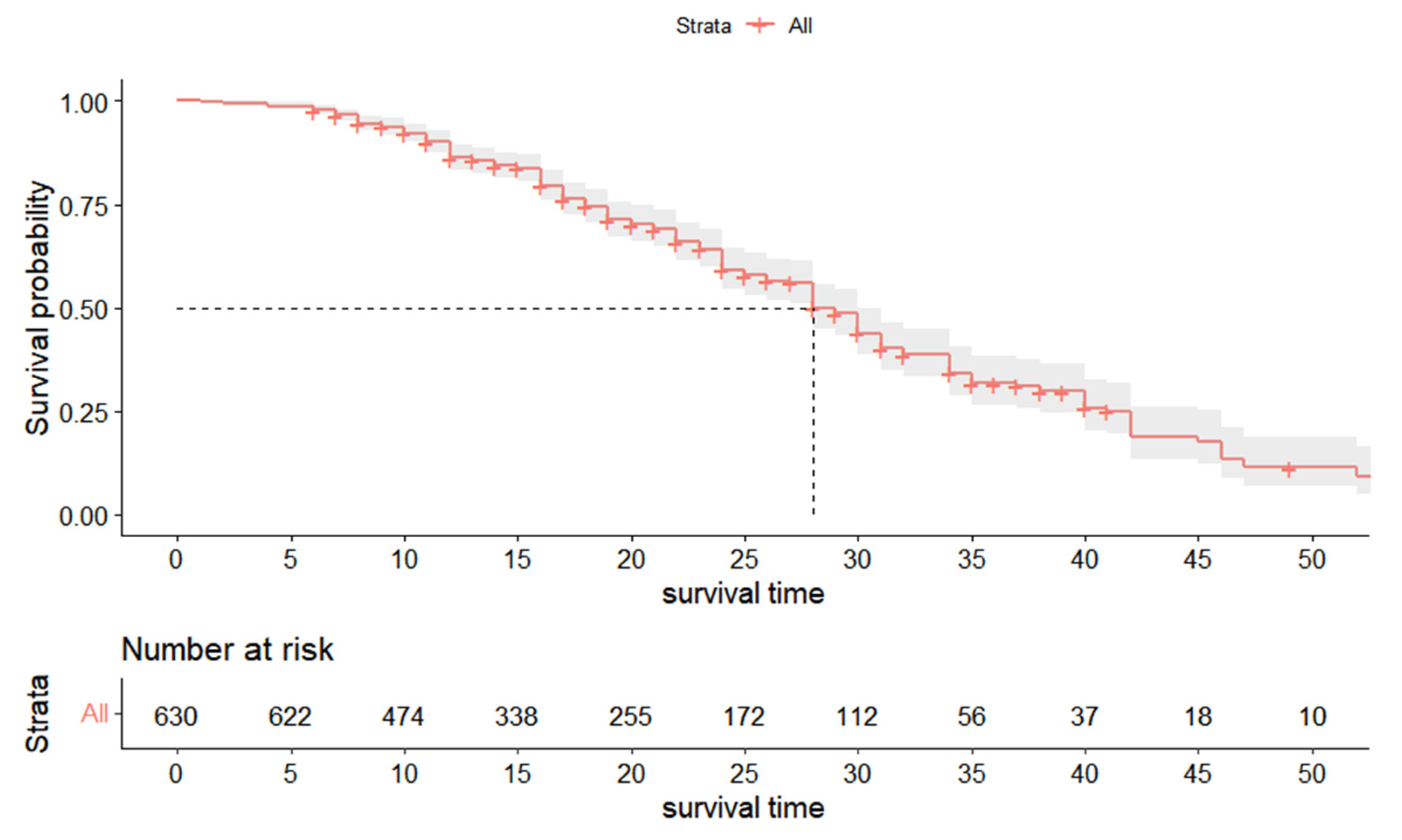
3.1. K-M Survival Analysis
3.2. Characteristics of the Teeth Receiving Pulpectomy
3.3. Potential Risk Factors for the Primary Tooth by Univariate and Multivariate Analyses
3.4. Potential Risk Factors for the Anterior and Posterior Primary Tooth
3.5. Anterior Primary Tooth
3.6. Posterior Primary Tooth
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wen, P.Y.F.; Chen, M.X.; Zhong, Y.J.; Dong, Q.Q.; Wong, H.M. Global Burden and Inequality of Dental Caries, 1990 to 2019. J. Dent. Res. 2022, 101, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Tinanoff, N. Introduction to the Conference: Innovations in the Prevention and Management of Early Childhood Caries. Pediatr. Dent. 2015, 37, 198–199. [Google Scholar] [PubMed]
- Uribe, S.E.; Innes, N.; Maldupa, I. The global prevalence of early childhood caries: A systematic review with meta-analysis using the WHO diagnostic criteria. Int. J. Paediatr. Dent. 2021, 31, 817–830. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wulaerhan, J.; Liu, Y.; Abudureyimu, A.; Zhao, J. Prevalence of severe early childhood caries and associated socioeconomic and behavioral factors in Xinjiang, China: A cross-sectional study. BMC Oral. Health 2017, 17, 144. [Google Scholar] [CrossRef] [PubMed]
- Priyadarshini, H.R.; Hiremath, S.S.; Puranik, M.; Rudresh, S.M.; Nagaratnamma, T. Prevalence of early childhood caries among preschool children of low socioeconomic status in Bangalore city, India. J. Int. Soc. Prev. Community Dent. 2011, 1, 27–30. [Google Scholar] [CrossRef]
- Souza, J.G.S.; Souza, S.E.; Noronha, M.d.S.; Ferreira, E.F.e.; Martins, A.M.E.d.B.L. Impact of untreated dental caries on the daily activities of children. J. Public Health Dent. 2018, 78, 197–202. [Google Scholar] [CrossRef]
- Ferraz, N.K.L.; Nogueira, L.C.; Pinheiro, M.L.P.; Marques, L.S.; Ramos-Jorge, M.L.; Ramos-Jorge, J. Clinical consequences of untreated dental caries and toothache in preschool children. Pediatr. Dent. 2014, 36, 389–392. [Google Scholar]
- Pulp Therapy for Primary and Immature Permanent Teeth. Pediatr. Dent. 2018, 40, 343–351.
- Camp, J. Pathways of the Pulp; CV Mosby: St. Louis, MO, USA, 2002; pp. 833–839. [Google Scholar]
- Brustolin, J.P.; Mariath, A.A.S.; Ardenghi, T.M.; Casagrande, L. Survival and factors associated with failure of pulpectomies performed in primary teeth by dental students. Braz. Dent. J. 2016, 28, 121–128. [Google Scholar] [CrossRef]
- Dou, G.; Wang, D.; Zhang, S.; Ma, W.; Xu, M.; Xia, B. A retrospective study on the long-term outcomes of pulpectomy and influencing factors in primary teeth. J. Dent. Sci. 2022, 17, 771–779. [Google Scholar] [CrossRef]
- Bartella, A.K.; Lechner, C.; Kamal, M.; Steegmann, J.; Holzle, F.; Lethaus, B. The safety of paediatric dentistry procedures under general anaesthesia. A five-year experience of a tertiary care center. Eur. J. Paediatr. Dent. 2018, 19, 44–48. [Google Scholar] [CrossRef] [PubMed]
- El Batawi, H.Y.; Panigrahi, P.; Awad, M.A. Perceived outcomes and satisfaction of Saudi parents and their children following dental rehabilitation under general anesthesia: A 2-year follow-up. J. Int. Soc. Prev. Community Dent. 2014, 4, S153. [Google Scholar] [CrossRef]
- Jankauskiene, B.; Virtanen, J.I.; Kubilius, R.; Narbutaite, J. Oral health-related quality of life after dental general anaesthesia treatment among children: A follow-up study. BMC Oral. Health 2014, 14, 81. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Loomans, B.A.; Huysmans, M.C. 12-year survival of composite vs. amalgam restorations. J. Dent. Res. 2010, 89, 1063–1067. [Google Scholar] [CrossRef]
- Daloğu, M.; Güzel, K.G.U. Root canal treatment for deciduous teeth: A review. Meandros Med. Dent. J. 2017, 18, 80. [Google Scholar] [CrossRef]
- Nadelman, P.; Bedran, N.; Magno, M.B.; Masterson, D.; de Castro, A.C.R.; Maia, L.C. Premature loss of primary anterior teeth and its consequences to primary dental arch and speech pattern: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2020, 30, 687–712. [Google Scholar] [CrossRef]
- Feu, D.; Lessa, F.C.R.; Barcellos, L.A.; Goulart, M.A.; Grillo, C.B.; Freitas, L.A. The impact on the quality of life caused by the early loss of primary molars. Int. J. Dent. Hyg. 2022, 20, 620–626. [Google Scholar] [CrossRef]
- Al-Shahrani, N.; Al-Amri, A.; Hegazi, F.; Al-Rowis, K.; Al-Madani, A.; Hassan, K.S. The prevalence of premature loss of primary teeth and its impact on malocclusion in the Eastern Province of Saudi Arabia. Acta Odontol. Scand. 2015, 73, 544–549. [Google Scholar] [CrossRef]
- Macena, M.C.; Tornisiello Katz, C.R.; Heimer, M.V.; de Oliveira e Silva, J.F.; Costa, L.B. Space changes after premature loss of deciduous molars among Brazilian children. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 771–778. [Google Scholar] [CrossRef]
- Boutsiouki, C.; Frankenberger, R.; Krämer, N. Clinical and radiographic success of (partial) pulpotomy and pulpectomy in primary teeth: A systematic review. Eur. J. Paediatr. Dent. 2021, 22, 273–285. [Google Scholar]
- Cleghorn, B.M.; Boorberg, N.B.; Christie, W.H. Primar.ry human teeth and their root canal systems. Endod. Top. 2010, 23, 6–33. [Google Scholar] [CrossRef]
- Gutierrez, R.G. Parametric frailty and shared frailty survival models. Stata J. 2002, 2, 22–44. [Google Scholar] [CrossRef]
- Hougaard, P. Shared frailty models. In Analysis of Multivariate Survival Data; Springer: New York, NY, USA, 2000; pp. 215–262. [Google Scholar]
- Dou, G.; Xia, B.; Zhu, J.; Wang, D.; Zhao, Y.; Sun, Z.; Cao, Z. Outcomes of pulpectomy in the primary dentition and age-related morphological changes in the root canal of primary molars: A retrospective study. Mapp. Intimacies, 2021; Preprint. [Google Scholar]
- Mesbahi, M.; Talei, Z.; Mollaverdi, F.; Kadkhodazadeh, M. Comparison of root canal system configuration in primary teeth. Res. J. Biol. Sci. 2010, 5, 488–491. [Google Scholar]
- Mendoza-Mendoza, A.; Caleza-Jiménez, C.; Solano-Mendoza, B.; Iglesias-Linares, A. Are there any differences between first and second primary molar pulpectomy prognoses? A retrospective clinical study. Eur. J. Paediatr. Dent. 2017, 18, 41–44. [Google Scholar] [CrossRef]
- Barcelos, R.; Tannure, P.N.; Gleiser, R.; Luiz, R.R.; Primo, L.G. The influence of smear layer removal on primary tooth pulpectomy outcome: A 24-month, double-blind, randomized, and controlled clinical trial evaluation. Int. J. Paediatr. Dent. 2012, 22, 369–381. [Google Scholar] [CrossRef]
- Seale, N.S. Stainless steel crowns improve success rate of root canal treatment in primary teeth. J. Evid. Based Dent. Pract. 2005, 5, 205–206. [Google Scholar] [CrossRef]
- Jeong, M.-a.; Kim, A.-h.; Shim, Y.-s.; An, S.-y. Restoration of Strip Crown with a Resin-Bonded Composite Cement in Early Childhood Caries. Case Rep. Dent. 2013, 2013, 581934. [Google Scholar] [CrossRef]
- Chen, Y.; Li, H.; Li, M.; Yang, L.; Sun, Q.; Chen, K. Analysis of survival and factors associated with failure of primary tooth pulpectomies performed under general anaesthesia in children from South China. Int. J. Paediatr. Dent. 2020, 30, 225–233. [Google Scholar] [CrossRef]
- Tang, J. The analyzing of the causes of pulpectomy treatment failure and retreatment of primary teeth [Chinese]. Chin. Med. 2018, 16, 142–143. [Google Scholar] [CrossRef]
- Shen, Y. The causes of pulpectomy treatment failure and retreatment of primary teeth from the clinical perspective[Chinese]. Chin. Foreign Med. Res. 2016, 14, 120–121. [Google Scholar] [CrossRef]
- Pramila, R.; Muthu, M.S.; Deepa, G.; Farzan, J.M.; Rodrigues, S.J. Pulpectomies in primary mandibular molars: A comparison of outcomes using three root filling materials. Int. Endod. J. 2016, 49, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Nakornchai, S.; Banditsing, P.; Visetratana, N. Clinical evaluation of 3Mix and Vitapex as treatment options for pulpally involved primary molars. Int. J. Paediatr. Dent. 2010, 20, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, X.; Zhong, J. Clinical and radiographic evaluation of pulpectomy in primary teeth: A 18-months clinical randomized controlled trial. Head Face Med. 2017, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitch, B.Z. Pulp management in primary teeth. Oral Surg. Oral Med. Oral Pathol. 1953, 6, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Rajsheker, S.; Mallineni, S.; Nuvvula, S. Obturating Materials Used for Pulpectomy in Primary Teeth-A Mini Review. J. Dent. Craniofac. Res. 2018, 3, 3. [Google Scholar] [CrossRef]
- Chonat, A.; Rajamani, T.; Rena, E. Obturating Materials in Primary Teeth—A Review. J. Dent. Sci. 2018, 6, 20–25. [Google Scholar]
- Reddy, V.V.; Fernandes. Clinical and radiological evaluation of zinc oxide-eugenol and Maisto’s paste as obturating materials in infected primary teeth--nine months study. J. Indian Soc. Pedod. Prev. Dent. 1996, 14, 39–44. [Google Scholar]
- Najjar, R.S.; Alamoudi, N.M.; El-Housseiny, A.A.; Al Tuwirqi, A.A.; Sabbagh, H.J. A comparison of calcium hydroxide/iodoform paste and zinc oxide eugenol as root filling materials for pulpectomy in primary teeth: A systematic review and meta-analysis. Clin. Exp. Dent. Res. 2019, 5, 294–310. [Google Scholar] [CrossRef]
- Coll, J.A.; Dhar, V.; Vargas, K.; Chen, C.-Y.; Crystal, Y.O.; AlShamali, S.; Marghalani, A.A. Use of non-vital pulp therapies in primary teeth. Pediatr. Dent. 2020, 42, 337–349. [Google Scholar]
- Anil, S.; Anand, P.S. Early Childhood Caries: Prevalence, Risk Factors, and Prevention. Front. Pediatr. 2017, 5, 157. [Google Scholar] [CrossRef] [PubMed]





| Factors | S (%) | F (%) | p * | HR |
|---|---|---|---|---|
| Gender | ||||
| male | 455 (65.4) | 241 (34.6) | 1 | |
| female | 368 (70.2) | 156 (29.8) | 0.77 | 0.91 |
| Age | <0.001 | 1.85 | ||
| 1–2 years | 7 (100) | 0 (0.0) | ||
| 2–3 years | 114 (69.1) | 51 (30.9) | ||
| 3–4 years | 310 (71.8) | 122 (28.2) | ||
| 4–5 years | 288 (62.5) | 173 (37.5) | ||
| 5–6 years | 104 (67.1) | 51 (32.9) | ||
| Tooth type | ||||
| anterior teeth | 451 (76.4) | 139 (23.6) | 1 | |
| molars | 372 (59.0) | 258 (41.0) | <0.001 | 1.83 |
| Preoperative condition mobility | ||||
| physiological | 695 (69.6) | 303 (30.4) | 1 | |
| abnormal | 128 (57.7) | 94 (42.3) | 0.02 | 1.52 |
| Soft tissue | ||||
| normal | 713 (69.0) | 320 (31.0) | 1 | |
| swelling or fistula | 110 (58.8) | 77 (41.2) | 0.02 | 1.55 |
| Radiographic evaluation | ||||
| normal | 648 (71.2) | 262 (28.8) | 1 | |
| abnormal | 175 (56.5) | 135 (43.5) | <0.001 | 2.25 |
| Obturation materials | ||||
| Vitapex | 336 (62.9) | 198 (37.1) | 1 | |
| ZOE | 487 (71.0) | 199 (29.0) | 0.14 | 0.68 |
| Degree of root filling | ||||
| underfilling | 202 (70.6) | 84 (29.4) | 1 | |
| optimal fillling | 506 (67.3) | 246 (32.7) | 0.02 | 0.50 |
| overfilling | 115 (63.2) | 67 (36.8) | 0.75 | 0.90 |
| Factor | Coef | SE (Coef) | p * | HR | 95% CI | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | 0.45 | 0.18 | 0.02 | 1.56 | 1.09 | 2.24 |
| Tooth type | ||||||
| anterior tooth | 1 | |||||
| posterior tooth | 0.64 | 0.17 | <0.001 | 1.90 | 1.36 | 2.65 |
| Radiological evaluation | ||||||
| normal | 1 | |||||
| abnormal | 0.88 | 0.17 | <0.001 | 2.41 | 1.74 | 3.36 |
| Factors | S (%) | F (%) | p * | HR |
|---|---|---|---|---|
| Age | 0.53 | 1.22 | ||
| 1–2 years | 7 (100.0) | 0 (0.0) | ||
| 2–3 years | 90 (70.3) | 38 (29.7) | ||
| 3–4 years | 185 (76.8) | 56 (23.2) | ||
| 4–5 years | 135 (75.8) | 43 (24.2) | ||
| 5–6 years | 34 (94.4) | 2 (5.6) | ||
| Tooth type | ||||
| central incisor | 203 (68.8) | 95 (31.2) | ||
| lateral incisor | 189 (81.6) | 45 (18.4) | <0.001 | 0.45 |
| canine | 55 (94.8) | 3 (5.2) | <0.001 | 0.03 |
| Number of surfaces affected | ||||
| Double | 187 (79.2) | 49 (20.8) | 0.32 | 1 |
| multiple | 246 (75.2) | 81 (24.8) | 1.64 | |
| Preoperative tooth mobility | ||||
| physiological | 368 (80.5) | 89 (19.5) | 0.09 | 1 |
| abnormal | 83 (62.4) | 50 (37.6) | 1.63 | |
| Soft tissue | ||||
| Normal | 377 (78.5) | 103 (21.5) | 1 | |
| swelling or Sinus tract | 74 (87.3) | 36 (12.7) | 0.09 | 1.66 |
| Radiographic evaluation | ||||
| Normal | 344 (81.1) | 80 (18.9) | 1 | |
| abnormal | 107 (64.5) | 59 (35.5) | <0.001 | 3.27 |
| Obturation materials | ||||
| Vitapex | 178 (70.4) | 75 (29.6) | 1 | |
| ZOE | 273 (76.4) | 64 (23.6) | 0.77 | 0.86 |
| Restoration method | ||||
| strip resin crown | 357 (75.8) | 114 (24.2) | 1 | |
| resin directly | 94 (79.0) | 25 (21.0) | 0.63 | 1.22 |
| Degree of root filling | ||||
| underfill | 113 (81.3) | 26 (18.7) | 1 | |
| optimal fill | 292 (73.9) | 103 (26.1) | 0.63 | 1.40 |
| Overfill | 46 (82.1) | 10 (18.9) | 0.67 | 1.27 |
| Coef | SE (Coef) | p * | HR | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Type of primary tooth | ||||||
| Central incisor | 1 | |||||
| Lateral incisor | −0.65 | 0.22 | <0.001 | 0.51 | 0.34 | 0.80 |
| Canine | −3.41 | 0.86 | <0.001 | 0.03 | 0.01 | 0.18 |
| Radiological evaluation | ||||||
| Abnormal | 1 | |||||
| Normal | 1.01 | 0.31 | <0.001 | 2.75 | 1.49 | 5.08 |
| Factors | S (%) | F (%) | p * | HR |
|---|---|---|---|---|
| Age | 0.001 | 2.16 | ||
| 2–3 years | 24 (64.9) | 13 (35.1) | ||
| 3–4 years | 125 (65.4) | 66 (34.6) | ||
| 4–5 years | 153 (54.1) | 130 (45.9) | ||
| 5–6 years | 70 (58.8) | 49 (41.2) | ||
| Tooth location | ||||
| maxillary molar | 142 (67.6) | 68 (32.4) | 1 | |
| mandibular molar | 230 (54.8) | 190 (45.2) | <0.001 | 2.00 |
| Tooth type | ||||
| 1st molar | 165 (52.9) | 147 (47.1) | 1 | |
| 2nd molar | 207 (65.1) | 111 (34.9) | 0.04 | 0.72 |
| Number of surfaces affected | ||||
| Single | 110 (66.3) | 56 (33.7) | 1 | |
| Double | 157 (56.5) | 121 (43.5) | 0.002 | 2.66 |
| Multiple | 100 (56.5) | 77 (43.5) | <0.001 | 4.29 |
| Preoperative tooth mobility | ||||
| physiological | 327 (60.4) | 214 (39.6) | 1 | |
| Abnormal | 45 (50.6) | 44 (49.4) | 0.03 | 1.94 |
| Soft tissue | ||||
| Normal | 336 (60.8) | 217 (39.2) | 1 | |
| swelling or fistula | 36 (46.8) | 41 (53.2) | 0.05 | 1.83 |
| Radiographic evaluation | ||||
| Normal | 304 (62.6) | 182 (37.4) | 1 | |
| Abnormal | 68 (47.2) | 76 (52.8) | <0.001 | 2.39 |
| Obturation materials | ||||
| Vitapex | 158 (56.2) | 123 (43.8) | 1 | |
| ZOE | 214 (61.3) | 135 (38.7) | 0.14 | 0.58 |
| Degree of root filling | ||||
| Underfilling | 89 (60.5) | 58 (39.5) | 1 | |
| optimal filling | 214 (59.9) | 143 (40.1) | 0.01 | 0.38 |
| Overfilling | 69 (54.8) | 57 (45.2) | 0.15 | 0.57 |
| Factor | Coef | SE (Coef) | p * | HR | 95%CI | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | 0.69 | 0.24 | 0.005 | 1.99 | 1.24 | 3.21 |
| Location: | ||||||
| Maxillary | 1 | |||||
| Mandibular | 0.88 | 0.20 | <0.001 | 2.42 | 1.65 | 3.56 |
| Number of surfaces affected | ||||||
| One | 1 | |||||
| Two | 1.39 | 0.33 | <0.001 | 4.01 | 2.09 | 7.68 |
| Multiple | 1.48 | 0.40 | <0.001 | 4.39 | 2.00 | 9.65 |
| Radiological evaluation | ||||||
| Normal | 1 | |||||
| Abnormal | 0.83 | 0.27 | 0.002 | 2.30 | 1.36 | 3.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, S.-y.; Li, J.-y.; Dai, S.-s.; Yang, Y.-h.; Wen, Y.-f.; Guo, Q.-y.; Liu, F. Survival Analysis and Risk Factors of Pulpectomy among Children with Severe Early Childhood Caries Treated under General Anesthesia: A Retrospective Study. Int. J. Environ. Res. Public Health 2023, 20, 1191. https://doi.org/10.3390/ijerph20021191
He S-y, Li J-y, Dai S-s, Yang Y-h, Wen Y-f, Guo Q-y, Liu F. Survival Analysis and Risk Factors of Pulpectomy among Children with Severe Early Childhood Caries Treated under General Anesthesia: A Retrospective Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1191. https://doi.org/10.3390/ijerph20021191
Chicago/Turabian StyleHe, Shu-yang, Jin-yi Li, Shan-shan Dai, Yu-hui Yang, Yi-feng Wen, Qing-yu Guo, and Fei Liu. 2023. "Survival Analysis and Risk Factors of Pulpectomy among Children with Severe Early Childhood Caries Treated under General Anesthesia: A Retrospective Study" International Journal of Environmental Research and Public Health 20, no. 2: 1191. https://doi.org/10.3390/ijerph20021191
APA StyleHe, S.-y., Li, J.-y., Dai, S.-s., Yang, Y.-h., Wen, Y.-f., Guo, Q.-y., & Liu, F. (2023). Survival Analysis and Risk Factors of Pulpectomy among Children with Severe Early Childhood Caries Treated under General Anesthesia: A Retrospective Study. International Journal of Environmental Research and Public Health, 20(2), 1191. https://doi.org/10.3390/ijerph20021191






