Education Level and Self-Reported Cardiovascular Disease in Norway—The Tromsø Study, 1994–2016
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Questionnaires, and Clinical Visits
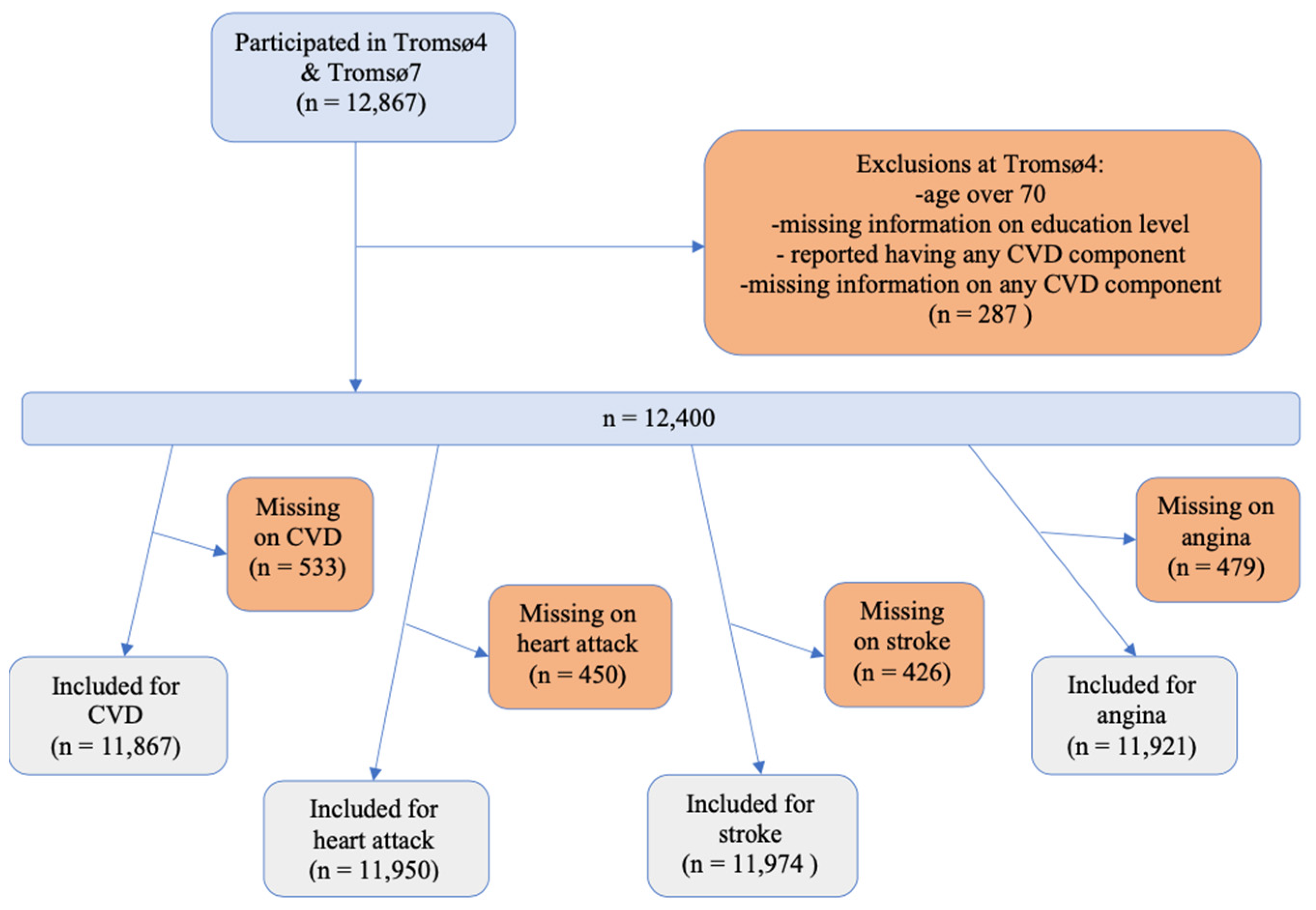
2.2. Study Sample
2.3. Assessment of Education Level, Covariates, and Cardiovascular Disease
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Norwegian Institute of Public Health. Norhealth. Available online: http://norgeshelsa.no/norgeshelsa/ (accessed on 23 May 2023).
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Kilkenny, M.F.; Dunstan, L.; Busingye, D.; Purvis, T.; Reyneke, M.; Orgill, M.; Cadilhac, D.A. Knowledge of risk factors for diabetes or cardiovascular disease (CVD) is poor among individuals with risk factors for CVD. PLoS ONE 2017, 12, e0172941. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Kivimäki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 2012, 9, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Mannsverk, J.; Wilsgaard, T.; Mathiesen, E.B.; Løchen, M.L.; Rasmussen, K.; Thelle, D.S.; Njølstad, I.; Hopstock, L.A.; Bønaa, K.H. Trends in Modifiable Risk Factors Are Associated with Declining Incidence of Hospitalized and Nonhospitalized Acute Coronary Heart Disease in a Population. Circulation 2016, 133, 74–81. [Google Scholar] [CrossRef]
- Norwegian Institute of Public Health. Cardiovascular Disease in Norway. Available online: https://www.fhi.no/en/op/hin/health-disease/cardiovascular-disease-in-norway---/ (accessed on 15 January 2021).
- Olsen, J.A. Principles in Health Economics and Policy, 2nd ed.; Oxford University Press: New York, NY, USA, 2017. [Google Scholar]
- Schultz, W.M.; Kelli, H.M.; Lisko, J.C.; Varghese, T.; Shen, J.; Sandesara, P.; Quyyumi, A.A.; Taylor, H.A.; Gulati, M.; Harold, J.G.; et al. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation 2018, 137, 2166–2178. [Google Scholar] [CrossRef]
- Beauchamp, A.; Peeters, A.; Wolfe, R.; Turrell, G.; Harriss, L.R.; Giles, G.G.; English, D.R.; McNeil, J.; Magliano, D.; Harrap, S.; et al. Inequalities in cardiovascular disease mortality: The role of behavioural, physiological and social risk factors. J. Epidemiol. Community Health 2010, 64, 542–548. [Google Scholar] [CrossRef]
- de Mestral, C.; Stringhini, S. Socioeconomic Status and Cardiovascular Disease: An Update. Curr. Cardiol. Rep. 2017, 19, 115. [Google Scholar] [CrossRef]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W.; et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef]
- Igland, J.; Vollset, S.E.; Nygård, O.K.; Sulo, G.; Ebbing, M.; Tell, G.S. Educational inequalities in acute myocardial infarction incidence in Norway: A nationwide cohort study. PLoS ONE 2014, 9, e106898. [Google Scholar] [CrossRef]
- Khaing, W.; Vallibhakara, S.A.; Attia, J.; McEvoy, M.; Thakkinstian, A. Effects of education and income on cardiovascular outcomes: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 1032–1042. [Google Scholar] [CrossRef]
- Rosengren, A.; Smyth, A.; Rangarajan, S.; Ramasundarahettige, C.; Bangdiwala, S.I.; AlHabib, K.F.; Avezum, A.; Boström, K.B.; Chifamba, J.; Gulec, S.; et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: The Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob. Health 2019, 7, e748–e760. [Google Scholar] [CrossRef] [PubMed]
- Woodward, M.; Peters, S.A.; Batty, G.D.; Ueshima, H.; Woo, J.; Giles, G.G.; Barzi, F.; Ho, S.C.; Huxley, R.R.; Arima, H.; et al. Socioeconomic status in relation to cardiovascular disease and cause-specific mortality: A comparison of Asian and Australasian populations in a pooled analysis. BMJ Open 2015, 5, e006408. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Jeong, M.H.; Park, I.H.; Choi, J.S.; Rhee, J.A.; Lee, D.H.; Park, S.H.; Kim, I.S.; Jeong, H.C.; Cho, J.Y.; et al. The association of socioeconomic status with three-year clinical outcomes in patients with acute myocardial infarction who underwent percutaneous coronary intervention. J. Korean Med. Sci. 2014, 29, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Psaltopoulou, T.; Hatzis, G.; Papageorgiou, N.; Androulakis, E.; Briasoulis, A.; Tousoulis, D. Socioeconomic status and risk factors for cardiovascular disease: Impact of dietary mediators. Hell. J. Cardiol. 2017, 58, 32–42. [Google Scholar] [CrossRef]
- Yu, J.; Dwyer-Lindgren, L.; Bennett, J.; Ezzati, M.; Gustafson, P.; Tran, M.; Brauer, M. A spatiotemporal analysis of inequalities in life expectancy and 20 causes of mortality in sub-neighbourhoods of Metro Vancouver, British Columbia, Canada, 1990–2016. Health Place 2021, 72, 102692. [Google Scholar] [CrossRef]
- Kivimäki, M.; Batty, G.D.; Pentti, J.; Shipley, M.J.; Sipilä, P.N.; Nyberg, S.T.; Suominen, S.B.; Oksanen, T.; Stenholm, S.; Virtanen, M.; et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: A multi-cohort study. Lancet Public Health 2020, 5, e140–e149. [Google Scholar] [CrossRef]
- Enroth, L.; Jasilionis, D.; Németh, L.; Strand, B.H.; Tanjung, I.; Sundberg, L.; Fors, S.; Jylhä, M.; Brønnum-Hansen, H. Changes in socioeconomic differentials in old age life expectancy in four Nordic countries: The impact of educational expansion and education-specific mortality. Eur. J. Ageing 2022, 19, 161–173. [Google Scholar] [CrossRef]
- Klitkou, S.T.; Wangen, K.R. Educational attainment and differences in relative survival after acute myocardial infarction in Norway: A registry-based population study. BMJ Open 2017, 7, e014787. [Google Scholar] [CrossRef]
- Sulo, G.; Igland, J.; Øverland, S.; Sulo, E.; Kinge, J.M.; Roth, G.A.; Tell, G.S. Socioeconomic Gradients in Mortality Following HF Hospitalization in a Country with Universal Health Care Coverage. JACC Heart Fail. 2020, 8, 917–927. [Google Scholar] [CrossRef]
- Hopstock, L.A.; Grimsgaard, S.; Johansen, H.; Kanstad, K.; Wilsgaard, T.; Eggen, A.E. The seventh survey of the Tromsø Study (Tromsø7) 2015–2016: Study design, data collection, attendance, and prevalence of risk factors and disease in a multipurpose population-based health survey. Scand. J. Public Health 2022, 50, 919–929. [Google Scholar] [CrossRef]
- Jacobsen, B.K.; Eggen, A.E.; Mathiesen, E.B.; Wilsgaard, T.; Njølstad, I. Cohort profile: The Tromso Study. Int. J. Epidemiol. 2012, 41, 961–967. [Google Scholar] [CrossRef] [PubMed]
- The Tromsø Study. Questionnaire Q1. Available online: https://uit.no/Content/686864/cache=20201407122756/Sporreskjema.Q1.engelskTromso7.pdf (accessed on 31 January 2021).
- University of Tromsø. Health Survey. Available online: https://uit.no/Content/271764/T4_Q1.pdf (accessed on 12 September 2021).
- IBM Corp. SPSS Statistics for Macintosh, Version 28.0; IBM Corp.: Armonk, NY, USA, 2021; Released 2021. [Google Scholar]
- Bijwaard, G.E. Educational differences in mortality and hospitalisation for cardiovascular diseases. J. Health Econ. 2022, 81, 102565. [Google Scholar] [CrossRef]
- Cajita, M.I.; Cajita, T.R.; Han, H.R. Health Literacy and Heart Failure: A Systematic Review. J. Cardiovasc. Nurs. 2016, 31, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Diederichs, C.; Jordan, S.; Domanska, O.; Neuhauser, H. Health literacy in men and women with cardiovascular diseases and its association with the use of health care services—Results from the population-based GEDA2014/2015-EHIS survey in Germany. PLoS ONE 2018, 13, e0208303. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.A. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. Patient Educ. Couns. 2016, 99, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Backholer, K.; Peters, S.A.E.; Bots, S.H.; Peeters, A.; Huxley, R.R.; Woodward, M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: A systematic review and meta-analysis. J. Epidemiol. Community Health 2017, 71, 550–557. [Google Scholar] [CrossRef]
- Albrektsen, G.; Heuch, I.; Løchen, M.L.; Thelle, D.S.; Wilsgaard, T.; Njølstad, I.; Bønaa, K.H. Lifelong Gender Gap in Risk of Incident Myocardial Infarction: The Tromsø Study. JAMA Intern. Med. 2016, 176, 1673–1679. [Google Scholar] [CrossRef]
- Breitborde, N.J.K.; Srihari, V.H.; Pollard, J.M.; Addington, D.N.; Woods, S.W. Mediators and moderators in early intervention research. Early Interv. Psychiatry 2010, 4, 143–152. [Google Scholar] [CrossRef]
- O’Keefe, J.H.; Bhatti, S.K.; Bajwa, A.; DiNicolantonio, J.J.; Lavie, C.J. Alcohol and cardiovascular health: The dose makes the poison…or the remedy. Mayo Clin. Proc. 2014, 89, 382–393. [Google Scholar] [CrossRef]
- Mortensen, E.L.; Jensen, H.H.; Sanders, S.A.; Reinisch, J.M. Better psychological functioning and higher social status may largely explain the apparent health benefits of wine: A study of wine and beer drinking in young Danish adults. Arch. Intern. Med. 2001, 161, 1844–1848. [Google Scholar] [CrossRef]
- Jones, D.P.; Wootton, R.E.; Gill, D.; Carter, A.R.; Gunnell, D.; Munafò, M.R.; Sallis, H.M. Mental Health as a Mediator of the Association Between Educational Inequality and Cardiovascular Disease: A Mendelian Randomization Study. J. Am. Heart Assoc. 2021, 10, e019340. [Google Scholar] [CrossRef] [PubMed]
- Dégano, I.R.; Marrugat, J.; Grau, M.; Salvador-González, B.; Ramos, R.; Zamora, A.; Martí, R.; Elosua, R. The association between education and cardiovascular disease incidence is mediated by hypertension, diabetes, and body mass index. Sci. Rep. 2017, 7, 12370. [Google Scholar] [CrossRef] [PubMed]
- Kershaw, K.N.; Droomers, M.; Robinson, W.R.; Carnethon, M.R.; Daviglus, M.L.; Monique Verschuren, W.M. Quantifying the contributions of behavioral and biological risk factors to socioeconomic disparities in coronary heart disease incidence: The MORGEN study. Eur. J. Epidemiol. 2013, 28, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, A.; Sebastiani, G.; Di Napoli, A.; Macciotta, A.; Di Filippo, P.; Strippoli, E.; Mirisola, C.; D’errico, A. Education inequalities in cardiovascular and coronary heart disease in Italy and the role of behavioral and biological risk factors. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 918–928. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, S.; Cerin, E.; Wilsgaard, T.; Løvsletten, O.; Njølstad, I.; Grimsgaard, S.; Hopstock, L.A.; Schirmer, H.; Rosengren, A.; Kristoffersen, K.; et al. Lifestyle factors as mediators of area-level socio-economic differentials in cardiovascular disease risk factors. The Tromsø Study. SSM Popul. Health 2022, 19, 101241. [Google Scholar] [CrossRef]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Rangul, V.; Bauman, A.; Holmen, T.L.; Midthjell, K. Is physical activity maintenance from adolescence to young adulthood associated with reduced CVD risk factors, improved mental health and satisfaction with life: The HUNT Study, Norway. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 144. [Google Scholar] [CrossRef]
- Tripepi, G.; Jager, K.J.; Dekker, F.W.; Zoccali, C. Selection bias and information bias in clinical research. Nephron Clin. Pract. 2010, 115, c94–c99. [Google Scholar] [CrossRef]
- Engstad, T.; Bonaa, K.H.; Viitanen, M. Validity of self-reported stroke: The Tromso Study. Stroke 2000, 31, 1602–1607. [Google Scholar] [CrossRef]
- Vo, C.Q.; Samuelsen, P.J.; Sommerseth, H.L.; Wisløff, T.; Wilsgaard, T.; Eggen, A.E. Validity of self-reported educational level in the Tromsø Study. Scand. J. Public Health 2022, 14034948221088004. [Google Scholar] [CrossRef]
| Abbreviation | Highest Obtained Education Level |
|---|---|
| EL1 | 7–10 years primary/secondary school, modern secondary school |
| EL2 | Technical school, middle school, vocational school, 1–2 years senior high school |
| EL3 | High school diploma (3–4 years) |
| EL4 | College/university, less than 4 years |
| EL5 | College/university, 4 or more years |
| Education Level 2 | |||||
|---|---|---|---|---|---|
| EL1 | EL2 | EL3 | EL4 | EL5 | |
| N (%) | 3106 (25.0) | 3717 (30.0) | 1271 (10.3) | 2213 (17.8) | 2093 (16.9) |
| Gender | |||||
| Women | 26.8 | 28.4 | 11.4 | 16.7 | 16.7 |
| Men | 23.0 | 31.8 | 8.9 | 19.2 | 17.1 |
| Age (years, %) | |||||
| 25–29 | 13.3 | 28.0 | 21.9 | 20.7 | 16.1 |
| 30–39 | 17.5 | 31.5 | 13.5 | 19.5 | 18.0 |
| 40–49 | 26.9 | 30.1 | 6.5 | 17.4 | 19.2 |
| 50–59 | 39.2 | 29.0 | 3.9 | 14.5 | 13.4 |
| 60–69 | 49.1 | 27.1 | 4.2 | 13.1 | 6.5 |
| Alcohol consumption (times/month) | 2.3 (2.8) | 2.8 (3.0) | 2.9 (3.2) | 3.6 (3.6) | 4.8 (4.6) |
| Daily cigarette smoking (%) | 32.7 | 34.1 | 10.3 | 14.1 | 8.8 |
| BMI (kg/m2, %) | |||||
| <25 | 22.0 | 29.2 | 11.0 | 18.6 | 19.2 |
| ≥25<30 | 27.8 | 31.3 | 9.1 | 17.2 | 14.6 |
| ≥30 | 34.4 | 29.8 | 10.0 | 15.6 | 10.1 |
| SBP (mmHg) | 131.9 (16.3) | 129.5 (15.5) | 126.3 (14.2) | 128.0 (15.4) | 126.8 (14.2) |
| Total cholesterol (mmol/L) | 6.2 (1.2) | 5.9 (1.2) | 5.5 (1.1) | 5.6 (1.2) | 5.6 (1.1) |
| Age-Adjusted | Multivariable | |||
|---|---|---|---|---|
| Cases/n | OR (95% CI) | Cases/n | OR (95% CI) | |
| Any CVD | 1024/11,867 | 0.91 (0.87–0.96) | 1023/11,825 1 | 0.96 (0.92–1.01) |
| Women | 343/6341 | 0.86 (0.79–0.94) | 343/6320 | 0.95 (0.87–1.04) |
| Men | 681/5526 | 0.91 (0.86–0.97) | 680/5505 | 0.97 (0.91–1.03) |
| Heart attack | 542/11,950 | 0.90 (0.84–0.96) | 488/11,000 2 | 0.97 (0.91–1.05) |
| Women | 144/6395 | 0.77 (0.67–0.88) | 125/5777 | 0.89 (0.76–1.04) |
| Men | 398/5555 | 0.91 (0.85–0.98) | 363/5223 | 1.00 (0.92–1.09) |
| Stroke | 366/11,974 | 0.97 (0.90–1.05) | 365/11,932 1 | 1.01 (0.93–1.09) |
| Women | 143/6405 | 0.94 (0.83–1.06) | 143/6384 | 1.01 (0.89–1.15) |
| Men | 223/5569 | 0.97 (0.88–1.06) | 222/5548 | 1.00 (0.91–1.10) |
| Angina | 261/11,921 | 0.98 (0.90–1.07) | 261/11,879 1 | 1.04 (0.95–1.14) |
| Women | 105/6381 | 0.92 (0.79–1.06) | 105/6360 | 1.02 (0.88–1.19) |
| Men | 156/5540 | 1.02 (0.91–1.14) | 156/5519 | 1.08 (0.96–1.21) |
| Age-Adjusted | Multivariable | |||
|---|---|---|---|---|
| Cases/n | OR (95% CI) | Cases/n | OR (95% CI) | |
| Any CVD | 1024/11,867 | 1023/11,825 1 | ||
| EL1 | 332/2894 | 1.00 (Ref) | 332/2883 | 1.00 (Ref) |
| EL2 | 343/3551 | 1.07 (0.91–1.26) | 342/3538 | 1.08 (0.91–1.28) |
| EL3 | 60/1235 | 0.73 (0.54–0.98) | 60/1229 | 0.83 (0.61–1.12) |
| EL4 | 171/2150 | 0.93 (0.76–1.14) | 171/2144 | 1.01 (0.82–1.24) |
| EL5 | 118/2037 | 0.66 (0.53–0.82) | 118/2031 | 0.83 (0.66–1.05) |
| Heart attack | 542/11,950 | 488/11,000 2 | ||
| EL1 | 185/2929 | 1.00 (Ref) | 158/2569 | 1.00 (Ref) |
| EL2 | 181/3577 | 1.01 (0.82–1.26) | 169/3309 | 1.05 (0.83–1.33) |
| EL3 | 28/1246 | 0.62 (0.41–0.93) | 24/1161 | 0.69 (0.44–1.08) |
| EL4 | 92/2159 | 0.91 (0.70–1.18) | 82/1924 | 0.98 (0.73–1.32) |
| EL5 | 56/2039 | 0.58 (0.43–0.79) | 55/1924 | 0.91 (0.65–1.28) |
| Stroke | 366/11,974 | 365/11,932 1 | ||
| EL1 | 107/2935 | 1.00 (Ref) | 107/2924 | 1.00 (Ref) |
| EL2 | 124/3580 | 1.23 (0.94–1.60) | 123/3567 | 1.22 (0.93–1.60) |
| EL3 | 25/1245 | 1.00 (0.64–1.58) | 25/1239 | 1.09 (0.69–1.72) |
| EL4 | 62/2163 | 1.08 (0.78–1.50) | 62/2157 | 1.13 (0.81–1.57) |
| EL5 | 48/2051 | 0.89 (0.62–1.26) | 48/2045 | 1.04 (0.73–1.49) |
| Angina | 261/11,921 | 261/11,879 1 | ||
| EL1 | 84/2924 | 1.00 (Ref) | 84/2913 | 1.00 (Ref) |
| EL2 | 77/3555 | 0.96 (0.70–1.32) | 77/3542 | 1.00 (0.73–1.39) |
| EL3 | 17/1239 | 0.85 (0.50–1.46) | 17/1233 | 1.00 (0.58–1.73) |
| EL4 | 46/2161 | 1.02 (0.70–1.47) | 46/2155 | 1.16 (0.79–1.69) |
| EL5 | 37/2042 | 0.87 (0.58–1.29) | 37/2036 | 1.16 (0.77–1.74) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cathro, C.J.; Brenn, T.; Chen, S.L.F. Education Level and Self-Reported Cardiovascular Disease in Norway—The Tromsø Study, 1994–2016. Int. J. Environ. Res. Public Health 2023, 20, 5958. https://doi.org/10.3390/ijerph20115958
Cathro CJ, Brenn T, Chen SLF. Education Level and Self-Reported Cardiovascular Disease in Norway—The Tromsø Study, 1994–2016. International Journal of Environmental Research and Public Health. 2023; 20(11):5958. https://doi.org/10.3390/ijerph20115958
Chicago/Turabian StyleCathro, Celina Janene, Tormod Brenn, and Sairah Lai Fa Chen. 2023. "Education Level and Self-Reported Cardiovascular Disease in Norway—The Tromsø Study, 1994–2016" International Journal of Environmental Research and Public Health 20, no. 11: 5958. https://doi.org/10.3390/ijerph20115958
APA StyleCathro, C. J., Brenn, T., & Chen, S. L. F. (2023). Education Level and Self-Reported Cardiovascular Disease in Norway—The Tromsø Study, 1994–2016. International Journal of Environmental Research and Public Health, 20(11), 5958. https://doi.org/10.3390/ijerph20115958






