Gender Felt Pressure, Affective Domains, and Mental Health Outcomes among Transgender and Gender Diverse (TGD) Children and Adolescents: A Systematic Review with Developmental and Clinical Implications
Abstract
1. Introduction
1.1. Definitional Issues
1.2. Routes to Gender Affirmation
1.3. TGD Youth’s Mental Health and Emotional or Affective Functioning
1.4. TGD Youth, Gender Pressure, and Minority Stress
1.5. The Present Work
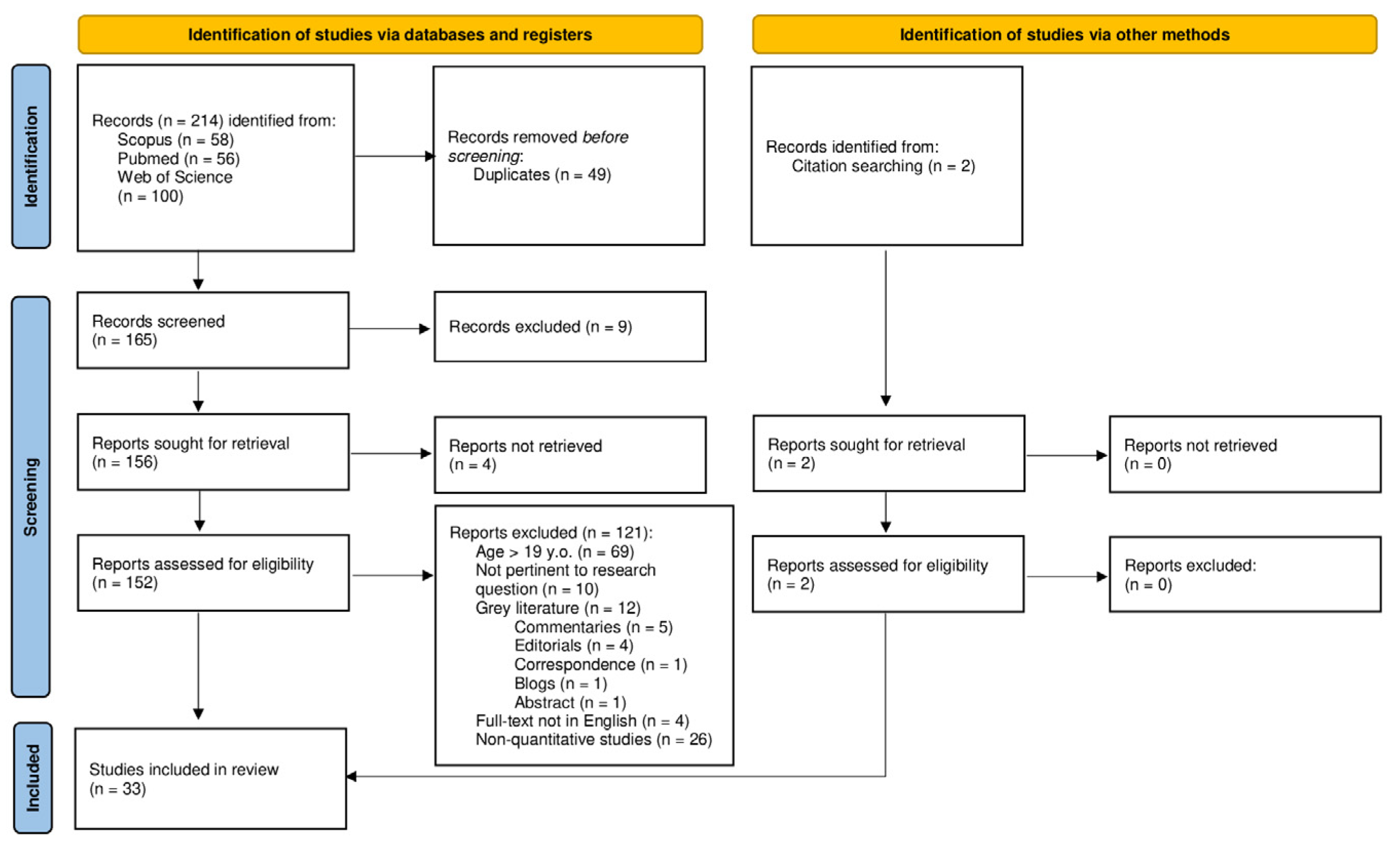
2. Methodology
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Selection Process
2.4. Data Extraction Process
2.5. Quality Assessment
3. Results
3.1. Mental Health Outcomes
3.2. Types of Respondents
3.3. Depression and Anxiety
3.4. Emotional and Behavioral Problems
3.5. Trauma and Victimization
3.6. Family-Related Factors
3.7. TGD and ASD
3.8. External Factors
3.9. Resilience Factors
3.10. Quality Assessment
4. Discussion
4.1. Mental Health Problems among TGD Individuals: The High Prevalence of Depression and Anxiety
4.2. Gender Felt Pressure and TGD Transition
4.3. Developmental Challenges of Children and Adolescents
4.4. Minority Stress and Trauma
4.5. External and Cultural Factors
4.6. Internalizing Symptoms and Emotion Regulation
4.7. The Role of Social Support
4.8. Gender Role Discrepancy Stress
4.9. Sex Trading and Sexual Exploitation
4.10. Developmental Trajectories of TGD Children and Adolescents
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
List of Abbreviations
| AC | appearance congruence |
| ACEs | adverse childhood experiences |
| ADHD | attention deficit and/or hyperactivity disorder |
| ASD | autism spectrum disorder |
| CBCL | child behavior checklist |
| CD | conduct disorder |
| DSM | diagnostic and statistical manual of mental disorders |
| GAD | generalized anxiety disorder |
| GRD | gender role discrepancy |
| GSAs | gay-straight alliances or gender-sexuality alliances |
| IT | internalized transphobia |
| LGBT(Q) | lesbian, gay, bisexual, transgender, (queer) |
| MDD | major depressive disorder |
| MDS | masculine discrepancy stress |
| MST | minority stress theory |
| PTSD | post-traumatic stress disorder |
| TGD | transgender and gender diverse |
| YSR | Youth Self Report |
References
- Kroger, J. Why is identity achievement so elusive? Identity 2007, 7, 331–348. [Google Scholar] [CrossRef]
- Steensma, T.D.; Kreukels, B.P.; de Vries, A.L.; Cohen-Kettenis, P.T. Gender identity development in adolescence. Horm. Behav. 2013, 64, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Hidalgo, M.A.; Leibowitz, S.; Leininger, J.; Simons, L.; Finlayson, C.; Garofalo, R. Multidisciplinary care for gender-diverse youth: A narrative review and unique model of gender-affirming care. Transgender Health 2016, 1, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Leibowitz, S.F.; Spack, N.P. The development of a gender identity psychosocial clinic: Treatment issues, logistical considerations, interdisciplinary cooperation, and future initiatives. Child Adolesc. Psychiatr. Clin. N. Am. 2011, 20, 701–724. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, J.; Committee on Psychosocial Aspects of Child and Family Health; Committee on Adolescence; Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents. Pediatrics 2018, 142, e20182162. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Ristori, J.; Steensma, T.D. Gender dysphoria in childhood. Int. Rev. Psychiatry 2016, 28, 13–20. [Google Scholar] [CrossRef]
- McPhate, L.; Williams, K.; Vance, A.; Winther, J.; Pang, K.; May, T. Gender variance in children and adolescents with neurodevelopmental and psychiatric conditions from Australia. Arch. Sex. Behav. 2021, 50, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Lowry, R.; Johns, M.M.; Gordon, A.R.; Austin, S.B.; Robin, L.E.; Kann, L.K. Nonconforming gender expression and associated mental distress and substance use among high school students. JAMA Pediatr. 2018, 172, 1020–1028. [Google Scholar] [CrossRef]
- Steensma, T.D.; McGuire, J.K.; Kreukels, B.P.; Beekman, A.J.; Cohen-Kettenis, P.T. Factors associated with desistence and persistence of childhood gender dysphoria: A quantitative follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 582–590. [Google Scholar] [CrossRef]
- Turban, J.L. Transgender youth: The building evidence base for early social transition. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 101–102. [Google Scholar] [CrossRef]
- Chodzen, G.; Hidalgo, M.A.; Chen, D.; Garofalo, R. Minority stress factors associated with depression and anxiety among transgender and gender-nonconforming youth. J. Adolesc. Health 2018, 64, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Kozee, H.B.; Tylka, T.L.; Bauerband, L.A. Measuring transgender individuals’ comfort with gender identity and appearance: Development and validation of the Transgender Congruence Scale. Psychol. Women Q. 2012, 36, 179–196. [Google Scholar] [CrossRef]
- Durwood, L.; McLaughlin, K.A.; Olson, K.R. Mental health and self-worth in socially transitioned transgender youth. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Lev, A.; Sennott, S. Clinical work with LGBTQ parents and prospective parents. In LGBTQ-Parent Families; Goldberg, A., Allen, K., Eds.; Springer: Cham, Switzerland, 2020; pp. 383–404. [Google Scholar] [CrossRef]
- Berli, J.U.; Knudson, G.; Fraser, L.; Tangpricha, V.; Ettner, R.; Ettner, F.M.; Safer, J.D.; Graham, J.; Monstrey, S.; Schechter, L. What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: A review. JAMA Surg. 2017, 152, 394–400. [Google Scholar] [CrossRef]
- Jackman, K.B.; Dolezal, C.; Bockting, W.O. Generational differences in internalized transnegativity and psychological distress among feminine spectrum transgender people. LGBT Health 2018, 5, 54–60. [Google Scholar] [CrossRef]
- Aitken, M.; VanderLaan, D.P.; Wasserman, L.; Stojanovski, S.; Zucker, K.J. Self-harm and suicidality in children referred for gender dysphoria. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 513–520. [Google Scholar] [CrossRef]
- Connolly, M.D.; Zervos, M.J.; Barone, C.J.; Johnson, C.C.; Joseph, C.L. The mental health of transgender youth: Advances in understanding. J. Adolesc. Health 2016, 59, 489–495. [Google Scholar] [CrossRef]
- Perez-Brumer, A.; Day, J.K.; Russell, S.T.; Hatzenbuehler, M.L. Prevalence and correlates of suicidal ideation among transgender youth in California: Findings from a representative, population-based sample of high school students. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 739–746. [Google Scholar] [CrossRef]
- Peterson, C.M.; Matthews, A.; Copps-Smith, E.; Conard, L.A. Suicidality, self-harm, and body dissatisfaction in transgender adolescents and emerging adults with gender dysphoria. Suicide Life-Threat. Behav. 2017, 47, 475–482. [Google Scholar] [CrossRef]
- Grossman, A.H.; D’Augelli, A.R. Transgender youth and life-threatening behaviors. Suicide Life-Threat. Behav. 2007, 37, 527–537. [Google Scholar] [CrossRef]
- Horwitz, A.G.; Berona, J.; Czyz, E.K.; Yeguez, C.E.; King, C.A. Positive and negative expectations of hopelessness as longitudinal predictors of depression, suicidal ideation, and suicidal behavior in high-risk adolescents. Suicide Life-Threat. Behav. 2017, 47, 168–176. [Google Scholar] [CrossRef]
- Kosnes, L.; Whelan, R.; O’Donovan, A.; McHugh, L.A. Implicit measurement of positive and negative future thinking as a predictor of depressive symptoms and hopelessness. Conscious. Cogn. 2013, 22, 898–912. [Google Scholar] [CrossRef]
- De Vries, A.L.; Cohen-Kettenis, P.T. Clinical management of gender dysphoria in children and adolescents: The Dutch approach. J. Homosex. 2012, 59, 301–320. [Google Scholar] [CrossRef]
- Reisner, S.L.; Greytak, E.A.; Parsons, J.T.; Ybarra, M.L. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. J. Sex Res. 2014, 52, 243–256. [Google Scholar] [CrossRef]
- Hoy-Ellis, C.P. Minority stress and mental health: A review of the literature. J. Homosex. 2021, 1–25. [Google Scholar] [CrossRef]
- Meyer, I.H. Prejudice, social stress, and mental health in lesbian, gay and bisexual populations: Conceptual issues and research evidence. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef]
- Meyer, I.H. Prejudice and discrimination as social stressors. In The Health of Sexual Minorities: Public Health Perspectives on Lesbian, Gay, Bisexual, and Transgender Populations; Meyer, I.H., Northridge, M.E., Eds.; Springer Science + Business Media: New York, NY, USA, 2007; pp. 242–267. [Google Scholar] [CrossRef]
- Scandurra, C.; Mezza, F.; Bochicchio, V.; Valerio, P.; Amodeo, A.L. La salute degli anziani LGBT dalla prospettiva del minority stress. Rassegna della letteratura e raccomandazioni di ricerca [LGBT elders health from the minority stress perspective. Literature review & research recommendations]. Psicol. Della Salut. 2017, 2, 70–96. [Google Scholar] [CrossRef]
- Meyer, I.H. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 209–213. [Google Scholar] [CrossRef]
- Frost, D.M.; Meyer, I.H. Measuring community connectedness among diverse sexual minority populations. J. Sex Res. 2012, 49, 36–49. [Google Scholar] [CrossRef]
- De Lira, A.N.; de Morais, N.A. Resilience in lesbian, gay, and bisexual (LGB) populations: An integrative literature review. Sex. Res. Soc. Policy 2018, 15, 272–282. [Google Scholar] [CrossRef]
- Bockting, W.O.; Miner, M.H.; Swinburne Romine, R.E.; Hamilton, A.; Coleman, E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am. J. Public Health 2013, 103, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Delozier, A.M.; Kamody, R.C.; Rodgers, S.; Chen, D. Health disparities in transgender and gender expansive adolescents: A topical review from a minority stress framework. J. Pediatr. Psychol. 2020, 45, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Griffin, J.A.; Casanova, T.N.; Eldridge-Smith, E.D.; Stepleman, L.M. Gender minority stress and health perceptions among transgender individuals in a small metropolitan Southeastern region of the United States. Transgender Health 2019, 4, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.; Butler, C.; Cooper, K. Gender minority stress in trans and gender diverse adolescents and young people. Clin. Child Psychol. Psychiatry 2021, 26, 1182–1195. [Google Scholar] [CrossRef]
- Scandurra, C.; Vitelli, R.; Maldonato, N.M.; Valerio, P.; Bochicchio, V. A qualitative study on minority stress subjectively experienced by transgender and gender nonconforming people in Italy. Sexologies 2019, 28, e61–e71. [Google Scholar] [CrossRef]
- Testa, R.J.; Michaels, M.S.; Bliss, W.; Rogers, M.L.; Balsam, K.F.; Joiner, T. Suicidal ideation in transgender people: Gender minority stress and interpersonal theory factors. J. Abnorm. Psychol. 2017, 126, 125–136. [Google Scholar] [CrossRef]
- Valentine, S.E.; Shipherd, J.C. A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clin. Psychol. Rev. 2018, 66, 24–38. [Google Scholar] [CrossRef]
- Testa, R.J.; Habarth, J.; Peta, J.; Balsam, K.; Bockting, W. Development of the Gender Minority Stress and Resilience Measure. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 65–77. [Google Scholar] [CrossRef]
- Goldberg, A.E.; Kuvalanka, K.A.; Budge, S.L.; Benz, M.B.; Smith, J.Z. Health care experiences of transgender binary and nonbinary university students. Couns. Psychol. 2019, 47, 59–97. [Google Scholar] [CrossRef]
- Bockting, W.O.; Miner, M.H.; Swinburne Romine, R.E.; Dolezal, C.; Robinson, B.; Rosser, B.; Coleman, E. The Transgender Identity Survey: A measure of internalized transphobia. LGBT Health 2020, 7, 15–27. [Google Scholar] [CrossRef]
- Rood, B.A.; Reisner, S.L.; Puckett, J.A.; Surace, F.I.; Berman, A.K.; Pantalone, D.W. Internalized transphobia: Exploring perceptions of social messages in transgender and gender-nonconforming adults. Int. J. Transgenderism 2017, 18, 411–4266. [Google Scholar] [CrossRef]
- Scandurra, C.; Bochicchio, V.; Dolce, P.; Caravà, C.; Vitelli, R.; Testa, R.J.; Balsam, K.F. The Italian validation of the Gender Minority Stress and Resilience measure. Psychol. Sex. Orientat. Gend. Divers. 2020, 7, 208–221. [Google Scholar] [CrossRef]
- Matsuno, E.; Israel, T. Psychological interventions promoting resilience among transgender individuals: Transgender Resilience Intervention Model (TRIM). Couns. Psychol. 2018, 46, 632–655. [Google Scholar] [CrossRef]
- Mackie, G.; Lambert, K.; Patlamazoglou, L. The mental health of transgender young people in secondary schools: A scoping review. Sch. Ment. Health 2021, 13, 13–27. [Google Scholar] [CrossRef]
- Caldarera, A.M.; Vitiello, B.; Turcich, C.; Bechis, D.; Baietto, C. The association of attachment, mentalization and reflective functioning with mental health in gender diverse children and adolescents: A systematic review. Clin. Child Psychol. Psychiatry 2022, 27, 13591045221075527. [Google Scholar] [CrossRef]
- Lekwauwa, R.; Funaro, M.C.; Doolittle, B. Systematic review: The relationship between religion, spirituality and mental health in adolescents who identify as transgender. J. Gay Lesbian Ment. Health 2022, 1–18. [Google Scholar] [CrossRef]
- Tankersley, A.P.; Grafsky, E.L.; Dike, J.; Jones, R.T. Risk and resilience factors for mental health among transgender and gender nonconforming (TGD) youth: A systematic review. Clin. Child Fam. Psychol. Rev. 2021, 24, 183–206. [Google Scholar] [CrossRef]
- Egan, S.K.; Perry, D.G. Gender identity: A multidimensional analysis with implications for psychosocial adjustment. Dev. Psychol. 2001, 37, 451–463. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Becerra-Culqui, T.A.; Liu, Y.; Nash, R.; Cromwell, L.; Flanders, W.D.; Getahun, D.; Giammattei, S.V.; Hunkeler, E.M.; Lash, T.L.; Millman, A.; et al. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics 2018, 141, e20173845. [Google Scholar] [CrossRef]
- Bluth, K.; Lathren, C.; Clepper-Faith, M.; Larson, L.M.; Ogunbamowo, D.O.; Pflum, S. Improving mental health among transgender adolescents: Implementing mindful self-compassion for teens. J. Adolesc. Res. 2021, 07435584211062126. [Google Scholar] [CrossRef]
- Cheung, D.H.; Boonmongkon, P.; Ojanen, T.T.; Damri, T.; Samoh, N.; Cholratana, M.; Ratchadapunnathikul, C.; Gilman, S.E.; Sass, J.; Guadamuz, T.E. Peer victimisation and depression among gender conforming and non-conforming Thai adolescents. Cult. Health Sex. 2020, 22, 808–821. [Google Scholar] [CrossRef] [PubMed]
- Craig, S.L.; Austin, A.; Levenson, J.; Leung, V.; Eaton, A.D.; D’Souza, S.A. Frequencies and patterns of adverse childhood events in LGBTQ+ youth. Child Abus. Negl. 2020, 107, 104623. [Google Scholar] [CrossRef]
- Durwood, L.; Eisner, L.; Fladeboe, K.; Ji, C.G.; Barney, S.; McLaughlin, K.A.; Olson, K.R. Social support and internalizing psychopathology in transgender youth. J. Youth Adolesc. 2021, 50, 841–854. [Google Scholar] [CrossRef]
- Eisenberg, M.E.; Gower, A.L.; McMorris, B.J.; Rider, G.N.; Shea, G.; Coleman, E. Risk and protective factors in the lives of transgender/gender nonconforming adolescents. J. Adolesc. Health 2017, 61, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.B.; Menvielle, E.; Sica, K.M.; Johnson, A. An affirmative intervention for families with gender variant children: Parental ratings of child mental health and gender. J. Sex Marital. Ther. 2010, 36, 6–23. [Google Scholar] [CrossRef] [PubMed]
- Katz-Wise, S.L.; Ehrensaft, D.; Vetters, R.; Forcier, M.; Austin, S.B. Family functioning and mental health of transgender and gender-nonconforming youth in the Trans Teen and Family Narratives Project. J. Sex Res. 2018, 55, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Kolbuck, V.D.; Muldoon, A.L.; Rychlik, K.; Hidalgo, M.A.; Chen, D. Psychological functioning, parenting stress, and parental support among clinic-referred prepubertal gender expansive children. Clin. Pract. Pediatr. Psychol. 2019, 7, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Kuper, L.E.; Mathews, S.; Lau, M. Baseline mental health and psychosocial functioning of transgender adolescents seeking gender-affirming hormone therapy. J. Dev. Behav. Pediatr. 2019, 40, 589–596. [Google Scholar] [CrossRef]
- Mahfouda, S.; Panos, C.; Whitehouse, A.; Thomas, C.S.; Maybery, M.; Strauss, P.; Zepf, F.D.; O’Donovan, A.; van Hall, H.W.; Saunders, L.A.; et al. Mental health correlates of autism spectrum disorder in gender diverse young people: Evidence from a specialised child and adolescent gender clinic in Australia. J. Clin. Med. 2019, 8, 1503. [Google Scholar] [CrossRef]
- Moyer, D.N.; Connelly, K.J.; Holley, A.L. Using the PHQ-9 and GAD-7 to screen for acute distress in transgender youth: Findings from a pediatric endocrinology clinic. J. Pediatr. Endocrinol. Metab. 2019, 32, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Munroe, C.; Clerkin, E.M.; Kuvalanka, K.A. The impact of peer and family functioning on transgender and gender-diverse children’s mental health. J. Child Fam. Stud. 2020, 29, 2080–2089. [Google Scholar] [CrossRef] [PubMed]
- Nahata, L.; Quinn, G.P.; Caltabellotta, N.M.; Tishelman, A.C. Mental health concerns and insurance denials among transgender adolescents. LGBT Health 2017, 4, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Nic Rider, G.; McMorris, B.J.; Brown, C.; Eisenberg, M.E.; Gower, A.L.; Johnston-Goodstar, K.; Filoteo, M.; Singerhouse, E.; Martin, L. Mental health and protective factors for transgender and gender-diverse youths who trade sex: A Minnesota statewide school-based study, 2019. Am. J. Public Health 2022, 112, 499–508. [Google Scholar] [CrossRef]
- Olson, K.R.; Durwood, L.; DeMeules, M.; McLaughlin, K.A. Mental health of transgender children who are supported in their identities. Pediatrics 2016, 137, e20153223. [Google Scholar] [CrossRef]
- Parodi, K.B.; Holt, M.K.; Green, J.G.; Katz-Wise, S.L.; Shah, T.N.; Kraus, A.D.; Xuan, Z. Associations between school-related factors and mental health among transgender and gender diverse youth. J. Sch. Psychol. 2022, 90, 135–149. [Google Scholar] [CrossRef]
- Perl, L.; Oren, A.; Klein, Z.; Shechner, T. Effects of the COVID-19 pandemic on transgender and gender non-conforming adolescents’ mental health. Psychiatry Res. 2021, 302, 114042. [Google Scholar] [CrossRef]
- Reidy, D.E.; Smith-Darden, J.P.; Vivolo-Kantor, A.M.; Malone, C.A.; Kernsmith, P.D. Masculine discrepancy stress and psychosocial maladjustment: Implications for behavioral and mental health of adolescent boys. Psychol. Men Masc. 2018, 19, 560–569. [Google Scholar] [CrossRef]
- Russell, D.H.; Hoq, M.; Coghill, D.; Pang, K.C. Prevalence of mental health problems in transgender children aged 9 to 10 years in the US, 2018. JAMA Netw. Open 2022, 5, e2223389. [Google Scholar] [CrossRef]
- Shumer, D.E.; Roberts, A.L.; Reisner, S.L.; Lyall, K.; Austin, S.B. Brief report: Autistic traits in mothers and children associated with child’s gender nonconformity. J. Autism Dev. Disord. 2015, 45, 1489–1494. [Google Scholar] [CrossRef]
- Stewart, S.L.; Van Dyke, J.N.; Poss, J.W. Examining the mental health presentations of treatment-seeking transgender and gender nonconforming (TGD) youth. Child Psychiatry Hum. Dev. 2021, 1–11. [Google Scholar] [CrossRef]
- Turban, J.L.; King, D.; Li, J.J.; Keuroghlian, A.S. Timing of social transition for transgender and gender diverse youth, K-12 harassment, and adult mental health outcomes. J. Adolesc. Health 2021, 69, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Vance, S.R., Jr.; Boyer, C.B.; Glidden, D.V.; Sevelius, J. Mental health and psychosocial risk and protective factors among Black and Latinx transgender youth compared with peers. JAMA Netw. Open 2021, 4, e213256. [Google Scholar] [CrossRef] [PubMed]
- VanderLaan, D.P.; Santarossa, A.; Nabbijohn, A.N.; Wood, H.; Owen-Anderson, A.; Zucker, K.J. Separation anxiety among birth-assigned male children in a specialty gender identity service. Eur. Child Adolesc. Psychiatry 2017, 27, 89–98. [Google Scholar] [CrossRef]
- Van der Miesen, A.I.; Nabbijohn, A.N.; Santarossa, A.; VanderLaan, D.P. Behavioral and emotional problems in gender-nonconforming children: A Canadian community-based study. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 491–499. [Google Scholar] [CrossRef]
- Wang, Y.; Yu, H.; Yang, Y.; Drescher, J.; Li, R.; Yin, W.; Yu, R.; Wang, S.; Deng, W.; Jia, Q.; et al. Mental health status of cisgender and gender-diverse secondary school students in China. JAMA Netw. Open 2020, 3, e2022796. [Google Scholar] [CrossRef]
- Watson, R.J.; Fish, J.N.; Denary, W.; Caba, A.; Cunningham, C.; Eaton, L.A. LGBTQ state policies: A lever for reducing SGM youth substance use and bullying. Drug Alcohol Depend. 2021, 221, 108659. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Edelbrock, C.S. Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monogr. Soc. Res. Child Dev. 1981, 46, 1–82. [Google Scholar] [CrossRef]
- Achenbach, T.M. Manual for The Child Behavior Checklist/4-18 and 1991 Profile; Department of Psychiatry, University of Vermont: Burlington, VT, USA, 1991. [Google Scholar]
- Scandurra, C.; Carbone, A.; Baiocco, R.; Mezzalira, S.; Maldonato, N.M.; Bochicchio, V. Gender identity milestones, minority stress and mental health in three generational cohorts of Italian binary and nonbinary transgender people. Int. J. Environ. Res. Public Health 2021, 18, 9057. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef]
- Boullier, M.; Blair, M. Adverse childhood experiences. Paediatr. Child Health 2018, 28, 132–137. [Google Scholar] [CrossRef]
- Cheong, E.V.; Sinnott, C.; Dahly, D.; Kearney, P.M. Adverse childhood experiences (ACEs) and later-life depression: Perceived social support as a potential protective factor. BMJ Open 2017, 7, e013228. [Google Scholar] [CrossRef] [PubMed]
- Reiser, S.; Power, H.; Wright, K. Examining the relationships between childhood abuse history, attachment, and health anxiety. J. Health Psychol. 2019, 26, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Schneeberger, A.R.; Dietl, M.F.; Muenzenmaier, K.H.; Huber, C.G.; Lang, U.E. Stressful childhood experiences and health outcomes in sexual minority populations: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1427–1445. [Google Scholar] [CrossRef]
- Elze, D.E. The lives of lesbian, gay, bisexual, and transgender people: A trauma-informed and human rights perspective. In Trauma and Human Rights; Butler, L., Critelli, F., Carello, J., Eds.; Palgrave Macmillan: Cham, Switzerland, 2019; pp. 179–206. [Google Scholar] [CrossRef]
- Clark, T.C.; Lucassen, M.F.; Bullen, P.; Denny, S.J.; Fleming, T.M.; Robinson, E.M.; Rossen, F.V. The health and well-being of transgender high school students: Results from the New Zealand adolescent health survey (Youth’12). J. Adolesc. Health 2014, 55, 93–99. [Google Scholar] [CrossRef]
- Bluth, K.; Gaylord, S.A.; Campo, R.A.; Mullarkey, M.C.; Hobbs, L. Making friends with yourself: A mixed methods pilot study of a mindful selfcompassion program for adolescents. Mindfulness 2016, 7, 479–492. [Google Scholar] [CrossRef]
- Bluth, K.; Eisenlohr-Moul, T.A. Response to a mindful self-compassion intervention in teens: A within-person association of mindfulness, self-compassion, and emotional well-being outcomes. J. Adolesc. 2017, 57, 108–118. [Google Scholar] [CrossRef]
- Donovan, E.; Bluth, K.; Scott, H.; Mohammed, M.; Cousineau, T.M. Feasibility and acceptability of implementing the making friends with yourself intervention on a college campus. J. Am. Coll. Health 2021, 1–8. [Google Scholar] [CrossRef]
- Carver, P.R.; Yunger, J.L.; Perry, D.G. Gender identity and adjustment in middle childhood. Sex Roles 2003, 49, 95–109. [Google Scholar] [CrossRef]
- Yunger, J.L.; Carver, P.R.; Perry, D.G. Does Gender Identity Influence Children’s Psychological Well-Being? Dev. Psychol. 2004, 40, 572–582. [Google Scholar] [CrossRef]
- Menon, M. Does Felt gender compatibility mediate influences of self-perceived gender nonconformity on early adolescents’ psychosocial adjustment? Child Dev. 2011, 82, 1152–1162. [Google Scholar] [CrossRef] [PubMed]
- Menon, M. Multidimensional gender identity and gender-typed relationship styles in adolescence. Sex Roles 2017, 76, 579–591. [Google Scholar] [CrossRef]
- Corby, B.C.; Hodges, E.V.; Perry, D.G. Gender identity and adjustment in Black, Hispanic, and White preadolescents. Dev. Psychol. 2007, 43, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Bochicchio, V.; Perillo, P.; Valenti, A.; Chello, F.; Amodeo, A.L.; Valerio, P.; Scandurra, C. Pre-service teachers’ approaches to gender-nonconforming children in preschool and primary school: Clinical and educational implications. J. Gay Lesbian Ment. Health 2019, 23, 117–144. [Google Scholar] [CrossRef]
- Vantieghem, W.; Van Houtte, M. Are girls more resilient to gender-conformity pressure? The association between gender-conformity pressure and academic self-efficacy. Sex Roles 2015, 73, 1–15. [Google Scholar] [CrossRef]
- Nielson, M.G.; Schroeder, K.M.; Martin, C.L.; Cook, R. Investigating the relation between gender typicality and pressure to conform to gender norms. Sex Roles 2020, 83, 523–535. [Google Scholar] [CrossRef]
- Shiffman, M.; VanderLaan, D.P.; Wood, H.; Hughes, S.K.; Owen-Anderson, A.; Lumley, M.M.; Lollis, S.P.; Zucker, K.J. Behavioral and emotional problems as a function of peer relationships in adolescents with gender dysphoria: A comparison with clinical and nonclinical controls. Psychol. Sex. Orientat. Gend. Divers. 2016, 3, 27–36. [Google Scholar] [CrossRef]
- Van Beusekom, G.; Baams, L.; Bos, H.M.; Overbeek, G.; Sandfort, T.G. Gender nonconformity, homophobic peer victimization, and mental health: How same-sex attraction and biological sex matter. J. Sex Res. 2016, 53, 98–108. [Google Scholar] [CrossRef]
- Gordon, A.R.; Conron, K.J.; Calzo, J.P.; White, M.T.; Reisner, S.L.; Austin, S.B. Gender expression, violence, and bullying victimization: Findings from probability samples of high school students in 4 US school districts. J. Sch. Health 2018, 88, 306–314. [Google Scholar] [CrossRef]
- Olson, J.; Schrager, S.M.; Belzer, M.; Simons, L.K.; Clark, L.F. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J. Adolesc. Health 2015, 57, 374–380. [Google Scholar] [CrossRef]
- Deutsch, M.B. Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People; Center of Excellence for Transgender Health: San Francisco, CA, USA, 2016. [Google Scholar]
- Scandurra, C.; Dolce, P.; Vitelli, R.; Esposito, G.; Testa, R.J.; Balsam, K.F.; Bochicchio, V. Mentalizing stigma: Reflective functioning as a protective factor against depression and anxiety in transgender and gender-nonconforming people. J. Clin. Psychol. 2020, 76, 1613–1630. [Google Scholar] [CrossRef] [PubMed]
- Scandurra, C.; Pennasilico, A.; Esposito, C.; Mezza, F.; Vitelli, R.; Bochicchio, V.; Maldonato, N.M.; Amodei, A.L. Minority stress and mental health in Italian bisexual people. Soc. Sci. 2020, 9, 46. [Google Scholar] [CrossRef]
- McGuire, J.K.; Anderson, C.R.; Toomey, R.B.; Russell, S.T. School climate for transgender youth: A mixed method investigation of student experiences and school responses. J. Youth Adolesc. 2010, 39, 1175–1188. [Google Scholar] [CrossRef] [PubMed]
- Russell, S.T.; Fish, J.N. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annu. Rev. Clin. Psychol. 2016, 12, 465–487. [Google Scholar] [CrossRef] [PubMed]
- Craig, S.L.; McInroy, L.B.; D’Souza, S.A.; Austin, A.; McCready, L.T.; Eaton, A.D.; Wagaman, M.A. Influence of information and communication technologies on the resilience and coping of sexual and gender minority youth in the United States and Canada (Project #Queery): Mixed methods survey. JMIR Res. Protoc. 2017, 6, e189. [Google Scholar] [CrossRef] [PubMed]
- Steinke, C.M.; Derrick, R.M. An exploration of the role of adverse childhood experiences (ACEs) on youth engagement in residential treatment. Child. Youth Serv. Rev. 2018, 89, 335–363. [Google Scholar] [CrossRef]
- Khanlou, N.; Wray, R. A whole community approach toward child and youth resilience promotion: A review of resilience literature. Int. J. Ment. Health Addict. 2014, 12, 64–79. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G.; Groleau, J.M. Clinical applications of posttraumatic growth. In Positive Psychology in Practice; Joseph, S., Ed.; John Wiley & Sons: New York, NY, USA, 2015; pp. 503–518. [Google Scholar] [CrossRef]
- Zucker, K.J.; Bradley, S.J.; Lowry Sullivan, C.B. Traits of separation anxiety in boys with gender identity disorder. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 791–798. [Google Scholar] [CrossRef]
- Cohen-Kettenis, P.T.; Owen, A.; Kaijser, V.G.; Bradley, S.J.; Zucker, K.J. Demographic characteristics, social competence, and behavior problems in children with gender identity disorder: A cross-national, cross-clinic comparative analysis. J. Abnorm Child. Psychol. 2003, 31, 41–53. [Google Scholar] [CrossRef]
- Rijn, A.B.; Steensma, T.D.; Kreukels, B.P.; Cohen-Kettenis, P.T. Self-perception in a clinical sample of gender variant children. Clin. Child Psychol. Psychiatry 2013, 18, 464–474. [Google Scholar] [CrossRef]
- Olson, K.R. Prepubescent transgender children: What we do and do not know. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 155–156. [Google Scholar] [CrossRef]
- De Graaf, N.M.; Cohen-Kettenis, P.T.; Carmichael, P.; de Vries, A.; Dhondt, K.; Laridaen, J.; Pauli, D.; Ball, J.; Steensma, T.D. Psychological functioning in adolescents referred to specialist gender identity clinics across Europe: A clinical comparison study between four clinics. Eur. Child Adolesc. Psychiatry 2018, 27, 909–919. [Google Scholar] [CrossRef] [PubMed]
- De Vries, A.L.; Steensma, T.D.; Cohen-Kettenis, P.T.; VanderLaan, D.P.; Zucker, K.J. Poor peer relations predict parent- and self-reported behavioral and emotional problems of adolescents with gender dysphoria: A cross-national, cross-clinic comparative analysis. Eur. Child Adolesc. Psychiatry 2016, 25, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Veale, J.F.; Watson, R.J.; Peter, T.; Saewyc, E.M. Mental health disparities among Canadian transgender youth. J. Adolesc. Health 2017, 60, 44–49. [Google Scholar] [CrossRef]
- Katz-Wise, S.L.; Budge, S.L.; Fugate, E.; Flanagan, K.; Touloumtzis, C.; Rood, R.; Perez-Brumer, A.; Leibowitz, S. Transactional pathways of transgender identity development in transgender and gender-nonconforming youth and caregiver perspectives from the Trans Youth Family Study. Int. J. Transgenderism 2017, 18, 243–263. [Google Scholar] [CrossRef] [PubMed]
- Neff, K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef]
- Hatchel, T.; Merrin, G.J.; Espelage, A.D. Peer victimization and suicidality among LGBTQ youth: The roles of school belonging, self-compassion, and parental support. J. LGBT Youth 2019, 16, 134–156. [Google Scholar] [CrossRef]
- Levant, R.F.; Powell, W.A. The gender role strain paradigm. In The Psychology of Men and Masculinities; Levant, R.F., Wong, Y.J., Eds.; American Psychological Association: Washington, DC, USA, 2017; pp. 15–43. [Google Scholar] [CrossRef]
- Reidy, D.E.; Brookmeyer, K.A.; Gentile, B.; Berke, D.S.; Zeichner, A. Gender role discrepancy stress, high-risk sexual behavior, and sexually transmitted disease. Arch. Sex. Behav. 2016, 45, 459–465. [Google Scholar] [CrossRef]
- Reidy, D.E.; Smith-Darden, J.P.; Cortina, K.S.; Kernsmith, R.M.; Kernsmith, P.D. Masculine discrepancy stress, teen dating violence, and sexual violence perpetration among adolescent boys. J. Adolesc. Health 2015, 56, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Harrington, A.G.; Overall, N.C.; Maxwell, J.A. Feminine gender role discrepancy strain and women’s self-esteem in daily and weekly life: A person X context perspective. Sex Roles 2022, 87, 35–51. [Google Scholar] [CrossRef]
- Craig, S.L.; Austin, A. The AFFIRM open pilot feasibility study: A brief affirmative cognitive behavioral coping skills group intervention for sexual and gender minority youth. Child. Youth Serv. Rev. 2016, 64, 136–144. [Google Scholar] [CrossRef]
- Levenson, J. Trauma-informed social work practice. Soc. Work 2017, 62, 105–113. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association. Guidelines for Psychological Practice with Transgender and Gender Nonconforming People. Am. Psychol. 2015, 70, 832–864. [Google Scholar] [CrossRef] [PubMed]
- Coleman, E.; Radix, A.E.; Bouman, W.P.; Brown, G.R.; de Vries, A.L.; Deutsch, M.B.; Ettner, R.; Fraser, L.; Goodman, M.; Green, J.; et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int. J. Transgender Health 2022, 23, S1–S259. [Google Scholar] [CrossRef]
- Tuck, E. Suspending damage: A letter to communities. Harv. Educ. Rev. 2009, 79, 409–427. [Google Scholar] [CrossRef]
- Levitt, H.M.; Kehoe, K.A.; Hand, A.B. Beyond minority stress: Toward a multidimensional psychology of trans/nonbinary gender. Curr. Opin. Psychol. 2022, 49, 101515, Advance online publication. [Google Scholar] [CrossRef]
| Author(s) | Country | Study Design | Sample Size | [Age Range] Mean (SD) | Types of Respondent | Measures |
|---|---|---|---|---|---|---|
| Becerra-Culqui et al., 2018 [53] | N/A | Cross-sectional | 1333 TGD, 26,300 cisgenders | [3–17] N/A | TGD youth | Anxiety disorder, ADHD, ASD, conduct and/or disruptive disorder, depressive disorder, eating disorders |
| Bluth et al., 2021 [54] | USA and Canada | Non-randomized experimental | 41 | [13–17] 14.5 (1.49) | TGD adolescents | Self-compassion (17 items from the SCS-Y), student life satisfaction (SLSS), state anxiety (ANX-SF), depression (PHQ-9), interpersonal needs (INQ), resilience (BRS) |
| Cheung et al., 2020 [55] | Thailand | Cross-sectional | 2070 | [13–18] N/A | TGD adolescents | Gender role conformity, peer victimization, current health risk behaviors, depressive symptoms |
| Chodzen et al., 2018 [12] | USA | Cross-sectional | 109 | [12–18] 15.46 (1.55) | TGD adolescents | Mental health (i.e., Major Depression Disorder and Generalized Anxiety Disorder) (YI-4), appearance congruence (TCS, AC subscale), minority stress and resilience (GMSR) |
| Clark et al., 2014 [12] | New Zealand | Cross-sectional | 8166 | N/A | TGD adolescents | Awareness of or disclosure about being transgender, protective factors (i.e., feeling cared about, family relationships), violence and personal safety, mental health (i.e., depression, self-harm, suicide attempts, having drunk alcohol in the past month, having had sex, health care access) |
| Craig et al., 2020 [56] | USA and Canada | Cross-sectional | 3508 | [14–18] 16.02 (1.24) | TGD adolescents | ACEs (ACE Scale) |
| Durwood et al., 2017 [14] | USA and Canada | Cross-sectional | (a) for depression and anxiety measurements: 63 TGD, 63 cisgenders, 38 siblings (b) for self-worth measurements: 116 TGD, 122 cisgenders | (a) [9–14] 10.8 (1.3) (b) [6–14] N/A | TGD youth, caregivers | Internalizing psychopathology (PROMIS scale); self-worth (Global Self-Worth Subscale from the Harter Self-Perception Profile for Children) |
| Durwood et al., 2021 [57] | USA | Cross-sectional | 265 | [3–15] 9.41 (2.62) | Caregivers | Family-, peer-, school-, and state-level support, victimization, internalizing symptoms (NIH PROMIS Scales for Anxiety and Depression, parent proxy short forms) |
| Eisenberg et al., 2017 [58] | USA | Cross-sectional | 2168 | [14–17] N/A | TGD adolescents | Risk behaviors and experiences (i.e., substance use, sexual behavior, emotional distress, bullying, victimization), emotional distress (i.e., depression, anhedonia) (PHQ-2), family connectedness, teacher-student relationship (SEI), feeling of safety in the community |
| Hill et al., 2010 [59] | USA and Canada | Cross-sectional | 31 TGD, 42 parents (16 mother and father or lesbian couples; 16 one parent) | [4–17.5] 8.0 | Caregivers | Emotional and maladaptive behaviors (CBCL), extent of child cross-gendering (GIQ), anti-transgender attitudes (GTS) |
| Katz-Wise et al., 2018 [60] | USA | Cross-sectional | 96: (a) 33 TGD youth (b) 48 cisgender caregivers (c) 15 cisgender siblings | (a) [13–17] 15.18 (1.24) (b) [37–69] 50.33 (6.70) (c) [14–24] 17.93 (3.28) | TGD adolescents, cisgender caregivers, cisgender siblings of TGD adolescents | Family communication (8-item subscale from FACES IV), family satisfaction (10-item subscale from FACES IV), suicidality (YRBSS), self-harm, depression (CES-D Short Form), anxiety (SCAS), self-esteem (RSES), resiliency (READ) |
| Kolbuck et al., 2019 [61] | USA | Cross-sectional | 71 | [3–11] 7.79 (2.08) | Caregivers | Gender nonconformity (GIQC), parenting stress (PSI-SF), parental support (PSGV), psychological functioning (CSI and ECI) |
| Kuper et al., 2019 [62] | USA | Cross-sectional | 396: 149 TGD youth; 137 mothers; 110 fathers | [12–18] 15.3 (1.52) | Adolescents, caregivers | CBCL (completed by parents/guardians), YSR and BIS (completed by adolescents) |
| Lowry et al., 2018 [9] | USA | Cross-sectional | 6082 | [14–18] N/A | TGD adolescents | Gender expression, sexual identity, substance use and mental distress (YRBS) |
| Mahfouda et al., 2019 [63] | Australia | Cross-sectional | 104 TGD | 14.62 (1.72) | Children, caregivers | Autistic traits (SRS-2), behavioral and emotional difficulties (YSR), health-related quality of life and adaptive functioning (Pediatric Quality of Life Inventory) |
| Moyer et al., 2018 [64] | USA | Cross-sectional | 79 | [11–18] 15.6 (1.8) | Medical doctor | Depression (PHQ-9), anxiety (GAD-7) |
| Munroe et al., 2020 [65] | USA | Longitudinal | 45 TGD children; 45 caregivers | [6–12] 8.5 (1.5) | Caregivers | Emotional and maladaptive behaviors (CBCL), caregiver-rated family functioning (Family Assessment Device), peer problems (peer relations subscale of the CBCL) |
| Nahata et al., 2017 [66] | USA | Retrospective cohort | 79 | [9–18] 15 | TGD youth | Insurance coverage, mental health diagnosis (i.e., depression, anxiety, PTSD, eating disorders, ASD, bipolar disorder), self-injurious behavior (i.e., suicidal ideation, self-harm, suicidal attempts), school victimization |
| Nic Rider et al., 2022 [67] | N/A | Cross-sectional | 67,806 (1024 TGD; 66,782 cisgenders) | [14–17] N/A | TGD youth, cisgender individuals | Sex trading, mental health, teacher-student relationship (4 items from SEI), feeling of safety at school |
| Olson et al., 2016 [68] | USA | Cross-sectional | 73 TGD; 49 siblings; 73 cisgender controls | [3–12] 7.7 (2.2) | Caregivers | Symptoms of anxiety and depression (PROMIS—Parental Proxy short forms for anxiety and depression) |
| Parodi et al., 2022 [69] | USA | Cross-sectional | 252 | [14–18] 16.07 (1.01) | TGD adolescents | Anxiety (GAD-7), depression (PHQ-2), non-suicidal self-injury (Youth Risk Behavior Survey), PTSD (PC-PTSD-5), school connectedness (PSSM), presence of GSAs, nondiscrimination laws in the state of residence |
| Perl et al., 2021 [70] | Israel | Cross-sectional | 76 (18 TGD, 58 cisgender) | [9–18] N/A | TGD youth | Coronavirus health impact (CRISIS-V0.2), emotion regulation (ERQ) |
| Reidy et al., 2018 [71] | USA | Cross-sectional | 592 | [11–16] 13.1 (1.6) | TGD youth | GRD and masculine discrepancy stress (MDSS), trauma (Child PTSD Symptom Scale), neighborhood disorganization (RYDS), ACEs, psychosocial adjustment, substance use, sexual behavior, mood disorder symptom (K6), hopelessness (HSC), violence (NYS) |
| Reisner et al., 2015 [26] | USA | Cross-sectional | 5907 | [13–18] N/A | TGD adolescents | Gender minority identity, past-12-month ever and regular substance use, past-12-month bullying experiences |
| Russell et al., 2022 [72] | USA | Cross-sectional | 58 | [9,10] 10.03 (0.62) | Caregivers | Emotional and maladaptive behaviors (CBCL) |
| Shumer et al., 2015 [73] | USA | Cross-sectional | 2128 youth, 2876 caregivers | [9–14] N/A | Youth, mothers | Social functioning, reciprocal social interaction, restrictive or stereotypical behaviors associated with ASD (SRS) |
| Stewart et al., 2021 [74] | USA and Canada | Cross-sectional | 94,804 | [4–18] 12.1 (3.72) | Medical doctor | Youth’s mental health needs and risks (interrail ChYMH), child’s functioning and aids (interRAI ChYMH Screener (ChYMH-S), child’s functioning (interRAI ChYMH Screener) |
| Turban et al., 2021 [75] | USA | Cross-sectional | 9711 | [18–65+] 34.8 (13.9) | TGD adults | Mental health, age recalled for social transition |
| Vance et al., 2021 [76] | USA | Cross-sectional | 19,780: 252 Black and Latinx TGD individuals, 104 White TGD individuals, 19,424 Black and Latinx cisgender individuals | [14,15] N/A | TGD adolescents, cisgenders | Mental health (depressive symptomatology, suicidal ideation), school-based victimization, harassment, school connectedness |
| VanderLaan et al., 2017 [77] | N/A | Cross-sectional | 360 AMAB | [N/A] 6.86 (2.31) | TGD children | Separation anxiety (SAI), gender non-conformity (GIIC, GIQC), CBCL |
| Van der Miesen et al., 2018 [78] | Canada | Cross sectional | 1719 | [6–12] N/A | Caregivers | Extent of childhood cross-gendering (GIQC), emotional and maladaptive behaviors (CBCL) |
| Wang et al., 2020 [79] | China | Cross-sectional | 12,108: 2111 TGD, 9997 cisgenders | [N/A] 15.8 (1.0) | TGD and cisgender adolescents | Physical health (SFSI, item 1), depressive symptoms (PHQ-9), anxiety symptoms (GAD-7), sleep quality (CPSQI), bullying, self-harm and suicidal ideation |
| Watson et al., 2021 [80] | USA | Cross-sectional | 8831 | [13–17] 15.59 (1.27) | TGD adolescents | LGBTQ equity index, substance use (i.e., recent alcohol use, binge drinking, cigarette use), bias-based bullying |
| Author(s) | 1a | 2a | 3a | 4a | 5a | 6a | 7a | 8a | 9a | 10a | 11a | 12a | 13a | 14a | Overall Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Becerra-Culqui et al., 2018 [53] | Yes | Yes | N.R. | Yes | No | No | No | N.A | Yes | N.A. | Yes | N.A. | N.A. | Yes | Good |
| Cheung et al., 2020 [55] | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | N.A. | N.A. | Yes | Good |
| Chodzen et al., 2018 [18] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Clark et al., 2014 [12] | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | N.A. | N.A. | Yes | Good |
| Craig et al., 2020 [56] | Yes | Yes | Yes | Yes | No | No | No | N.A | Yes | N.A. | Yes | N.A. | N.A. | N.A. | Good |
| Durwood et al., 2017 [14] | Yes | Yes | N.R. | Yes | No | No | No | N.A | Yes | N.A. | Yes | N.A. | N.A. | N.A. | Good |
| Durwood et al., 2021 [57] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Eisenberg et al., 2017 [58] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | N.A. | Good |
| Hill et al., 2010 [59] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | No | Fair |
| Katz-Wise et al., 2018 [60] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Kolbuck et al., 2019 [61] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Kuper et al., 2019 [62] | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Lowry et al., 2018 [9] | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Mahfouda et al., 2019 [63] | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Moyer et al., 2018 [64] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | N.A. | Fair |
| Munroe et al., 2020 [65] | Yes | Yes | N.R. | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | N.A. | N.A. | No | Good |
| Nahata et al., 2017 [66] | Yes | Yes | N.R. | Yes | No | No | No | N.A. | Yes | No | No | N.A. | N.A. | N.A. | Fair |
| Nic Rider et al., 2022 [67] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | N.A. | Good |
| Olson et al., 2016 [68] | Yes | Yes | N.R. | Yes | No | No | No | N.A. | Yes | No | Yes | N.A. | N.A. | N.A. | Good |
| Parodi et al., 2022 [69] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Perl et al., 2021 [70] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | No | Fair |
| Reidy et al., 2018 [71] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Reisner et al., 2015 [26] | Yes | Yes | Yes | Yes | No | No | No | N.A. | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Russell et al., 2022 [72] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Shumer et al., 2015 [73] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Stewart et al., 2021 [74] | Yes | Yes | N.R. | Yes | No | No | No | N.A. | Yes | No | Yes | N.A. | N.A. | Yes | Fair |
| Turban et al., 2021 [75] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Vance et al., 2021 [76] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| VanderLaan et al., 2017 [77] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Van der Miesen et al., 2018 [78] | Yes | Yes | N.R. | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Wang et al., 2020 [79] | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | Yes | N.A. | N.A. | Yes | Good |
| Watson et al., 2021 [80] | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | No | N.A. | N.A. | Yes | Good |
| 1b | 2b | 3b | 4b | 5b | 6b | 7b | 8b | 9b | 10b | 11b | 12b | − | − | Overall rating | |
| Bluth et al., 2021 [54] | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | − | − | Good |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mezzalira, S.; Scandurra, C.; Mezza, F.; Miscioscia, M.; Innamorati, M.; Bochicchio, V. Gender Felt Pressure, Affective Domains, and Mental Health Outcomes among Transgender and Gender Diverse (TGD) Children and Adolescents: A Systematic Review with Developmental and Clinical Implications. Int. J. Environ. Res. Public Health 2023, 20, 785. https://doi.org/10.3390/ijerph20010785
Mezzalira S, Scandurra C, Mezza F, Miscioscia M, Innamorati M, Bochicchio V. Gender Felt Pressure, Affective Domains, and Mental Health Outcomes among Transgender and Gender Diverse (TGD) Children and Adolescents: A Systematic Review with Developmental and Clinical Implications. International Journal of Environmental Research and Public Health. 2023; 20(1):785. https://doi.org/10.3390/ijerph20010785
Chicago/Turabian StyleMezzalira, Selene, Cristiano Scandurra, Fabrizio Mezza, Marina Miscioscia, Marco Innamorati, and Vincenzo Bochicchio. 2023. "Gender Felt Pressure, Affective Domains, and Mental Health Outcomes among Transgender and Gender Diverse (TGD) Children and Adolescents: A Systematic Review with Developmental and Clinical Implications" International Journal of Environmental Research and Public Health 20, no. 1: 785. https://doi.org/10.3390/ijerph20010785
APA StyleMezzalira, S., Scandurra, C., Mezza, F., Miscioscia, M., Innamorati, M., & Bochicchio, V. (2023). Gender Felt Pressure, Affective Domains, and Mental Health Outcomes among Transgender and Gender Diverse (TGD) Children and Adolescents: A Systematic Review with Developmental and Clinical Implications. International Journal of Environmental Research and Public Health, 20(1), 785. https://doi.org/10.3390/ijerph20010785









