A Systematic Review of the Influence of Overweight and Obesity across the Lifespan on Obstacle Crossing during Walking
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility, Inclusion, and Exclusion Criteria
2.3. Data Sources and Search Strategy
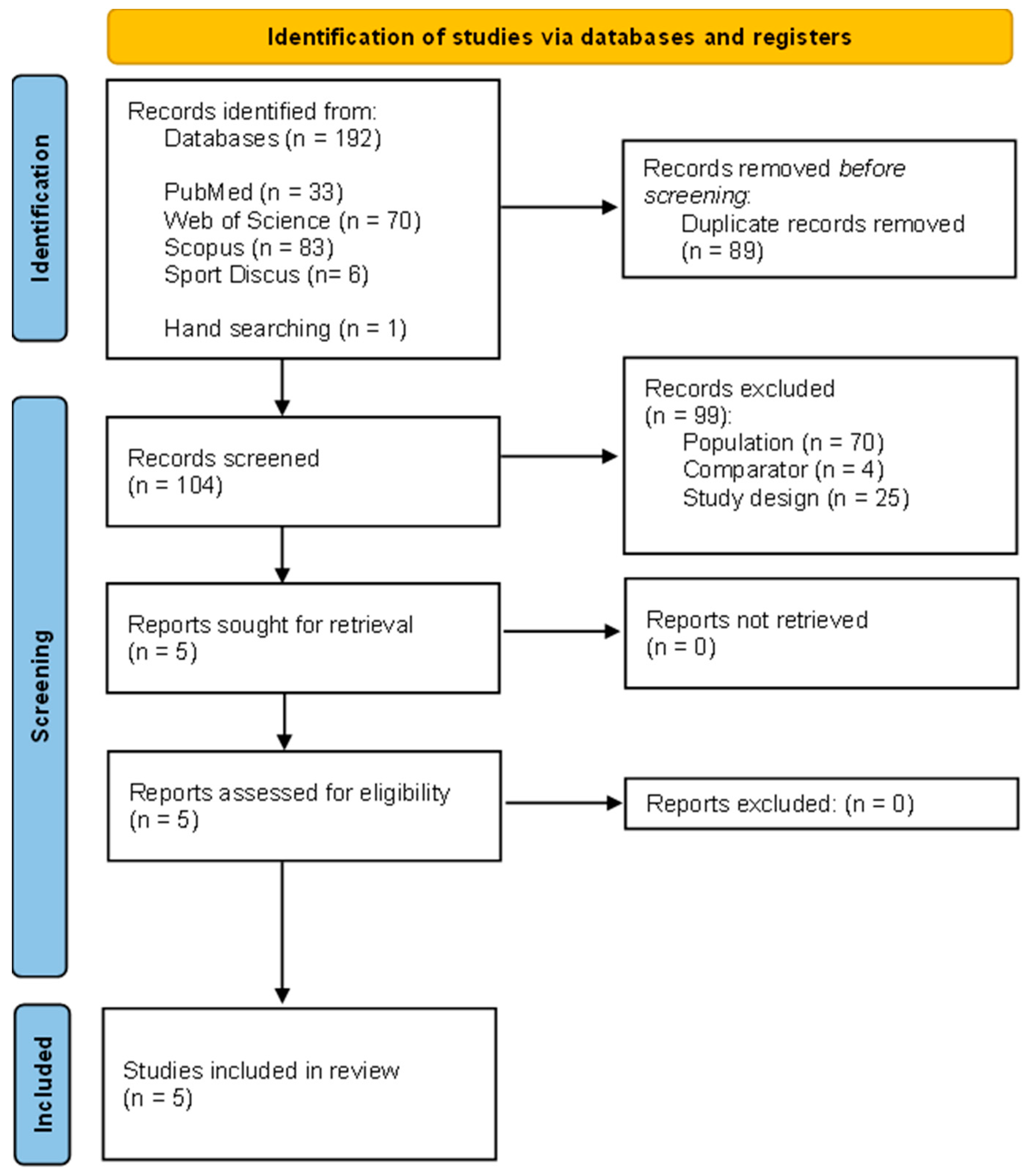
2.4. Study Selection
2.5. Data Extraction
- (1)
- Study characteristics: first author, title, year of publication, journal name, country, study design, mention of any adverse events occurring during the study, and funding;
- (2)
- Sample description: sample size, age, sex, body weight, body height, body mass index, lower limb length, health status, fall status, and limb preference;
- (3)
- Obstacle-crossing protocol: task requirement, instrumentation, data acquisition methodology, and gait parameters assessed;
- (4)
- Main results obtained from gait measurement: spatial-temporal parameters, muscle activity, joint angle and moment, ground reaction force, and obstacle contacts.
2.6. Quality Assessment
2.7. Data Synthesis
3. Results
3.1. Study Selection
3.2. General Information about the Studies Included in the Systematic Review
3.3. Study Characteristics
3.4. Quality Assessment
Sample Characteristics
3.5. Obstacle-Crossing Task
- -
- Step length, width, cadence, and single- and double-limb support phases [18];
- -
- Stance and swing time and their coefficients of variation, and the coefficient of variation of velocity [22];
- -
- Time from foot lift to maximum knee height and from maximum knee height to foot contact, maximum knee height (plus sagittal knee and ankle angles at maximum knee height), and ankle angle at foot contact [19];
- -
- Leading- and trailing-leg toe clearance, hip and knee angles at maximum knee height in the sagittal and frontal planes, COM (centre of mass) anterior and posterior, and medial, lateral and vertical acceleration at the leading and trailing legs’ maximum knee height during crossing [20];
- -
- Relative foot temporal data at initial and final foot contact and duration of contact of the HL (lateral heel), HM (medial heel), MF (midfoot), M1-5 (metatarsal areas), T2-5 (toes), and T1 (hallux) areas of the leading and trailing legs [21].
3.6. Influence of Overweight/Obesity on Obstacle Crossing during Walking
3.6.1. Kinematic Parameters
- Being OB led to a significantly lower crossing step length [18].
- The OB group showed a significantly lower cadence [18].
- OB individuals spent less time in single limb support [18].
- The OB group had a greater step width [18].
- OB individuals spent more time in the double-limb support phase [18].
- The OW/Class I OB group spent more time in stance than the NOB and Class II OB groups [22].
- The OW/Class I OB, Class II OB, and Class III OB groups had lower swing times during crossing [22].
3.6.2. Kinetic Parameters
3.7. Synthesis
4. Discussion
4.1. Influence of Overweight/Obesity on Kinematic Parameters during Obstacle Crossing
4.2. Influence of Overweight/Obesity on Kinetic Parameters during Obstacle Crossing
4.3. Limitations and Strengths
4.4. Practical Implications and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 4 October 2022).
- Akram, D.S.; Astrup, A.V.; Atinmo, T.; Boissin, J.L.; Bray, G.A.; Caroll, K.K.; Chitson, P.; Chunming, C.; Dietz, W.H.; Hill, J.O.; et al. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; World Health Organization Technical Repport Series: Geneva, Switzerland, 2000; Volume 894, pp. 1–253. [Google Scholar]
- Apovian, C. Obesity: Definition, Comorbidities, Causes, and Burden. Am. J. Manag. Care 2016, 22, s176–s185. [Google Scholar] [PubMed]
- Han, E.; Truesdale, K.P.; Taber, D.R.; Cai, J.; Juhaeri, J.; Stevens, J. Impact of Overweight and Obesity on Hospitalization: Race and Gender Differences. Int. J. Obes. 2009, 33, 249–256. [Google Scholar] [CrossRef] [PubMed]
- di Angelantonio, E.; Bhupathiraju, S.N.; Wormser, D.; Gao, P.; Kaptoge, S.; de Gonzalez, A.B.; Cairns, B.J.; Huxley, R.; Jackson, C.L.; Joshy, G.; et al. Body-Mass Index and All-Cause Mortality: Individual-Participant-Data Meta-Analysis of 239 Prospective Studies in Four Continents. Lancet 2016, 388, 776–786. [Google Scholar] [CrossRef]
- Heo, M.; Pietrobelli, A.; Wang, D.; Heymsfield, S.B.; Faith, M.S. Obesity and Functional Impairment: Influence of Comorbidity, Joint Pain, and Mental Health. Obesity 2010, 18, 2030–2038. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Nemet, D.; Pantanowitz, M.; Eliakim, A. Gait Pattern, Impact to the Skeleton and Postural Balance in Overweight and Obese Children: A Review. Sports 2018, 6, 75. [Google Scholar] [CrossRef]
- del Porto, H.; Pechak, C.; Smith, D.; Reed-Jones, R. Biomechanical Effects of Obesity on Balance. Int. J. Exerc. Sci. 2012, 5, 301–320. [Google Scholar]
- Molina-Garcia, P.; Migueles, J.H.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Plaza-Florido, A.; Vanrenterghem, J.; Ortega, F.B. A Systematic Review on Biomechanical Characteristics of Walking in Children and Adolescents with Overweight/Obesity: Possible Implications for the Development of Musculoskeletal Disorders. Obes. Rev. 2019, 20, 1033–1044. [Google Scholar] [CrossRef]
- Backholer, K.; Wong, E.; Freak-Poli, R.; Walls, H.L.; Peeters, A. Increasing Body Weight and Risk of Limitations in Activities of Daily Living: A Systematic Review and Meta-Analysis. Obes. Rev. 2012, 13, 456–468. [Google Scholar] [CrossRef]
- Wearing, S.C.; Hennig, E.M.; Byrne, N.M.; Steele, J.R.; Hills, A.P. The Biomechanics of Restricted Movement in Adult Obesity. Obes. Rev. 2006, 7, 13–24. [Google Scholar] [CrossRef]
- Neri, S.G.R.; Oliveira, J.S.; Dario, A.B.; Lima, R.M.; Tiedemann, A. Does Obesity Increase the Risk and Severity of Falls in People Aged 60 Years and Older? A Systematic Review and Meta-Analysis of Observational Studies. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 952–960. [Google Scholar] [CrossRef]
- Capodaglio, P.; Gobbi, M.; Donno, L.; Fumagalli, A.; Buratto, C.; Galli, M.; Cimolin, V. Effect of Obesity on Knee and Ankle Biomechanics during Walking. Sensors 2021, 21, 7114. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Máximo, R.; de Oliveira, D.C.; Ramírez, P.C.; Luiz, M.M.; de Souza, A.F.; Delinocente, M.L.B.; Steptoe, A.; de Oliveira, C.; da Silva Alexandre, T. Dynapenia, Abdominal Obesity or Both: Which Accelerates the Gait Speed Decline Most? Age Ageing 2021, 50, 1616–1625. [Google Scholar] [CrossRef]
- Kim, D.; Lewis, C.L.; Gill, S.V. Effects of Obesity and Foot Arch Height on Gait Mechanics: A Cross-Sectional Study. PLoS ONE 2021, 16, e0260398. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Capodaglio, P.; Leban, B.; Porta, M.; Galli, M.; Cimolin, V. Kinematics Adaptation and Inter-Limb Symmetry during Gait in Obese Adults. Sensors 2021, 21, 5980. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Lim, J.; Lee, S. Body Fat-Related Differences in Gait Parameters and Physical Fitness Level in Weight-Matched Male Adults. Clin. Biomech. 2021, 81, 105243. [Google Scholar] [CrossRef] [PubMed]
- Desrochers, P.C.; Kim, D.; Keegan, L.; Gill, S.V. Association between the Functional Gait Assessment and Spatiotemporal Gait Parameters in Individuals with Obesity Compared to Normal Weight Controls: A Proof-of-Concept Study. J. Musculoskelet. Neuronal Interact. 2021, 21, 335–342. [Google Scholar]
- Gill, S.V.; Hung, Y.C. Influence of Weight Classification on Children Stepping over Obstacles. Am. J. Phys. Med. Rehabil. 2012, 91, 625–630. [Google Scholar] [CrossRef]
- Gill, S.V.; Hung, Y.C. Effects of Overweight and Obese Body Mass on Motor Planning and Motor Skills during Obstacle Crossing in Children. Res. Dev. Disabil. 2014, 35, 46–53. [Google Scholar] [CrossRef]
- Silva, D.; Gabriel, R.; Moreira, H.; Abrantes, J.; Faria, A. Foot Rollover Temporal Parameters During Walking Straight Ahead and Stepping Over Obstacles: Obese and Non-Obese Postmenopausal Women. J. Aging Phys. Act. 2018, 26, 227–234. [Google Scholar] [CrossRef]
- Gill, S.V. Effects of Obesity Class on Flat Ground Walking and Obstacle Negotiation. J. Musculoskelet. Neuronal Interact. 2019, 19, 448–454. [Google Scholar]
- Pavol, M.J.; Owings, T.M.; Foley, K.T.; Grabiner, M.D. Mechanisms Leading to a Fall from an Induced Trip in Healthy Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Berg, W.P.; Alessio, H.M.; Mills, E.M.; Tong, C. Circumstances and Consequences of Falls in Independent Community-Dwelling Older Adults. Age Ageing 1997, 26, 261–268. [Google Scholar] [CrossRef]
- Brown, L.A.; McKenzie, N.C.; Doan, J. Age-Dependent Differences in the Attentional Demands of Obstacle Negotiation. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 924–927. [Google Scholar] [CrossRef] [PubMed]
- Hahn, M.E.; Lee, H.-J.; Chou, L.-S. Increased Muscular Challenge in Older Adults during Obstructed Gait. Gait Posture 2005, 22, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P.; Sievänen, H.; Palvanen, M.; Järvinen, T.; Parkkari, J. Prevention of Falls and Consequent Injuries in Elderly People. Lancet 2005, 366, 1885–1893. [Google Scholar] [CrossRef]
- Uemura, K.; Yamada, M.; Nagai, K.; Ichihashi, N. Older Adults At High Risk of Falling Need More Time for Anticipatory Postural Adjustment in the Precrossing Phase of Obstacle Negotiation. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 904–909. [Google Scholar] [CrossRef]
- Pieruccini-Faria, F.; Montero-Odasso, M.; Newman, A. Obstacle Negotiation, Gait Variability, and Risk of Falling: Results From the “Gait and Brain Study”. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1422–1428. [Google Scholar] [CrossRef]
- Patla, A.E.; Prentice, S.D.; Robinson, C.; Neufeld, J. Visual Control of Locomotion: Strategies for Changing Direction and for Going Over Obstacles. J. Exp. Psychol. Hum. Percept. Perform. 1991, 17, 603–634. [Google Scholar] [CrossRef]
- Patla, A.; Rietdyk, S. Visual Control of Limb Trajectory over Obstacles during Locomotion: Effect of Obstacle Height and Width. Gait Posture 1993, 1, 45–60. [Google Scholar] [CrossRef]
- Walsh, T.P.; Arnold, J.B.; Evans, A.M.; Yaxley, A.; Damarell, R.A.; Shanahan, E.M. The Association between Body Fat and Musculoskeletal Pain: A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2018, 19, 233. [Google Scholar] [CrossRef]
- Chardon, M.; Barbieri, F.A.; Penedo, T.; Santos, P.C.R.; Vuillerme, N. The Effects of Overweight and Obesity on Obstacle Crossing During Walking: Protocol for a Systematic Review. JMIR Res. Protoc. 2022, 11, e36234. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Kuczmarski, R.J.; National Center for Health Statistics (U.S.); National Health and Nutrition Examination Survey (U.S.). 2000 CDC Growth Charts for the United States: Methods and Development; Department of Health and Human Services: Washington, DC, USA; Centers for Disease Control and Prevention: Atlanta, GA, USA; National Center for Health Statistics: Hyattsville, MD, USA, 2002.
- Galna, B.; Peters, A.; Murphy, A.T.; Morris, M.E. Obstacle Crossing Deficits in Older Adults: A Systematic Review. Gait Posture 2009, 30, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Overweight & Obesity|CDC. Available online: https://www.cdc.gov/obesity/index.html (accessed on 14 December 2021).
- Brochu, M.; Mathieu, M.E.; Karelis, A.D.; Doucet, É.; Lavoie, M.E.; Garrel, D.; Rabasa-Lhoret, R. Contribution of the Lean Body Mass to Insulin Resistance in Postmenopausal Women with Visceral Obesity: A Monet Study. Obesity 2008, 16, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.V. Optimising Motor Adaptation in Childhood Obesity. Aust. Occup. Ther. J. 2011, 58, 386–389. [Google Scholar] [CrossRef]
- Wearing, S.C.; Hennig, E.M.; Byrne, N.M.; Steele, J.R.; Hills, A.P. The Impact of Childhood Obesity on Musculoskeletal Form. Obes. Rev. 2006, 7, 209–218. [Google Scholar] [CrossRef]
- Maktouf, W.; Durand, S.; Boyas, S.; Pouliquen, C.; Beaune, B. Interactions among Obesity and Age-Related Effects on the Gait Pattern and Muscle Activity across the Ankle Joint. Exp. Gerontol. 2020, 140, 111054. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Park, W.; Levy, M.S.; Jung, E.E. The Effects of Obesity and Standing Time on Postural Sway during Prolonged Quiet Standing. Ergonomics 2009, 52, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Deforche, B.I.; Hills, A.P.; Worringham, C.J.; Davies, P.S.W.; Murphy, A.J.; Bouckaert, J.J.; de Bourdeaudhuij, I.M. Balance and Postural Skills in Normal-Weight and Overweight Prepubertal Boys. Int. J. Pediatr. Obes. 2009, 4, 175–182. [Google Scholar] [CrossRef]
- Smith, L.; Johansson, J.; Kerrigan, D. Gender Differences in Pelvic Motions and Center of Mass Displacement during Walking: Stereotypes Quantified. J. Womens Health Gend. Based Med. 2002, 11, 453–458. [Google Scholar] [CrossRef]
- Chardon, M.; Barbieri, F.A.; Penedo, T.; Santos, P.C.R.; Vuillerme, N. The Effects of Experimentally-Induced Fatigue on Gait Parameters during Obstacle Crossing: A Systematic Review. Neurosci. Biobehav. Rev. 2022, 142, 104854. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.S.; Draganich, L.F. Stepping over an Obstacle Increases the Motions and Moments of the Joints of the Trailing Limb in Young Adults. J. Biomech. 1997, 30, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.L.; Lu, T.W. Comparisons of the Joint Moments between Leading and Trailing Limb in Young Adults When Stepping over Obstacles. Gait Posture 2006, 23, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-C.; Ashton-Miller, J.; Alexander, N.; Schultz, A. Stepping Over Obstacles: Gait Patterns of Healthy Young and Old Adults. J. Gerontol. 1991, 46, M196–M203. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | Overweight or obese individuals | Acute or overuse injuries or with neurological, musculoskeletal or systemic diseases unrelated to OB comorbidities |
| Intervention | Obstacle-crossing task during walking | Obstacle avoidance during a non-walking task Walking task without obstacle crossing |
| Comparator | Healthy normal-weight individuals | Non-healthy normal-weight individuals |
| Outcomes | Kinematic, kinetic, and electromyographic | None |
| Study design | Randomised controlled trials, non-randomised controlled trials, and non-randomised, non-controlled trials. Published in English in a peer-reviewed journal | Case reports, abstracts, editorials, letters to the editor, case studies, reviews, meta-analyses, theses, grey literature (annual, research, technical, or project reports), working papers, and government documents |
| Author | Gill and Hung [19] | Gill and Hung [20] | Silva et al. [21] | Gill [22] | Desrochers et al. [18] |
|---|---|---|---|---|---|
| Publication year | 2012 | 2014 | 2018 | 2019 | 2021 |
| Country | USA | USA | Portugal | USA | USA |
| Title | Influence of weight classification on children stepping over obstacles | Effects of overweight and obese body mass on motor planning and motor skills during obstacle crossing in children | Foot rollover temporal parameters during walking straight ahead and stepping over obstacles: obese and non-obese post-menopausal women | Effects of obesity class on flat ground walking and obstacle negotiation | Association between the Functional Gait Assessment and spatiotemporal gait parameters in individuals with obesity compared to normal-weight controls: A proof-of-concept study |
| Journal | American Journal of Physical Medicine and Rehabilitation | Research in Developmental Disabilities | Journal of Aging and Physical Activity | Journal of Musculoskeletal Neuronal Interactions | Journal of Musculoskeletal Neuronal Interactions |
| Study design | Observational cross-sectional | Observational cross-sectional | Observational cross-sectional | Observational cross-sectional | Observational cross-sectional, proof-of-concept |
| Main objective | To examine how weight classification relates to children’s ability to meet a task constraint: crossing obstacles of various heights. | To examine whether body mass index would influence the ability of 4- to 13-year-olds to plan and coordinate their movements to cross obstacles of various heights. | To explore the potential differences between walking straight ahead and walking stepping over obstacles for OB and NOB post-menopausal women. | To investigate how increasing obesity classes affected gait and gait variability in adults. | To determine how to capture gait and balance impairments in adults with obesity using an inexpensive method as a proof-of-concept for possible future validation. |
| Main Findings | During obstacle crossing, children who were overweight or obese took longer to cross obstacles and had a dorsiflexed ankle position when landing. We also found that children demonstrated high variability in ankle position when crossing medium obstacles and during the final baseline trials. | Differences in motor planning and motor skills between normal weight and overweight/obese children during obstacle crossing may reflect movement patterns evident during early skill acquisition in which children attempt to freeze degrees of freedom, exhibit difficulty planning and controlling their movements with excess adiposity, or use unknown mechanisms responsible for motor planning and motor skill abilities | Significant differences were found in temporal characteristics of foot rollover during walking straight ahead and stepping over obstacles in both groups, with most of these differences being common for both OB and NOB subjects. | Increases in classes of obesity are associated with more difficulties with spatiotemporal gait and gait variability. Most importantly, there were few differences between Class II and Class III obesity. | Poorer FGA scores in the obese group were associated with slowing of gait when encountering obstacles but not during flat over-ground walking. Further, the presence of obstacles during gait tasks may be helpful in revealing meaningful gait impairments in obesity and other populations. |
| Funding | No funding information reported. | Boston University start-up funds. | European Investment Funds via FEDER/COMPETE/POCI—Operational Competitiveness and Internationalisation Programme, under project POCI-01-0145-FEDER-006958 and National Funds via FCT—Portuguese Foundation for Science and Technology, under project UID/AGR/04033/2013 | R03 AR066344-01 A1 (Gill, PI). | NIH R03 AR066344-01A1 (Gill, PI). |
| Question | Scoring Criteria | Gill and Hung [19] | Gill and Hung [20] | Silva et al. [21] | Gill [22] | Desrochers et al. [18] | Average |
|---|---|---|---|---|---|---|---|
| 1. Research aims or questions stated clearly | Y = 1; L = 0.5; N = 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2. Participants detailed | Number | 1 | 1 | 1 | 1 | 1 | 1 |
| Age | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sex | 1 | 1 | 1 | 1 | 1 | 1 | |
| Height | 0 | 0 | 1 | 0 | 1 | 0.4 | |
| Body mass | 0 | 0 | 1 | 0 | 1 | 0.4 | |
| Body mass index | 1 | 1 | 1 | 1 | 1 | 1 | |
| Subtotal | 0.67 | 0.67 | 1 | 0.67 | 1 | 0.8 | |
| 3. Recruitment and sampling methods described | Y = 1; L = 0.5; N = 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| 4. Inclusion and exclusion criteria detailed | Y = 1; L = 0.5; N = 0 | 1 | 1 | 1 | 1 | 0.5 | 0.9 |
| 5. Covariates controlled for | Age | 1 | 1 | 1 | 1 | 1 | 1 |
| Sex | 0 | 0 | 1 | 1 | 0 | 0.4 | |
| Height | 0 | 0.5 | 1 | 0 | 0 | 0.3 | |
| Body mass | 0 | 0 | 0 | 0 | 0 | 0 | |
| Body mass index | 1 | 1 | 1 | 1 | 1 | 1 | |
| Limb asymmetries | 0 | 0 | 1 | 0 | 1 | 0.4 | |
| Strength | 0 | 0 | 0 | 0 | 0 | 0 | |
| Stride/step Speed | 1 | 1 | 1 | 1 | 0 | 0.8 | |
| Subtotal | 0.38 | 0.44 | 0.88 | 0.5 | 0.38 | 0.52 | |
| 6. Key outcome variables clearly described | Y = 1; L = 0.5; N = 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| 7. Adequate methodology ables study replication | Participants | 0.5 | 0.5 | 1 | 0.5 | 1 | 0.7 |
| Equipment | 1 | 1 | 1 | 1 | 1 | 1 | |
| Procedure | 1 | 1 | 1 | 1 | 1 | 1 | |
| Processing | 1 | 1 | 1 | 1 | 1 | 1 | |
| Statistics | 1 | 1 | 1 | 1 | 1 | 1 | |
| Subtotal | 0.9 | 0.9 | 1 | 0.9 | 1 | 0.94 | |
| 8. Methodology able to answer the research question | Participants | 1 | 1 | 1 | 1 | 1 | 1 |
| Equipment | 1 | 1 | 1 | 1 | 1 | 1 | |
| Procedure | 1 | 1 | 1 | 1 | 1 | 1 | |
| Processing | 1 | 1 | 1 | 1 | 1 | 1 | |
| Statistics | 1 | 1 | 1 | 1 | 1 | 1 | |
| Subtotal | 1 | 1 | 1 | 1 | 1 | 1 | |
| 9. Reliability of the methodology is stated | Y = 1, N = 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10. Internal validity of the methodology was stated | Y = 1, N = 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 11 Research questions were answered adequately in the discussion | Y = 1, N = 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| 12. Key findings were supported by the results | Y = 1, N = 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| 13. Key findings were interpreted logically, supported by references | Y = 1, N = 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| 14. Clinical implications were stated | Y = 1; L = 0.5; N = 0 | 0 | 0.5 | 0 | 0 | 0 | 0.1 |
| Study average | 0.69 | 0.71 | 0.85 | 0.72 | 0.75 | 0.74 |
| Author | Gill and Hung [19] | Gill and Hung [20] | Silva et al. [21] | Gill [22] | Desrochers et al. [18] |
|---|---|---|---|---|---|
| Number of groups (n) | 2: | 2: | 2: | 4: | 2: |
| Normal BMI (between 5th and 85th percentile). (C) | Normal weight (between 5th and 85th percentile). (C) | Non-OB (<27 kg/m2). | Normal BMI (≥18.5 kg/m2 and <25 kg/m2). | Normal BMI (≥19 kg/m2 and ≤25 kg/m2). | |
| High BMI (children at or above 85th percentile and below 95th percentile were classified as OW; those above 95th percentile were classified as OB). (C) | OW/OB (children at or above 85th percentile and below 95th percentile were classified as OW; those above 95th percentile were classified as OB). (C) | OB (Z) (>27 kg/m2). | OW/Class I OB (C) (≥25 kg/m2 and <35 kg/m2). | OB BMI (≥30 kg/m2). (C) | |
| Class II OB (C) (≥35 kg/m2 and <40 kg/m2). | |||||
| Class III OB (C) (>40 kg/m2). | |||||
| Number of participants (n) | Non-OB: 10 | Non-OB: 10 | Non-OB: 27 | Normal BMI: 13 | Non-OB: 20 |
| OW/Class I OB: 18 | |||||
| OW/OB: 12 | OW/OB: 12 | OB: 40 | Class II OB: 16 | OB: 14 | |
| Class III OB: 20 | |||||
| Sex (F: female; M: male) (n) | Non-OB: F:6; M: 6 | All participants: F: 9; M: 13 | Non-OB: F: 27 | Normal BMI: F: 13 | Non-OB: F: 14; M: 6 |
| OW/Class I OB: F: 18 | |||||
| OW/OB: F:5; M: 7 | OB: F: 40 | Class II OB: F: 16 | OB: F: 12; M: 2 | ||
| Class III OB: F: 20 | |||||
| Exclusion criteria | Not reported. | Not reported. | (1) Diabetes and/or signs associated with neuropathy, (2) acute foot pain and deformities, (3) severe lower extremity trauma, and (4) coordination problems resulting from eye disorders. Scheduled to undergo knee surgery, having no significant cardiovascular, musculoskeletal, vestibular or other neurological disorders. These criteria were confirmed via participant reports and investigators’ observations. | Scheduled to undergo knee surgery, having no significant cardiovascular, musculoskeletal, vestibular or other neurological disorders. These criteria were confirmed via participant reports and investigators’ observations. | Not reported. |
| Inclusion criteria | Being free of intellectual impairment or physical conditions that precluded independent walking based on parents’ reports and investigators’ observations and being 4–13 years old. | Having normal cognitive abilities, no known physical conditions that would preclude independent walking, and being 4–13 years old. | Not reported. | All participants could walk without the aid of an assistive device. | All participants were free of neurological difficulties, had normal or corrected-to-normal vision, and could walk without assistive devices. |
| Age, mean (SD) (Range), years | Non-OB: 8.42 (1.00) (4.5–13). | All participants: 8.62 (0.93) (not reported). | Non-OB: 58.2 (4.8) (not reported). | Normal BMI: 33.2 (7.04) (not reported). | Non-OB: 45.55 (8.77) (35–64). |
| OW/Class I OB: 36.16 (12.76) (not reported). | |||||
| OW/OB: 8.58 (0.73) (6–13). | OB: 57.1 (4.7) (not reported). | Class II OB: 41.17 (5.89) (not reported) | OB: 50.36 (10.97) (35–66). | ||
| Class III OB: 42.72 (11.43) (not reported). | |||||
| Height, mean (SD) (Range), cm | Not reported. | Not reported. | Non-OB: 155.8 (5.2) (not reported). | Not reported. | Non-OB: 170.15 (8) (150–180). (X) |
| OB: 156.3 (4.5) (not reported). | OB: 168.83 (8.69) (155–184). (X) | ||||
| Body mass, mean (SD) (Range), kg | Not reported. | Not reported. | Non-OB: 58.4 (7.1) (not reported). | Not reported. | Non-OB: 69.36 (12.17) (47.20–86.20). (X) |
| OB: 73.1 (7.3) (not reported). | OB: 120.58 (20.13) (99.20–173.01). (X) | ||||
| BMI, mean (SD) (Range), kg/m2 | Non-OB: 15.85 (0.68) (11.65–18.35). (C) | Non-OB: 15.85 (0.68) (not reported). (C) | Non-OB: 24.0 (2.0) (not reported). | Normal BMI: 22.56 (1.61) (not reported). | Non-OB: 23.77 (2.53) (18.59–27.55). (C) |
| OW/Class I OB: 29.36 (3.19) (not reported). (C) | |||||
| OW/OB: 21.41 (1.31) (16.67–31.23). (C) | OW/OB: 21.85 (0.50) (not reported). (C) | OW/OB: 29.9 (2.5) (not reported). | Class II OB: 37.78 (1.42) (not reported). (C) | OB: 40.95 (5.46) (35.3–52.64). (C) | |
| Class III OB: 44.31 (4.24) (not reported). (C) |
| Author | Gill & Hung [19] | Gill & Hung [20] | Silva et al. [21] | Gill [22] | Desrochers et al. [18] |
|---|---|---|---|---|---|
| Task | Participants first walked once along a 406-cm-long walkway. In balance order, they walked and stepped over low, medium, and high obstacles. | Children walked along a 406-cm-long walkway and crossed low, medium, and high obstacles. | Walking straight ahead with or without stepping over an obstacle whose height was 30% of the leg length in a two-step protocol. | Participants walked down a 1600 cm walkway with a gait carpet (610 cm long × 89 cm wide) in the centre and crossed 3 obstacles of low, medium, and high height placed halfway down the path. | Participants walked along the GAITRite (488 cm long × 61 cm wide) walkway under five conditions. |
| Obstacle | A wooden dowel inserted into two 25-cm-high wooden towers at 4 cm (low obstacle), 11 cm (medium obstacle), and 16 cm (high obstacle). | A wooden dowel inserted into two 25-cm-high wooden towers at 4 cm (low obstacle), 11 cm (medium obstacle), and 16 cm (high obstacle). | Not reported. | The obstacles were created using a wooden dowel (121 cm long) and two rectangular towers (9 cm × 10 cm × 22 cm) with holes drilled at 4 cm, 8 cm, and 16 cm (low, medium, and high). | The obstacle was a wooden dowel suspended across the walkway that was inserted into holes in two wooden towers. Participants encountered small (4 cm), medium (8 cm), or large (16 cm) obstacles. |
| Expected/Unexpected | Expected. | Expected. | Expected. | Expected. | Expected. |
| Starting point | Not reported. | 203 cm from the obstacle. | Two-step protocol with the left leg as the leading limb during obstacle crossing. | 800 cm from the obstacle. | 244 cm from the obstacle. |
| Number of sessions | 1. | 1. | 1. | 1. | 1. |
| Number of conditions | 5: No obstacle = flat surface without obstacle (baseline initial and final trials). Low obstacle height (4 cm). Medium obstacle height (11 cm). High obstacle height (16 cm). | 5: No obstacle = flat surface without obstacle (baseline initial and final trial). Low obstacle height (4 cm). Medium obstacle height (11 cm). High obstacle height (16 cm). | 2: Straight ahead walking without obstacle = flat ground surface without obstacle. Straight ahead walking and stepping over an obstacle height of 30% of leg length. | 5: No obstacle = flat ground surface without obstacles (baseline initial and final trials). Low obstacle height (4 cm). Medium obstacle height (8 cm). High obstacle height (16 cm). | 5: No obstacle = flat ground surface without obstacles (baseline initial and final trials). Low obstacle height (4 cm). Medium obstacle height (8 cm). High obstacle height (16 cm). |
| Obstacle condition order | Initial and final overground trials. Obstacle conditions were counterbalanced. | Not reported. | Two-step protocol without obstacle. Two-step protocol with obstacle. | Initial and final overground trials Obstacle conditions were randomised. | Initial and final overground trials Obstacle conditions were counterbalanced. |
| Number of trials per condition | 5 for obstacle-crossing trials. 1 for baseline and final trials (no obstacle condition). | 5. | 5 valid trials. [y] | 5. | 5. |
| Walking speed | Self-selected pace. | Self-selected pace. | Self-selected pace. | Self-selected pace. | Self-selected pace. |
| Experimental condition | Single task. | Single task. | Single task. | Single task. | Single task. |
| Practice | Not reported. | 3 practice trials. | 10 min familiarisation period. | Not reported. | Not reported. |
| Author | Gill and Hung [19] | Gill and Hung [20] | Silva et al. [21] | Gill [22] | Desrochers et al. [18] |
|---|---|---|---|---|---|
| Parameters measured | Kinematics: Time from foot lift to maximum knee height, time from maximum knee height to foot contact, and maximum knee height. Ankle angles at foot contact to determine neutral (angles near 90 degrees) or dorsiflexed ankle positions (angles < 90 degrees) and sagittal knee and ankle angles at maximum knee height. Estimated variability of ankle positions at foot contact by calculating the coefficient of variation. | Kinematics: Maximum toe height for each leg during obstacle crossing; hip and knee angles in sagittal and frontal planes; vertical, anterior/posterior, and medial/lateral acceleration of centre of mass. | Kinematics: Plantar pressure parameters: relative foot temporal data for the initial contact, final contact, and duration of contact. | Kinematics: Velocity, percentage of gait cycle spent in swing and in stance, and coefficient of variation for each variable to obtain a measure of variability. | Kinematics: Gait velocity, step length and width, cadence, and single- and double-limb support during leading leg step across the obstacle. |
| Kinetics: Ground reaction force: normalised vertical, anterior/posterior, and medial/lateral ground reaction forces of both legs. | |||||
| Acquisition system | Vicon Nexus Model 1.4 motion capture system (120 Hz) and 41 reflective markers. | Whole-body plug-in-gait model of Vicon Nexus 1.51 (120 Hz) with 7 infrared cameras and 41 reflective markers. | Two Footscan platforms (100 × 40 cm, 8192 sensors; RSscan International, Olen, Belgium; 250 Hz). | Gait carpet (Protokinetics, LLC; Peekskill, NY, USA; 610 cm long × 89 cm wide; 120 Hz). | -GAITRite software and custom Matlab scripts (Mathworks, Inc., Natick, MA, USA) (488 cm long × 61 cm wide; 120 Hz). |
| Two AMTI OR6-6 force platforms (46 × 50 cm; 1200 Hz). |
| Gait Parameters | Number of Studies | Study | Between-Group Differences | Results (Mean ± SD or Median (IQR)) and Direction of Difference (↑↓) |
|---|---|---|---|---|
| Kinematics outcomes | ||||
| Velocity (cm/s) | 2 | Gill, 2019 | NW vs. OBI: p = 0.03 NW vs. OBII: p = 0.000002 NW vs. OBIII: p = 0.000000058 OBI vs. OBII: p = 0.018 OBI vs. OBIII: p = 0.001 | NW = 125.08 ± 1.98 OBI = 105.72 ± 3.08 (↓ 15.5% vs. NW) OBII = 91.46 ± 3.06 (↓ 26.9% vs. NW; ↓ 13.5% vs. OBI) OBIII = 85.46 ± 2.43 (↓ 31.7% vs. NW; ↓ 19.2% vs. OBI). |
| Desrochers et al., 2021 | p = 0.0001 (OB vs. C) | NW = 97.49 ± 6.14 OB = 67.53 ± 5.83 (↓ 30.7% vs. NW) | ||
| Leading-leg step length (cm) | 1 | Desrochers et al., 2021 | NW vs. OB: p = 0.01 | NW = 60.40 ± 0.37 OB = 51.94 ± 0.18 (↓ 14.0% vs. NW) |
| Leading-leg step width (cm) | 1 | Desrochers et al., 2021 | NW vs. OB: p = 0.01 | NW = 8.40 ± 0.21 OB = 11.54 ± 0.70 (↑ 37.4% vs. NW) |
| Leading-leg single-limb support (% of gait cycle) | 1 | Desrochers et al., 2021 | NW vs. OB: p = 0.001 | NW = 41.38 ± 1.16 OB = 38.87 ± 1.03 (↓ 6.1% vs. NW) |
| Double-limb support (% of gait cycle) | 1 | Desrochers et al., 2021 | NW vs. OB: p = 0.001 | NW = 8.90 ± 0.85 OB = 11.09 ± 0.96 (↑ 24.5% vs. NW) |
| Cadence (steps/min) | 1 | Desrochers et al., 2021 | NW vs. OB: p = 0.001 | NW = 104.46 ± 2.33 OB = 90.24 ± 3.07 (↓ 13.6% vs. NW) |
| Stance time (% of gait cycle) | 1 | Gill, 2019 | NW vs. OBI: p = 0.012 OBI vs. OBII: p = 0.029 | NW = 61.64 ± 1.71 OBI = 65.13 ± 0.35 (↑ 5.7% vs. NW; ↑ 4.6% vs. OBII) OBII = 62.83 ± 0.02 Low obstacle (4 cm): NW = 60.79 ± 6.97 OBI = 64.85 ± 2.31 (↑ 6.7% vs. NW) Medium obstacle (8 cm): NW = 60.52 ± 8.04 OBI = 65.01 ± 3.71 (↑ 7.4% vs. NW) |
| NW vs. OBI, low obstacle: p = 0.004 | ||||
| NW vs. OBI, medium obstacle: p = 0.007 | ||||
| Swing time (% of gait cycle) | 1 | Gill, 2019 | NW vs. OBI: p = 0.003 NW vs. OBII: p = 0.001 NW vs. OBIII: p = 0.00024 | C = 42.55 ± 0.85 OBI = 38.42 ± 0.85 (↓ 9.7% vs. NW) OBII = 37.72 ± 0.02 (↓ 11.4% vs. NW) OBIII = 37.14 ± 0.21 (↓ 12.7% vs. NW) |
| CV velocity | 1 | Gill, 2019 | NW vs. OBII: p = 0.00042 OBI vs. OBII: p = 0.00015 NW vs. OBIII: p = 0.000023 OBI vs. OBIII: p = 0.000006 | NW = 0.03 ± 0.01 OBI = 0.03 ± 0.01 OBII = 0.06 ± 0 (↑ 80% vs. NW and OBI) OBIII = 0.07 ± 0.01 (↑ 100% vs. NW and OBI) |
| CV stance time | 1 | Gill, 2019 | NS | |
| CV swing time | 1 | Gill, 2019 | NS | |
| Time from foot lift to maximum knee height (s) | 1 | Gill and Hung, 2012 | NW vs. OB, high obstacle: p = 0.04 | High obstacle (16 cm): NW = 0.08 ± 0.01 OB = 0.11 ± 0.01 (↑ 37.5% vs. NW) |
| NW vs. OB, low obstacle: p = 0.41 | ||||
| NW vs. OB, medium obstacle: p = 0.31 | ||||
| Time from maximum knee height to foot contact (s) | 1 | Gill and Hung, 2012 | NW vs. OB, high obstacle: p = 0.04 | High obstacle (16 cm): NW = 0.0011 ± 0.001 OB = 0.0006 ± 0.0005 (↓ 45.5% vs. NW) |
| NW vs. OB, low obstacle: p = 0.13 | ||||
| NW vs. OB, medium obstacle: p = 0.96 | ||||
| Maximum knee height | 1 | Gill and Hung, 2012 | C vs. OB: p = 0.57 | |
| Ankle angle at foot contact (°) | 1 | Gill and Hung, 2012 | C vs. OB, low obstacle: p = 0.04 | Low obstacle (4 cm): NW = 99.24 ± 6.18 OB = 79.90 ± 6.18 (↓ 19.5% vs. NW) |
| NW vs. OB, medium obstacle: p = 0.07 | ||||
| NW vs. OB, high obstacle: p = 0.89 | ||||
| Sagittal ankle angle at maximum knee height (°) | 1 | Gill and Hung, 2012 | NW vs. OB: p = 0.65 | |
| Sagittal knee angle at maximum knee height (°) | 1 | Gill and Hung, 2012 | NW vs. OB: p = 0.18 | |
| Leading-leg toe clearance (cm) | 1 | Gill and Hung, 2014 | NS | |
| Trailing-leg toe clearance (cm) | 1 | Gill and Hung, 2014 | NW, high low obstacle: p = 0.02 | Low obstacle (4 cm): NW = 13.73 ± 1.47 O = 23.13 ± 1.53 (↑ 38% vs. high obstacle) |
| OB, low vs. high obstacle: p = 0.01 | High obstacle (16 cm): NW = 18.38 ± 1.53 (↑ 33.9% vs. low obstacle) OB = 16.76 ± 1.59 | |||
| Leading-leg hip angles at maximum knee height in frontal plane (°) | 1 | Gill and Hung, 2014 | OB, high vs. medium and low obstacles: p = 0.02 | Low obstacle (4 cm): OB = 47.28 ± 0.47 |
| Medium obstacle (11 cm): OB = 50.28 ± 0.52 | ||||
| No other effects were observed | High obstacle (16 cm): OB = 66.75 ± 0.57 (↑ 32.8% and 41.18% vs. medium and low obstacles, respectively) | |||
| Trailing-leg hip angles at maximum knee height in frontal plane (°) | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed (p > 0.05). | |
| Hip angles at maximum knee height in sagittal plane (°) | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed for both legs (p > 0.05). | |
| Trailing-leg knee angles at maximum knee height in sagittal plane (°) | 1 | Gill and Hung, 2014 | NW vs. OB, high obstacle: p = 0.04 | Low obstacle (4 cm): NW = 6.99 ± 0.66 OB = 11.09 ± 1.16 (↑ 58.7% vs. NW) |
| NW vs. OB, low obstacle: p = 0.04 | High obstacle (16 cm): NW = 4.64 ± 0.64 OB = 12.02 ± 1.05 (↑ 159.1% vs. NW) | |||
| No other effects were observed. | ||||
| COM acceleration in anterior/posterior direction at maximum knee height of leading leg during crossing | 1 | Gill and Hung, 2014 | NW vs. OB, low obstacle: p = 0.006 No other effects were observed. | Low obstacle (4 cm): C = 0.63 ± 0.08 OB = 1.05 ± 0.05 (↑ 66.7% vs. NW) |
| COM acceleration in anterior/posterior direction at maximum knee height of trailing leg during crossing | 1 | Gill and Hung, 2014 | NW vs. OB, low obstacle: p = 0.01 | Low obstacle (4 cm): NW = 0.66 ± 0.12 OB = 1.02 ± 0.12 (↑ 54.5% vs. NW; ↑ 45.7% and 82.1% vs. medium and high obstacles, respectively) |
| Medium obstacle (11 cm): NW = 0.83 ± 0.06 OB = 0.70 ± 0.06 | ||||
| OB, low vs. medium and high obstacles: p = 0.01 | High obstacle (16 cm): NW = 0.73 ± 0.09 OB = 0.56 ± 0.09 | |||
| COM acceleration in medial/lateral direction at maximum knee height | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed for both legs (p > 0.05). | |
| COM acceleration in vertical direction at maximum knee height | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed for both legs (p > 0.05). | |
| Duration of contact of HL, HM, MF, M5, M4, M3, M2, M1, T2-5, T1 of leading and trailing leg (ms) | 1 | Silva et al., 2018 | No difference between OB and C for any area for both legs. | |
| Kinetics outcomes | ||||
| Trailing-leg normalised, anterior/posterior ground reaction forces at maximum knee height of leading leg during crossing (N/kg) | 1 | Gill and Hung, 2014 | OB, low vs. medium and high obstacles: p = 0.001 | Low obstacle (4 cm): NW = 0.17 ± 0.06 OB = 0.66 ± 0.02 (↑266.7%, and 100% vs. medium and high obstacles, respectively) |
| NW, high vs. medium and low obstacles: p = 0.001 | Medium obstacle (11 cm): NW = 0.29 ± 0.03 OB = 0.18 ± 0.08 | |||
| No other effects were observed. | High obstacle (16 cm): NW = 0.33 ± 0.04 (↑ 94,1%, and 13.8% vs. low and medium obstacles, respectively) OB = 0.33 ± 0.12 | |||
| Leading-leg normalised, anterior/posterior ground reaction forces at maximum knee height of trailing leg during crossing (N/kg) | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed (p > 0.05). | |
| Trailing-leg normalised, medial/lateral ground reaction forces at maximum knee height of leading leg during crossing (N/kg) | 1 | Gill and Hung, 2014 | OB, high vs. medium obstacle: p = 0.01 | Medium obstacle (11 cm): NW = 0.19 ± 0.06 OB = 0.04 ± 0.02 |
| No other effects were observed. | High obstacle (16 cm): NW = 0.12 ± 0.07 OB = 0.19 ± 0.05 (↑ 375% vs. medium obstacle) | |||
| Leading-leg normalised, medial/lateral ground reaction forces at maximum knee height of trailing leg during crossing (N/kg) | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed (p > 0.05). | |
| Trailing-leg normalised, vertical ground reaction forces at maximum knee height of leading leg during crossing (N/kg) | 1 | Gill and Hung, 2014 | OB, high vs. medium obstacle: p = 0.05 | Low obstacle (4 cm): NW = 1.38 ± 0.27 OB = 1.99 ± 0.19 |
| NW, medium vs. low obstacle: p = 0.05 | Medium obstacle (11 cm): NW = 2.14 ± 0.22 (↑ 55.1% vs. low obstacle) OB = 1.58 ± 0.29 | |||
| No other effects were observed. | High obstacle (16 cm): NW = 1.92 ± 0.26 OB = 2.23 ± 0.24 (↑ 41.1% vs. medium obstacle) | |||
| Leading-leg normalised, vertical ground reaction forces at maximum knee height of leading leg during crossing (N/kg) | 1 | Gill and Hung, 2014 | No BMI or BMI*condition effects were observed (p > 0.05). | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chardon, M.; Barbieri, F.A.; Penedo, T.; Santos, P.C.R.; Vuillerme, N. A Systematic Review of the Influence of Overweight and Obesity across the Lifespan on Obstacle Crossing during Walking. Int. J. Environ. Res. Public Health 2023, 20, 5931. https://doi.org/10.3390/ijerph20115931
Chardon M, Barbieri FA, Penedo T, Santos PCR, Vuillerme N. A Systematic Review of the Influence of Overweight and Obesity across the Lifespan on Obstacle Crossing during Walking. International Journal of Environmental Research and Public Health. 2023; 20(11):5931. https://doi.org/10.3390/ijerph20115931
Chicago/Turabian StyleChardon, Matthias, Fabio A. Barbieri, Tiago Penedo, Paulo C. R. Santos, and Nicolas Vuillerme. 2023. "A Systematic Review of the Influence of Overweight and Obesity across the Lifespan on Obstacle Crossing during Walking" International Journal of Environmental Research and Public Health 20, no. 11: 5931. https://doi.org/10.3390/ijerph20115931
APA StyleChardon, M., Barbieri, F. A., Penedo, T., Santos, P. C. R., & Vuillerme, N. (2023). A Systematic Review of the Influence of Overweight and Obesity across the Lifespan on Obstacle Crossing during Walking. International Journal of Environmental Research and Public Health, 20(11), 5931. https://doi.org/10.3390/ijerph20115931







